* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cryptococcal meningitis Melicent Peck MD, PhD Stanford University Department of Medicine
Meningococcal disease wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Cryptosporidiosis wikipedia , lookup
Leptospirosis wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Microbicides for sexually transmitted diseases wikipedia , lookup
Onchocerciasis wikipedia , lookup
Diagnosis of HIV/AIDS wikipedia , lookup
Epidemiology of HIV/AIDS wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
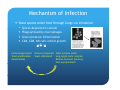
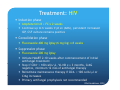
Cryptococcal meningitis Melicent Peck MD, PhD Stanford University Department of Medicine Case One HPI: 73 y/o male admitted for 3-week h/o acute memory loss. Per pt’s wife, pt getting lost, repeating same story over and over, unable to recall details of recent events. No F/C, no HA, no recent illness. Patient had acute-onset aphasia in 07/09 and 09/09 with resolution over several weeks. Found to have L temporal stroke on MRI brain. PMHx: IDDM, HLD, HTN, vertigo (x 2 years, attributed to Meniere's disease) Meds: Metformin, Lantus, Nicardipine, Citicholine SR SHx: No etoh, tobacco. Retired administrator, lives in Bangalore, India but travels to US ~ 1x/year to see family. No rural contacts, no hiking, no pets. FHx: NC PE: VSS. AAO x 3. Exam unremarkable. Labs: Na 133, CRP < 0.2, ESR 38, HIV negative, serum CrAg 1:4 LP: OP 22cm, 116 wbc ((N28L66M6)), 12,625 rbc, xanthochromia, g glucose 69, TP 536, CrAg g 1:4 Gram Stain: small number polys, small number PMNs, small number rbc, no organisms, Cx: NGTD MRI brain: new temporal lobe CVA Case Two HPI: 55 y/o male with h/o HIV (CD4+ 2 cells/l, VL 1850 copies/ml) not on HAART with OI disseminated KS and Candidiasis, homeless admitted for abdominal pain, SOB. Pt found to have SBO s/p lysis of adhesions, PNA 2/2 KS vs CAP. +HA primarily in morning, diffuse. PMHx: HIV (1990), disseminated KS (lung, skin), Candidiasis (esophageal), polysubstance abuse Meds: Atazanavir, Truvada, Ritonovir, Bactrim, Fluconazole, Azithromycin SHx: Homeless, + etoh, + crack cocaine FHx: NC PE: VS: RR 24 Chronically ill-appearing male, cachectic OP: oral thrush, areas of mild ulceration on hard palate, CV: RRR no mrg Lung: diffuse coarse crackles, decreased BS in RLL Abd: TTP RLQ with voluntary guarding Skin: 2 x 2 cm violaceous macule on dorsum of L foot Neuro: non-focal Labs: Hct 29, Na 132, albumin 2 BCx +Cryptococcemia, CrAg 1:256 LP <1 LP: 1 wbc, b <1 1 rbc, b Glucose Gl 66, 66 TP 24 24,CrAg C A 1:8 18 GS: no polys, no orgs Cx: NGTD Fungal Cx: Cryptococcus neoformans (liquid media, not on plate) CT Head: unremarkable DDX: Chronic Meningitis Bacteria Mycobacterium Tb Syphilis Lyme disease Nocardiosis Parasites Cysticercosis y Acanthamebiasis Fungal • Cryptococcosis Coccidiomycosis Histoplasmosis Candidiasis Aspergillosis Viral • • HSV VZV •Sarcoid •Tumor Cryptococcal Meningitis Signs/Symptoms HA,, F,, nuchal rigidity, g y, p photophobia p Decreased vision, unsteady gait, CN palsies Confusion, lethargy, memory loss over several weeks Seizure or strokes in multiple vascular territories Causative Agent Strain Global Distribution Environmental Reservoir C. neoformans Global Temperate climates Pigeon droppings/ guano/ birds nests Rotting g vegetation g Epidemiology Occurs O in i ~ 1 million illi people l per year ~600,000 deaths annually 3-month mortality rate ~20% in developed countries, ~70% in Africa Primarily seen in immunocompromised patients Newly diagnosed HIV patients Most common OI in AIDS (CD4+ < 50 cells/l) Incidence 0.04%-12% per year Look for co-morbid CNS processes (Toxoplasma, Nocardia, lymphoma) Solid organ transplant patients Median time to disease onset 21 months after transplantation g transplant p recipients p Documented in 2.8% of sold-organ High dose CS, monoclonal Abs, other immunosuppressants Global disease burden Sub-Saharan Sub Saharan Africa > S and SE Asia > Latin America > E Europe and Central Asia > > N America > N Africa and Middle East> W and Central Europe 95% of cryptococcal meningitis cases in developing countries are HIV associated i t d Account for 10-20% of all deaths in HIV infected patients in Africa (> Tb) Pathogenesis g Virulence Factors Capsule Antiphagocytosis barrier, depletes complement, dysregulates cytokine secretion Melanin Antioxidant (UV light, toxic free radicals), interferes with T-cell response Growth at high-temperature (37o C) Mechanism of Infection Yeast spores enter host through lungs via inhalation Spores deposited in alveoli Phagocytosed by macrophages Granulomatous inflammation CD4, CD8, NK cells inhibit growth Immunosuppressed Yeast proliferates/ disseminates Immunocompetent Yeast produce small Yeast eliminated lung-lymph node complex Remain dormant (latency) Host asymptomatic y p Clinical Manifestations Lung 1/3 pts asymptomatic (abnormal CXR with single or multiple pulmonary nodules) PNA (F, chest pain, SOB, productive cough) CXR: lobar infiltrate, hilar LAD, pleural effusions, lung cavitations CNS Subacute meningitis or meningoencephalitis Skin Ulceration, cellulitis, abscess Prostate Usually asymptomatic Can serve as reservoir of infection Eye Ocular p palsies,, p papilledema p Can lead to blindness Optic neuritis Cerebral edema 2/2 elevated ICPs Bone/joint (osteolytic lesion) Diagnosis CSF Elevated opening pressure Mononuclear pleocytosis Elevated protein Decreased glucose (< 40mg/dl) Cryptococcal antigen Direct detection (India Ink) Spherical, narrow based, budding, encapsulated yeast 50% of non non-AIDS AIDS pts, 80% of AIDS pts CNS positive Culture Growth 48-72 hours on laboratory media at 20-37o C Routine R ti blood bl d culture lt can d detect t t cryptococcemia t i (3 (3-7 7 days) d ) CSF fungal culture Diagnosis Serology Cryptococcal polysaccharide antigen (sera and CSF) Latex agglutination and enzyme immunoassay >90% sensitive and specific CSF titer ≥ 1:4 positive Titer ≥ 1:1024 -High burden of yeasts, poor host immunity, greater chance of therapeutic h ffailure l Serial titers imprecise but can be used for disease follow-up Can be negative in pulmonary disease Radiology No pathognomonic scan CT brain: cryptococcomas (single/multiple), hydrocephalus, gyral enhancement 50% of CT scans normal MRI brain: hyperintense clustered foci in basal ganglia or midbrain Follow-up scans may show worsening of lesions Represents enhancement by inflammation as yeast being eliminated Not necessarilyy treatment failure Treatment: Drugs Amphotericin B Amphotericin B deoxycholate (0.7 mg/kg/day) Nephrotoxic Acute infusion rxn (F/C, N/V, SOB) Liposomal amphotericin B (Ambisome:3-6 mg/kg/day) Amphotericin B lipid complex (Abelcet:3-6 (Abelcet:3 6 mg/kg/day) Flucytosine (100 mg/kg/day) (FC) MIC ≥ 128 g/ml associated with treatment failure Drug resistance as monotherapy Monitor for cytopenias 2hr post-dose level 30-80 g/ml 3-5 days after initiation of treatment Fluconazole (200-1200 mg/day) MIC ≥ 16 g/ml g/ml associated with treatment failure Resistance emerging problem when used as monotherapy (Africa) Treatment: HIV Induction phase Amphotericin B + FC x 2 weeks Continue up to 6 weeks if pt sx (AMS), (AMS) persistent increased ICP, CSF culture remains positive Consolidation phase p Fluconazole 400 mg Qday (6 mg/kg) x 8 weeks Suppressive phase Fluconazole 200 mg Qday Initiate HAART 2-10 weeks after commencement of initial antifungal treatment Stop if CD4+ > 100 cells/l, VL ND x ≥ 3 months, CrAG negative, minimum 12 mos of antifungal therapy Reinstitute maintenance therapy if CD4+ < 100 cells/l or C A iincreases CrAg Primary antifungal prophylaxis not recommended IDSA Guidelines, 2010 Treatment: Organ Transplant Induction phase Amphotericin B + FC x 2 weeks Consolidation phase Fluconazole 400 mg-800 mg Qday (6 mg/kg) x 8 weeks Suppressive phase Fluconazole 200-400 mg Qday x 6-12 months Reduce immunosuppressants Lower prednisone to < 20 mg/day IDSA Guidelines, 2010 Treatment: Normal Induction phase Amphotericin B + FC x 4 weeks No neurological l l complications l CSF culture results negative after 2 weeks of treatment Extend treatment to 6 weeks if neurological complications If low-risk for therapeutic failure can shorten treatment to 2 weeks Consolidation phase Fluconazole 400 mg Qday (6 mg/kg) x 8 weeks Suppressive phase Fluconazole 200 mg Qday x 6-12 months IDSA Guidelines, 2010 Elevated ICP Seen in ~ 50% of HIV infected patients Linked to high burden of yeast in CSF Opening CSF pressure ≥ 25 cm H2O + symptoms CSF drainage to reduce OP by 50% or to ≤ 20 cm H2O Repeat LP daily until CSF pressure and sx stabilized for > 2 days Consider placement of temporary CSF shunt or lumbar drain IDSA Guidelines, 2010 Treatment in Resource-Limited S tti Settings Induction/Consolidation Amphotericin B (1 mg/kg/day) x 2 weeks -> fluconazole (800 mg/day) x 8 weeks Amphotericin B (0.7 mg/kg/day) + fluconazole (800 mg/day) x 2 weeks -> fluconazole (800 mg/day) x 8 weeks Fluconazole (1200 mg/day) + FC (100 mg/kg/day) x 2-10 weeks Fluconazole (1200 mg/day) x 10-12 weeks Maintenance M i t Fluconazole 200-400 mg/day Open-labeled p RCT in Malawi ((2008)) HIV positive adults (mean CD4+ count 21 cells/l, VL 99,000 cells/ml) with first episode of cryptococcal meningitis Patients with ANC < 500, plt < 50K, ALT > 200, or on ART excluded Randomized to fluconazole (1200 mg/day) (n (n=20) 20) vs fluconazole + FC (100 mg/kg/day) (n=21) x 14 days -> 800 mg fluconazole Qday ART started after 4 weeks of antifungal therapy Monitored LP at t =0, 1, 3, 7, 14 days More frequent LP if OP > 30 cm H2O (mean OP at baseline 34 cm H2O) Followed LFTs, creatinine, CD4+ cells, HIV VL at baseline, LFTS and cbc at weeks 1,2,4,6,10. Primary outcome: mean rate of decrease in CSF cryptococcal counts Secondary S d outcomes: t serious i adverse d events, t d drug S/E S/E, mortality t lit att 2 & 10 weeks Results/Conclusions Fungicidal Activity: High-dose fluconazole + FC > than high high-dose dose fluconazole alone (p< 0.001). Four patients in combination arm and one in monotherapy arm had sterile cultures lt att D14 D14. 10% 37% 43% 58% Survival: Trend toward improved survival at 2 and 10 weeks among patients who received combination therapy. Results/Conclusions Safety: Combination regimen safe w/o monitoring g FC levels Limitations: -FC not available in most of developing world, including Africa -Underpowered to detect mortality benefit References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10 10. 11. 12. Buchanan K & Murphy p y J ((1998)) What makes Cryptococcus yp neoformans a p pathogen? g Emerging Infectious Diseases 4(1):71-83. Idnurm A, et al. (2005) Deciphering the model pathogenic fungus Cryptococcus neoformans. Nat Rev Microbiol 3(10):753-764. Longley N, et al. (2008) Dose response effect of high-dose fluconazole for HIV-associated cryptococcal meningitis in southwestern Uganda. Uganda Clin Infect Dis 47(12):1556-1561. 47(12):1556 1561 Mandell G, Bennett J, & Dolin R (2010) Principles and Practices of Infectious Diseases,. (Churchill Livingstone) 7th Ed p 4320. Makombe SD, Nkhata A, Schouten EJ, Kamoto K, & Harries AD (2009) Burden of cryptococcal meningitis in Malawi. Trop Doct 39(1):32-34. Mayanja-Kizza H, et al. (1998) Combination therapy with fluconazole and flucytosine for cryptococcal meningitis in Ugandan patients with AIDS. Clin Infect Dis 26(6):1362-1366. Nussbaum JC, et al. (2010) Combination flucytosine and high-dose fluconazole compared with fluconazole monotherapy for the treatment of cryptococcal meningitis: a randomized trial in Malawi Clin Infect Dis 50(3):338 Malawi. 50(3):338-344 344. Pappas PG (2010) Cryptococcosis in the developing world: an elephant in the parlor. Clin Infect Dis 50(3):345-346. Park BJ, et al. (2009) Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS 23(4):525-530. P f t JR, Perfect JR ett al. l (2010) Cli Clinical i l practice ti guidelines id li ffor th the managementt off cryptococcal t l disease: 2010 update by the infectious diseases society of america. Clin Infect Dis 50(3):291322. Sloan D, Dlamini S, Paul N, & Dedicoat M (2008) Treatment of acute cryptococcal meningitis in HIV infected adults,, with an emphasis p on resource-limited settings. g Cochrane Database Syst y Rev (4):CD005647. Sloan DJ, Dedicoat MJ, & Lalloo DG (2009) Treatment of cryptococcal meningitis in resource limited settings. Curr Opin Infect Dis 22(5):455-463.