* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The role of carbohydrate in diabetes management
Survey
Document related concepts
Food choice wikipedia , lookup
Chromium(III) picolinate wikipedia , lookup
Calorie restriction wikipedia , lookup
Abdominal obesity wikipedia , lookup
Human nutrition wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Diet-induced obesity model wikipedia , lookup
Low-carbohydrate diet wikipedia , lookup
Thrifty gene hypothesis wikipedia , lookup
Transcript
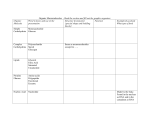
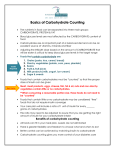
Review The role of carbohydrate in diabetes management Paul D McArdle BSc (Hons), MA, RD, MBDA, Birmingham Community Healthcare NHS Foundation Trust, UK Duane Mellor PhD, RD, APD, Faculty of Health, University of Canberra, Australia Sian Rilstone BSc, MSc, RD, Imperial College Healthcare NHS Trust, London, UK Julie Taplin BSc, RD, North East London NHS Foundation Trust, UK Correspondence to: Paul D McArdle, St Patrick’s Centre for Community Heath, Frank Street, Birmingham B12 0YA, UK; email: [email protected] Received: 2 May 2016 Accepted in revised form: 11 July 2016 Abstract The role of carbohydrate in the diet of people living with diabetes is an area of much debate. This relates to both type and quantity of carbohydrate consumed, with low carbohydrate diets increasing in popularity. However, it is important to take a whole diet approach and not just in terms of single nutrients. This review considers what carbohydrates are and how recommendations for people with diabetes might differ from those for the general population. There are no obligate requirements for dietary carbohydrate. UK recommendations suggest 50% of total energy should come from carbohydrate for the general population; however, evidence does not support an optimal carbohydrate intake for people living with diabetes. Equally, there is no evidence to support a change in other macronutrient intakes including fat; thereby challenging the perspective of low carbohydrate diet advocates, which may encourage higher saturated fat intakes. Carbohydrate quality is important in terms of glycaemic index and fibre, and may have other health benefits; however, the quantity of carbohydrate is a more important predictor of glycaemic response. People with type 1 diabetes can improve the accuracy of insulin dosing with carbohydrate counting and technology may also have a role to play in this, with the introduction of bolus advisor meters. There is no universal recommendation for the amount of carbohydrate for people living with diabetes. Recommendations should therefore be based on personal preference, individual glycaemic response and other health targets, ideally with the support of a registered dietitian specialising in diabetes. Copyright © 2016 John Wiley & Sons. Practical Diabetes 2016; 33(7): 237–242 Key words carbohydrate; diabetes; dietary advice; dietitian Introduction The role of dietary carbohydrate in diabetes is the subject of much debate – especially with respect to ideal amounts and types of carbohydrate.1 This review aims to explore these issues in relation to clinical practice in adults, considered in the context of recommendations given to the general public compared to clinically supervised advice given as part of therapeutic patient education. The individual preferences and interests of the person with diabetes are also a key consideration. What are carbohydrates? There are many definitions of carbohydrate. Table 1 summarises the definition set out by the World Health Organisation,2 which is based on the chemical structure of carbohydrates. Simply put, carbohydrates can be defined as sugars, starches and fibre – often referred to as simple (sugars) and complex (starches and fibre). However, this does not accurately reflect their biological effects: with some starches being more readily broken down to glucose than PRACTICAL DIABETES VOL. 33 NO. 7 some sugars. The measure of how quickly carbohydrate-containing foods result in a rise in blood glucose is known as glycaemic index or ‘GI’.3 Taken out of context, the use of GI has a number of limitations including the serving size and the mixed nature of meals, and it may not consider the overall nutritional quality of the meal. Glycaemic load (GL) reflects more accurately the glycaemic effect and has been described as ‘the product of the GI of a food item and the available carbohydrate content’.4 Thereby, the potential glycaemic effect of a meal may be altered by changing either the GI or the carbohydrate content, consequently affecting the GL. What is sugar? As shown in Table 1, there are many different types of ‘sugar’. For the purpose of health advice, the Scientific Advisory Committee on Nutrition (SACN) and the World Health Organisation2 now use the term ‘free sugar’ to describe the sugars found in honey, syrups, soft drinks, fruit juices, smoothies and purees, as well as sugar added in COPYRIGHT © 2016 JOHN WILEY & SONS 237 Review The role of carbohydrate in diabetes management cooking and food processing.5,6 Free sugars have been associated with an increased risk of weight gain and developing diabetes,7 and is a more precise term than added sugars which has also been used.8 Sources of carbohydrate In the UK, as in many countries, cereal and cereal products make the largest contribution to daily carbohydrate intake, principally from white bread, pasta and rice (Figure 1).9 The greatest contributors to free sugar intake are sugars, preserves and confectionery and non-alcoholic drinks – each group making up about 25% of our free sugar intake.10 Patients and the public may misunderstand the word ‘carbohydrate’ and recent research suggests a ‘sugar-centric’ approach to dietary behaviours in people with diabetes, also indicating a poor understanding of the term ‘carbohydrate’.11 The biggest source of carbohydrate in the diet is in fact not sugar, as described above;9 however, the link between sugar and diabetes is probably due to the association between blood glucose and sugar intake. Although the amount of sugar consumed will influence increases in blood glucose,12 this viewpoint is somewhat simplistic. Dietary requirements for carbohydrate There is no direct physiological requirement for dietary carbohydrate, since the body can make all the glucose required.13 However, basing nutritional recommendations on a single nutrient is unwise, particularly as many of the less processed sources of carbohydrate are low energy density, high in fibre and good sources of vitamins and minerals. This makes them incredibly valuable as part of the diet,14 not only with respect to preventing and managing diabetes, but also to health in general. So, although carbohydrate is not a dietary essential, glucose is required and needs to be synthesised from amino acids or glycerol if not available from the diet. This means it is not possible to consider carbohydrate needs independently of fat and protein as part of the overall diet, and dietary 238 PRACTICAL DIABETES VOL. 33 NO. 7 Class (degree of polymerisation) Subgroup Components Sugars (1–2) Monosaccharides Glucose, galactose, fructose Disaccharides Sucrose, lactose, trehalose Polyols Sorbitol, mannitol Malto-oligosaccharides Maltodextrins Other oligosaccharides Raffinose, stachyose, fructo-oligosaccharides Starch Amylose, amylopectin, modified starches Non-starch polysaccharides (fibre) Cellulose, hemicellulose, pectins, hydrocolloids Oligosaccharides (3–9) Polisaccharides (>9) Table 1. The major dietary carbohydrates. (Adapted from Food and Agriculture Organisation/World Health Organisation, 1998)2 Cereals and cereal products Vegetables and potatoes Fruit Non-alcoholic beverages Sugar, preserves and confectionery Meat and meat products Milk and milk products Other Figure 1. Percentage contribution of food groups to average daily carbohydrate intake (male and female, aged 19–64 years). (Adapted from National Diet & Nutrition Survey data [NDNS, 2014]; Crown copyright © 2014)9 recommendations should be based on foods and eating patterns.15 Current recommendations for carbohydrate The Scientific Advisory Committee on Nutrition6 recently updated the recommendations for the general population and has made subtle changes to guidelines, as outlined in Table 2. It is important to note that these recommendations may not be applicable to people living with diabetes, as recent reviews undertaken suggest that there is a lack of evidence to support an ideal percentage of total energy from carbohydrate.16,17 However, the SACN report does state that there is also no evidence of an association between increasing the percentage of energy consumed from carbohydrate and the risk of developing type 2 diabetes. The SACN recommendations encourage diets that are lower in highly refined sources and higher in minimally refined and whole grain sources of carbohydrate. The recommendations to increase fibre and encourage consumption of whole grains relate to evidence that they may lower risk of developing cardiovascular disease14,18 and some cancers such as colon cancer.19 The Diabetes UK Nutrition Working Group reviewed the evidence for people with diabetes and found there was a lack of evidence for an optimal proportion of energy COPYRIGHT © 2016 JOHN WILEY & SONS Review The role of carbohydrate in diabetes management Nutrient Recommendation Comment Total carbohydrate 50% of total energy No evidence found to change this from previous recommendation Of which free sugars 5% of total energy Re-defined and reduced from 10% (previously ‘non-milk extrinsic sugars’) Fibre 30g per day Re-defined and increased Table 2. Summary of key recommendations of the Scientific Advisory Committee on Nutrition report (SACN, 2015;6 Crown copyright © 2015) Carbohydrate: g per day Carbohydrate: % of energy* Very low carbohydrate 20–50g 6–10% Low carbohydrate <130g <26% Moderate carbohydrate 130–225g 26–45% High carbohydrate >225g >45% *Based on 2000kcal diet. Table 3. Consensus definition of different levels of dietary carbohydrate. (Adapted from Feinman, et al. Nutrition 2015;31(1):1–13)25 from carbohydrate.12 The American Diabetes Association reached the same conclusion,20 and current recommendations for carbohydrate suggest flexibility tailored to the individual, and acknowledge at least the short to medium term benefits of carbohydrate reduction.16 However, there is also agreement on the need to look beyond single dietary components and look at dietary patterns in a more holistic manner.12,20 Quantity of carbohydrate in diabetes Evidence is lacking on the optimal quantity of carbohydrate to consume for glycaemic control in both type 1 and type 2 diabetes. Many individual studies are confounded by differential changes in weight between groups, differences in the total energy intake of participants consuming the different diets (with carbohydrate restriction often inducing a greater relative energy deficit)21 and wide variations in the definitions of ‘low’ and ‘high’ carbohydrate. This makes it difficult to state confidently that the change in carbohydrate intake was responsible for any differences in glycaemic control. Several recent reviews have examined the effect of differing proportions of macronutrients (carbohydrate, protein and fat) on PRACTICAL DIABETES VOL. 33 NO. 7 blood glucose control and weight loss in type 2 diabetes,16,17,22 none of which were able to demonstrate superiority for any proportion of macronutrients in terms of glycaemic control. Franz et al.22 found trials comparing high and low carbohydrate diets resulted in non-significant changes in HbA1c, lipids and blood pressure at 12 months. Dyson16 reports that low carbohydrate diets were no more effective in achieving weight loss in type 2 diabetes, and significantly lower HbA1c values occurred in only three of the eight included studies. The outcomes with regard to blood pressure and lipids also showed no overall superiority in low carbohydrate diets. However, low carbohydrate diets have shown greater potential to reduce medication requirements.23 The debate around low carbohydrate diets warrants continued attention. ‘Low carbohydrate’ can refer to a wide range of carbohydrate intakes, which can lead to confusion. Anything from just less than the recommended intake, e.g. <50% of total energy down to 25g of carbohydrate per day, has been described ‘low carbohydrate’;24 however, a consensus definition is now emerging, as outlined in Table 3.25,26 Van Wyk et al.17 found in many studies the participants were unable to maintain the level of carbohydrate prescribed and the ‘high’ and ‘low’ groups often converged with as little as an 8g difference per day in carbohydrate intake between groups. This may also explain the lack of a definitive conclusion about carbohydrate quantity and is an important observation about the acceptability of particularly high or low carbohydrate diets to patients. The other challenge in considering low carbohydrate diets is the impact that changing the proportion of carbohydrate has on the quantity of other macronutrients, particularly fat. If the carbohydrate in the diet is dramatically reduced, then something is needed to replace it. Fat is typically preferred to protein by proponents of low carbohydrate diets, as protein can be synthesised back to glucose so this may not improve glycaemic control, whereas fat will promote increased ketone synthesis.27 This has been hypothesised to have additional metabolic benefits in type 2 diabetes; however, there is no clear evidence to support the role of ketones in improving glycaemia and cardiovascular risk. There is also no evidence of the benefits of high fat diets including increased intakes of saturated fat in reducing cardiovascular risk.28 Despite this, reviewing the evidence for low saturated fat intakes also reveals an absence of evidence to support saturated fat intakes below 10% of total energy. Emerging evidence suggests that diets based on unsaturated fat such as the Mediterranean diet – which includes around 10% of energy from saturated fat and a total of 40% of total energy from fat (approximately half is from monounsaturated fats) – have been shown to reduce the risk of cardiovascular disease, including in people with type 2 diabetes in Spain.29 Weight loss in those who are overweight remains the most effective strategy to improve glycaemic control in type 2 diabetes.12 Limiting carbohydrate intake often serves to limit energy intake, and thus aid weight management.16 The ultimate fate of all carbohydrate as glucose and its effect on insulin is often used as a rationale for severe carbohydrate restrictions,25 with type 2 COPYRIGHT © 2016 JOHN WILEY & SONS 239 Review The role of carbohydrate in diabetes management diabetes in particular being described by low carbohydrate advocates as a condition of carbohydrate intolerance. Evidence to support this is limited and it is likely that it works primarily by energy restriction,30 which may be achieved through portion control of all energy-dense foods. To summarise: The object of determining the ‘ideal’ carbohydrate intake for each individual must be based on a number of factors, including individual preferences, current and future diabetes treatment, degree of overweight and, where appropriate, individual blood glucose responses. The goal is to equip the person with diabetes with knowledge of the range of dietary approaches available, their relative holistic merits and potential impacts on blood glucose, and a means of assessing the success of each approach. This needs to be delivered in the context of the overall nutritional benefit of the diet, and for reducing cardiovascular risk. Carbohydrate quality in diabetes Fibre and whole grains Evert31 concluded that people with diabetes should consume the same quantity of fibre as the general population (30g per day) but another review found higher intakes (up to about 42.5g per day) improved HbA1c by 6mmol/mol.32 It could be argued this is an unrealistic target given that many people do not achieve the recommended 30g per day, and so to achieve this higher intake would probably require supplementation. Evert et al.20 also reported no association between whole grain intake and glycaemic control; however, whole grains are known to reduce the risk of cardiovascular disease and cancer and so should be promoted to all patients.33 Glycaemic index A Cochrane review suggested the potential benefit of low GI diets is a reduction in HbA1c of approximately 5–6mmol/mol,34 and one recent meta-analysis showed low GI diets resulted in a <2mmol/mol reduction.35 However, the studies are often small in number, the definitions of low GI diets differ and, in 240 PRACTICAL DIABETES VOL. 33 NO. 7 some cases, even the quantities of carbohydrate vary between groups. In the review by Ajala et al.,35 the methods under which the metaanalysis was conducted have also been questioned for their validity.36 The majority of research into the value of low GI diets in diabetes focuses on type 2 diabetes and the Cochrane review34 included just one study involving people with type 1 diabetes. Therefore, low GI diets are not recommended in the management of type 1 diabetes;37 however, many people with type 1 diabetes will need to be aware of the GI and the slower release of glucose from low GI foods, as studies have shown that foods that are low GI as a result of a high fat content can still be releasing glucose into the bloodstream up to 8–12 hours after consumption.38 The relevance of GI in type 1 diabetes is mostly concerned with understanding the use of very high GI foods as effective treatments for hypoglycaemia, and optimising insulin dose adjustment, which will be discussed later. It is clear from the available evidence that the quantity of carbohydrate is of greater importance than the GI with respect to glycaemic control in diabetes,39 but there does appear to be a small additional benefit to reducing the GI of the diet in type 2 diabetes. Carbohydrate counting Carbohydrate is the nutrient that has the greatest effect on postprandial blood glucose and it is widely acknowledged that monitoring of carbohydrate intake and matching mealtime insulin doses is an important strategy in the glycaemic management of type 1 diabetes.12 However, evidence is lacking in type 2 diabetes, since very few studies in this area have been published. In type 2 diabetes, Bergenstal et al.40 found that there was no difference in blood glucose control between a weekly dose adjustment algorithm based on blood glucose, versus matching insulin doses at each meal based on the carbohydrate content. Both approaches yielded similar improvements in glycaemic control. The most widely used insulin regimen for people with type 1 diabetes is a combination of background (long or intermediate acting) insulin and mealtime (quick or short acting) insulin, although this is increasingly also seen in patients with type 2 diabetes. This multiple daily injections (MDI) regimen, sometimes known as ‘basal-bolus’, permits the greatest flexibility by allowing patients to adjust insulin doses based on carbohydrate intake. Insulin pumps use a similar strategy and are increasingly common, especially in children and young people. NICE37 recommends that carbohydrate counting should be offered to adults with type 1 as part of self-management structured education. Those who are unable to attend structured education groups should be provided with the same education on a one-to-one basis. Counting carbohydrates to enable adjustment of mealtime insulin doses has been shown as an effective way of not only improving glycaemic control but also improving quality of life.12,41 This approach is vastly different from the advice given 15 years ago that focused on healthy eating and glycaemic index.42 Carbohydrate counting and insulin adjustment should be taught by someone with specific expertise and competencies, such as a diabetes specialist dietitian. There are many practical tools used in carbohydrate estimation, such as: food models, food plates, carbohydrate reference tables, food weighing scales, food labels, various commercial nutritional analysis books and mobile applications, and the internet. Although the dose of insulin required for each meal will depend on several factors, including physical activity, illness and pre-meal blood glucose results, the accuracy of carbohydrate estimations is paramount in determining the correct insulin dose. Brazeau et al.43 found that underestimation of carbohydrate intake occurred in over 60% of meals when compared with results from computer analysis, resulting in higher and more variable blood glucose results. Accurate carbohydrate counting is important but challenging in everyday life. The other macronutrients (fat and protein) present in food may also influence insulin requirements;44 COPYRIGHT © 2016 JOHN WILEY & SONS Review The role of carbohydrate in diabetes management Practice recommendations Key points • Encourage all people with diabetes to attend a structured patient education programme to improve their understanding of carbohydrate and the range of dietary options available to them • All people with diabetes should have access to a registered dietitian, and those having particular difficulty in achieving glycaemic control should be referred to a diabetes specialist dietitian • In type 2 diabetes: support dietary changes that result in weight loss in the overweight • In type 1 diabetes: support carbohydrate estimation and insulin dose adjustment to allow flexibility and improve quality of life Useful websites and apps • Carbs and Cals: www.carbsandcals.com Best-selling books and award-winning app supporting people with diabetes to track their carbohydrate and calorie intake (plus other nutrients). An excellent pictorial resource • Myfitnesspal: www.myfitnesspal.com A popular personal exercise and food tracker for smartphones (not diabetes specific) • DAFNE online: www.dafneonline.co.uk Free smartphone app available to anyone, containing a carbohydrate portion database and ability to record blood glucose. Website resources restricted to people with type 1 diabetes who have completed the DAFNE course • MySugr: https://mysugr.com Smartphone app allowing users to track and sync information about blood glucose and their wider diabetes management • Diabetes UK: www.diabetes.org.uk A wide array of information on all aspects of diabetes for patients and health care professionals. The free Carbs Count resource is a downloadable book guide to carbohydrate counting and insulin dose adjustment in type 1 diabetes however, this is an area needing further development and outside the scope of this article. People with type 1 diabetes using continuous subcutaneous insulin infusion, also known as insulin pump therapy, are able to extend the duration of insulin bolus infusion to match the delayed glucose release from low GI foods. People on MDI are unable to do this in the same way but may choose to split their bolus dose into two, delaying the second injection in order to extend the duration of active insulin, or may need to give a correction bolus several hours after the meal. New technology Specialist blood glucose meters are now available incorporating bolus advice systems. These devices can help increase accuracy of insulin dose estimation; however, accuracy of carbohydrate estimation remains paramount to ensure accurate bolus advice, as users are required to input this information themselves. Research suggests that PRACTICAL DIABETES VOL. 33 NO. 7 the use of bolus advice meters, along with carbohydrate counting education, has a positive effect on glycaemic control.45 Various mobile phone apps and online resources also exist to help with the estimation of carbohydrate counting, examples of which are provided in the boxed panel above. Carbohydrate awareness This term is used frequently by health professionals, particularly in type 2 diabetes, but there is not currently an agreed definition.46 The general principle is to support patients’ understanding of sources of carbohydrate and the effects of differing the types and quantities of carbohydrate on glycaemic control. This is an area that warrants further research and the development of more clearly defined interventions. Conclusion There is no universal recommendation regarding carbohydrate for people with diabetes. In line with recommendations for the general ● E vidence is lacking with respect to the optimal quantity or proportion of dietary carbohydrate for people with diabetes (type 1, type 2, maturity-onset diabetes of the young [MODY] or gestational diabetes) ● Dietary recommendations should be based on foods and overall eating patterns, not focused on single nutrients ● P eople with diabetes should be offered appropriate and ongoing education and support to determine an individual approach to carbohydrate that helps optimise their blood glucose control, based on their preferences and considering the overall nutritional quality of the diet population, dietary advice should include information on weight management and reducing cardiovascular risk, as well as blood glucose control.47 Advice should be individualised based on an assessment of the person with diabetes, their clinical and personal needs, and ideally undertaken by a registered dietitian specialising in diabetes. Declaration of interests This report is independent research arising from a Clinical Doctoral Research Fellowship, awarded to Paul McArdle (CDRF-2014-05-030), supported by the National Institute for Health Research and Health Education England. The views expressed in this article are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health. Julie Taplin has received speaker honoraria from Roche, Lilly, Boehringer and AstraZenica. There are no other potential conflicts of interest. References 1. Mann J, Morenga LT. Carbohydrates in the treatment and prevention of type 2 diabetes. Diabet Med 2015;32(5):572–5. 2. FAO/WHO. Carbohydrates in human nutrition (FAO Food and Nutrition Paper 66). Rome: World Health Organisation and Food and Agriculture Organisation, 1998. 3. Jenkins DJ, Wolever TM. Slow release carbohydrate and the treatment of diabetes. Proc Nutr Soc 1981;40(2):227–35. 4. Dong JY, et al. Dietary glycaemic index and glycaemic COPYRIGHT © 2016 JOHN WILEY & SONS 241 Review The role of carbohydrate in diabetes management load in relation to the risk of type 2 diabetes: a meta-analysis of prospective cohort studies. Br J Nutr 2011;106(11):1649–54. 5. World Health Organisation. Guideline: Sugars intake for adults and children. Geneva: WHO, 2015. 6.Scientific Advisory Committee on Nutrition. Carbohydrates and Health. London: SACN, 2015. 7. Te Morenga L, et al. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ 2013;346:e7492. 8. Mann J, Morenga LT. Carbohydrates in the treatment and prevention of type 2 diabetes. Diabet Med 2015;32(5):572–5. 9. National Diet & Nutrition Survey: Results from Years 1–4 (combined) of the Rolling Programme (2008/9 to 2011/12). London: Public Health England, 2014. 10. Bates B, et al. National Diet and Nutrition Survey: Results from Years 1, 2, 3 and 4 (combined) of the Rolling Programme (2008/2009 – 2011/2012). London: Public Health England & The Food Standards Agency, 2014. 11.Breen C, et al. A qualitative investigation of patients’ understanding of carbohydrate in the clinical management of type 2 diabetes. J Hum Nutr Diet 2016;29(2):146–55. 12. Dyson PA, et al. Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes. Diabet Med 2011;28(11):1282–8. 13. Westman EC, et al. A review of low-carbohydrate ketogenic diets. Curr Atheroscler Rep 2003;5(6): 476–83. 14. Ye EQ, et al. Greater whole-grain intake is associated with lower risk of type 2 diabetes, cardiovascular disease, and weight gain. J Nutr 2012; 142(7):1304–13. 15. EFSA Panel on Dietetic Products NA. Scientific opinion on dietary reference values for carbohydrates and dietary fibre. Palma: European Food Safety Agency, 2010. 16. Dyson P. Low carbohydrate diets and type 2 diabetes: What is the latest evidence? Diabetes Ther 2015;6(4):411–24. 17. van Wyk HJ, et al. A critical review of low-carbohydrate diets in people with type 2 diabetes. Diabet Med 2016;33(2):148–57. 18. Liu S, et al. Whole-grain consumption and risk of coronary heart disease: results from the Nurses’ Health Study. Am J Clin Nutr 1999;70(3):412–9. 19.Aune D, et al. Dietary carbohydrates, glycemic index, glycemic load and endometrial cancer risk: A systematic review and meta-analysis of prospective studies. Proceedings of the Nutrition Society Conference: Summer Meeting of the Nutrition Society Hosted by the Irish Section 2012;71 [no pagination]. 20. Evert AB, et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 2014;37(Suppl 1):S120–43. 21. Bazzano LA, et al. Effects of low-carbohydrate and low-fat diets: a randomized trial. Ann Intern Med 2014;161(5):309–18. 22. Franz MJ, et al. Lifestyle weight-loss intervention outcomes in overweight and obese adults with type 2 diabetes: a systematic review and metaanalysis of randomized clinical trials. J Acad Nutr Diet 2015;115(9):1447–63. 23. Tay J, et al. Comparison of low- and high-carbohydrate diets for type 2 diabetes management: A randomized trial. Am J Clin Nutr 2015;102(4):780–90. 24.Santos FL, et al. Systematic review and metaanalysis of clinical trials of the effects of low carbohydrate diets on cardiovascular risk factors. Obes Rev 2012;13(11):1048–66. 25. Feinman RD, et al. Dietary carbohydrate restriction as the first approach in diabetes management: Critical review and evidence base. Nutrition 2015;31(1):1–13. 26. Accurso A, et al. Dietary carbohydrate restriction in type 2 diabetes mellitus and metabolic syndrome: time for a critical appraisal. Nutr Metab (Lond) 2008;5:9. 27. Hall KD, et al. Calorie for calorie, dietary fat restriction results in more body fat loss than carbohydrate restriction in people with obesity. Cell Metab 2015;22(3):427–36. 28. Diabetes UK, The British Dietetic Association. Policy statement: Dietary fat consumption in the management of type 2 diabetes. London: 2015. 29. Diez-Espino J, et al. Adherence to the Mediterranean diet in patients with type 2 diabetes mellitus and HbA1c level. Ann Nutr Metab 2011;58(1):74–8. 30. Yudkin J, Carey M. The treatment of obesity by the “highfat” diet. The inevitability of calories. Lancet 1960;2(7157):939–41. 31. Evert AB. Treatment of mild hypoglycemia. Diabetes Spectr 2014;27(1):58–62. 32. Silva FM, et al. Fiber intake and glycemic control in patients with type 2 diabetes mellitus: a systematic review with meta-analysis of randomized controlled trials. Nutr Rev 2013;71(12):790–801. 33. Aune D, et al. Whole grain consumption and risk of cardiovascular disease, cancer, and all cause and cause specific mortality: systematic review and dose-response meta-analysis of prospective studies. BMJ 2016;353:i2716. Get connected 34. Thomas D, Elliott EJ. Low glycaemic index, or low glycaemic load, diets for diabetes mellitus. Cochrane Database Syst Rev 2009;(1):CD006296. 35.Ajala O, et al. A systematic review and metaanalysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr 2013;97:505–16. 36. Mann JI, Te Morenga L. Diet and diabetes revisited, yet again. Am J Clin Nutr 2013;97(3):453–4. 37. NICE. Type 1 diabetes in adults: diagnosis and managment. NICE guidelines [NG17]. London: National Institute for Health and Care Excellence, 2015. 38.Jones SM, et al. Optimal insulin pump dosing and postprandial glycemia following a pizza meal using the continuous glucose monitoring system. Diabetes Technol Ther 2005;7(2):233–40. 39. Franz MJ, et al. Evidence-based diabetes nutrition therapy recommendations are effective: the key is individualization. Diabetes Metab Syndr Obes 2014;7:65–72. 40. Bergenstal RM, et al. Adjust to target in type 2 diabetes: comparison of a simple algorithm with carbohydrate counting for adjustment of mealtime insulin glulisine. Diabetes Care 2008; 31(7):1305–10. 41. DAFNE Study Group. Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating (DAFNE) randomised controlled trial. BMJ 2002;325(7367):746. 42. Goff L, Dyson P. Advanced nutrition and dietetics in diabetes. Chichester: John Wiley & Sons, 2016. 43. Brazeau AS, et al. Carbohydrate counting accuracy and blood glucose variability in adults with type 1 diabetes. Diabetes Res Clin Pract 2013;99(1): 19–23. 44. Bell KJ, et al. Impact of fat, protein, and glycemic index on postprandial glucose control in type 1 diabetes: implications for intensive diabetes management in the continuous glucose monitoring era. Diabetes Care 2015;38(6):1008–15. 45. Rabbone I, et al. Carbohydrate counting with an automated bolus calculator helps to improve glycaemic control in children with type 1 diabetes using multiple daily injection therapy: an 18-month observational study. Diabetes Res Clin Pract 2014; 103(3):388–94. 46. McArdle P. CADDi: Carbohydrate advice by dietitians in diabetes [unpublished MA thesis]. Nottingham: University of Nottingham, 2013. 47. NICE. Clinical Guideline NG28. Type 2 diabetes in adults: management. London: National Institute for Health and Care Excellence, 2015. Stay one step ahead by signing up for Practical Diabetes e-alerts. Please include me on your electronic mail updates What is your job? Diabetologist Name ______________________________________________________ Specialist registrar GP with an interest in diabetes Email ______________________________________________________ Place of work ________________________________________________ Do you have a formal diabetes clinic in your practice? YES (to be answered by GPs and Practice Nurses only (please tick box)) NO Estimate the proportion (%) of your workload represented by diabetes _____% 242 PRACTICAL DIABETES VOL. 33 NO. 7 Diabetes specialist nurse Practice nurse Podiatrist Dietitian Other (please specify) ______________________________ Signed ___________________________________ Date ___________ By submitting your email address here you consent to receive any relevant email content alerts from Practical Diabetes. Your email will not be shared with any third party. Please note you can opt out by replying to any email with the words ‘unsubscribe’. Return to: Practical Diabetes, FREEPOST, NAT 21640, Chichester, PO19 8BR, UK. Fax: +44 (0) 1243 770144 COPYRIGHT © 2016 JOHN WILEY & SONS