* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Therapy with anti-flagellin A monoclonal antibody limits
Survey
Document related concepts
Human microbiota wikipedia , lookup
Bacterial cell structure wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Triclocarban wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Urinary tract infection wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Sarcocystis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Hepatitis C wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
Hepatitis B wikipedia , lookup
Infection control wikipedia , lookup
Transcript
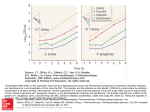
JBUR-2892; No of Pages 7 burns xxx (2008) xxx–xxx available at www.sciencedirect.com journal homepage: www.elsevier.com/locate/burns Therapy with anti-flagellin A monoclonal antibody limits Pseudomonas aeruginosa invasiveness in a mouse burn wound sepsis model Yoav Barnea a,b,*, Yehuda Carmeli a, Lewis F. Neville c, Hamutal Kahel-Reifer c, Rachel Eren c, Shlomo Dagan c, Shiri Navon-Venezia a a The Division of Epidemiology & Laboratory for Molecular Epidemiology and Antimicrobials Research, Israel The Department of Plastic and Reconstructive Surgery, Tel Aviv Sourasky Medical Center, Affiliated with the Sackler Faculty of Medicine, Israel c XTL Biopharmaceuticals, Rehovot, Israel b article info abstract Article history: Background: The aim of this study was to evaluate the effect of an anti-flagellin sub-type Accepted 12 August 2008 monoclonal antibody (anti-fla-a) on Pseudomonas aeruginosa infection in a mouse burn model and to assay bacterial dissemination and invasiveness. Keywords: Methods: After immediate post-burn infection with P. aeruginosa, mortality and morbidity Anti-flagellin A (daily weight changes) were monitored in mice treated with anti-fla-a as compared to Pseudomonas aeruginosa untreated mice. Bacterial dissemination and invasiveness were monitored by bacterial Mouse burn wound sepsis model counts at the burn site and spleen. Three different timing regimens for anti-fla-a treatment were studied: (a) prophylaxis (pre-infection), (b) therapeutic (post-infection), and (c) combined mode. Results: Combined regimen of anti-fla-a markedly improved survival of mice infected with P. aeruginosa from 6% to 96% ( p < 0.0001), similar to treatment with Imipenem. Furthermore, a significant improvement in survival was obtained when anti-fla-a was given prior to (75% survival) or post-infection (50% survival). It reduced bacterial load in the spleen ( p = 0.01), preventing bacterial sepsis. Conclusion: Anti-fla-a is effective in reducing mortality and morbidity in murine P. aeruginosa-infected burn model. # 2008 Elsevier Ltd and ISBI. All rights reserved. 1. Introduction Patients suffering from major burns have extensive disruption of the skin barrier, with a concurrent suppression of the immune system [1–3]. These conditions expose the burn area to bacterial wound colonization that can lead to burn wound infection, sepsis, multi-organ failure and subsequent death [1–6]. Bacterial infection is the leading cause of death in major burns (responsible to 50–80% of overall thermal injury mortality), and Pseudomonas aeruginosa is the most prevalent pathogen isolated from burn wound infections [5] mainly due to its high persistence in the environment and its high intrinsic and acquired antibiotic resistance [7–9]. Moreover, excessive antibiotic pressure in burn units has resulted in the * Corresponding author at: Department of Plastic and Reconstructive Surgery, Tel Aviv Sourasky Medical Center, 6 Weizmann Street, Tel Aviv 64239, Israel. Tel.: +972 3 697 3320; fax: +972 3 697 3890. E-mail address: [email protected] (Y. Barnea). 0305-4179/$34.00 # 2008 Elsevier Ltd and ISBI. All rights reserved. doi:10.1016/j.burns.2008.08.014 Please cite this article in press as: Barnea Y, et al. Therapy with anti-flagellin A monoclonal antibody limits Pseudomonas aeruginosa invasiveness in a mouse burn wound sepsis model. Burns (2008), doi:10.1016/j.burns.2008.08.014 JBUR-2892; No of Pages 7 2 burns xxx (2008) xxx–xxx emergence of multidrug-resistant strains of P. aeruginosa [5,10]. Therefore, supplemental approaches to antibiotic therapy such as immunotherapy, that can target centrally important virulent factors implicated in P. aeruginosamediated lethality, have been extensively investigated [11,12]. Flagellin protein, the principal component of bacterial flagellum, has long been recognized as an important virulence factor in Pseudomonas infections [13,14]. Flagellin’s effects are mediated via binding to Toll-5 receptor, TLR-5 [15], whose activation results in a profound inflammatory response [16]. Structure-function-studies revealed specific N0 - and C0 -terminal domains responsible for flagellin binding, pro-inflammatory signaling [15,17], and flagellar protofilament assembly and bacterial motility [18]. Since more than 95% of clinical P. aeruginosa isolates are flagellated (with either type-a or type-b antigen), specific-type monoclonal antibodies against flagellin demonstrated profound biological effects affording protection in lethal P. aeruginosa infection burn wound models [19,20]. Although the importance of motility to the pathogenesis of P. aeruginosa has been shown previously [21], the precise mechanism(s) by which anti-flagellin antibodies protect animals in experimental models of P. aeruginosa infection, have not yet been fully elucidated. In a previous study, we showed that antibodies raised against the highly conserved N0 -terminal region of P. aeruginosa flagellin dramatically improved the survival of mice in two different mouse models of lethal Pseudomonas infections [22]. Therefore, this study was aimed to further elucidate the primary mechanism of protection afforded by anti-Pseudomonas flagellin antibodies through employment of a mouse monoclonal antibody raised against this virulence factor. Specifically, we chose to work with a previously described anti-Pseudomonas type-a flagellin monoclonal antibody (termed anti-fla-a in this study) which was raised against P. aeruginosa-derived flagellin [19] and evaluate its specificity and therapeutic potential against a clinical strain of P. aeruginosa using a murine lethal infected burn wound sepsis model. Furthermore, the effects of (anti-fla-a) on the local and systemic dissemination of the bacteria were investigated. 2. Materials and methods 2.1. Anti-P. aeruginosa flagellin type-a and -b antibodies The mouse hybridoma FA6IIG5 (IgG3) raised against P. aeruginosa bacterium harboring flagellin type a [19] was obtained from ATCC. This hybridoma was grown in complete RPMI-1640 media and 5 106 cells injected into Pristaneprimed, nude female mice for the generation of ascites fluid. Ascites fluid was thereafter pooled, diluted 10-fold with PBS and purified on protein-G chromatography. Following extensive dialysis against PBS, the purified monoclonal antibody was stored at 20 8C as aliquots at a concentration of 1–5 mg/ ml. A polyclonal rabbit IgG raised against the N0 -terminal domain (amino acid nos. 1–156) of P. aeruginosa flagellin type-b was prepared as previously described [20]. Commercial rabbit IgG (not exposed to any immunogen) was used as a nonspecific IgG (NS-Ab) (Sigma, Rehovot, Israel) control in the in vivo experiments. 2.2. Preparation of P. aeruginosa flagellin proteins Purified, recombinant (E.coli-produced) N’-terminal P. aeruginosa flagellin types a and b (PAK and PA01 cDNA sequences) as well as the full-length flagellin proteins of both sub-types were prepared as previously described [22]. Exotoxin-A (List Biological Laboratories Inc., USA) was also included in immunoblots as a negative control protein. 2.3. Live bacterial ELISA screen Laboratory P. aeruginosa strains (PA01 and PAK) as well as a panel of different P. aeruginosa clinical strains including PA409 were grown overnight and diluted to an optical density of 0.2. One hundred ml of this culture was allowed to bind for 60 min at 37 8C to ELISA plates coated with poly-L-lysine. Plates were washed with PBS/Tween-20, blocked for 60 min at room temperature with 1% BSA and incubated with anti-fla-a (111–1000 ng/ml) for 30 min at 37 8C with constant shaking. Thereafter plates were taken for colorimetry assay with 5,50 tetramethylbenzidine substrate (TMB) used for detection of peroxidase activity following incubation with a peroxidase goat anti-mouse IgG (Zymed, CA). 2.4. Immunoblots 100 ng of purified, recombinantly-produced PA flagellin proteins were electrophoresed on SDS-PAGE gels (In-Vitrogen, CA), electro blotted onto Nitrocellulose and probed with antifla-a (final concentration = 0.5 mg/ml). Following washing with PBS/0.4% Tween-20, blots were incubated with peroxidase conjugated goat anti-mouse IgG (H+L; Zymed, 1:10,000 dilution) and taken for enhanced chemiluminescence (ECL). 2.5. Survival studies using mice Female CBL57 inbred mice, 18–20 g (Harlan Laboratories, Rehovot, Israel) were housed in specific pathogen free conditions using individually ventilated cages (IVC, Techniplast, Italy) in a central animal research facility. The facility maintains an environment of controlled temperature and relative humidity, with a 12-h light/dark cycle and laminar airflow compartments. The mice were supplied with sterile bedding, food and water. Each experimental group included 12 mice per group. All procedures, care and handling of the animals were reviewed and approved by the Tel-Aviv Medical Center Institutional Animal Care and Use Committee. A burn-wound sepsis model previously described by us was used to study the efficacy of antibodies [23,24]. In this model a non-lethal full-thickness burn wound consisting of 6–8% of the body surface area was induced in the right posterior flank area of mice. Infection was induced immediately after burn formation and fluid resuscitation by subeschar injection of 0.1 ml of a logarithmic culture of P. aeruginosa clinical strain PA409, which was shown to harbor antigenic flagellin type-a. The infecting bacterial inoculum was prepared on a brain heart infusion broth (BHI, Becton-Dickinson) with agitation (180 rpm) at 37 8C for 5–6 h. The cells were harvested (optical density of 0.8 at 620 nm), centrifuged and resuspended in a sterile BHI. The number of infected bacteria was verified by Please cite this article in press as: Barnea Y, et al. Therapy with anti-flagellin A monoclonal antibody limits Pseudomonas aeruginosa invasiveness in a mouse burn wound sepsis model. Burns (2008), doi:10.1016/j.burns.2008.08.014 JBUR-2892; No of Pages 7 burns xxx (2008) xxx–xxx plating serial dilutions of the injected inocula onto BHI agar plates. Based on previous data on the lethal dose (LD) of P. aeruginosa PA409 [23] an inoculum of 3 105 was used for all the in vivo studies corresponding to 5 times LD50 of the bacterium. incubation. The average concentrations of P. aeruginosa in the burn and in the spleen were calculated from an average of bacterial counts obtained from three mice that were sacrificed at each time point. 2.9. 2.6. 3 Statistical analysis Treatment modalities Prior to each in vivo experiment, freshly prepared antibody solutions were diluted in PBS to the desired concentration. Negative controls for anti-fla-a included a non-specific antibody (NS-Ab) and a polyclonal anti-P. aeruginosa flagellin typeb IgG fraction [22]. Imipenem freshly prepared before each experiment in PBS (0.01 M, pH 7.2) was used for the P. aeruginosa conventional systemic antibiotic control group. Anti-fla-a was given intraperitoneally as a combined regimen (0.05 mg 4 h before infection and at 4 h and once daily for 3 days after infection). Anti-fla-a was further studied in 2 other regimens: prophylaxis (pre-infection: 0.05 mg at 4 h before infection) and treatment (post-infection: 0.05 mg at 4 h and 20 h after infection). Imipenem was given intraperitoneally 0.5 mg 4 h after infection and twice daily for 4 days. Both NSAb and polyclonal anti-flagellin type-b were given as combined (pre- and post-infection) regimens, similarly to anti-flaa (0.5 mg 4 h before infection and at 4 h and once daily for 3 days after infection). Statistics were run in Stata version 7 (Stata Corp., College Station, Texas). The differences between the anti-fla-a-treated groups and the non-treated or the control NS IgG-treated groups were analyzed. Dichotomous outcomes were evaluated by Fisher’s exact test, and continuous variables by Student’s t-test. All tests were two-sided and a p < 0.05 was considered statistically significant. Each fitting curve point represents the average value of surviving mice in that group at that point in time. Non-surviving mice were excluded from the average calculation and were regarded as ‘‘blank’’ rather than zero. 3. Results 3.1. Specificity of anti-fla-a to Pseudomonas flagellin Morbidity and mortality post-PA409 injection was the primary outcome used to assess the in vivo efficacy of the anti-fla-a treatment. Mortality was monitored daily in both control and experimental groups for a period of 14 days from induction of infected burns. Morbidity was determined by monitoring the individual mouse’s daily weight changes. The mice were individually tagged and weighed before the infected burn induction and afterwards were weighed on days 1, 2, 3, 7, and 14 after burn infection. Relative body weight (%) was defined as the average body weight of each group at a point of time, relatively to the average baseline (pre-infected-burn) body weight (defined as 100%). Non-surviving mice at each point of time were excluded from the average body weight calculations. To confirm the specificity of the anti-fla-a towards Pseudomonas strains harboring flagellin proteins, laboratory P. aeruginosa strains PAK (flagellin type-a) and PA01 (flagellin type-b) as well as a panel of clinical P. aeruginosa isolates, were screened for anti-fla-a binding in a live bacterial assay. Immobilization of P. aeruginosa bacteria to coated ELISA plates followed by addition of anti-fla-a clearly confirmed the specificity of this monoclonal antibody towards type-a flagellin since positive reactivity was only observed towards PAK and one clinical P. aeruginosa isolate, strain PA409 (Fig. 1A). Further confirmation for specificity of anti-fla-a binding towards P. aeruginosa flagellin type-a was observed from immunoblots. In these studies, anti-fla-a binding was only observed towards the fulllength P. aeruginosa flagellin type a protein (Fig. 1B, lane 3), with no binding towards the full length type b flagellin (lane 4) or Nterminal flagellin types a (lane 1) and b (lane 2) domains. As anticipated, a control protein of exotoxin A (lane 5) was not recognized by anti-fla-a. 2.8. Bacterial proliferation, dissemination and burn histopathology 3.2. Anti-fla-a is protective against P. aeruginosa infection in passive administration Bacterial proliferation and dissemination was studied in the anti-fla-a-treated group and in the control groups (noninfected burn group, infected non-burned group and nontreated infected burn group). Surviving mice were sacrificed (n = 4) from each group at each time point at various time intervals from infection (6 h, 1, and 2 days), and bacterial counts were taken from the burn areas (as a measure of local proliferation) and from the spleen (as a measure of systemic dissemination [bacteremia]). Samples from each animal’s burn area and spleen were taken aseptically, weighed, homogenized and resuspended in a sterile saline solution. Bacterial counts of P. aeruginosa per gram of tissue (eschar or spleen) were determined by serial dilutions of the sample and by colony counting on the BHI agar plates after an overnight To study the efficacy of anti-fla-a against P. aeruginosa infection and elucidate their local and systemic effects in vivo, we used our established infected burn wound sepsis model [23] using the clinical strain of P. aeruginosa, PA409, confirmed as a type-a flagellin serotype (Fig. 1). In this model, neither burn or infection alone were sufficient to elicit mortality. However, in the infected burn groups, mortality increased by elevating bacterial inoculum injected subeschar. Infected burn, with inoculum of 3 105, 6 105, 1 106 and 5 106 CFU per burn, resulted within 14 days in 83%, 92%, 100% and 100% mortality, respectively. Most cases of fatality occurred within the first four days. An inocula of 3 105 CFU per burn corresponding to 5 times lethal dose fifty (LD50) of the bacterium, was chosen for the in vivo studies. Anti-fla-a (at a 2.7. Morbidity and mortality follow-up Please cite this article in press as: Barnea Y, et al. Therapy with anti-flagellin A monoclonal antibody limits Pseudomonas aeruginosa invasiveness in a mouse burn wound sepsis model. Burns (2008), doi:10.1016/j.burns.2008.08.014 JBUR-2892; No of Pages 7 4 burns xxx (2008) xxx–xxx Fig. 1 – Anti-fla-a recognition of Pseudomonas strains by live ELISA and immunoblot analysis. Panel A: laboratory (PA01, PAK) and clinical Pseudomonas isolates (strain #’s 201, 35225, 409, 183, 184, 185 and 188) were bound to coated ELISA plates (see Section 2) and probed with antifla-a. Colorimetric analysis indicated the specificity of this monoclonal antibody solely towards Pseudomonas strains harboring type-a flagellin. Panel B: Anti-fla-a binding towards P. aeruginosa flagellin protein by immunoblot analysis. AntI-fla-a bound only full-length flagellin type a (lane 3) but not flagellin type b (lane 4). N’-terminal P. aeruginosa flagellin types a (lane 1) or b (lane 2) were essentially devoid of reactivity towards anti-fla-a, as was Exotoxin (lane 5). total amount of 0.25 mg) decreased mortality of PA409infected burn-mice from 94% (34/36), to 4% (1/24) [p < 0.0001], when monoclonal antibodies were administrated in a combined regimen, prior and post-bacterial infection. Control mice that received either of the control IgG fractions exhibited essentially complete mortality (96% mortality (23/ 24), p = 0.8 for the NS-Ab group; 100% (12/12) for the polyclonal IgG group). The results achieved with anti-fla-a treatment were equivalent to treatment with Imipenem (4% mortality), as shown in Fig. 2A. Daily weight changes over time post-bacterial challenge is shown in Fig. 2B. Groups treated with anti-fla-a and Imipenem Fig. 2 – In vivo efficacy of anti-fla-a against Pseudomonas aeruginosa PA409 infection in infected burn sepsis model during passive immunization. Mice were infected with 3 T 105 PA409 CFU per burn, followed by different treatment modalities. Panel A: survival in the non-treated and non-specific antibodies-treated groups (6% and 4%, respectively) was significantly lower than that of the antifla-a-treated group (96%). Survival in the Imipenemtreated group (96%) was equivalent to that of the anti-fla-a treated group. Anti-flagellin-b-treated control group displayed no survival. Error bars (standard deviation) were determined from an average of two or three independent experiments. Panel B: daily weight changes over time revealed a rapid weight loss, maximal on day 2, followed by a steady weight gain, reaching constant weight at 2 weeks post-infection. Groups treated with anti-fla-a and Imipenem demonstrated on day 2 post-infection less weight loss than the untreated and non-specific monoclonal antibodies-treated groups. The latter 2 groups continued to loose weight until 100% mortality. revealed a rapid weight loss in the first 2 days, followed by a steady weight gain in the surviving mice reaching constant weight at 2 weeks after infection. Non-treated infected burn and NS-Ab-treated groups displayed a rapid weight loss in surviving mice until 100% mortality in both groups (Fig. 2B). Encouraged by these in vivo findings whereby anti-fla-a was given as a combined regimen, we further studied its efficacy when administered in two additional modes: prophylaxis (given only before infection) and treatment (given only after infection). Fig. 3A shows that anti-fla-a administered in all three regimens Please cite this article in press as: Barnea Y, et al. Therapy with anti-flagellin A monoclonal antibody limits Pseudomonas aeruginosa invasiveness in a mouse burn wound sepsis model. Burns (2008), doi:10.1016/j.burns.2008.08.014 JBUR-2892; No of Pages 7 burns xxx (2008) xxx–xxx Fig. 3 – The effect of treatment by different antibody regimens on the survival of mice infected with PA409 (3 T 105 CFU/burn). Panel A: non-treated and non-specific antibodies-treated groups displayed low survival rates (6% and 4%, respectively). Anti-fla-a treatment in all three regimens (pre-infection, post-infection and combined) enhanced survival rate to 75%, 50%, and 96% (respectively). Imipenem-treated groups showed 96% survival rates. Panel B: relative daily weight changes over time revealed a rapid weight loss, maximal on day 2, followed by a steady weight gain, reaching constant weight at 2 weeks postinfection in the treated groups. Weight change in the preinfection group is very similar to the Imipenem-treated group and both are superior to the post-infection and combined treated groups. All the treated groups were advantageous compared to the weight change in the untreated group. reduced mortality rates compared to the untreated infected burn mice group. Mortality rates of the combined, prophylaxis (pre-infection) and treatment (post-infection) regimens were 4% ( p < 0.0001), 25% ( p < 0.0.0001), and 50% ( p = 0.001), respectively, compared to 94% mortality in the non-treated infected burn groups. Morbidity in the different anti-fla-a regimens, as expressed by daily weight changes, paralleled survival results. Maximal weight loss occurred on day 2 post-infection, with a subsequently gradual weight gain (Fig. 3B). 3.3. Anti-fla-a antibodies limit P. aeruginosa invasiveness The proliferation and dissemination of P. aeruginosa in our infected burn model were assessed by bacterial counts taken from the burn eschar (local proliferation) and from the spleen 5 Fig. 4 – Bacterial counts in mice infected with PA409 in theinfected burn-wound sepsis model and the effect of antifla-a on bacterial dissemination. Bacterial counts assessed (n = 3 from each group at each time point) in the burn area and in the spleen during two days after subeschar infection of PA409 (3 T 105 CFU per mouse). Bacterial proliferation was maximal 24 h after infection induction both in the infected burn group and the anti-fla-a-treated group. Anti-fla-a-treated group had significantly lower bacterial counts in the spleen compared to the non-treated infected burn group ( p = 0.001). (systemic dissemination) during the first 48 h (Fig. 4). In the non-treated infected burn and in the anti-fla-a treated groups, bacterial proliferation in the burn eschar was maximal 24 h after infection, with an ensuing mild decline after 48 h. No statistical difference in bacterial counts was found between the two groups. Spleen samples removed during the first 48 h after the induction of P. aeruginosa infection demonstrated that spleens from the anti-fla-a-treated group showed significantly lower bacterial counts after 48 h compared to spleens from non-treated infected burn group ( p = 0.001), as seen in Fig. 4. 4. Discussion This study demonstrates the profound in vivo efficacy of an anti-flagellin type-a at doses of 0.05–0.25 mg against a clinical P. aeruginosa isolate in a lethal burn wound infection model in mice. This monoclonal antibody provided significant protection in mice challenged with up to five times lethal doses of a clinical isolate of P. aeruginosa with equivalent levels of protection observed with Imipenem, the conventional antibiotic used to treat Pseudomonas infections in the hospital setting. The protective effect observed with anti-fla-a was a specific effect since pre-immune or a polyclonal IgG fraction raised against N0 -terminal type-b flagellin were both totally devoid in preventing P. aeruginosa-induced mortality. To assess the in vivo efficacy of anti-fla-a we chose a murine burn wound sepsis model previously adapted by us in which mortality is driven via the dual presence of a burn injury with P. aeruginosa infection, in which mortality was found to be directly proportional to the infecting inoculum [23,24]. Murine Please cite this article in press as: Barnea Y, et al. Therapy with anti-flagellin A monoclonal antibody limits Pseudomonas aeruginosa invasiveness in a mouse burn wound sepsis model. Burns (2008), doi:10.1016/j.burns.2008.08.014 JBUR-2892; No of Pages 7 6 burns xxx (2008) xxx–xxx body weight loss observed in this model was attributed to the sepsis state after burn wound infection, with a vicious cycle of decreased appetite (lower food and water intake) and dehydration. No parenteral fluid was administered after burn wound infection. Passive immunization with anti-fla-a given in a combined regimen (before and after infection induction) resulted in a dramatic reduction in mortality rates, in marked contrast with the control IgG antibody groups (Fig. 2A). The data described herein confirms the seminal study by Rosok et al. [19], whereby FA6IIG5 monoclonal antibodies afforded prophylactic protection at doses of 10–50 mg when given as a treatment paradigm. The potency and efficacy of the anti-fla-a mAb initially reported by Rosok [19] and confirmed in this present study, presumably highlights the optimal methodological approach adapted by Rosok [19] in generating the mAb. In that study, immunization was performed with P. aeruginosa-derived flagellin type a protein. Thereafter, the critical hybridoma screen utilized intact P. aeruginosa bacterium on ELISA as opposed to employment of a coated, purified antigen. Using this optimal screening approach, (as adapted by us in Fig. 1A to discriminate between type a and b flagellin), anti-fla-a mAb was identified as a lead mAb. Administration with anti-fla-a reduced morbidity as well (Fig. 2B). Mice body weight loss in the anti-fla-a-treated groups was significantly lower than in the control groups (Fig. 2B). Body weight changes within the 2-week follow-up paralleled the survival results and were similar to the Imipenem-treated group, as seen in Fig. 2B. Non-specific immunoglobulins have been used previously against P. aeruginosa infection, given both locally and systemically, with various treatment effectiveness results [25,26]. In this current study, treatment with a pre-immune IgG still resulted in similar mortality and morbidity rates as the nontreated groups, with no apparent anti-bacterial effect. In contrast, anti-fla-a significantly lowered mortality and morbidity rates, whereas treatment with a high-titer polyclonal antiflagellin type-b IgG, previously shown to be highly neutralizing against PA01 bacteria [22], failed to affect mortality rates using PA409. These data indicate that the absolute neutralizing specificity of the anti-fla-a is solely toward P. aeruginosa bacteria harboring the type-a flagellin protein. As a caveat to our previous studies which demonstrated a remarkable in vivo efficacy of a polyclonal anti-N0 -terminal flagellin type-b IgG towards its homologous P. aeruginosa bacteria [22], it is highly plausible that a similar epitopetargeted type-a flagellin IgG might neutralize lethality associated with strain PA409. This is likely to be due to prevention of binding of a critical hexapeptide stretch (amino acids 88–97), which is critical for binding to the Toll-5 receptor. Interestingly, the anti-fla-a epitope however, appears to be directed downstream from amino acid 156 according to the immunoblot analysis (Fig. 1B), indicating the presence of a second, proinflammatory motif within the C0 -terminal of P. aeruginosa flagellin in agreement with previously published findings [15,17]. Consequently, these findings lay credence that neutralizing antibodies could be developed by targeting both the N0 - and C0 -terminal domains and thereby providing a highly effective, bifurcating passive immunization approach to disable and neutralize P. aeruginosa bacteria. The use of anti-flagellin antibodies for the treatment of P. aeruginosa infections has been described previously [19,20,25]. In this study, we tested the efficacy of passive immunization with anti-fla-a at three different regimens: before infection induction (prophylaxis regimen), after infection (treatment regimen), and combined regimen (before and after infection induction). All regimens displayed significantly enhanced survival compared to control antibody groups but at different potencies (Fig. 2A). The combined regimen afforded the highest survival rate (96%), followed by the prophylactic (75% survival) and treatment (50% survival) regimens. anti-flaa given only before infection induction (prophylactic regimen) significantly lowered mortality and morbidity rates (Fig. 3A and B), suggesting a protective effect of anti-fla-a against P. aeruginosa infection. This observation is of particular importance in an era of increasing drug resistance, when strains of P. aeruginosa become prevalent in many hospitals in general, and particularly in burn units. With the use of conventional antimicrobial agents, resistant bacterial strains are likely to develop both to systemic and topical agents [5,9,10]. Nonetheless, inhibition of P. aeruginosa by anti-fla-a allows a selective antibacterial effect, without promoting the emergence of resistant strains. In an attempt to understand the mechanism in which antiflagella antibodies protect mice in the burn wound sepsis model, bacterial counts sampled from the burn area up to 48 h after infection induction were carried out. Similar bacterial proliferation in the non-treated and the anti-fla-a-treated groups was observed in the burn area (Fig. 4). In marked contrast, bacterial counts assayed from the spleen showed significant lower bacterial proliferation in the anti-fla-a treated groups, compared to the non-treated groups (Fig. 4). These results support the mechanism of action of anti-fla-a, which selectively inhibits the flagellar action of the bacteria and therefore reduces its ability to systemically disseminate via the blood stream. Our results would indicate that the effect of anti-fla-a is in attenuating bacterial motility at the burn site without affecting its ability to divide thereby ultimately resulting in failure of the bacteria to disseminate systemically. This mechanism supports the important role of the flagella in the progression of a local bacterial colonization into an invasive disease [25]. The protective effect of anti-fla-a given as a prophylactic regimen (pre-infection only) can be attributed to the selective blockage of the P. aeruginosa flagella, thereby interfering in its binding to the Toll-5 receptor. This monoclonal antibody-target recognition can be executed in the marginal area of the burn or in the blood stream. Treatment with anti-fla-a before infection induction allows recruitment of antibodies in the infected area, lowering the virulence of P. aeruginosa and reducing mortality rates. Anti-fla-a given prophylactically to high-risk populations such as burn patients may have an important potential in preventing P. aeruginosa infections. Moreover, even after infection has established, these antibodies may be used as effective therapy, decreasing the morbidity and mortality rates. Indeed, such a mechanism might involve mAb-mediated neutralization of shedded. pro-inflammatory P. aeruginosa flagellin present in the systemic circulation. In the era of increasing antibiotic resistance, a monoclonal antibody therapy approach might provide a novel therapeutic Please cite this article in press as: Barnea Y, et al. Therapy with anti-flagellin A monoclonal antibody limits Pseudomonas aeruginosa invasiveness in a mouse burn wound sepsis model. Burns (2008), doi:10.1016/j.burns.2008.08.014 JBUR-2892; No of Pages 7 burns xxx (2008) xxx–xxx paradigm. In the case of P. aeruginosa infections, the data described herein further supports the notion that such an approach to target a P. aeruginosa noxious molecule, namely flagellin, might represent a promising modality for prevention and treatment of infected burns. Acknowledgement The study has been financially supported in part by XTL Biopharmaceuticals, Rehovot, Israel. Authors Yoav Barnea, Yehuda Carmeli, and Shiri NavonVenezia do not have commercial association that might pose a conflict of interest in this study. Authors Lewis F. Neville, Hamutal Kahel-Reifer, Rachel Eren, and Shlomo Dagan were employees of XTL Biopharmaceuticals, Rehovot, Israel, at the time of the study. references [1] Nguyen TT, Gilpin DA, Meyer NA, Herndon DN. Current treatment of severely burned patients. Ann Surg 1996;223:14–25. [2] Herndon DN, Tompkins RG. Support of the metabolic response to burn injury. Lancet 2004;363:1895–902. [3] Mooney DP, Gamelli RL. Sepsis following thermal injury. Compr Ther 1989;15:22–9. [4] Waymack JP. Antibiotics and the postburn hypermetabolic response. J Trauma 1990;30:S30–3. [5] Edward-Jones V, Greenwood JE, On behalf of the Manchester Burns Research Group 2003. What’s new in burn microbiology? James Laing Memorial Prize Essay. Burns 2000;29:15–24. [6] Komolafe OO, James J, Kalongolera L, Makoka M. Bacteriology of burns at the Queen Elizabeth Central Hospital, Blantyre, Malawi. Burns 2003;29: 235–8. [7] Stieritz DD, Holder IA. Experimental studies of the pathogenesis of infections due to Pseudomonas aeruginosa: description of a burned mouse model. J Infect Dis 1975;131:688–91. [8] Estahbanati HK, Hashani PP, Ghanaatpisheh F. Frequency of Pseudomonas aeruginosa serotypes in burn wound infections and their resistance to antibiotics. Burns 2002;28:340–8. [9] Pirnay JP, De Vos D, Cochez C, Bilocq F, Pirson J, Struelens M, et al. Molecular epidemiology of Pseudomonas aeruginosa colonization in a burn unit: persistence of a multi-drugresistance clone and a silver sulfadiazine-resistant clone. J Clin Microbiol 2003;41:1192–202. [10] Singh NP, Goyal R, Manchanda V, Das S, Kaur I, Talwar V. Changing trends in bacteriology of burns in the burns unit, Delhi, India. Burns 2003;29:129–32. [11] Cryz Jr SJ, Furer E, Germanier R. Protection against Pseudomonas aeruginosa infection in a murine burn wound sepsis model by passive transfer of antitoxin A, antielastase, and antilipopolysaccharide. Infect Immun 1983;39:1067–71. [12] Sawada S, Kawamura T, Masuho Y. Immunoprotective human monoclonal antibodies against five major serotypes of Pseudomonas aeruginosa. J Gen Microbiol 1987;133:3581–90. [13] Drake D, Montie TC. Protection against Pseudomonas aeruginosa infection by passive transfer of anti-flagellar serum. Can J Microbiol 1987;33:755–63. [14] Holder IA, Naglich MS. Experimental studies of the pathogenesis of infections due to Pseudomonas aeruginosa: immunization using divalent flagella preparation. J Trauma 1986;26:118–22. [15] Smith KD, Andersen-Nissen E, Hayashi F, Strobe K, Bergman MA, Barrett SL, et al. Toll-like receptor 5 recognizes a conserved site on flagellin required for protofilament formation and bacterial motility. Nat Immunol 2003;4:1247–53. [16] Hayashi F, Smith KD, Ozinsky A, Hawn TR, Yi EC, Goodlett DR, et al. The innate immune response to bacterial flagellin is mediated by Toll-receptor 5. Nature 2001;410:1099–103. [17] Murthy KG, Deb A, Goonesekera S, Szabó C, Salzman AL. Identification of conserved domains in Salmonella muenchen flagellin that are essential for its ability to activate TLR5 and to induce an inflammatory response in vitro. J Biol Chem 2004;279:5667–75. [18] Samatey FA, Imada K, Nagashima S, Vonderviszt F, Kumasaka T, Yamamoto M, et al. Structure of the bacterial flagellar protofilament and implications for a switch for supercoiling. Nature 2001;410:331–7. [19] Rosok MJ, Stebbins MR, Connelly K, Lostrom ME, Siadak AW. Generation and characterization of murine antiflagellum monoclonal antibodies that are protective against lethal challenge with Pseudomonas aeruginosa. Infect Immun 1990;58:3819–28. [20] Ochi H, Ohtsuka H, Yokota S, Uezumi I, Terashima M, Irie K, et al. Inhibitory activity on bacterial motility and in vivo protective activity of human monoclonal antibodies against flagella of Pseudomonas aeruginosa. Infect Immun 1991;59:550–4. [21] Montie TC, Doyle-Huntzinger D, Craven RC, Holder IA. Loss of virulence associated with absence of flagellum in an isogenic mutant of Pseudomonas aeruginosa in the burnedmouse model. Infect Immun 1982;38:1296–8. [22] Neville LF, Barnea Y, Hammer-Munz O, Gur E, Kuzmenko B, Kahel-Raifer H, et al. Antibodies raised against N0 -terminal Pseudomonas aeruginosa flagellin prevent mortality in lethal murine models of infection. Int J Mol Med 2005;16:165–71. [23] Barnea Y, Carmeli Y, Kuzmenko B, Gur E, Hammer-Munz O, Navon-Venezia S. The establishment of a Pseudomonas aeruginosa-infected burn wound sepsis model and the effect of IPM treatment. Ann Plast Surg 2006;56:674–9. [24] Barnea Y, Carmeli Y, Gur E, Kuzmenko B, Gat A, Neville LF, et al. Efficacy of antibodies against the N-terminal of Pseudomonas aeruginosa flagellin for treating infections in a murine burn wound model. Plast Reconstr Surg 2006;117(7):2284–91. [25] Felts AG, Giridhar G, Grainger DW, Slunt JB. Efficacy of locally delivered polyclonal immunoglobulin against Pseudomonas aeruginosa infection in a murine burn wound model. Burns 1999;25:415–23. [26] Van Asten FJ, Hendriks HG, Koninkx JF, Van der Zeijst BA, Gaastra W. Inactivation of the flagellin gene of Salmonella enterica serotype enteriditis strongly reduces invasion into differentiated Caco-2 cells. FEMS Microbiol Lett 2000;185:175–9. Please cite this article in press as: Barnea Y, et al. Therapy with anti-flagellin A monoclonal antibody limits Pseudomonas aeruginosa invasiveness in a mouse burn wound sepsis model. Burns (2008), doi:10.1016/j.burns.2008.08.014 7