* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Diseases and Conditions Table: Recommendations for
Schistosomiasis wikipedia , lookup
Ebola virus disease wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Rocky Mountain spotted fever wikipedia , lookup
West Nile fever wikipedia , lookup
Oesophagostomum wikipedia , lookup
Herpes simplex wikipedia , lookup
Orthohantavirus wikipedia , lookup
Hepatitis B wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Henipavirus wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Leptospirosis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Marburg virus disease wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Infection Prevention and Control (IPC)
Resource Manual
for
Continuing Care
February 2014
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Acknowledgements
The Infection Prevention and Control Resource Manual was developed by a committee of Alberta
Health Services Infection Prevention and Control Professionals.
Co-Chairs
Pamela Armstrong
Christine Knaus
Core Committee Members
Karen Cargill
Yvette Gable
Nicole Henderson
Karen Hope
Brenda Jenkins
Maureen Kano
Heather MacLaurin
Lori Pohl
Linda Siminoski
Betty Soanes
Joy Scott
Jan Stoesz
Ad Hoc Members
Karen Hope, IPC Director
Sue Lafferty, IPC Director
Standards and Projects
Sara Gallinger
Isabelle Ho
1
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Introduction
Quick Links
Glossary
RPAP
Additional Precautions for ARO
Positive Residents in Continuing
Care
Airborne and Contact Precautions
Airborne Precautions
Contact Precautions
Droplet and Contact Precautions
Droplet Precautions
Routine Practices
Additional Precaution Signs
Airborne
Airborne and Contact
Droplet
Droplet and Contact
Contact
Fact Sheets
Choosing Personal Protective
Equipment for Resident Interactions
in Continuing Care (RP)
General Instructions for Putting on
an N95 Respirator (Mask)
Proper Glove Use as part of
Personal Protective Equipment
Additional Resources
AHS Donning and Doffing PPE
posters
AHS Guidelines for Outbreak
Prevention, Control and
Management in Acute Care and
Facility Living Sites
AHS Guidelines for Outbreak
Prevention, Control and
Management in Supportive Living
and Home Living Sites.
Alberta Health Notifiable Disease
List
Alberta Health, Public Health Act –
Bodies of Deceased Persons
Regulation
Bedbug Management Protocols for
Health Care Workers
Dermatome Chart
This manual is intended to support staff in caring for residents living in
Alberta Health Services (AHS) owned and contracted Continuing Care
settings who have a known or suspected infectious disease or condition.
It is organized in alphabetical order based on either the common or
scientific spelling of the disease, condition or microorganism.
The most up-to-date version of the Manual is the electronic version on the
website. Printed copies of the document should be considered current only
on the date printed.
Instructions
1. To view a disease, condition or microorganism:
• If you know what you are looking for; click on its first letter in the
list below to move to an alphabetical index of diseases and
conditions for that letter. Click on the organism or disease you are
looking for to view its table.
ABCDEFGHIJKLMNOPQRSTUVWXYZ
•
If you are unsure what you are looking for; review the Index of
Diseases and Conditions on the next pages. Click the disease or
condition you would like to see. You will be brought directly to its
table.
2. If a disease, condition or microorganism you are looking for is not
listed; follow Routine Practices and contact Infection Control or your
Zone Medical Officer of Health or designate as needed for additional
information.
3. To access interactive features:
• In the specific disease or condition, click the hyperlink that you
would like to view. This will open the linked document.
• Routine Practices and Additional Precautions (RPAP) information
sheets are linked to this document and appear in the tables as
follows: Routine Practices; Airborne Precautions; Airborne and
Contact Precautions; Droplet and Contact Precautions;
Droplet Precautions; Contact Precautions
• Other links in this document are underlined
• Additional Precautions (AP) information sheets are linked to their
Precautions sign, Routine Practices (RP) information sheet and
other information. Links in the RPAP information sheets are
underlined. Click on the underlined words to access the link.
• RPAP information sheets, signs and additional resources may also
be accessed by the links in the left hand column.
Please contact Infection Prevention and Control (IPC) or your Zone
Medical Officer of Health (MOH) or designate with any questions.
2
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Index of Diseases and Conditions
A
Abscess – (Staphylococcus aureus, Streptococcus
[Group A], many other bacteria) See Draining Wounds
Acinetobacter – (Multi-drug Resistant) (MDRA)
Acquired Immunodeficiency Syndrome (AIDS)
Actinomycosis (Actinomyces sp.)
Adenovirus – Conjunctivitis
C
Calicivirus (Norwalk-like, Norovirus) See Norovirus
Campylobacter jejuni
Candidiasis (Candida sp.)
Carbapenem-Resistant Enterobacteriaceae (CRE)
See Enterobacteriaceae (Multi-Drug Resistant;
Carbapenem resistant [CRE]; ESBL or Amp-C
producing)
Cat-scratch Fever (Bartonella henselae)
Adenovirus – Gastroenteritis
Cellulitis – (Staphylococcus aureus, Streptococcus
[Group A], many other bacteria)
Adenovirus – Respiratory tract infection
Chancroid (Hemophilus ducreyi)
Aeromonas spp.
Amebiasis – diarrhea (Entamoeba histolytica)
Chickenpox – Exposed Susceptible Contact (Varicella
zoster virus)
Anthrax – confirmed, probable or suspect case
Chickenpox – Known Case (Varicella zoster virus)
Antibiotic Resistant Organisms (ARO)
Chikungunya virus (alphavirus CHIKV)
Arthropod borne virus (Arboviruses)
Chlamydia (Chlamydia trachomatis)
Ascariasis – Roundworm (Ascaris lumbricoides)
Cholera (Vibrio cholerae)
Aspergillosis (Aspergillus spp.)
Citrobacter spp. (Multi-Drug Resistant; Carbapenem
resistant [CRE]; ESBL or Amp-C producing) See
Enterobacteriaceae (Multi-Drug Resistant;
Carbapenem resistant [CRE]; ESBL or Amp-C
producing)
Astrovirus – diarrhea
Avian Influenza See Influenza -Avian
B
Bedbugs (Cimex lectularius)
Blastomycosis – Pneumonia (Blastomyces
dermatitidis)
Clostridium difficile Infection (CDI)
Clostridium perfringens – Food poisoning
Clostridium perfringens – Gas gangrene
Coccidioidomycosis (Coccidioides immitis)
Blastomycosis – Skin lesions (Blastomyces
dermatitidis)
Colorado tick fever (Arbovirus)
Botulism (Clostridium botulinum)
Conjunctivitis – Pink Eye; Viral
Bronchiolitis
Coronavirus – (Severe Acute Respiratory Syndrome,
SARS CoV)
Brucellosis – Skin lesions (Brucella sp.)
Brucellosis – Undulant fever, Malta fever,
Mediterranean fever (Brucella sp.)
Burkholderia cepacia – Non-respiratory infections
Burkholderia cepacia – Respiratory infection
Burns (infected) – (Staphylococcus aureus,
Streptococcus [Group A], many other bacteria) See
Draining Wounds
3
Conjunctivitis – Pink Eye; Bacterial
Coronavirus – not SARS
Cough, fever, acute upper respiratory tract infection
(Rhinovirus, Respiratory syncytial virus [RSV],
Parainfluenza virus, Influenza, Adenovirus,
Coronavirus, Bordetella pertussis, Mycoplasma
pneumoniae)
Cough, fever, pulmonary infiltrates in person at risk for
tuberculosis (Mycobacterium tuberculosis)
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Coxsackievirus Disease (Enterovirus and
Picornavirdae)
Creutzfeldt-Jakob Disease – classic (CJD) and variant
(vCJD)
Crimean-Congo Hemorrhagic Fever (Arbovirus) See
Hemorrhagic Viral Fevers
Croup (Hemophilus influenzae, Mycoplasma
pneumoniae, adenoviruses, RSV, influenza virus,
parafluenza virus, measles virus , human
metapneumovirus)
Cryptococcosis (Cryptococcus neoformans)
Cryptosporidiosis (Cryptosporidium parvum)
Cyclosporiasis (Cyclospora cayetanensis)
Cytomegalovirus
D
Decubitus ulcer, infected – (Staphylococcus aureus,
Streptococcus [Group A], many other bacteria) See
Draining Wounds
Dengue Fever (Arbovirus)
Dermatitis – (Many bacteria, viruses, fungi) See
Draining Wounds
Diarrhea – (Many bacteria, viruses, parasites)
Diphtheria: skin or pharyngeal (Corynebacterium
diphtheriae)
Draining Wounds
E
Eastern Equine Encephalitis (alpha virus)
Ebola See Hemorrhagic Viral Fevers
Echinococcosis/Hydatidosis (Echinococcus
granulosis, Echinococcus multilocularis)
Encephalitis – (Herpes Simplex Virus [HSV types 1
and 2], Enterovirus, Arbovirus)
Endometritis – (Streptococcus [Group A])
Enterobacter spp. (Multi-Drug Resistant; Carbapenem
resistant [CRE]; ESBL or Amp-C producing) See
Enterobacteriaceae (Multi-Drug Resistant;
Carbapenem resistant [CRE]; ESBL or Amp-C
producing)
4
Enterobacteriaceae (Multi-Drug Resistant;
Carbapenem resistant [CRE]; ESBL or Amp-C
producing)
Enterobiasis (pinworm) (Oxyuriasis, Enterobius
vermicularis)
Enteroviral Infections
Epiglottitis – (Haemophilus influenza type B [HIB],
Streptococcus [Group A], Staphylococcus aureus)
Epstein-Barr virus (Human Herpes Virus 4)
Erysipelas – (Streptococcus [Group A]) See
Streptococcus [Group A] – Skin Infection
ESBL (Extended Spectrum Beta Lactamase
producers)
Escheria coli (Multi-Drug Resistant; Carbapenem
resistant [CRE]; ESBL or Amp-C producing) See
Enterobacteriaceae (Multi-Drug Resistant;
Carbapenem resistant [CRE]; ESBL or Amp-C
producing)
Escherichia coli 0157: H7
F
Febrile respiratory illness, acute respiratory tract
infection – (Rhinovirus, Respiratory syncytial virus,
[RSV], Parainfluenza virus, Influenza, Adenovirus,
Coronavirus, Bordetella pertussis, Mycoplasma
pneumoniae)
Fever unknown origin, fever without focus (acute) –
(Many bacteria, viruses, fungi)
Fifth Disease – Parvovirus B-19 See Parvovirus B-19
Food poisoning – (Bacillus cereus, Clostridium
perfringens, Staphylococcus aureus, Salmonella sp.,
Vibro paraheaemolyticus, Escherichia coli 0157: H7)
G
Gas Gangrene (Clostridium sp.) See Clostridium
perfringens – Gas gangrene
GAS – Group A Streptococcus (Streptococcus
pyogenes) Scarlet fever, pharyngitis See
Streptococcus [Group A] (Streptococcus pyogenes) –
Scarlet Fever, Pharyngitis
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
GAS – Group A Streptococcus (Streptococcus
pyogenes)-skin infections See Streptococcus [Group
A] – Skin Infection
GAS – Group A Streptococcus (Streptococcus
pyogenes) invasive disease, toxic shock See
Streptococcus [Group A] (Streptococcus pyogenes) –
Invasive
Gastroenteritis – (Several bacteria, viruses, parasites)
German measles (Rubella virus) – Acquired See
Rubella: German measles – Acquired
German measles (Rubella virus) – Exposed
Susceptible Contact See Rubella virus (German
measles) - Exposed Susceptible Contact
Giardiais (Giardia lamblia)
Gingivostomatitis – (Herpes simplex virus)
Gonococcus (Neisseria gonorrhoeae) See Neisseria
gonorrhoeae
Guillain-Barre Syndrome
H
Haemophilus influenzae type b (HIB) – invasive
disease
Hafnia spp. (Multi-Drug Resistant; Carbapenem
resistant [CRE]; ESBL or Amp-C producing) See
Enterobacteriaceae (Multi-Drug Resistant;
Carbapenem resistant [CRE]; ESBL or Amp-C
producing)
Herpes simplex – Recurrent
Herpes zoster: Shingles (Varicella zoster virus) –
Disseminated See Shingles: (Herpes zoster) Varicella
zoster virus – Disseminated
Herpes zoster: Shingles (Varicella zoster virus) –
Exposed Susceptible Contact See Shingles: (Herpes
zoster) Varicella zoster virus – Exposed Susceptible
Contact
Herpes zoster: Shingles (Varicella zoster virus) –
Immunocompromised Host WITH Localized Lesions (1
or 2 dermatomes) See Shingles: (Herpes zoster)
Varicella zoster virus – Immunocompromised Host
WITH Localized lesions (1 or 2 dermatomes)
Herpes zoster: Shingles (Varicella zoster virus) –
Normal Host With Localized Lesions(1 or 2
dermatomes) AND lesions that CAN be covered with
dressings or clothing See Shingles: (Herpes zoster)
Varicella zoster virus – Normal Host, Localized (1 or 2
dermatomes) AND lesions that CAN be covered with
dressings or clothing
Herpes zoster: Shingles (Varicella zoster virus) –
Normal Host With Localized Lesions (1 or 2
dermatomes) AND lesions that CANNOT be covered
with dressings or clothing See Shingles: (Herpes
zoster) Varicella zoster virus – Normal Host, Localized
(1 or 2 dermatomes) AND lesions that CANNOT be
covered with dressings or clothing
Histoplasmosis (Histoplasma capsulatum)
Hook worm (Necator americanus, Ancyclostoma
duodenale)
Hand, foot and mouth disease – (Enterovirus)
Human Immunodeficiency Virus (HIV)
Hantavirus
Human Metapneumovirus
Helicobacter pylori
Hemolytic uremic syndrome (HUS) – May be
associated with Escherichia coli 0157: H7
Hemorrhagic viral fever acquired in identified endemic
geographic location – (Ebola virus, Lassa virus,
Marburg virus, Crimean-congo and others)
Hepatitis – A, E
Hepatitis – B, C, D, and other unspecified non-A, nonB
I
Impetigo – (Staphylococcus aureus, Streptococcus
[Group A], many other bacteria) See Draining Wounds
Influenza – New Pandemic Strain, Novel Influenza
Viruses
Influenza – Seasonal
Herpangina (vesicular pharyngitis) – (Enterovirus)
J
Herpes simplex – Mucocutaneous Disseminated or
primary and extensive
No organisms at this time
5
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
K
Klebsiella spp. (Multi-Drug Resistant; Carbapenem
resistant {CRE}; ESBL or Amp-C producing) See
Enterobacteriaceae (Multi-Drug Resistant;
Carbapenem resistant [CRE]; ESBL or Amp-C
producing)
Mononucleosis (Epstein-Barr virus) See Epstein –
Barr virus (Human Herpes Virus 4)
Morganella spp. (Multi-Drug Resistant; Carbapenem
resistant [CRE]; ESBL or Amp-C producing) See
Enterobacteriaceae (Multi-Drug Resistant;
Carbapenem resistant [CRE]; ESBL or Amp-C
producing)
L
Mucormycosis (phycomycosis, zygomycosis) – (Mucor
sp., Zygomycetes sp., Rhizopus sp.)
Lassa fever (Lassa Virus) See Hemorrhagic Viral
Fevers
Multi-Drug Resistant (MDR) Gram Negative Bacilli
Legionella (Legionella spp.)
Leprosy (Hansen’s disease) (Mycobacterium leprae)
Leptospirosis (Leptospira sp.)
Lice (Pediculosis) – (Pediculus humanus, Phthirus
pubis)
Listeriosis (Listeria monocytogenes)
Mumps (Mumps virus) – Known Case
Mumps – (Mumps virus) Exposed Susceptible Contact
Mycobacterium – Non-tuberculosis (atypical) (e.g.,
Mycobacterium avium complex)
Mycobacterium tuberculosis (TB) –extrapulmonary
disease or not respiratory; (also M. africanum,
M.bovis, M. caprae, M. microti, M. pinnipedii)
Lymphocytic choriomeningitis virus
Mycobacterium tuberculosis (TB) –respiratory or
pulmonary disease; (also M. africanum, M.bovis, M.
caprae, M. microti, M. pinnipedii)
Lymphogranuloma venereum (Chlamydia trachomatis)
Mycoplasma pneumoniae
M
N
Malaria (Plasmodium spp.)
Neisseria gonorrhoeae
Marburg virus See Hemorrhagic Viral Fevers
Neisseria meningitidis
Measles – (Rubeola) – Exposed Susceptible Contact
Nocardiosis (Nocardia sp.)
Measles – (Rubeola) – Known Case
Norovirus
Lyme disease (Borrelia burgdorferi)
Melioidosis (Burkholderia pseudomallei)
Meningitis
O
Meningococcus (Neisseria meningitidis) See Neisseria
meningitidis
Orf – parapoxvirus
MERS - Middle Eastern Respiratory Syndrome;
Coronavirus) See Coronavirus – Severe Acute
Respiratory Syndrome (SARS-CoV), Middle Eastern
Respiratory Syndrome (MERS-CoV)
Methicillin Resistant Staphylococcus aureus (MRSA)
Osteomyelitis (Haemophilus influenzae type B (HIB)
[possible in non-immune infant <2 yrs of age],
Staphylococcus aureus, other bacteria)
Otitis, draining (Streptococcus [Group A],
Staphylococcus aureus, Many other bacteria) See
Draining Wounds
Molluscum contagiosum (Molluscum contagiosum
virus)
Monkey Pox
P
Parainfluenza virus
6
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Parvovirus B19 – Fifth’s Disease, Erythema
infectiosum (rash), Aplastic crisis
Rash, petechial or purpuric – (Suspected Neisseria
meningitidis)
Pediculosis (Lice) – (Pediculus humanus, Phthirus
pubis) See Lice (Pediculosis) – (Pediculus humanus,
Phthirus pubis)
Rash, vesicular – (Suspected Varicella virusChickenpox)
Pertussis – Whooping Cough (Bordetella pertussis)
Pharyngitis – (Streptococcus [Group A],
Corynebacterium diphtheriae, many viruses)
Pinworm (Oxyuriasis) – (Enterobius vermicularis) See
Enterobiasis (pinworm) (Oxyuriasis, Enterobius
vermicularis)
Plague – Bubonic (Yersinia pestis)
Plague – Pneumonic (Yersinia pestis)
Pleurodynia (Enterovirus, Coxsackievirus)
Pneumocystis jiroveci Pneumonia (PJP) – formerly
known as P. carinii (PCP)
Pneumonia
Poliomyelitis
Prion Disease – Creutzfeldt-Jakob Disease (CJD);
classic and variant (vCJD) See Creutzfeldt-Jakob
Disease – classic (CJD) and variant (vCJD)
Providencia spp. (Multi-Drug Resistant; Carbapenem
resistant [CRE]; ESBL or Amp-C producing) See
Enterobacteriaceae (Multi-Drug Resistant;
Carbapenem resistant [CRE]; ESBL or Amp-C
producing)
Pseudomembraneous colitis – (Clostridium difficile)
See Clostridium difficile Infection (CDI)
Rat-bite fever – (Streptobacillus moniliformis; Spirillum
minus)
Relapsing fever (Borrelia sp.)
Rhinovirus
Rickettsialpox (Rickettsia akari)
Ringworm (Tinea) – (Trichophyton sp., Microsporum
sp., Epidermophyton sp.)
Ritters Disease – Staphylococcal scalded skin
syndrome (SSSS) See Scalded skin syndrome –
Ritter’s Disease (Staphylococcus aureus)
Rocky Mountain Spotted Fever (Rickettsia rickettsii)
Roseola infantum – Human herpes virus 6
Rotavirus
Roundworm – Ascariasis (Ascaris spp.) See
Ascariasis – Round worm (Ascaris lumbricoides)
RSV – Respiratory syncytial virus
Rubella – Acquired
Rubella – Exposed Susceptible Contact
Rubeola – (Measles) – Known Case See Measles –
(Rubeola) – Known Case
Rubeola – (Measles) Exposed Susceptible Contact
See Measles – (Rubeola) – Exposed Susceptible
Contact
Pseudomonas aeruginosa (Multi-Drug Resistant or
Metallo-Carbapenamase producing**)
Psittacosis (Ornithosis) – (Chlamydia psittaci)
S
Salmonella (Salmonella sp.)
Q
Q Fever (Coxiella burnetii)
R
Rabies
Rash, compatible with scabies – (Ectoparasite)
Rash, maculopapular – (Suspected Rubeola virus
[Measles])
7
Salmonella spp. (Multi-Drug Resistant; Carbapenem
resistant [CRE]; ESBL or Amp-C producing)
SARS – (Severe Acute Respiratory Syndrome;
Coronavirus) See Coronavirus – Severe Acute
Respiratory Syndrome (SARS-CoV), Middle Eastern
Respiratory Syndrome (MERS-CoV)
Scabies (Sarcoptes scabiei)
Scalded skin syndrome – (Staphylococcus aureus)
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Scarlet Fever –Streptococcus pyogenes [Group A]
See Streptococcus, [Group A] (Streptococcus
pyogenes) – Scarlet Fever, Pharyngitis
Schistosomiasis (Schistosoma sp.)
Septic arthritis – (Haemophilus influenza type B [HIB]
[possible in non-immune child <5 years of age],
Streptococcus [Group A], Staphylococcus aureus,
many other bacteria)
Streptococcus [Group A] (Streptococcus pyogenes) Skin Infection
Streptococcus [Group A] (Streptococcus pyogenes) –
Invasive, Toxic shock
Streptococcus pneumoniae
Stronglyoidiasis (Stronglyoides stercoralis)
Syphilis (Treponema pallidum)
Serratia spp. (Multi-Drug Resistant; Carbapenem
resistant [CRE]; ESBL or Amp-C producing) See
Enterobacteriaceae (Multi-Drug Resistant;
Carbapenem resistant [CRE]; ESBL or Amp-C
producing)
T
Shigella (Shigella sp.)
Tetanus (Clostridium tetani)
Shingles: (Herpes zoster) Varicella zoster virus –
Disseminated
Tinea (Ringworm) – (Trichophyton sp., Microsporum
sp., Epidermophyton sp., Malazzezia sp.) See
Ringworm (Tinea) – (Trichophyton sp., Microsporum
sp., Epidermophyton sp., Malassezia furfur)
Shingles: (Herpes zoster) Varicella zoster virus –
Exposed Susceptible Contact
Tapeworm (Taenia saginata, Taenia solium,
Diphyllobothrium latum, Hymenolepsis nana)
Shingles: (Herpes zoster) Varicella zoster virus –
Immunocompromised Host WITH Localized lesions (1
or 2 dermatomes)
Toxic shock syndrome – (Streptococcus pyogenes
[Group A], Staphylococcus aureus)
Shingles: (Herpes zoster) Varicella zoster virus –
Normal Host With Localized Lesions(1 or 2
dermatomes) AND lesions that CAN be covered with
dressings or clothing
Toxoplasmosis (Toxoplasma gondii)
Shingles: (Herpes zoster) Varicella zoster virus –
Normal Host With Localized Lesions (1 or 2
dermatomes) AND lesions that CANNOT be covered
with dressings or clothing
Trench Fever (Bartonella quintana)
Skin Infection – (Staphylococcus aureus,
Streptococcus [Group A], many other bacteria) See
Cellulitis – (Staphylococcus aureus, Streptococcus
[Group A], many other bacteria)
Trichuriasis – Whipworm (Trichuris trichiura)
Smallpox (Variola major virus, Variola minor virus)
Sporotrichosis (Sporothrix schenckii)
Staphylococcus aureus – MRSA See Methicillin
Resistant Staphylococcus aureus (MRSA)
Staphylococcus aureus – pneumonia (not MRSA)
Toxocariasis (Toxocara canis, Toxocara cati)
Trachoma (Chlamydia trachomatis) See Chlamydia
(Chlamydia trachomatis)
Trichinosis (Trichinella spiralis)
Trichomoniasis (Trichomonas vaginalis)
Tuberculosis – non-respiratory or extrapulmonary
(Mycobacterium tuberculosis) See Mycobacterium
tuberculosis (TB) – extrapulmonary disease or not
respiratory
Tuberculosis – respiratory or pulmonary
(Mycobacterium tuberculosis) See Mycobacterium
tuberculosis (TB) –respiratory or pulmonary disease
Tularemia (Francisella tularenis)
Staphylococcus aureus – toxic shock syndrome
Typhoid or Paratyphoid fever (Salmonella typhi,
Salmonella paratyphi) See Salmonella (Salmonella
sp.)
Stenotrophomonas maltophilia
Typhus fever (Rickettsia typhi, Rickettsia prowazekii)
Staphylococcus aureus – skin infection (not MRSA)
Streptococcus [Group A] (Streptococcus pyogenes) –
Scarlet Fever
8
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
U
Western Equine Encephalitis
Urinary tract infection
Whipworm (Trichuris trichiura) See Trichuriasis –
Whipworm (Trichuris trichiura)
V
Whooping cough – Pertussis (Bordetella pertussis)
See Pertussis – Whooping Cough (Bordetella
pertussis)
Vancomycin-intermediate Staphylococcus aureus
(VISA)
Vancomycin-resistant Enterococcus (VRE)
Wound infection – (Staphylococcus aureus,
Streptococcus [Group A], many other bacteria) See
Draining Wounds
Vancomycin-resistant Staphylococcus aureus (VRSA)
Varicella zoster virus: Chickenpox – Exposed
Susceptible Contact See Chickenpox – Exposed
Susceptible Contact (Varicella zoster virus)
X
No organisms at this time
Varicella zoster virus: Chickenpox – Known Case See
Chickenpox – Known Case (Varicella zoster virus)
Varicella zoster virus: Herpes zoster (Shingles) –
Disseminated See Shingles: (Herpes zoster) Varicella
zoster virus – Disseminated
Varicella zoster virus: Herpes zoster (Shingles) –
Exposed Susceptible Contact See Shingles: (Herpes
zoster) Varicella zoster virus – Exposed Susceptible
Contact
Varicella zoster virus: Herpes zoster (Shingles) –
Immunocompromised Host With Localized Lesions (1
or 2 dermatomes) See Shingles: (Herpes zoster)
Varicella zoster virus – Immunocompromised Host
With Localized lesions (1 or 2 dermatomes)
Varicella zoster virus: Herpes zoster (Shingles) –
Normal Host With Localized Lesions (1 or 2
dermatomes) AND lesions that CAN be covered with
dressings or clothing See Shingles: (Herpes zoster)
Varicella zoster virus – Normal Host With Localized
Lesions (1 or 2 dermatomes) AND lesions that CAN
be covered with dressings or clothing
Varicella zoster virus: Herpes zoster (Shingles) –
Normal Host With Localized Lesions(1 or 2
dermatomes) AND lesions that CANNOT be covered
with dressings or clothing See Shingles: (Herpes
zoster) Varicella zoster virus – Normal Host With
Localized Lesions (1 or 2 dermatomes) AND lesions
that CANNOT be covered with dressings or clothing
Vibrio parahaemolyticus Enteritis
W
West Nile (West Nile Virus)
9
Y
Yaws (Treponema pallidum)
Yellow Fever
Yersinia enterocolitica; Yersinia pseudotuberculosis
Z
Zygomycosis (Phycomycosis, Mucormycosis) –
(Mucor sp., Zygomycetes sp., Rhizopus sp.) See
Mucormycosis (phycomycosis, zygomycosis) – (Mucor
sp., Zygomycetes sp., Rhizopus sp.)
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
AA
Abscess – (Staphylococcus aureus, Streptococcus [Group A], many other bacteria) See Draining Wounds
Acinetobacter – (Multi-drug Resistant) (MDRA)
Acquired Immunodeficiency Syndrome (AIDS)
Actinomycosis (Actinomyces sp.)
Adenovirus – Conjunctivitis
Adenovirus – Gastroenteritis
Adenovirus – Respiratory tract infection
Aeromonas spp.
Amebiasis – diarrhea (Entamoeba histolytica)
Anthrax – confirmed, probable or suspect case
Antibiotic Resistant Organisms (ARO)
Arthropod borne virus (Arboviruses)
Ascariasis – Roundworm (Ascaris lumbricoides)
Aspergillosis (Aspergillus spp.)
Astrovirus – diarrhea
Avian Influenza See Influenza - Avian
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
10
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Abscess (Staphylococcus aureus, Streptococcus [Group A], many
other bacteria)
See Draining Wounds
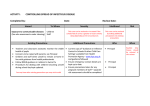
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
11
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Acinetobacter – Multi-drug Resistant (MDRA)
MDRA is an Antibiotic Resistant Organism (ARO)
Clinical Presentation
Colonization or infection of any body site
Infectious Substances
How it is Transmitted
Colonized or infected secretions or excretions
Direct Contact
Indirect Contact
Large Droplets if symptoms of acute respiratory tract
infection
Precautions Needed*
See Additional Precautions for ARO Positive Residents in Continuing Care information sheet
Duration of Precautions
Residents must be reassessed regularly and as conditions and behaviours change
Additional precautions for ARO positive residents in continuing care may be discontinued when resident
is cooperative with hygiene practices and drainage and body fluids are contained.
If needed, consult IPC or Zone Medical Officer of Health (MOH) or designate for assistance determining
when to discontinue additional precautions for ARO positive resident
Incubation Period
Period of Communicability
Variable
While organism is present in secretions/excretions
Comments
*Precautions required are in addition to Routine Practices
•
Acinetobacter is classified as multi-drug resistant if it is resistant to all agents in at least 3
antimicrobial classes usually tested, including cephalosporins and/or carbapenems. Screening
specimens for MDR Acinetobacter include nares, groins, draining wounds and urine. If the resident is
intubated or has a tracheostomy; sputum/endotracheal secretions also need to be screened.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
12
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Acquired Immunodeficiency Syndrome (AIDS)
Clinical Presentation
Asymptomatic; multiple clinical presentations
Infectious Substances
How it is Transmitted
Blood and certain body fluids*
Mucous membrane or percutaneous exposure to
infected blood or body fluids
Sexual transmission
Vertical mother to newborn
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Weeks to years
From onset of infection
Comments
*Fluids include: blood; semen; uterine/vaginal fluid; breast milk; pleural, amniotic, pericardial, peritoneal,
synovial, and cerebral spinal fluids, but exclude other body fluids (feces, nasal secretions, sputum,
saliva, tears, urine or emesis) unless these fluids are visibly blood stained.
•
Refer to your facility’s policy for care of body after death
•
See Public Health Act – Bodies of Deceased Persons Regulation
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
13
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Actinomycosis (Actinomyces sp.)
Clinical Presentation
Cervicofacial, thoracic or abdominal infection
Infectious Substances
How it is Transmitted
Actinomyces bacteria when part of normal flora
in the lining of mouth, throat, digestive system
and vagina
Not person-to-person transmission
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Variable
Not person-to-person transmission
Comments
•
Normal flora; infection is usually secondary to trauma
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
14
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Adenovirus – Conjunctivitis
Clinical Presentation
Conjunctivitis
Infectious Substances
How it is Transmitted
Discharge from eyes
Direct Contact
Indirect Contact
Precautions Needed*
Contact Precautions
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
5 – 12 days
Late in incubation period until 14 days after onset
Comments
*Precautions required are in addition to Routine Practices
•
Careful attention to aseptic technique and reprocessing of ophthalmology equipment is required.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
15
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Adenovirus – Gastroenteritis
Clinical Presentation
Diarrhea
Infectious Substances
How it is Transmitted
Feces
Direct Contact (fecal/oral)
Indirect Contact (fecal/oral)
Precautions Needed*
Adults: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions
Duration of Precautions
Until symptoms have been resolved for at least 48 hours and stools are normal
Incubation Period
Period of Communicability
3 – 10 days
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
•
Symptomatic residents must not participate in food handling activities
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
16
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Adenovirus – Respiratory tract infection
Clinical Presentation
Respiratory tract infection, pneumonia
Infectious Substances
How it is Transmitted
Respiratory secretions
Large Droplets
Direct Contact
Indirect Contact
Precautions Needed*
Droplet and Contact Precautions
Duration of Precautions
Until symptoms have resolved
For immunocompromised hosts (i.e. oncology, transplant residents), isolation precautions need to be
maintained for a longer duration due to prolonged viral shedding. Consult IPC or Zone Medical Officer of
Health (MOH) or designate for assistance determining when to discontinue additional precautions
Incubation Period
Period of Communicability
1 – 10 days
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
•
Different strains responsible for respiratory and gastrointestinal disease
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
17
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Aeromonas spp.
Clinical Presentation
Diarrhea
Infectious Substances
How it is Transmitted
Feces
Direct Contact (Fecal/oral)
Indirect Contact (Fecal/oral)
Precautions Needed*
Adults: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions
Duration of Precautions
Until symptoms have been resolved for at least 48 hours and stools are normal
Incubation Period
Period of Communicability
3 – 10 days
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
•
Symptomatic residents must not participate in food handling activities
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
18
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Amebiasis – Diarrhea (Entamoeba histolytica)
Clinical Presentation
Dysentery, diarrhea
Infectious Substances
How it is Transmitted
Feces
Direct Contact (Fecal/oral)
Indirect Contact (Fecal/oral)
Precautions Needed*
Adults: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions
Duration of Precautions
Until symptoms have been resolved for at least 48 hours and stools are normal
Incubation Period
Period of Communicability
Days to weeks
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
•
Symptomatic residents must not participate in food handling activities
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
19
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Anthrax – Cutaneous, Pulmonary - confirmed, probable or suspect
case - (Bacillus anthracis)
Clinical Presentation
Skin lesions or pneumonia
Infectious Substances
How it is Transmitted
Anthrax spores of B. anthracis in soil and in
infected animals, including livestock and wild
life
Not person-to-person transmission for inhalational
forms of anthrax; acquired from contact with infected
animals and animal products.
Lesion drainage (very rare)
Very rarely reported for cutaneous anthrax where it
requires direct contact with skin lesions.
Precautions Needed*
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
1 – 7 days
Not person-to-person transmission for inhalational
anthrax. Very rarely reported for cutaneous anthrax.
Comments
*Consider Contact Precautions in addition to Routine Practices if drainage from skin lesions cannot
be contained until drainage has resolved or can be contained
•
May be Bioterrorism related
•
Notify Zone Medical Officer of Health of case by fastest means possible.
•
Refer to your facility’s existing policy re: care of body after death
•
See Public Health Act – Bodies of Deceased Persons Regulation
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
20
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Antibiotic Resistant Organisms (AROs)
Examples include: Methicillin Resistant Staphylococcus aureus (MRSA), Vancomycin
Resistant Enterococci (VRE), Vancomycin Resistant Staphylococcus aureus (VRSA),
Extended Spectrum Beta-lactamase (ESBL), Carbapenem-resistant Enterobacteriaceae
(CRE), Multi Drug resistant Acinetobacter (MDRA)
Clinical Presentation
Colonization or infection of any body site
Infectious Substances
How it is Transmitted
Colonized or infected secretions or excretions
Direct Contact
Indirect Contact
Large Droplets if symptoms of acute respiratory tract
infection
Precautions Needed*
See Additional Precautions for ARO Positive Residents in Continuing Care information sheet
Duration of Precautions
Residents must be reassessed regularly and as conditions and behaviours change
Additional precautions for ARO positive residents in continuing care may be discontinued when resident
is cooperative with hygiene practices and drainage and body fluids are contained.
If needed, consult IPC or Zone Medical Officer of Health (MOH) or designate for assistance determining
when to discontinue additional precautions for ARO positive resident
Incubation Period
Period of Communicability
Variable
While organism is present in secretions or excretions
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
21
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Arthropod borne virus (Arboviruses)
Clinical Presentation
Encephalitis, fever, rash, arthralgia, meningitis
Infectious Substances
How it is Transmitted
Infected tick/mosquito
Vector-borne: spread by ticks, mosquitos
Blood, tissues**
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Variable 3 – 21 days
**Not person-to-person transmission except rarely by
blood transfusion or organ transplantation. For West
Nile virus extremely rarely by breast milk or
transplacentally (CDC)
Comments
•
•
•
•
•
Several hundred different viruses exist. Most are limited to specific geographic areas.
Most common North American diseases caused by Arboviruses:
Colorado tick fever (reovirus)
West Nile encephalitis (flavivirus)
Other North American diseases caused by Arboviruses:
o California encephalitis (bunyavirus)
o St. Louis encephalitis (flavivirus)
o Western equine encephalitis (alphavirus)
o Eastern equine encephalitis (alphavirus)
o Powassan encephalitis (flavivirus)
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
22
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Ascariasis – Roundworm (Ascaris lumbricoides)
Clinical Presentation
Usually asymptomatic, gastric upsets
Infectious Substances
How it is Transmitted
Soil containing infective ascarid eggs
Not person-to-person transmission
Acquired from ingestion of infective eggs/larvae
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Life cycle requires 4 – 8 weeks for completion
Not person-to-person transmission.
Comments
•
•
Transmission occurs by ingestion of infective eggs from contaminated soil.
Ova must hatch in soil to become infectious.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
23
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Aspergillosis (Aspergillus spp.)
Clinical Presentation
Infection of skin, lung, wound or central nervous system
Infectious Substances
How it is Transmitted
Ubiquitous in nature, particularly in decaying
material and in soil, air, water and food
Not person-to-person transmission.
Acquired from inhalation of airborne spores
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Variable
Not person-to-person transmission
Comments
•
Spores may be present in dust; infections in immunocompromised residents have been associated
with exposure to construction dust.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
24
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Astrovirus – diarrhea
Clinical Presentation
Diarrhea
Infectious Substances
How it is Transmitted
Feces
Direct Contact (fecal/oral)
Indirect Contact (fecal/oral)
Precautions Needed*
Adults: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions
Duration of Precautions
Until symptoms have been resolved for at least 48 hours and stools are normal
Incubation Period
Period of Communicability
3 – 4 days
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
•
Symptomatic residents must not participate in food handling activities
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
25
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Avian Influenza
See Influenza – Avian
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
26
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
B
Bedbugs (Cimex lectularius)
Blastomycosis – Pneumonia (Blastomyces dermatitidis)
Blastomycosis – Skin lesions (Blastomyces dermatitidis)
Botulism (Clostridium botulinum)
Bronchiolitis
Brucellosis – Skin lesions (Brucella sp.)
Brucellosis – Undulant fever, Malta fever, Mediterranean fever (Brucella sp.)
Burkholderia cepacia – Non-respiratory infections
Burkholderia cepacia – Respiratory infection
Burns - Infected (Staphylococcus aureus, Streptococcus [Group A], many other bacteria) See Draining Wounds
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
27
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Bedbugs (Cimex lectularius)
Clinical Presentation
Allergic reactions and itchy welts. Bites are usually in rows.
Infectious Substances
How it is Transmitted
Not applicable
Not applicable
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Not applicable
Not applicable
Comments
•
Bedbugs are not known to transmit disease. Consult professional pest control for infestation or
consult Alberta Health Services, Environmental Public Health
http://www.albertahealthservices.ca/eph.asp
•
See Alberta Health Services, Environmental Health and Infection Prevention and Control, Bedbug
Management Protocols for Health Care Workers
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
28
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Blastomycosis – Pneumonia (Blastomyces dermatitidis)
Clinical Presentation
Pneumonia
Infectious Substances
How it is Transmitted
Spores in soil
Not person-to-person transmission.
Acquired from inhalation of spore-laden dust
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
30 – 45 days
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
29
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Blastomycosis – Skin lesions (Blastomyces dermatitidis)
Clinical Presentation
Skin lesions
Infectious Substances
How it is Transmitted
Spores in soil
Not person-to-person transmission
Hematogenous dissemination following primary lung
infection
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
30 – 45 days
Not person-to-person transmission
Comments
•
Acquired from spores in soil
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
30
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Botulism (Clostridium botulinum)
Clinical Presentation
Flaccid paralysis, cranial nerve palsies
Infectious Substances
How it is Transmitted
Toxin producing spores in soil, agricultural
products, honey, and animal intestine
Not person-to-person transmission.
Acquired from ingestion of spores/toxin in
contaminated food or wounds contaminated by
spores in soil
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Variable
Not person-to-person transmission
Comments
•
May be bioterrorism related
•
Notify Zone Medical Officer of Health of case by fastest means possible
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
31
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Bronchiolitis
(Various causative agents: respiratory syncytial virus (RSV), parainfluenza virus,
adenovirus, influenza virus, human metapneumovirus)
Clinical Presentation
Respiratory infection
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Indirect Contact
Large Droplets
Precautions Needed
Droplet and Contact Precautions
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
Variable
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
•
May cohort individuals infected with the same virus. If possible, residents should not share room with
high-risk immunocompromised roommates
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
32
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Brucellosis – Skin lesions (Brucella sp.)
Clinical Presentation
Skin lesions
Infectious Substances
How it is Transmitted
Drainage from open lesions
Person-to-person transmission is extremely rare –
possible direct contact.
Precautions Needed*
Major drainage not contained: Contact Precautions
Minor drainage contained: Routine Practices
Duration of Precautions
Until drainage has resolved or can be contained
Incubation Period
Period of Communicability
Weeks to months
Person-to-person transmission is extremely rare
Comments
*Precautions required are in addition to Routine Practices
•
Acquired from direct contact through breaks in skin tissues with infected animals or ingestion of
unpasteurized dairy products from infected animals.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
33
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Brucellosis – Undulant fever, Malta fever, Mediterranean fever
(Brucella sp.)
Clinical Presentation
Systemic bacterial disease of acute or insidious onset
Infectious Substances
How it is Transmitted
Infected animals and contaminated food from
infected animals
Not person-to-person transmission except rarely via
banked spermatozoa and sexual contact
Acquired contact with infected animals or from
contaminated food, mostly dairy products.
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Weeks to months
Rarely person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
34
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Burkholderia cepacia – Non-respiratory infections
Clinical Presentation
Based on site of infection
Infectious Substances
How it is Transmitted
Potentially skin and body fluids
Direct Contact
Indirect Contact
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Variable
Variable
Comments
•
Do not room with resident with cystic fibrosis (CF) who is not infected or colonized with Burkholderia
cepacia
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
35
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Burkholderia cepacia – Respiratory infection
Clinical Presentation
Exacerbation of chronic lung disease in residents with cystic fibrosis
Infectious Substances
How it is Transmitted
Respiratory Secretions
Direct Contact
Indirect Contact
Large Droplets
Precautions Needed*
Droplet and Contact Precautions
Duration of Precautions
Consult IPC or Zone Medical Officer of Health (MOH) or designate for assistance determining when to
discontinue additional precautions
Incubation Period
Period of Communicability
Variable
Variable
Comments
*Precautions required are in addition to Routine Practices
•
Do not room with resident with cystic fibrosis (CF) who is not infected or colonized with Burkholderia
cepacia
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
36
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Burns - Infected (Staphylococcus aureus, Streptococcus [Group
A], many other bacteria)
See Draining Wounds
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
37
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
C
Calicivirus (Norwalk-like, Norovirus) See Norovirus
Campylobacter jejuni
Candidiasis (Candida spp.)
Carbapenem-Resistant Enterobacteriaceae (CRE) See Enterobacteriaceae (Multi-Drug Resistant; Carbapenem
resistant [CRE]; ESBL or Amp-C producing)
Cat-scratch Fever (Bartonella henselae)
Cellulitis – (Staphylococcus aureus, Streptococcus [Group A], many other bacteria)
Chancroid (Hemophilus ducreyi)
Chickenpox – Exposed Susceptible Contact (Varicella zoster virus)
Chickenpox – Known Case (Varicella zoster virus)
Chikungunya virus (alphavirus CHIKV)
Chlamydia (Chlamydia trachomatis)
Cholera (Vibrio cholerae)
Citrobacter spp. (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing) See
Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing)
Clostridium difficile Infection (CDI)
Clostridium perfringens – Food poisoning
Clostridium perfringens – Gas gangrene
Coccidioidomycosis (Coccidioides immitis)
Colorado tick fever (Arbovirus)
Conjunctivitis – Pink Eye; Bacterial
Conjunctivitis – Pink Eye; Viral
Coronavirus – Severe Acute Respiratory Syndrome (SARS-CoV); Middle Eastern respiratory syndrome (MERS-CoV)
Coronavirus – not SARS, not MERS
Cough, fever, acute upper respiratory tract infection (Rhinovirus, Respiratory syncytial virus [RSV], Parainfluenza
virus, Influenza, Adenovirus, Coronavirus, Bordetella pertussis, Mycoplasma pneumoniae)
Cough, fever, pulmonary infiltrates in person at risk for tuberculosis (Mycobacterium tuberculosis)
Coxsackievirus Disease (Enterovirus and Picornavirdae)
Creutzfeldt-Jakob Disease – classic (CJD) and variant (vCJD)
Crimean-Congo Hemorrhagic Fever (Arbovirus) See Hemorrhagic Viral Fevers
Croup (Hemophilus influenzae, Mycoplasma pneumoniae, adenoviruses, RSV, influenza virus, parafluenza virus,
measles virus , human metapneumovirus)
Cryptococcosis (Cryptococcus neoformans)
Cryptosporidiosis (Cryptosporidium parvum)
Cyclosporiasis (Cyclospora cayetanensis)
Cytomegalovirus
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
38
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Calicivirus (Norwalk-like, Norovirus)
See Norovirus
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
39
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Campylobacter jejuni
Clinical Presentation
Diarrhea
Infectious Substances
How it is Transmitted
Feces
Direct Contact (fecal/oral)
Contaminated Food
Indirect Contact (fecal/oral)
Precautions Needed*
Adults: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions
Duration of Precautions
Until symptoms have been resolved for at least 48 hours and stools are normal
Incubation Period
Period of Communicability
2 – 5 days
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
•
Symptomatic residents must not participate in food handling activities.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
40
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Candidiasis (Candida spp.)
Clinical Presentation
Mucocutaneous lesions, systemic disease
Infectious Substances
How it is Transmitted
Mucocutaneous secretions and excretions
Contact with infected/colonized secretions or
excretions
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Variable
Not applicable
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
41
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Carbapenem-Resistant Enterobacteriaceae (CRE)
E. coli, Klebsiella spp., Serratia spp., Providencia spp., Proteus spp., Citrobacter spp.,
Enterobacter spp., Morganella spp., Salmonella spp., Hafnia spp.
See Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE];
ESBL or Amp-C producing)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
42
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Cat-scratch Fever (Bartonella henselae)
Clinical Presentation
Fever, lymphadenopathy
Infectious Substances
How it is Transmitted
Infected domestic cats
Not person-to-person transmission
Acquired from scratch, bite, lick or other exposure to
a cat
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
16 – 22 days
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
43
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Cellulitis – (Staphylococcus aureus, Streptococcus [Group A],
many other bacteria)
Clinical Presentation
Purulent inflammation of cellular or subcutaneous tissue
Infectious Substances
How it is Transmitted
Wound drainage
Direct Contact
Indirect Contact
Precautions Needed* **
Major drainage not contained: Contact Precautions
Minor drainage contained: Routine Practices
Duration of Precautions
Until drainage has resolved or can be contained
Incubation Period
Period of Communicability
Not applicable
Not applicable
Comments
*Precautions required are in addition to Routine Practices
**Droplet and Contact Precautions until 24 hours of effective antimicrobial therapy has been received
If invasive group A streptococcal infection suspected
•
Periorbital cellulitis in children <5 years old may be caused by H. influenzae and require Droplet
Precautions
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
44
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Chancroid (Hemophilus ducreyi)
Clinical Presentation
Genital ulcers
Infectious Substances
How it is Transmitted
Drainage
Sexually transmitted
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
3 – 5 days
As long as the infectious agent present in unhealed
lesions.
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
45
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Chickenpox – Exposed Susceptible Contact (Varicella zoster virus)
Clinical Presentation
Susceptible contact. Asymptomatic - may develop chickenpox
Infectious Substances
How it is Transmitted
Respiratory secretions Lesion drainage
Airborne Direct Contact Indirect Contact
Precautions Needed*
8 days after first contact until 21 days after last contact (or 28 days if given varicella zoster
immunoglobulin (VZIG)) with person with active disease during their period of communicability: Airborne
Precautions
If lesions develop: Airborne and Contact Precautions
Duration of Precautions
From 8 days after first contact until 21 days after last contact (or 28 days if given VZIG) with person with
active disease during their period of communicability
If lesions develop: Until all lesions have crusted and dried
Incubation Period
Period of Communicability
10 – 21 days
2 days before rash starts and until all lesions have
crusted and dried
Comments
*Precautions required are in addition to Routine Practices
• Defer non-urgent admission if a non-immune person is incubating the disease
• Individuals with known immunity to chicken pox (history of past illness or vaccination with 2
appropriately timed doses of varicella vaccine) are not required to wear the N95 respirator when
entering the room.
• Susceptible HCWs should not enter the room if immune staff are available. If they must enter the
room, an N95 respirator must be worn. Other non-immune persons should not enter except in urgent
or compassionate circumstances. If immunity is unknown, assume person is non-immune
Discharge Settle Time
Non-negative pressure rooms:
• Do not admit a new resident into this room for at least 4 hours. If staff must enter room before 4
hours has passed and non-immune, wear an N95 respirator.
Negative pressure rooms:
• Do not admit a new resident into this room for at least 45 minutes. If staff must enter room before 45
minutes has passed and non-immune, wear an N95 respirator.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
46
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Chickenpox – Known Case (Varicella zoster virus)
Clinical Presentation
Vesicular rash, Fever
Infectious Substances
How it is Transmitted
Lesion drainage
Airborne
Respiratory secretions
Direct Contact
Indirect Contact
Precautions Needed*
Airborne and Contact Precautions
Duration of Precautions
Until all lesions have crusted and dried
Incubation Period
Period of Communicability
10 – 21 days
2 days before rash starts and until all lesions have
crusted and dried
Comments
*Precautions required are in addition to Routine Practices
• Defer non-urgent admissions if chicken pox or disseminated zoster is present
• Individuals with known immunity (history of past illness or vaccination with 2 appropriately timed
doses of varicella vaccine) are not required to wear the N95 respirator when entering the room.
• Susceptible HCWs should not enter the room if immune staff are available. If they must enter the
room, an N95 respirator must be worn. Other non-immune persons should not enter except in urgent
or compassionate circumstances
• If immunity is unknown, assume person is non-immune
Discharge Settle Time
Non-negative pressure rooms:
• Do not admit a new resident into this room for at least 4 hours. If staff must enter room before 4
hours has passed and non-immune, wear an N95 respirator.
Negative pressure rooms:
• Do not admit a new resident into this room for at least 45 minutes. If staff must enter room before 45
minutes has passed and non-immune, wear an N95 respirator.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
47
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Chikungunya virus (alphavirus CHIKV)
Clinical Presentation
Crippling arthritic manifestations
Infectious Substances
How it is Transmitted
Aedes albopictus mosquitoes
Not person-to-person transmission
Vector borne: Mosquito bite
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Not applicable
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
48
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Chlamydia (Chlamydia trachomatis)
Clinical Presentation
Urethritis, cervicitis, pelvic inflammatory disease; neonatal conjunctivitis, infant pneumonia; trachoma
Infectious Substances
How it is Transmitted
Conjunctival and genital secretions
Sexually transmitted
Mother to newborn at birth
Trachoma: Direct/indirect contact
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Variable
As long as organism present in secretions
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
49
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Cholera (Vibrio cholerae)
Clinical Presentation
Diarrhea
Infectious Substances
How it is Transmitted
Contaminated food or water
Direct Contact (fecal/oral)
Feces
Indirect Contact (fecal/oral)
Ingestion of contaminated food or water
Precautions Needed*
Adults: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
1 – 5 days
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
•
Symptomatic residents must not participate in food handling activities.
•
Notify Zone Medical Officer of Health of case by fastest means possible.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
50
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Citrobacter spp. (Multi-Drug Resistant; Carbapenem resistant
[CRE]; ESBL or Amp-C producing)
E. coli, Klebsiella spp., Serratia spp., Providencia spp., Proteus spp., Citrobacter spp.,
Enterobacter spp., Morganella spp., Salmonella spp., Hafnia spp.
See Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE];
ESBL or Amp-C producing)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
51
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Clostridium difficile Infection (CDI)
Clinical Presentation
Diarrhea, toxic megacolon, pseudomembranous colitis
Infectious Substances
How it is Transmitted
Feces
Direct contact (fecal/oral)
Indirect contact (fecal/oral)
Precautions Needed*
Contact Precautions
Duration of Precautions
Until symptoms have been resolved for at least 48 hours and stools are normal
A negative Clostridium difficile test is not required to discontinue Contact Precautions.
Incubation Period
Period of Communicability
Variable
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
•
Use soap and water for hand washing, alcohol-based hand rubs are not as effective.
•
Bacterial spores persist in the environment. Ensure thorough cleaning of the resident’s environment
particularly toileting equipment, e.g., commodes, toilet grab rails. Careful discharge cleaning is
required.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
52
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Clostridium perfringens – Food poisoning
Clinical Presentation
Gastroenteritis (abdominal pain, severe diarrhea)
Infectious Substances
How it is Transmitted
Feces
Not person-to-person transmission
Soil contaminated food
Foodborne
Precautions Needed
Routine Practices
Duration of Precautions
6 – 24 hours
Incubation Period
Period of Communicability
Not applicable
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
53
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Clostridium perfringens – Gas Gangrene
Clinical Presentation
Crepitus abscesses, myonecrosis
Infectious Substances
How it is Transmitted
Found in normal gut flora, soil
Not person-to-person transmission
Precautions Needed*
Routine Practices
If wound drainage is present and not contained: Contact Precautions
Duration of Precautions
If on Contact Precautions, discontinue when drainage has resolved or can be contained
Incubation Period
Period of Communicability
Variable
Not person-to-person transmission
Comments
*Precautions required are in addition to Routine Practices
•
Infection related to devitalized tissue
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
54
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Coccidioidomycosis (Coccidioides immitis)
Clinical Presentation
Pneumonia, draining lesions
Infectious Substances
How it is Transmitted
Spores from soil and dust in endemic areas
Not person-to-person transmission
Acquired from inhalation of spores
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
1 – 4 weeks
Not person-to-person transmission
Comments
•
Transmission occurs by inhalation of spores in soil and dust
•
Exercise care when changing or discarding dressings, casts or other materials that may be
contaminated with exudate.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
55
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Colorado tick fever (Arbovirus)
Clinical Presentation
Fever
Infectious Substances
How it is Transmitted
Tick
Not person-to-person transmission
Vector borne: Tick
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
3 – 6 days
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
56
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Conjunctivitis – Pink Eye; Bacterial
Clinical Presentation
Swelling, redness and soreness of the whites of the eyes, purulent discharge, itching
Infectious Substances
How it is Transmitted
Eye discharge
Direct Contact
Indirect Contact
Precautions Needed*
Adult: Routine Practices
Children: Contact Precautions
Duration of Precautions
Adults: Not applicable
Children: Until 24 hours of effective antimicrobial therapy has been received
Incubation Period
Period of Communicability
24 – 72 hours
During active infection
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
57
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Conjunctivitis – Pink Eye; Viral
Clinical Presentation
Swelling, redness and soreness of the whites of the eyes, purulent discharge, itching
Infectious Substances
How it is Transmitted
Eye discharge and respiratory secretions
Direct Contact
Indirect Contact
Precautions Needed*
Adults: Contact Precautions
Children: Contact Precautions or, if child is also coughing: Droplet and Contact Precautions
Duration of Precautions
Until symptoms have resolved or a non-viral cause is found
Incubation Period
Period of Communicability
Adenovirus: 5 – 12 days
Up to 14 days
Picornavirus: 12 hours – 3 days
Comments
*Precautions required are in addition to Routine Practices
•
If the cause of the conjunctivitis is adenovirus: See Adenovirus-Conjunctivitis
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
58
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Coronavirus – Severe Acute Respiratory Syndrome (SARS-CoV),
Middle Eastern Respiratory Syndrome (MERS-CoV)
Clinical Presentation
Febrile respiratory illness- new or worsening cough, shortness of breath; Pneumonia; acute respiratory
distress syndrome
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact Indirect Contact
Large Droplets
Aerosols during AGMP
Precautions Needed*
Droplet and Contact Precautions
Wear fit tested N95 respirator when performing Aerosol Generating Medical Procedures (AGMP)
Duration of Precautions
For SARS-CoV: 10 days following resolution of fever if respiratory symptoms have also resolved
For MERS-CoV: Until symptoms have resolved. For residents with prolonged symptoms or for immunocompromised hosts consult IPC or Zone Medical Officer of Health or designate for assistance
determining when to discontinue additional precautions
Incubation Period
Period of Communicability
3 – 10 days
Undetermined
Comments
*Precautions required are in addition to Routine Practices
•
Notify Zone Medical Officer of Health (or designate) of case by fastest means possible.
•
AGMPs include:
o
intubation
o
open tracheal suctioning
o
CPR
o
high frequency oscillatory ventilation
o
bronchoscopy
o
tracheostomy care
o
sputum induction
o
aerosolized medication administration
o
BiPAP
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
59
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Coronavirus – not SARS; not MERS
Clinical Presentation
Common cold
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Indirect Contact
Large Droplets
Precautions Needed*
Droplet and Contact Precautions
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
2 – 4 days
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
60
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Cough, fever, acute upper respiratory tract infection (Rhinovirus,
Respiratory syncytial virus [RSV], Parainfluenza virus, Influenza,
Adenovirus, Coronavirus, Bordetella pertussis, Mycoplasma
pneumoniae)
Clinical Presentation
Acute upper respiratory tract infection
Infectious Substances
How it is Transmitted
Respiratory Secretions
Direct Contact
Indirect Contact
Large Droplets
Precautions Needed*
Droplet and Contact Precautions
Duration of Precautions
Until symptoms have resolved or until infectious cause ruled out
Incubation Period
Period of Communicability
Not applicable
Until symptoms have resolved or until infectious
cause ruled out
Comments
*Precautions required are in addition to Routine Practices
•
May cohort individuals infected with the same virus.
•
Minimize exposure of immunocompromised residents. These residents should not be cohorted.
•
For outbreaks: Refer to the AHS Guidelines for Outbreak Prevention, Control and Management in
Acute Care and Facility Living Sites, OR AHS Guidelines for Outbreak Prevention, Control and
Management in Supportive Living and Home Living Sites
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
61
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Cough, fever, pulmonary infiltrates in person at risk for
tuberculosis (Mycobacterium tuberculosis)
Clinical Presentation
Fever, weight loss, cough, night sweats, abnormal chest x-ray
Infectious Substances
How it is Transmitted
Respiratory Secretions
Airborne
Precautions Needed*
Airborne Precautions
Duration of Precautions
Until tuberculosis ruled out or until resident has received at least two weeks of effective treatment and is
clinically improved and 3 sputum samples taken 24 hours apart are negative for AFB. Until negative
sputum culture if multi-drug resistant tuberculosis.
Incubation Period
Period of Communicability
Not applicable
If tuberculosis ruled out: Until symptoms have
resolved or until infectious cause ruled out
If tuberculosis: While organisms are in sputum
Comments
*Precautions required are in addition to Routine Practices
• Airborne Precautions should be maintained until an expert in tuberculosis management deems the
resident non-infectious.
Discharge Settle Time
Non-negative pressure rooms:
• Do not admit a new resident into this room for at least 4 hours. If staff must enter room before 4
hours has passed and non-immune, wear an N95 respirator.
Negative pressure rooms:
• Do not admit a new resident into this room for at least 45 minutes. If staff must enter room before 45
minutes has passed and non-immune, wear an N95 respirator
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
62
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Coxsackievirus Disease (Enterovirus and Picornavirdae)
Clinical Presentation
Acute febrile illness, aseptic, meningitis, encephalitis, pharyngitis, herpangina, rash, pleurodynia, hand,
foot and mouth disease
Infectious Substances
How it is Transmitted
Feces
Direct Contact including fecal/oral)
Respiratory secretions
Indirect Contact (including fecal/oral)
Large Droplets
Precautions Needed*
Adults: Routine Practices
Children: Contact Precautions
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
3 – 5 days
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
63
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Creutzfeldt-Jakob Disease – classic (CJD) and variant (vCJD)
Clinical Presentation
Chronic encephalopathy (swelling and tissue damage of the cerebrum)
Infectious Substances
How it is Transmitted
Contaminated surgical instruments
Contaminated surgical instruments (classical)
Tissues of infected animals and humans
Tissue grafts from infected donors
High Risk Tissues: Brain including dura mater,
spinal cord, eyes and tonsils
Ingestion of infected central nervous system tissue
Precautions Needed
Routine Practices except special precautions are needed for surgery and autopsy in all suspect and
confirmed cases*
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Months to years
Highest level of infectivity during symptomatic illness
Comments
*Special precautions for surgery and autopsy:
•
•
•
•
Immediately consult IPC or Zone Medical Officer of Health (MOH) or designate if resident
requires surgery or invasive procedure(s).
Special precautions are needed for neurosurgical procedures, autopsy and handling/autopsy of body
after death. Refer to AHS policy and procedure: Prion Disease (CJD) Precautions for the Surgical
Patient at http://insite.albertahealthservices.ca/Files/clp-policy-creutzfeldt-jacob-disease.pdf
Refer to your facility’s policy for care of body after death.
See Public Health Act – Bodies of Deceased Persons Regulation
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
64
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Crimean-Congo Hemorrhagic Fever (Arbovirus)
See Hemorrhagic Viral Fevers
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
65
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Croup (Hemophilus influenzae, Mycoplasma pneumoniae,
adenoviruses, RSV, influenza virus, parainfluenza virus, measles
virus , human metapneumovirus)
Clinical Presentation
Respiratory tract infection
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Indirect Contact
Large Droplets
Precautions Needed*
Droplet and Contact Precautions
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
Variable
Variable
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
66
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Cryptococcosis (Cryptococcus neoformans)
Clinical Presentation
Meningitis, pneumonia, adenopathy
Infectious Substances
How it is Transmitted
Spores in soil
Not person-to-person transmission
Acquired presumably from inhalation of the fungal
spores
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Unknown
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
67
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Cryptosporidiosis (Cryptosporidium parvum)
Clinical Presentation
Diarrhea
Infectious Substances
How it is Transmitted
Fecal oocysts
Direct Contact (fecal/oral)
Indirect Contact (fecal/oral)
Precautions Needed*
Adults: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
1 – 12 days
From onset of symptoms until several weeks after
symptoms are gone
Comments
*Precautions required are in addition to Routine Practices
•
Symptomatic residents must not participate in food handling activities.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
68
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Cyclosporiasis (Cyclospora cayetanensis)
Clinical Presentation
Asymptomatic, vomiting, diarrhea, weight loss, abdominal pain, nausea, fever
Infectious Substances
How it is Transmitted
Contaminated water, fruits and vegetables.
Imported, fresh raspberries, other fruits and
lettuce from Central America
Not person-to-person transmission
Acquired from ingestion of contaminated food or
water
Precautions Needed*
Adult: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions for diapered or incontinent children
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
2 – 14 days
Not person-to-person transmission
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
69
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Cytomegalovirus
Clinical Presentation
Usually asymptomatic; congenital infection, retinitis, disseminated infection in immunocompromised
person
Infectious Substances
How it is Transmitted
Saliva, genital secretions, urine, breast milk,
transplanted organs or stem cells, blood
products
Direct Sexual Contact
Direct Contact
Vertical mother to child in utero, at birth or through
breast milk.
Transfusion, transplantation
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Unknown for person-to-person transmission
Neonates: 5 – 6 years
3 – 12 weeks for blood transfusions,
Adults: Variable, linked to immuno-suppressed status
1 – 4 months for tissue transplants
Comments
•
Requires intimate personal contact for transmission.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
70
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
D
Decubitus ulcer - Infected (Staphylococcus aureus, Streptococcus [Group A], many other bacteria) See Draining
Wounds
Dengue Fever (Arbovirus)
Dermatitis – (Many bacteria, viruses, fungi) See Draining Wounds
Diarrhea** – (Many bacteria, viruses, parasites)
Diphtheria: Skin or Pharyngeal (Corynebacterium diphtheriae)
Draining Wounds (Staphylococcus aureus, Streptococcus [Group A], many other bacteria)
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
71
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Decubitus ulcer - Infected (Staphylococcus aureus, Streptococcus
[Group A], many other bacteria)
See Draining Wounds
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
72
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Dengue Fever (Arbovirus)
Clinical Presentation
Fever, joint pain, rash
Infectious Substances
How it is Transmitted
Infected mosquito
Not person-to-person transmission
Vector borne: Mosquito bite
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
3 – 14 days
Not person-to-person transmission
Comments
Infection in humans is incidental and is acquired most frequently during blood feeding by the infected
mosquito.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
73
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Dermatitis – (Many bacteria, viruses, fungi)
See Draining Wounds
Clinical Presentation
Drainage
Infectious Substances
How it is Transmitted
Drainage
Direct Contact
Indirect Contact
Precautions Needed*
Contact Precautions
Duration of Precautions
Until drainage has resolved or can be contained and infectious cause ruled out
Incubation Period
Period of Communicability
Not applicable
Not applicable
Comments
*Precautions required are in addition to Routine Practices
•
If compatible with scabies take appropriate precautions pending diagnosis
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
74
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Diarrhea** – (Many bacteria, viruses, parasites)
Clinical Presentation
Diarrhea
Infectious Substances
How it is Transmitted
Feces
Direct Contact (Fecal/oral)
Indirect Contact (Fecal/oral)
Precautions Needed*
Refer to specific organism, otherwise:
Adults: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions
Duration of Precautions
If organism identified, see specific organism, otherwise:
Until symptoms have resolved and stools are normal and infectious cause ruled out
Incubation Period
Period of Communicability
Variable
Variable
Comments
*Precautions required are in addition to Routine Practices
**Diarrhea = loose or watery stools above what is normally expected for that resident AND not attributed
to another cause (e.g., medication, laxatives, diet or prior medical condition)
•
Symptomatic residents must not participated in food handling activities.
•
For outbreaks: Refer to the AHS Guidelines for Outbreak Prevention, Control and Management in
Acute Care and Facility Living Sites, OR AHS Guidelines for Outbreak Prevention, Control and
Management in Supportive Living and Home Living Sites.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
75
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Diphtheria: Skin or Pharyngeal (Corynebacterium diphtheriae)
Clinical Presentation
Cutaneous (skin): Characteristic ulcerative lesions
Pharyngeal: Adherent grayish membrane
Infectious Substances
How it is Transmitted
Skin: Lesion drainage
Direct Contact
Pharyngeal: Nasopharyngeal secretions
Indirect Contact
Large Droplets
Precautions Needed*
Droplet and Contact Precautions
Duration of Precautions
Cutaneous: Until two cultures from skin lesions are negative
Pharyngeal: Until both nose and throat cultures are negative
Incubation Period
Period of Communicability
2 – 5 days
If untreated, 2 weeks to several months
Comments
*Precautions required are in addition to Routine Practices
•
Notify Zone Medical Officer of Health of case by fastest means possible.
•
Cultures should be taken at least 24 hours apart and at least 24 hours after the completion of
antimicrobial treatment. If cultures are not available, maintain precautions until 2 weeks after
completion of antimicrobial therapy.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
76
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Draining Wounds (Staphylococcus aureus, Streptococcus [Group
A], many other bacteria)
Clinical Presentation
Draining wounds
Infectious Substances
How it is Transmitted
Wound drainage
Direct Contact
Indirect Contact
Precautions Needed*
Major drainage not contained: Contact Precautions**
Minor drainage contained: Routine Practices
Duration of Precautions
Until drainage has resolved or can be contained
Incubation Period
Period of Communicability
Not applicable
Not applicable
Comments
*Precautions required are in addition to Routine Practices
** Droplet and Contact Precautions until 24 hours of effective antimicrobial therapy has been received
If invasive group A streptococcal infection suspected
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
77
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
E
Eastern Equine Encephalitis (alpha virus)
Ebola See Hemorrhagic Viral Fevers
Echinococcosis/Hydatidosis (Echinococcus granulosis, Echinococcus multilocularis)
Encephalitis – (Herpes Simplex Virus [HSV types 1 and 2], Enterovirus, Arbovirus
Endometritis – (Streptococcus [Group A])
Enterobacter spp. (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing) See
Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing)
Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing)
Enterobiasis (pinworm) (Oxyuriasis, Enterobius vermicularis)
Enteroviral Infections
Epiglottitis – (Haemophilus influenza type B [HIB], Streptococcus [Group A], Staphylococcus aureus)
Epstein-Barr virus (Human Herpes Virus 4)
Erysipelas (Streptococcus [Group A]) See Streptococcus [Group A] - Skin Infection
ESBL (Extended Spectrum Beta Lactamase producers)
Escheria coli (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing) See
Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing)
Escherichia coli 0157: H7
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
78
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Eastern Equine Encephalitis (alpha virus)
Clinical Presentation
Fever, encephalomyelitis (headache, chills, vomiting, disorientation, seizures)
Infectious Substances
How it is Transmitted
Aedes mosquito bite (virus found in birds, bats,
and possibly rodents)
Not person-to-person transmission
Vector borne: Mosquito bite
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
5 – 15 days
Not person-to-person transmission
Comments
•
Notify Zone Medical Officer of Health of case by fastest means possible.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
79
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Ebola
See Hemorrhagic Viral Fevers
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
80
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Echinococcosis/Hydatidosis (Echinococcus granulosis,
Echinococcus multilocularis)
Clinical Presentation
Cyst present in various organs, typically asymptomatic except for noticeable mass. Rupture or leaking
cysts can cause anaphylactic reactions.
Infectious Substances
How it is Transmitted
Worm eggs in feces from dogs. Contaminated
food and water.
Not person-to-person transmission
Acquired by ingestion of eggs passed in the feces of
infected animals
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
12 months to years
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
81
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Encephalitis – (Herpes Simplex Virus [HSV types 1 and 2],
Enterovirus, Arbovirus)
Clinical Presentation
Encephalitis
Infectious Substances
How it is Transmitted
Feces
Direct Contact
Respiratory Secretions
Indirect Contact
Large Droplets
Precautions Needed*
Adult: Routine Practices
Children: Droplet and Contact Precautions
Duration of Precautions
Until specific cause established
Incubation Period
Period of Communicability
Not applicable
Not applicable
Comments
*Precautions required are in addition to Routine Practices
•
May be associated with measles, mumps, varicella, Mycoplasma pneumoniae, Epstein-Barr Virus
(EBV). If so, take appropriate precautions for associated disease.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
82
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Endometritis – (Streptococcus [Group A], many other bacteria)
Clinical Presentation
Abdominal distension or swelling, abnormal vaginal bleeding or discharge, fever, lower abdominal pain
Infectious Substances
How it is Transmitted
Not applicable
Not applicable
Precautions Needed*
Routine Practices**
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Not applicable
Not applicable
Comments
*Precautions required are in addition to Routine Practices
**Droplet and Contact Precautions until 24 hours of effective antimicrobial therapy has been received
If invasive group A streptococcal infection suspected
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
83
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Enterobacter spp. (Multi-Drug Resistant; Carbapenem resistant
[CRE]; ESBL or Amp-C producing)
E. coli, Klebsiella spp., Serratia spp., Providencia spp., Proteus spp., Citrobacter spp.,
Enterobacter spp., Morganella spp., Salmonella spp., Hafnia spp.
See Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE];
ESBL or Amp-C producing)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
84
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant
[CRE]; ESBL or Amp-C producing)
E. coli, Klebsiella spp., Serratia spp., Providencia spp., Proteus spp., Citrobacter spp.,
Enterobacter spp., Morganella spp., Salmonella spp., Hafnia spp.
Clinical Presentation
Colonization or infection of any body site
Infectious Substances
How it is Transmitted
Colonized or infected secretions or excretions
Direct Contact Indirect Contact
Large Droplets if symptoms of acute respiratory tract
infection
Precautions Needed*
See Additional Precautions for ARO Positive Residents in Continuing Care information sheet
Duration of Precautions
Residents must be reassessed regularly and as conditions and behaviours change.
Additional precautions for MDR Enteobacteriaceae positive residents in continuing care may be
discontinued when resident is cooperative with hygiene practices and drainage and body fluids are
contained.
If needed, consult IPC or Zone Medical Officer of Health (MOH) or designate for assistance determining
when to discontinue additional precautions for CRE positive resident
Incubation Period
Period of Communicability
Variable
While organism is present in secretions or excretions
Comments
*Precautions required are in addition to Routine Practices
•
Any of the above listed organisms if they are reported to be resistant to one or more carbapenem
antibiotic (i.e., at least one of ertapenem, imipenem, meropenem, or doripenem)
•
Lab report may identify organism as a CRE
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
85
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Enterobiasis (pinworm) (Oxyuriasis, Enterobius vermicularis)
Clinical Presentation
Perianal itching. Occasionally ulcer-like bowel lesions
Infectious Substances
How it is Transmitted
Ova in stool, perianal region
Direct Contact (fecal/oral)
Contaminated fomites
Indirect Contact (fecal/oral)
Precautions Needed
Routine Practices and careful handling of contaminated linens and undergarments
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
1 – 2 months
Until host colonization no longer occurs
Comments
•
Close contacts may need treatment.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
86
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Enteroviral Infections
(Coxsackievirus A and B, Echovirus, Enterovirus, Poliovirus)
Clinical Presentation
Acute febrile illness, aseptic meningitis, encephalitis, pharyngitis, herpangina, rash, pleurodynia, hand,
foot and mouth disease
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact (including fecal/oral)
Feces
Indirect Contact (including fecal/oral)
Large Droplets
Precautions Needed*
Adults: Routine Practices
Children: Contact Precautions
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
3 – 5 days
Until symptoms have resolved. If poliovirus see
Poliomyelitis
Comments
*Precautions required are in addition to Routine Practices
•
If the respiratory viral panel test has a combined Enterovirus-Rhinovirus positive result; manage as
for Rhinovirus.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
87
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Epiglottitis – (Haemophilus influenza type B [HIB], Streptococcus
[Group A], Staphylococcus aureus)
Clinical Presentation
Sore throat, muffling or change in voice, difficulty speaking or swallowing, fever
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Indirect Contact
Large Droplets
Precautions Needed*
Droplet Precautions
Duration of Precautions
Until 24 hours of effective antimicrobial therapy has been received or until HIB ruled out
Incubation Period
Period of Communicability
Not applicable
Not applicable
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
88
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Epstein-Barr virus (Human Herpes Virus 4)
Clinical Presentation
Infectious mononucleosis; fever, sore throat, lymphadenopathy, splenomegaly
Infectious Substances
How it is Transmitted
Saliva
Direct oropharyngeal route via saliva
Transplanted organs or stem cells
Transplantation
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
30 – 50 days
30 – 50 days
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
89
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Erysipelas – (Streptococcus [Group A])
See Streptococcus [Group A] – Skin Infection
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
90
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
ESBL (Extended Spectrum Beta Lactamase producers)
E. coli, Klebsiella spp., Others
See Specific Organism
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
91
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Escherichia coli (Multi-Drug Resistant; Carbapenem resistant
[CRE]; ESBL or Amp-C producing)
E. coli, Klebsiella spp., Serratia spp., Providencia spp., Proteus spp., Citrobacter spp.,
Enterobacter spp., Morganella spp., Salmonella spp., Hafnia spp.
See Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE];
ESBL or Amp-C producing)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
92
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Escherichia coli 0157: H7
Clinical Presentation
Diarrhea, hemolytic-uremic syndrome (HUS), thrombotic thrombocytopenic purpura
Infectious Substances
How it is Transmitted
Feces
Ingestion of contaminated food
Direct Contact (fecal/oral)
Indirect Contact (fecal/oral)
Precautions Needed*
Adults: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions
Duration of Precautions
Until symptoms have resolved and stools are normal
If HUS: Until two (2) successive stools are negative for E. coli 0157: H7 or 10 days from onset of
diarrhea
Incubation Period
Period of Communicability
10 hours to 8 days
As long as organism present in feces
Comments
*Precautions required are in addition to Routine Practices
•
Symptomatic residents must not participate in food handling activities.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
93
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
F
Febrile respiratory illness, acute respiratory tract infection – (Rhinovirus, Respiratory syncytial virus, [RSV],
Parainfluenza virus, Influenza, Adenovirus, Coronavirus, Bordetella pertussis, Mycoplasma pneumoniae)
Fever unknown origin, fever without focus (acute) – (Many bacteria, viruses, fungi)
Fifth Disease – Parvovirus B-19 See Parvovirus B 19
Food poisoning – (Bacillus cereus, Clostridium perfringens, Staphylococcus aureus, Salmonella spp., Vibro
paraheaemolyticus, Escherichia coli 0157: H7)
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
94
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Febrile respiratory illness, acute respiratory tract infection –
(Rhinovirus, Respiratory syncytial virus, [RSV], Parainfluenza
virus, Influenza, Adenovirus, Coronavirus, Bordetella pertussis,
Mycoplasma pneumoniae)
Clinical Presentation
Respiratory Tract Infection
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Indirect Contact
Large Droplets
Precautions Needed*
Droplet and Contact Precautions
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
Variable
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
•
May cohort individuals infected with the same virus.
•
Minimize exposure of immunocompromised residents. These residents should not be cohorted.
•
For outbreaks: Refer to the AHS Guidelines for Outbreak Prevention, Control and Management in
Acute Care and Facility Living Sites, OR the AHS Guidelines for Outbreak Prevention, Control and
Management in Supportive Living and Home Living Sites
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
95
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Fever unknown origin, fever without focus (acute) – (Many
bacteria, viruses, fungi)
Clinical Presentation
Fever
Infectious Substances
How it is Transmitted
Feces
Direct Contact (including fecal/oral)
Respiratory secretions
Indirect Contact (including fecal/oral)
Precautions Needed*
Adult: Routine Practices
Children: Droplet and Contact Precautions
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
Not applicable
Not applicable
Comments
*Precautions required are in addition to Routine Practices
•
If findings suggest a specific transmissible infection, take precautions for that infection pending
diagnosis.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
96
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Fifth Disease – Parvovirus B-19
See Parvovirus B19
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
97
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Food poisoning – (Bacillus cereus, Clostridium perfringens,
Staphylococcus aureus, Salmonella spp., Vibrio
paraheaemolyticus, Escherichia coli 0157: H7)
Clinical Presentation
Nausea, vomiting, diarrhea, abdominal cramps/pain
Infectious Substances
How it is Transmitted
Contaminated food
Foodborne
Feces
Direct Contact (Fecal/oral)
Indirect Contact (Fecal/oral)
Precautions Needed*
See specific organism, otherwise:
Adult: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions
Duration of Precautions
Until symptoms have resolved and stools are normal
Incubation Period
Period of Communicability
Not applicable
Not applicable
Comments
*Precautions required are in addition to Routine Practices
•
Symptomatic residents must not participate in food handling activities.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
98
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
G
Gas Gangrene (Clostridium spp.) See Clostridium perfringens – Gas gangrene
GAS – Group A Streptococcus (Streptococcus pyogenes) Invasive disease, Toxic shock See Streptococcus [Group
A] (Streptococcus pyogenes) – Invasive
GAS – Group A Streptococcus (Streptococcus pyogenes) Scarlet fever, pharyngitis See Streptococcus [Group A]
(Streptococcus pyogenes) – Scarlet Fever, Pharyngitis
GAS – Group A Streptococcus (Streptococcus pyogenes) - Skin infections See Streptococcus [Group A] - Skin
Infection
Gastroenteritis – (Several bacteria, viruses, parasites)
German measles – Acquired Rubella See Rubella – German measles –Acquired (Rubella virus)
German measles – Exposed Susceptible Contact See Rubella virus: German measles - Exposed Susceptible
Contact
Giardiais (Giardia lamblia)
Gingivostomatitis – (Herpes simplex virus)
Gonococcus (Neisseria gonorrhoeae) See Neisseria gonorrhoeae
Guillain-Barre Syndrome
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
99
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Gas Gangrene - (Clostridium sp.)
See Clostridium perfringens – Gas gangrene
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
100
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
GAS – Group A Streptococcus (Streptococcus pyogenes) Invasive
disease – iGAS, Toxic Shock
See Streptococcus [Group A] (Streptococcus pyogenes) – Invasive
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
101
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
GAS – Group A Streptococcus (Streptococcus pyogenes) Scarlet
fever, pharyngitis
See Streptococcus [Group A] (Streptococcus pyogenes) – Scarlet Fever,
Pharyngitis
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
102
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
GAS – Group A Streptococcus (Streptococcus pyogenes) - Skin,
infections
See Streptococcus [Group A] – Skin Infection
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
103
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Gastroenteritis – (Several bacteria, viruses, parasites)
Clinical Presentation
Diarrhea and/or vomiting
Infectious Substances
How it is Transmitted
Feces
Direct Contact (Fecal/oral)
Indirect Contact (Fecal/oral)
Large Droplets
Precautions Needed*
Refer to specific organism, otherwise
Adult: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
If resident is actively vomiting: Droplet and Contact Precautions
Children: Contact Precautions
Duration of Precautions
If organism identified, see specific organism
Until symptoms have resolved and stools are normal or infectious cause is ruled out
Incubation Period
Period of Communicability
Variable
Until symptoms have resolved and stools are normal
Comments
*Precautions required are in addition to Routine Practices
**Diarrhea = loose or watery stools above what is normally expected for that resident AND not attributed
to another cause (e.g., medication, laxatives, diet or prior medical condition)
•
Symptomatic residents must not participate in food handling activities.
•
For outbreaks: Refer to the AHS Guidelines for Outbreak Prevention, Control and Management in
Acute Care and Facility Living Sites, OR AHS Guidelines for Outbreak Prevention, Control and
Management in Supportive Living and Home Living Sites.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
104
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
German measles (Rubella virus) – Acquired
See Rubella Virus: German measles – Acquired
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
105
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
German measles (Rubella virus) – Exposed Susceptible Contact
See Rubella virus (German measles) - Exposed Susceptible Contact
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
106
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Giardiais (Giardia lamblia)
Clinical Presentation
Diarrhea
Infectious Substances
How it is Transmitted
Feces
Direct contact (fecal/oral)
Indirect contact (fecal/oral)
Precautions Needed*
Adults: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions
Duration of Precautions
Until symptoms have resolved and stools are normal
Incubation Period
Period of Communicability
1 – 4 weeks
As long as organism in feces
May continue for months
Comments
*Precautions required are in addition to Routine Practices
•
Symptomatic residents must not participate in food handling activities.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
107
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Gingivostomatitis – (Herpes simplex virus [HSV], other causes
including radiation therapy, chemotherapy, idiopathic [aphthous])
Clinical Presentation
Fever, redness and swelling of gingivae and oral mucosa, ulcerative lesions.
Infectious Substances
How it is Transmitted
Oral Secretions
Direct Contact
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Variable, 2 days to 2 weeks.
While lesions present.
Comments
*Precautions required are in addition to Routine Practices
•
Consider Contact Precautions* if extensive disease is present. Maintain precautions while
lesions are present.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
108
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Gonococcus (Neisseria gonorrhoeae)
See Neisseria gonorrhoeae
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
109
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Guillain-Barre Syndrome
Clinical Presentation
Acute polyneuropathy disorder affecting the peripheral nervous system. Ascending paralysis, weakness
beginning in the feet and hands and migrating towards the trunk. Associated with many infections.
Infectious Substances
How it is Transmitted
Not applicable
Not applicable
Precautions Needed*
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Not applicable
Not applicable
Comments
•
May follow within weeks of a respiratory or gastrointestinal infection, e.g. Mycoplasma pneumoniae,
Campylobacter jejuni
•
Implement Additional Precautions as needed for known or suspected associated infection.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
110
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
H
Haemophilus influenzae type b (HIB) – invasive disease
Hafnia spp. (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing) See
Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing)
Hand, foot and mouth disease – (Enterovirus)
Hantavirus
Helicobacter pylori
Hemolytic uremic syndrome (HUS) – May be associated with Escherichia coli 0157: H7
Hemorrhagic viral fever acquired in identified endemic geographic location – (Ebola virus, Lassa virus, Marburg virus,
Crimean-Congo and others)
Hepatitis – A, E
Hepatitis – B, C, D, and other unspecified non-A, non-B
Herpangina (vesicular pharyngitis) – (Enterovirus)
Herpes simplex – Mucocutaneous - Disseminated or primary and extensive
Herpes simplex –Mucocutaneous - Recurrent
Herpes zoster: Shingles (Varicella zoster virus) – Disseminated
Herpes zoster: Shingles (Varicella zoster virus) – Exposed Susceptible Contact See Shingles: (Herpes zoster)
Varicella zoster virus – Exposed Susceptible Contact
Herpes zoster: Shingles (Varicella zoster virus) – Immunocompromised Host WITH Localized Lesions (1 or 2
dermatomes) See Shingles: (Herpes zoster) Varicella zoster virus – Immunocompromised Host WITH Localized
lesions (1 or 2 dermatomes)
Herpes zoster: Shingles (Varicella zoster virus) – Normal Host With Localized (1 or 2 dermatomes) AND lesions that
CAN be covered with dressings or clothing See Shingles: (Herpes zoster) Varicella zoster virus – Normal Host,
Localized (1 or 2 dermatomes) AND lesions that CAN be covered with dressings or clothing
Herpes zoster: Shingles (Varicella zoster virus) – Normal Host With Localized Lesions (1 or 2 dermatomes) AND
lesions that CANNOT be covered with dressings or clothing See Shingles: (Herpes zoster) Varicella zoster virus –
Normal Host, Localized (1 or 2 dermatomes) AND lesions that CANNOT be covered with dressings or clothing
Histoplasmosis (Histoplasma capsulatum)
Hook worm (Necator americanus, Ancyclostoma duodenale)
Human Immunodeficiency Virus (HIV)
Human Metapneumovirus
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
111
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Haemophilus influenzae type b (HIB) – invasive disease
Clinical Presentation
Pneumonia, epiglottitis, meningitis, bacteremia, septic arthritis, cellulitis
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Large Droplets
Precautions Needed*
Adult: Routine Practices
Children: Droplet Precautions
Duration of Precautions
Until 24 hours of effective antimicrobial therapy has been received.
Incubation Period
Period of Communicability
Variable
Infectious in the week prior to onset of illness and
during the illness until treated
Comments
*Precautions required are in addition to Routine Practices
•
Close contact less than 48 months old and who are not immune may require chemoprophylaxis.
Household contact of infected children should also receive prophylaxis.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
112
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Hafnia spp. (Multi-Drug Resistant; Carbapenem resistant [CRE];
ESBL or Amp-C producing)
E. coli, Klebsiella spp., Serratia spp., Providencia spp., Proteus spp., Citrobacter spp.,
Enterobacter spp., Morganella spp., Salmonella spp., Hafnia spp.
See Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE];
ESBL or Amp-C producing)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
113
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Hand, foot and mouth disease – (Enterovirus)
Clinical Presentation
Blister-like lesions inside the mouth, sides of tongue, palms of hands, fingers, soles of feet, buttocks.
Encephalitis and meningitis in rare cases.
Infectious Substances
How it is Transmitted
Feces
Direct Contact (including fecal/oral)
Respiratory secretions
Indirect Contact (including fecal/oral)
Large Droplets
Precautions Needed*
Adults: Routine Practices
Children: Contact Precautions
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
4 -6 days
Most contagious during first week of illness. Virus can
remain in the body weeks after symptoms have
resolved.
Comment
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
114
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Hantavirus
Clinical Presentation
Fever, pneumonia
Infectious Substances
How it is Transmitted
Infected rodent excreta
Not person-to-person transmission
Presumed aerosol transmission from rodent excreta
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Days to weeks
Not person-to-person transmission
Comments
•
Notify Zone Medical Officer of Health of case by fastest means possible.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
115
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Helicobacter pylori
Clinical Presentation
Gastritis, duodenal ulcer disease
Infectious Substances
How it is Transmitted
Feces and gastric biopsies
Direct Contact
Probable ingestion of organisms; presumed
fecal/oral/oral/oral
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Possibly 5 – 10 days
Unknown
Comments
•
Humans are likely the major reservoir.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
116
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Hemolytic uremic syndrome (HUS) – May be associated with
Escherichia coli 0157: H7
Clinical Presentation
Not applicable
Infectious Substances
How it is Transmitted
Feces
Direct Contact (fecal/oral)
Indirect Contact (fecal/oral)
Precautions Needed*
Adults: Routine Practices
For incontinent residents if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions
Duration of Precautions
Until Escherichia coli: 0157: H7 ruled out.
For E. coli 0157: H7 disease: Until two (2) successive stools are negative for E. coli O157: H7
Incubation Period
Period of Communicability
Most E. coli strains, 10 hours to 6 days
Until two (2) successive stools are negative for E. coli
O157:H7
E. coli O157:H7, 1-8 days
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
117
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Hemorrhagic viral fevers – Acquired in identified endemic
geographic location – (Ebola virus, Lassa virus, Marburg virus,
Crimean-Congo and others)
Clinical Presentation
Hemorrhagic fever with or without pneumonia
Infectious Substances
How it is Transmitted
Blood and bloody body fluids
Direct Contact Indirect Contact
Respiratory secretions Lassa: urine
Aerosols during AGMP Lassa: Sexual contact
Crimean-Congo: Tick bite Ebola: skin
Precautions Needed*
Droplet and Contact Precautions
Wear fit tested N95 respirator when performing Aerosol Generating Medical Procedures (AGMP)**
Duration of Precautions
Until directed by IPC or Zone Medical Officer of Health (MOH) or designate
Incubation Period
Period of Communicability
Variable
Variable
Comments
*Precautions required are in addition to Routine Practices
•
•
•
•
Notify Zone Medical Officer of Health of case by fastest means possible.
Refer to your facility’s policy regarding care of body after death
See Public Health Act – Bodies of Deceased Persons Regulation
AGMPs include
o
o
o
o
o
intubation
CPR
bronchoscopy
sputum induction
BiPAP
o
o
o
o
open tracheal suctioning
high frequency oscillatory ventilation
tracheostomy care
aerosolized medication administration
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
118
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Hepatitis – A, E
Clinical Presentation
Hepatitis, anicteria acute febrile illness
Infectious Substances
How it is Transmitted
Feces
Direct Contact (fecal/oral)
Indirect Contact (fecal/oral)
Precautions Needed*
Adults: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions
Duration of Precautions
7 days after onset of symptoms, duration of hospitalization if newborn
Incubation Period
Period of Communicability
Hepatitis A: 28 – 30 days
Hepatitis A: Two (2) weeks before to one (1) week
after onset of symptoms; shedding is prolonged in the
newborn (up to 6 months)
Hepatitis E: 26 – 42 days
Hepatitis E: fecal shedding continues at least two (2)
weeks
Comments
*Precautions required are in addition to Routine Practices
•
Post-exposure prophylaxis indicated for non-immune contacts with significant exposure to Hepatitis
A
•
Symptomatic residents must not participate in food handling activities
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
119
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Hepatitis – B, C, D, and other unspecified non-A, non-B
Clinical Presentation
Hepatitis, often asymptomatic; cirrhosis, hepatic cancer
Infectious Substances
How it is Transmitted
Blood and certain body fluids*
Mucosal or percutaneous exposure to infective body
fluids;
Sexual transmission;
Vertical mother to newborn
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Not applicable
B: all persons who are HBsAG positive
C: indefinite
D: indefinite
Comments
*Fluids include: blood; semen; uterine/vaginal fluid; breast milk; pleural, amniotic, pericardial, peritoneal,
synovial, and cerebral spinal fluids, but exclude other body fluids (feces, nasal secretions, sputum,
saliva, tears, urine or emesis) unless these fluids are visibly blood stained.
•
Refer to your facility’s policy regarding care of body after death
•
See Public Health Act – Bodies of Deceased Persons Regulation
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
120
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Herpangina (vesicular pharyngitis) – (Enterovirus)
Clinical Presentation
Fever, headache, loss of appetite, sore throat, ulcers or small blisters in mouth and throat
Infectious Substances
How it is Transmitted
Feces
Direct Contact (fecal/oral)
Respiratory secretions
Indirect Contact (fecal/oral)
Large Droplets
Precautions Needed*
Adult: Routine Practices
Children: Droplet Precautions
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
3 – 6 days for non-poliovirus
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
121
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Herpes simplex – Mucocutaneous – Disseminated or primary and
extensive
Clinical Presentation
Disseminated or primary and extensive lesions
Infectious Substances
How it is Transmitted
Skin or Mucosal lesions
Direct contact
Sexual transmission
Mother to child at birth
Precautions Needed*
Contact Precautions
Duration of Precautions
Until all lesions have crusted and dried
Incubation Period
Period of Communicability
2 days to 2 weeks
While lesions present
Comments
*Precautions required are in addition to Routine Practices
•
A resident with herpetic lesions should not be roomed with residents with eczema or burns or with
immunocompromised residents.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
122
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Herpes simplex (mucocutaneous) – Recurrent
Clinical Presentation
Not applicable
Infectious Substances
How it is Transmitted
Not applicable
Not applicable
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Not applicable
Not applicable
Comments
•
A resident with herpetic lesions should not be roomed with residents with eczema or burns or with
immunocompromised residents.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
123
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Herpes zoster: Shingles (Varicella zoster virus) – Disseminated
See Shingles: (Herpes zoster) Varicella zoster virus – Disseminated
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
124
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Herpes zoster: Shingles (Varicella zoster virus) – Exposed
Susceptible Contact
See Shingles: (Herpes zoster) Varicella zoster virus – Exposed Susceptible
Contact
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
125
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Herpes zoster: Shingles (Varicella zoster virus) –
Immunocompromised Host With Localized Lesions (1 or 2
dermatomes)
See Shingles: (Herpes zoster) Varicella zoster virus – Immunocompromised
Host With Localized Lesions (1 or 2 dermatomes)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
126
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Herpes zoster: Shingles (Varicella zoster virus) – Normal Host
With Localized Lesions(1 or 2 dermatomes) AND lesions that CAN
be covered with dressings or clothing
See Shingles: (Herpes zoster) Varicella zoster virus – Normal Host With
Localized Lesions (1 or 2 dermatomes) AND lesions that CAN be covered
with dressings or clothing
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
127
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Herpes zoster: Shingles (Varicella zoster virus) – Normal Host
With Localized Lesions (1 or 2 dermatomes) AND lesions that
CANNOT be covered with dressings or clothing
See Shingles: (Herpes zoster) Varicella zoster virus – Normal Host With
Localized Lesions (1 or 2 dermatomes) AND lesions that CANNOT be
covered with dressings or clothing
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
128
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Histoplasmosis (Histoplasma capsulatum)
Clinical Presentation
Pneumonia, lymphadenopathy, fever
Infectious Substances
How it is Transmitted
Mold in soil
Not person-to-person transmission
Acquired from inhalation of spore laden soil
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
3 – 17 days
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
129
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Hook worm (Necator americanus, Ancyclostoma duodenale)
Clinical Presentation
Usually asymptomatic
Infectious Substances
How it is Transmitted
Infective larvae
Not person-to-person transmission
Acquired from larvae in soil
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
4 – 6 weeks
Not person-to-person transmission
Comments
•
Larvae must hatch in soil to become infectious. Human infection occurs when larvae penetrate the
skin, usually of the foot.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
130
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Human Immunodeficiency Virus (HIV)
Clinical Presentation
Asymptomatic; multiple clinical presentations
Infectious Substances
How it is Transmitted
Blood and certain body fluids*
Mucosal or percutaneous exposure to infective body
fluids
Sexual transmission;
Vertical mother to newborn
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Weeks to years
From onset of infection
Comments
*Fluids include: blood; semen; uterine/vaginal fluid; breast milk; pleural, amniotic, pericardial, peritoneal,
synovial, and cerebral spinal fluids, but exclude other body fluids (feces, nasal secretions, sputum,
saliva, tears, urine or emesis) unless these fluids are visibly blood stained.
•
Refer to your facility’s policy for care of body after death.
•
See Public Health Act – Bodies of Deceased Persons Regulation
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
131
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Human Metapneumovirus
Clinical Presentation
Acute respiratory tract infection; bronchiolitis, pneumonia, croup
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Indirect Contact
Large Droplets
Precautions Needed*
Droplet and Contact Precautions
Duration of Precautions
Until symptoms have resolved.
For immunocompromised hosts (i.e. oncology, transplant residents), isolation precautions need to be
maintained for a longer duration due to prolonged viral shedding. Consult IPC or Zone Medical Officer of
Health (MOH) or designate for assistance
Incubation Period
Period of Communicability
Likely similar to RSV, 3 – 5 days
While symptomatic, although viral shedding can occur
for 1 – 2 weeks
Comments
*Precautions required are in addition to Routine Practices
•
For outbreaks: Refer to the AHS Guidelines for Outbreak Prevention, Control and Management in
Acute Care and Facility Living Sites, OR AHS Guidelines for Outbreak Prevention, Control and
Management in Supportive Living and Home Living Sites
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
132
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
I
Impetigo – (Staphylococcus aureus, Streptococcus [Group A], many other bacteria) See Draining Wounds
Influenza - Avian
Influenza – New Pandemic Strain
Influenza – Seasonal
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
133
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Impetigo – (Staphylococcus aureus, Streptococcus [Group A],
many other bacteria)
See Draining Wounds
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
134
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Influenza – Avian
Clinical Presentation
Respiratory tract infection, conjunctivitis
Infectious Substances
How it is Transmitted
Excreta of birds
Direct Contact
Possibly human respiratory tract secretions
Indirect Contact
Large Droplets
Precautions Needed*
Droplet and Contact Precautions
Wear fit tested N95 respirator when performing Aerosol Generating Medical Procedures (AGMP)*
Duration of Precautions
As directed by Zone Medical Officer of Health (MOH) or designate
Incubation Period
Period of Communicability
7 days or less, often 2 – 5 days
21 days
Comments
*Precautions required are in addition to Routine Practices
•
Most human infections by animal/bird influenza viruses are thought to result from direct contact with
infected birds/animals
•
For current information on Avian influenza, see Human Health Issues Related to Domestic Avian
Influenza in Canada available at http://www.phac-aspc.gc.ca/influenza/index-eng.php
http://www.phac-aspc.gc.ca/publicat/daio-enia/9-eng.php
•
AGMPs include:
o
o
o
o
o
intubation
CPR
bronchoscopy
sputum induction
BiPAP
o
o
o
o
open tracheal suctioning
high frequency oscillatory ventilation
tracheostomy care
aerosolized medication administration
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
135
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Influenza – New Pandemic Strain, Novel Influenza Viruses
Clinical Presentation
Respiratory tract infection
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Indirect Contact
Large Droplets
Precautions Needed*
As per Canadian Pandemic Plan Annex F, available at: http://www.phac-aspc.gc.ca/cpippclcpi/annf/index-eng.php
Duration of Precautions
As per Canadian Pandemic Plan Annex F, available at: http://www.phac-aspc.gc.ca/cpippclcpi/annf/index-eng.php
Incubation Period
Period of Communicability
Unknown, possibly 1 - 7 days
Unknown, possibly up to 7 days
Comments
*Precautions required are in addition to Routine Practices
• Notify Zone Medical Officer of Health of case by fastest means possible.
See Canadian Pandemic Plan Annex F, Infection Prevention and Control and Occupational Health and
Hygiene guidelines during Pandemic Influenza in Existing and Temporary Healthcare Settings, available
at: http://www.phac-aspc.gc.ca/cpip-pclcpi/annf/index-eng.php
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
136
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Influenza – Seasonal
Clinical Presentation
Respiratory tract infection
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact , Indirect Contact, Large Droplets
Precautions Needed*
Droplet and Contact Precautions
Wear fit tested N95 respirator when performing Aerosol Generating Medical Procedures (AGMP)
Duration of Precautions
5 days from onset of acute illness OR until they are over the acute illness and have been afebrile for 48
hours
Consult IPC or Zone Medical Officer of Health (MOH) or designate for assistance determining
when to discontinue additional precautions
Incubation Period
Period of Communicability
1 – 3 days
7 days (shedding may be longer in infants or
immunocompromised hosts)
Comments
*Precautions required are in addition to Routine Practices
•
•
•
Minimize exposure of immunocompromised residents.
For outbreaks. Refer to the AHS Guidelines for Outbreak Prevention, Control and Management in
Acute Care and Facility Living Sites, OR AHS Guidelines for Outbreak Prevention, Control and
Management in Supportive Living and Home Living Sites
AGMPs include:
o
o
o
o
o
intubation
CPR
bronchoscopy
sputum induction
BiPAP
o
o
o
o
open tracheal suctioning
high frequency oscillatory ventilation
tracheostomy care
aerosolized medication administration
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
137
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
J
No organisms at this time
K
Klebsiella spp. (Multi-Drug Resistant; Carbapenem resistant {CRE}; ESBL or Amp-C producing)
See Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing)
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
138
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Klebsiella spp. (Multi-Drug Resistant; Carbapenem resistant
[CRE]; ESBL or Amp-C producing)
E. coli, Klebsiella spp., Serratia spp., Providencia spp., Proteus spp., Citrobacter spp.,
Enterobacter spp., Morganella spp., Salmonella spp., Hafnia spp.
See Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE];
ESBL or Amp-C producing)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
139
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
L
Lassa fever (Lassa Virus) See Hemorrhagic Viral Fevers
Legionella (Legionella spp.)
Leprosy (Hansen’s disease) (Mycobacterium leprae)
Leptospirosis (Leptospira sp.)
Lice (Pediculosis) – (Pediculus humanus, Phthirus pubis)
Listeriosis (Listeria monocytogenes)
Lyme disease (Borrelia burgdorferi)
Lymphocytic choriomeningitis virus
Lymphogranuloma venereum (Chlamydia trachomatis)
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
140
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Lassa fever (Lassa Virus)
See Hemorrhagic Viral Fevers
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
141
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Legionella (Legionella spp.)
Clinical Presentation
Pneumonia, Legionnaires’’ disease, Pontiac fever
Infectious Substances
How it is Transmitted
Contaminated water sources
Not person-to-person transmission
Transmission occurs with aerosolization of
contaminated water and subsequent airborne spread.
Acquired from contaminated water by inhalation or
aspiration.
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
2 – 10 days
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
142
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Leprosy (Hansen’s disease) (Mycobacterium leprae)
Clinical Presentation
Chronic disease of skin, nerves, nasopharyngeal mucosa
Infectious Substances
How it is Transmitted
Nasal secretions,
Direct Contact (requires prolonged and extensive
personal contact)
Skin lesions
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
One year to many years
Until treatment is established
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
143
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Leptospirosis (Leptospira sp.)
Clinical Presentation
Fever, jaundice, aseptic meningitis
Infectious Substances
How it is Transmitted
Urine or tissues of infected animals or water
contaminated with the urine of infected animals.
Not person-to-person transmission
Transmitted through skin or mucous membrane
contact with urine or tissues of infected animals or
water contaminated with the urine of infected animals.
Precautions Needed
Routine Practices
Duration of Precautions
Not Applicable
Incubation Period
Period of Communicability
2 – 26 days
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
144
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Lice (Pediculosis) – (Pediculus humanus, Phthirus pubis)
Clinical Presentation
Scalp or body itch, itchy rash
Infectious Substances
How it is Transmitted
Louse
Head and body lice: direct and indirect contact
Pubic lice: usually sexual contact
Precautions Needed*
Contact Precautions
Duration of Precautions
Until 24 hours after application of appropriate pediculicide; applied as directed
Incubation Period
Period of Communicability
6 – 10 days
Until effective treatment to kill lice and ova and
observed to be free of lice
Comments
*Precautions required are in addition to Routine Practices
•
Apply pediculicide as directed on label. If live lice found after therapy, repeat treatment.
•
Head lice: wash headgear, combs, pillow cases, towels with hot water or dry clean or seal in plastic
bag and store for 10 days.
•
Body lice: as above, for all exposed clothing and bedding
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
145
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Listeriosis (Listeria monocytogenes)
Clinical Presentation
Fever, meningitis, congenital or neonatal infection
Infectious Substances
How it is Transmitted
Contaminated food
Acquired from contaminated food
Animal reservoirs (infected/colonized domestic
and wild mammals, fowl and people)
Vertical mother to child in utero or at birth
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Average 21 days
Days to months
Comments
•
Rare nosocomial outbreaks reported in newborn nurseries attributed to contaminated equipment or
materials.
•
Listeria grows well at low temperatures and is able to multiply in refrigerated foods that are
contaminated.
•
Pregnant women and immunocompromised persons should avoid unpasteurized cheese, cold cuts,
and uncooked meat products including hot dogs.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
146
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Lyme disease (Borrelia burgdorferi)
Clinical Presentation
Fever, rash, arthritis, meningitis
Infectious Substances
How it is Transmitted
Tick
Not person-to-person transmission
Vector borne: Tick
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Rash occurs in 3 – 31 days after exposure
Not person-to-person transmission
Comments
•
Infection in humans is incidental and is acquired most frequently during blood feeding by the infected
tick.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
147
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Lymphocytic choriomeningitis virus
Clinical Presentation
Aseptic meningitis
Infectious Substances
How it is Transmitted
Urine of rodents
Not person-to-person transmission
Acquired from contact with rodents
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
6 – 21 days
Not person-to-person transmission
Comments
•
Transmission to humans is probably through oral or respiratory contact with virus contaminated
excreta of infected rodents.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
148
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Lymphogranuloma venereum (Chlamydia trachomatis)
Clinical Presentation
Genital ulcers, inguinal adenopathy
Infectious Substances
How it is Transmitted
Open lesions
Sexual contact
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
3 – 30 days for a primary lesion
As long as organism present in secretions
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
149
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
M
Malaria (Plasmodium spp.)
Marburg virus See Hemorrhagic Viral Fevers
Measles – (Rubeola) – Exposed Susceptible Contact
Measles – (Rubeola) – Known Case
Melioidosis (Burkholderia pseudomallei)
Meningitis
Meningococcus (Neisseria meningitidis) See Neisseria meningitidis
MERS – (Middle Eastern Respiratory Syndrome; Coronovirus) See Coronavirus – Severe Acute Respiratory
Syndrome (SARS-CoV), Middle Eastern Respiratory Syndrome (MERS-CoV)
Methicillin Resistant Staphylococcus aureus (MRSA)
Molluscum contagiosum (Molluscum contagiosum virus)
Monkey Pox
Mononucleosis (Epstein-Barr virus) See Epstein – Barr virus (Human Herpes Virus 4)
Morganella spp. (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing) See
Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing)
Mucormycosis (phycomycosis, zygomycosis) – (Mucor sp., Zygomycetes sp., Rhizopus sp.)
Multi-Drug Resistant (MDR) Gram Negative Bacilli
Mumps (Mumps virus) – Known Case
Mumps – (Mumps virus) Exposed Susceptible Contact
Mycobacterium – Non-tuberculosis (atypical) (e.g., Mycobacterium avium complex)
Mycobacterium tuberculosis (TB) – extrapulmonary disease or not respiratory; (also M. africanum, M.bovis, M.
caprae, M. microti, M. pinnipedii)
Mycobacterium tuberculosis (TB) – respiratory or pulmonary disease; (also M. africanum, M.bovis, M. caprae, M.
microti, M. pinnipedii)
Mycoplasma pneumoniae
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
150
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Malaria (Plasmodium spp.)
Clinical Presentation
Fever
Infectious Substances
How it is Transmitted
Blood
Vector borne: Mosquito bite
Rarely transplacental from mother to fetus
Blood transfusion
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Variable
Not usually person-to-person transmission
Comments
•
Infection in humans is incidental and is acquired most frequently during blood feeding by the infected
mosquito.
•
Can be transmitted via blood transfusion.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
151
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Marburg virus
See Hemorrhagic Viral Fevers
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
152
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Measles – (Rubeola) – Exposed Susceptible Contact
Clinical Presentation
Susceptible contact. Asymptomatic - may develop measles
Infectious Substances
How it is Transmitted
Respiratory secretions
Airborne
Precautions Needed*
Airborne Precautions
Duration of Precautions
From 5 days after first exposure until 21 days after last exposure
If measles develop: Stop 4 days after start of rash in immunocompetent residents or until all symptoms
are gone in immunocompromised residents
Incubation Period
Period of Communicability
7 – 18 days
5 days before start of rash (1 – 2 days before start of
other symptoms) and until 4 days after onset of rash
(longer in immunocompromised residents)
Comments
*Precautions required are in addition to Routine Practices
•
•
•
Defer non-urgent admission if a non-immune person is incubating the disease.
Individuals with known immunity to measles (serological proof of immunity; immunization with 2
appropriately timed doses of measles-containing vaccine) are not required to wear the N95
respirator when entering the room.
Susceptible HCWs should not enter the room if immune staff are available. If they must enter the
room, an N95 respirator must be worn. Other non-immune persons should not enter except in
urgent or compassionate circumstances. If immunity is unknown, assume person is non-immune.
Discharge Settle Time
Non-negative pressure rooms:
• Do not admit a new resident into this room for at least 4 hours. If staff must enter room before 4
hours has passed and non-immune, wear an N95 respirator.
Negative pressure rooms:
• Do not admit a new resident into this room for at least 45 minutes. If staff must enter room before 45
minutes has passed and non-immune, wear an N95 respirator.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
153
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Measles – (Rubeola) – Known Case
Clinical Presentation
Fever, coryza, maculopapular skin rash, conjunctivitis, cough
Infectious Substances
How it is Transmitted
Respiratory secretions
Airborne
Precautions Needed*
Airborne Precautions
Duration of Precautions
Stop 4 days after start of rash in immunocompetent residents or until all symptoms are gone in
immunocompromised residents.
Incubation Period
Period of Communicability
7 – 18 days
5 days before start of rash (1 – 2 days before start of
other symptoms) and until 4 days after onset of rash
(longer in immunocompromised residents)
Comments
*Precautions required are in addition to Routine Practices
•
•
•
•
•
Notify Zone Medical Officer of Health of case by fastest means possible.
Defer non-urgent admission if measles is present.
Individuals with known immunity to measles are not required to wear the N95 respirator when
entering the room. Known immunity: Serological proof of immunity or documentation of 2
appropriately timed doses of vaccine, or received a minimum dose of Immunoglobulin (0.25/kg)
within 5 months of exposure.
Susceptible HCWs should not enter the room if immune staff are available. If they must enter the
room, an N95 respirator must be worn. Other non-immune persons should not enter except in
urgent or compassionate circumstances. If immunity is unknown, assume person is non-immune
Immunoprophylaxis is indicated for susceptible contacts.
Discharge Settle Time
Non-negative pressure rooms:
• Do not admit a new resident into this room for at least 4 hours. If staff must enter room before 4
hours has passed and non-immune, wear an N95 respirator.
Negative pressure rooms:
• Do not admit a new resident into this room for at least 45 minutes. If staff must enter room before 45
minutes has passed and non-immune, wear an N95 respirator
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
154
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Melioidosis (Burkholderia pseudomallei)
Clinical Presentation
Pneumonia, fever, papules with umbilical centres
Infectious Substances
How it is Transmitted
Contaminated soil
Not person-to-person transmission
Acquired from direct contact with contaminated water
or soil, aspiration or ingestion of contaminated water
or inhalation of contaminated dust.
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Not applicable
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
155
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Meningitis
(Various causative agents: Bacterial: Neisseria meningitides, H. influenza type B
(possible in non-immune infant younger than 2 years of age), Streptococcus
pneumoniae, Group B Streptococcus, Listeria monocytogenes, E. coli and other Gramnegative rods, Mycobacterium tuberculosis. Viral: enterovirus, arborviruses)
Clinical Presentation
Meningitis
Infectious Substances
How it is Transmitted
Respiratory secretions
Feces (in viral meningitis)
Bacterial: Direct contact ; Large droplets
Viral: Direct and indirect contact (including fecal/oral)
Precautions Needed*
Adult:
Cause unknown or bacterial: Droplet Precautions until Neisseria meningitidis ruled out, otherwise
Routine Practices.
Neisseria meningitidis: Droplet Precautions
Viral: Routine Practices
Children:
Cause unknown or bacterial: Droplet and Contact Precautions
Viral: Contact Precautions
Duration of Precautions
Adult:
Neisseria meningitidis: Until 24 hours of effective antimicrobial therapy has been received
Children:
Bacterial meningitis: Until 24 hours of effective antimicrobial therapy has been received
Viral meningitis: Until symptoms have resolved or until enterovirus ruled out. See specific organism.
Incubation Period
Period of Communicability
Variable
Variable
Comments
*Precautions required are in addition to Routine Practices
•
•
For Mycobacterium tuberculosis meningitis rule out associated respiratory TB
May be associated with measles, mumps, varicella, or herpes simplex. If identified, take appropriate
precautions for associated disease.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
156
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Meningococcus (Neisseria meningitidis)
See Neisseria meningitidis
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
157
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
MERS – (Middle Eastern Respiratory Syndrome; Coronovirus)
See Coronavirus – Severe Acute Respiratory Syndrome (SARS-CoV), Middle
Eastern Respiratory Syndrome (MERS-CoV)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
158
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Methicillin Resistant Staphylococcus aureus (MRSA)
Clinical Presentation
Colonization or infection of any body site
Infectious Substances
How it is Transmitted
Colonized or infected skin, secretions or
excretions
Direct contact
Indirect contact
Large Droplets if symptoms of acute respiratory tract
infection
Precautions Needed*
See Additional Precautions for ARO Positive Residents in Continuing Care information sheet
Duration of Precautions
Residents must be reassessed regularly and as conditions and behaviours change
Additional precautions for ARO positive residents in continuing care may be discontinued when resident
is cooperative with hygiene practices and drainage and body fluids are contained.
If needed, consult IPC or Zone Medical Officer of Health (MOH) or designate for assistance determining
when to discontinue additional precautions for ARO positive resident
Incubation Period
Period of Communicability
Variable
While organism is present in secretions or excretions
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
159
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Molluscum contagiosum (Molluscum contagiosum virus)
Clinical Presentation
Umbilicated papules
Infectious Substances
How it is Transmitted
Contents of the papules
Direct contact*
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
1 week to 6 months
Unknown
Comments
*Requires close direct personal contact for transmission
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
160
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Monkey Pox
Clinical Presentation
Resembles smallpox, swollen lymph nodes
Infectious Substances
How it is Transmitted
Infected blood and body fluids
Bite from infected animal or direct contact with their
blood, body fluid or rash.
Pox secretions
Precautions Needed*
Routine Practices, Airborne Precautions and Droplet and Contact Precautions
Duration of Precautions
As directed by IPC or Zone Medical Officer of Health (MOH) or designate
Incubation Period
Period of Communicability
12 days
2 – 4 weeks
Comments
*Precautions required are in addition to Routine Practices
•
Notify Medical Officer of Health of case by fastest means possible.
•
Transmission in hospital settings is unlikely
•
See www.cdc.gov/ncidod/monkeypox for their current recommendations
•
Discharge Settle Time
o
o
Non-negative pressure rooms: Do not admit a new resident into this room for at least 4 hours.
If staff must enter room before 4 hours has passed and non-immune, wear an N95 respirator.
Negative pressure rooms: Do not admit a new resident into this room for at least 45 minutes.
If staff must enter room before 45 minutes has passed and non-immune, wear an N95
respirator.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
161
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Mononucleosis (Epstein-Barr virus)
See Epstein – Barr virus (Human Herpes Virus 4)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
162
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Morganella spp. (Multi-Drug Resistant; Carbapenem resistant
[CRE]; ESBL or Amp-C producing)
E. coli, Klebsiella spp., Serratia spp., Providencia spp., Proteus spp., Citrobacter spp.,
Enterobacter spp., Morganella spp., Salmonella spp., Hafnia spp.
See Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE];
ESBL or Amp-C producing)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
163
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Mucormycosis (phycomycosis, zygomycosis) – (Mucor sp.,
Zygomycetes sp., Rhizopus sp.)
Clinical Presentation
Skin, wound, rhino-cerebral, pulmonary, gastrointestinal, disseminated infection
Infectious Substances
How it is Transmitted
Fungal spores in dust and soil
Not person-to-person transmission
Acquired from inhalation or ingestion of fungal spores
in dust, soil
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Unknown
Not person-to-person transmission
Comments
•
Immunocompromised residents are at risk of infection.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
164
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Multi-Drug Resistant (MDR) Gram Negative Bacilli
•
•
•
•
•
MDR Acinetobacter sp.
MDR Pseudomonas sp. (ESBL, AmpC or MBL producing)
Stenotrophomonas maltophilia**
Burkholderia cepacia**
MDR Enterobacteriaceae (Carbapenem resistant (CRE); ESBL or Amp C producing)
E. coli, Klebsiella sp., Serratia sp., Providencia sp., Proteus sp., Citrobacter sp., Enterobacter sp.,
Morganella sp., Salmonella sp., Hafnia spp.
Clinical Presentation
Colonization or infection of any body site
Infectious Substances
How it is Transmitted
Colonized or infected secretions/ or excretions
Direct contact
Indirect contact
Large Droplets if symptoms of acute respiratory tract
infection
Precautions Needed*
See Additional Precautions for ARO Positive Residents in Continuing Care information sheet for all
organisms listed above except those identified by asterisks**
**See specific organism for more information.
Duration of Precautions
Residents must be reassessed regularly and as conditions and behaviours change
Additional precautions for ARO positive residents in continuing care may be discontinued when resident
is cooperative with hygiene practices and drainage and body fluids are contained.
If needed, consult IPC or Zone Medical Officer of Health (MOH) or designate for assistance determining
when to discontinue additional precautions for ARO positive resident
Incubation Period
Period of Communicability
Variable
While organism is present in secretions or excretions
Comments
*Precautions required are in addition to Routine Practices
•
Isolation precautions are dependent on organism type and antibiotic susceptibility pattern.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
165
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Mumps (Mumps virus) – Known Case
Clinical Presentation
Swelling of salivary glands, orchitis, meningitis
Infectious Substances
How it is Transmitted
Saliva
Direct Contact
Respiratory secretions
Large Droplets
Precautions Needed*
Droplet Precautions
Duration of Precautions
Maintain isolation until 5 days after the onset of symptoms
Incubation Period
Period of Communicability
14 – 25 days
2 days before and up to 5 days after onset of
symptoms
Comments
*Precautions required are in addition to Routine Practices
•
Droplet Precautions for exposed susceptible residents and healthcare workers should begin 10
days after first contact and continue through 26 days after last exposure.
•
Defer non-urgent admission if mumps is present.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
166
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Mumps – (Mumps virus) Exposed Susceptible Contact
Clinical Presentation
Susceptible contact. Asymptomatic - may develop mumps
Infectious Substances
How it is Transmitted
Saliva
Direct Contact
Respiratory secretions
Large Droplets
Precautions Needed*
Droplet Precautions
Duration of Precautions
Should begin 10 days after first contact and continue until 26 days after last exposure
If mumps develop: Maintain isolation until 5 days after the onset of symptoms
Incubation Period
Period of Communicability
14 – 25 days
2 days before and up to 5 days after onset of
symptoms
Comments
*Precautions required are in addition to Routine Practices
•
Defer non-urgent admission if a non-immune person is incubating the disease
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
167
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Mycobacterium – Non-tuberculosis (atypical) (e.g., Mycobacterium
avium complex)
Clinical Presentation
Lymphadenitis, pneumonia, disseminated disease in immunocompromised host
Infectious Substances
How it is Transmitted
In environmental sources – soil, water, animal
reservoirs
Not person-to-person transmission
Acquired from soil, water, animal reservoirs
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Unknown
Not person-to-person transmission
Comments
168
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
169
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Mycobacterium tuberculosis (TB) – extrapulmonary disease or not
respiratory; (also M. africanum, M. bovis, M. caprae, M. microti, M.
pinnipedii)
Clinical Presentation
Extrapulmonary: meningitis, bone or joint infections, draining lesions
Infectious Substances
How it is Transmitted
Aerosolized wound drainage if present
Airborne transmission possible if procedures that may
aerosolize wound drainage are being performed
Precautions Needed*
Routine Practices
Airborne Precautions required only if procedures that may aerosolize drainage from draining lesions
are being performed or for suspicion of miliary tuberculosis with pulmonary involvement (see
Mycobacterium tuberculosis-Respiratory)
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Weeks to years
While organisms are in drainage
Comments
*Precautions required are in addition to Routine Practices
•
Assess for concurrent pulmonary tuberculosis
•
Avoid procedures that may generate aerosols from drainage
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
170
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Mycobacterium tuberculosis (TB) – respiratory or pulmonary
disease; (also M. africanum, M. bovis, M. caprae, M. microti, M.
pinnipedii)
Clinical Presentation
Confirmed or suspected pulmonary tuberculosis (including pleural and laryngeal tuberculosis)
Infectious Substances
How it is Transmitted
Respiratory secretions
Airborne
Precautions Needed*
Airborne Precautions
Duration of Precautions
Contact Zone Medical Officer of Health or designate prior to stopping precautions.
Criteria for discontinuing precautions include: 1) Receipt of 2 weeks effective treatment, AND, 2) Clinical
improvement, AND, 3) Three (3) consecutive negative Acid Fast Bacilli (AFB) sputums collected 8 – 24
hours apart. If multi-drug resistant tuberculosis, until culture negative.
Incubation Period
Period of Communicability
Weeks to years
While organisms are in sputum
Comments
*Precautions required are in addition to Routine Practices
•
•
•
Refer to existing policy re: care of body after death
See Public Health Act – Bodies of Deceased Persons Regulation
Notify Zone Medical Officer of Health (or designate) of case by fastest means possible.
Discharge Settle Time
Non-negative pressure rooms:
• Do not admit a new resident into this room for at least 4 hours. If staff must enter room before 4
hours, wear an N95 respirator.
Negative pressure rooms:
• Do not admit a new resident into this room for at least 45 minutes. If staff must enter room before 45
minutes wear an N95 respirator
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
171
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Mycoplasma pneumoniae
Clinical Presentation
Pneumonia
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Large Droplets
Precautions Needed*
Droplet Precautions
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
1 – 4 weeks
Unknown
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
172
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
N
Neisseria gonorrhoeae
Neisseria meningitidis
Nocardiosis (Nocardia sp.)
Norovirus
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
173
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Neisseria gonorrhoeae
Clinical Presentation
Opthalmaia, neonatorum, gonorrhea, arthritis, pelvic inflammatory disease.
Infectious Substances
How it is Transmitted
Exudates from lesions
Mother to child at birth
Sexual contact
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
2 – 7 days
Until effective antimicrobial therapy has been
completed
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
174
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Neisseria meningitidis
Clinical Presentation
Rash (petechial/purpuric) with fever, meningococcemia, meningitis, pneumonia,
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Large droplets
Precautions Needed*
Droplet Precautions
Duration of Precautions
Until 24 hours of effective antimicrobial therapy has been received
Incubation Period
Period of Communicability
Usually 2 – 10 days
Until 24 hours of effective antimicrobial therapy has
been received
Comments
*Precautions required are in addition to Routine Practices
•
Notify Zone Medical Officer of Health of case by fastest means possible.
•
Close contacts may require chemoprophylaxis.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
175
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Nocardiosis (Nocardia sp.)
Clinical Presentation
Fever, pulmonary or central nervous system infection or disseminated disease
Infectious Substances
How it is Transmitted
Organisms in the soil and dust
Not person-to-person transmission
Acquired from inhalation or skin inoculation of the
organism in dust
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Unknown
Not person-to-person transmission
Comments
•
Infections in immunocompromised residents may be associated with construction.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
176
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Norovirus
Clinical Presentation
Diarrhea and/or vomiting
Infectious Substances
How it is Transmitted
Feces
Direct Contact (fecal/oral)
Emesis/vomit
Indirect Contact (fecal/oral)
Large Droplets
Precautions Needed*
Contact Precautions
If resident is actively vomiting: Droplet and Contact Precautions
Duration of Precautions
Until symptoms have been resolved for at least 48 hours and stools are normal
Incubation Period
Period of Communicability
12 hours to 4 days
Until 48 hours after symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
•
For outbreaks: Refer to the AHS Guidelines for Outbreak Prevention, Control and Management in
Acute Care and Facility Living Sites, OR AHS Guidelines for Outbreak Prevention, Control and
Management in Supportive Living and Home Living Sites.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
177
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
O
Orf – parapoxvirus
Osteomyelitis (Haemophilus influenzae type B (HIB) [possible in non-immune infant <2 yrs of age], Staphylococcus
aureus, other bacteria)
Otitis, draining (Streptococcus [Group A], Staphylococcus aureus, Many other bacteria) See Draining Wounds
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
178
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Orf – parapoxvirus
Clinical Presentation
Skin lesions
Infectious Substances
How it is Transmitted
Organism in various animals (sheep, goats,
reindeer, musk oxen) and soil
Not person-to-person transmission
Acquired from direct contact with infected animals
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
3 – 6 days
Not person-to-person transmission
Comments
•
Acquired from direct contact with infected animals, usually sheep and goats
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
179
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Osteomyelitis (Haemophilus influenzae type B (HIB) [possible in
non-immune infant less than 2 years of age], Staphylococcus
aureus, other bacteria)
Clinical Presentation
Inflammation, fever, wound drainage
Infectious Substances
How it is Transmitted
Respiratory secretions if HIB
Direct Contact if HIB
Large Droplets if HIB
Precautions Needed*
Adult: Routine Practices
Children: Droplet Precautions if HIB, otherwise Routine Practices
Duration of Precautions
Until 24 hours of effective antimicrobial therapy has been received, or HIB ruled out.
Incubation Period
Period of Communicability
Variable
Not applicable
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
180
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Otitis, draining (Streptococcus [Group A], Staphylococcus aureus,
Many other bacteria)
See Draining Wounds
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
181
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
P
Parainfluenza virus
Parvovirus B19 – Fifth’s Disease, Erythema infectiosum (rash), Aplastic crisis
Pediculosis (Lice) – (Pediculus humanus, Phthirus pubis) See Lice (Pediculosis) – (Pediculus humanus, Phthirus
pubis)
Pertussis – Bordetella pertussis
Pharyngitis – (Streptococcus [Group A], Corynebacterium diphtheriae, many viruses)
Pinworm (Oxyuriasis) – (Enterobius vermicularis) See Enterobiasis (pinworm) (Oxyuriasis, Enterobius vermicularis))
Plague – Bubonic (Yersinia pestis)
Plague – Pneumonic (Yersinia pestis)
Pleurodynia (Enterovirus, Coxsackievirus)
Pneumocystis jiroveci Pneumonia (PJP) – formerly known as P. carinii (PCP)
Pneumonia
Poliomyelitis
Prion Disease – Creutzfeldt-Jakob Disease (CJD); classic and variant (vCJD) See Creutzfeldt-Jakob Disease –
classic (CJD) and variant (vCJD)
Proteus spp. (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing)
See Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing)
Providencia spp. (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing) See
Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing)
Pseudomembraneous colitis – (Clostridium difficile) See Clostridium difficile Infection (CDI)
Pseudomonas aeruginosa (Multi-Drug Resistant or Metallo-Carbapenamase producing**)
Psittacosis (Ornithosis) – (Chlamydia psittaci)
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
182
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Parainfluenza virus
Clinical Presentation
Respiratory tract infection
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Indirect Contact
Large Droplets
Precautions Needed*
Droplet and Contact Precautions
Duration of Precautions
Until symptoms have resolved
For immunocompromised hosts (i.e. oncology, transplant residents), isolation precautions need to be
maintained for a longer duration due to prolonged viral shedding. Contact IPC or Zone Medical Officer
of Health (MOH) or designate for assistance with discontinuation of precautions.
Incubation Period
Period of Communicability
2 – 6 days
Variable
Comments
*Precautions required are in addition to Routine Practices
•
May cohort with others with same virus. Minimize exposure of immunocompromised residents
•
For outbreaks. Refer to the AHS Guidelines for Outbreak Prevention, Control and Management in
Acute Care and Facility Living Sites, OR AHS Guidelines for Outbreak Prevention, Control and
Management in Supportive Living and Home Living Sites.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
183
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Parvovirus B19 – Fifth Disease, Erythema infectiosum (rash),
Aplastic crisis
Clinical Presentation
Erythema Infectiousum (rash); aplastic crisis
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Large Droplets
Vertical, mother to fetus
Precautions Needed*
Fifth Disease: Routine Practices
Aplastic crisis: Droplet Precautions
Duration of Precautions
If aplastic crisis maintain precautions for 7 days. For immuno-suppressed residents with chronic infection
or those with papular purpuric gloves and socks syndrome (PPGS), consult IPC or Zone Medical Officer
of Health (MOH) or designate for assistance determining when to discontinue additional precautions
Incubation Period
Period of Communicability
4 – 21 days
Fifth disease: Immunocompetent residents are no
longer infectious by the time the rash appears
Aplastic crisis: up to 1 week after onset of crisis.
Immunocompromised with chronic infection: months
to years
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
184
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Pediculosis (Lice) – (Pediculus humanus, Phthirus pubis)
See Lice (Pediculosis) – (Pediculus humanus, Phthirus pubis)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
185
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Pertussis – Whooping Cough (Bordetella pertussis)
Clinical Presentation
Whooping cough, non-specific respiratory tract infections in infants, adolescents and adults.
Infectious Substances
How it is Transmitted
Respiratory secretions
Large Droplets
Precautions Needed*
Droplet Precautions
Duration of Precautions
Up to 3 weeks after onset of paroxysms if not treated or until 5 days of effective antimicrobial treatment
has been received
Incubation Period
Period of Communicability
6 – 20 days
At onset of mild respiratory tract symptoms (catarrhal
stage) up to 3 weeks after onset of paroxysms or
coughing if not treated; or until 5 days of effective
antimicrobial therapy has been received.
Comments
*Precautions required are in addition to Routine Practices
•
Close contacts may need chemoprophylaxis
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
186
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Pharyngitis – (Streptococcus [Group A], Corynebacterium
diphtheriae, many viruses)
Clinical Presentation
Sneezing, coughing, fever, headache, sore throat
Infectious Substances
How it is Transmitted
Respiratory secretions
See specific organism
Precautions Needed*
Adult: See specific organism, otherwise: Routine Practices
Children: Droplet and Contact Precautions
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Variable
Variable
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
187
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Pinworm (Oxyuriasis) – (Enterobius vermicularis)
See Enterobiasis (pinworm) (Oxyuriasis, Enterobius vermicularis)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
188
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Plague – Bubonic (Yersinia pestis)
Clinical Presentation
Lymphadenitis
Infectious Substances
How it is Transmitted
Infected rodents and their fleas
Not person-to-person transmission
Acquired from the bite of an infected flea
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
1 – 7 days
Not person-to-person transmission
Comments
•
Notify Zone Medical Officer of Health of case by fastest means possible.
•
Refer to your facility’s policy for care of body after death.
•
See Public Health Act – Bodies of Deceased Persons Regulation
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
189
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Plague – Pneumonic (Yersinia pestis)
Clinical Presentation
Pneumonia, cough, fever, hemoptysis
Infectious Substances
How it is Transmitted
Respiratory secretions
Large Droplets
Precautions Needed*
Droplet Precautions
Duration of Precautions
Until 48 hours of effective antimicrobial therapy has been received
Incubation Period
Period of Communicability
1 – 4 days
Until 48 hours of effective antimicrobial therapy has
been received.
Comments
*Precautions required are in addition to Routine Practices
•
Notify Zone Medical Officer of Health of case by fastest means possible.
•
Close contacts may require prophylaxis
•
Refer to your facility’s policy for care of body after death.
•
See Public Health Act – Bodies of Deceased Persons Regulation
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
190
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Pleurodynia (Enterovirus, Coxsackievirus)
Clinical Presentation
Brief fever, severe chest and lower back pain
Infectious Substances
How it is Transmitted
Feces
Direct Contact (including fecal/oral)
Respiratory secretions
Indirect Contact (including fecal/oral)
Large Droplets
Precautions Needed*
Adult: Routine Practices
Children: Contact Precautions
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
2 – 4 days
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
191
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Pneumocystis jiroveci Pneumonia (PJP) – formerly known as P.
carinii (PCP)
Clinical Presentation
Pneumonia in an immunocompromised host
Infectious Substances
How it is Transmitted
Not applicable
Unknown
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Unknown
Unknown
Comments
•
Ensure roommate is not immunocompromised
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
192
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Pneumonia
(Various causative agents: bacteria, viruses fungi, other agents)
See Specific Organism
Clinical Presentation
Pneumonia
Infectious Substances
How it is Transmitted
Respiratory secretions
Large Droplets
Direct Contact
Indirect Contact
Precautions Needed
As for specific organism, otherwise: Routine Practices
Duration of Precautions
As for specific organism
Incubation Period
Period of Communicability
Variable
Variable
Comments
•
Minimize exposure of immumocompromised residents.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
193
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Poliomyelitis
Clinical Presentation
Flaccid paralysis
Infectious Substances
How it is Transmitted
Feces
Direct Contact (fecal/oral)
Respiratory secretions
Indirect Contact (fecal/oral)
Precautions Needed*
Contact Precautions
Duration of Precautions
Until 6 weeks from start of illness or until feces culture negative
Incubation Period
Period of Communicability
3 – 35 days
Duration of shedding is up to 6 weeks.
Comments
*Precautions required are in addition to Routine Practices
•
Notify Zone Medical Officer of Health of case by fastest means possible
•
Most infectious during the days before and after onset of symptoms
•
Close contacts who are not immune should receive immunoprophylaxis
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
194
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Prion Disease – Creutzfeldt-Jakob Disease (CJD); classic and
variant (vCJD)
See Creutzfeldt-Jakob Disease – classic (CJD) and variant (vCJD)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
195
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Proteus spp. (Multi-Drug Resistant; Carbapenem resistant [CRE];
ESBL or Amp-C producing)
E. coli, Klebsiella spp., Serratia spp., Providencia spp., Proteus spp., Citrobacter spp.,
Enterobacter spp., Morganella spp., Salmonella spp., Hafnia spp.
See Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE];
ESBL or Amp-C producing)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
196
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Providencia spp. (Multi-Drug Resistant; Carbapenem resistant
[CRE]; ESBL or Amp-C producing)
E. coli, Klebsiella spp., Serratia spp., Providencia spp., Proteus spp., Citrobacter spp.,
Enterobacter spp., Morganella spp., Salmonella spp., Hafnia spp.
See Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE];
ESBL or Amp-C producing)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Comments
197
Period of Communicability
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
198
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Pseudomembranous colitis – (Clostridium difficile)
See Clostridium difficile Infection (CDI)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
199
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Pseudomonas aeruginosa (Multi-Drug Resistant or MetalloCarbapenamase producing**)
(ESBL, AmpC or MBL producing)
Clinical Presentation
Colonization or infection of any body site
Infectious Substances
How it is Transmitted
Colonized or infected secretions or excretions
Direct contact Indirect contact
Large Droplets if symptoms of acute respiratory tract
infection
Precautions Needed*
See Additional Precautions for ARO Positive Residents in Continuing Care information sheet
Duration of Precautions
Residents must be reassessed regularly and as conditions and behaviours change
Additional precautions for ARO positive residents in continuing care may be discontinued when resident
is cooperative with hygiene practices and drainage and body fluids are contained.
If needed, consult IPC or Zone Medical Officer of Health (MOH) or designate for assistance determining
when to discontinue additional precautions for ARO positive resident
Incubation Period
Period of Communicability
Variable
While organism is present in secretions or excretions
Comments
*Precautions required are in addition to Routine Practices
•
•
•
Must demonstrate complete resistance to more than 3 antibiotic classes usually tested, including
carbapenems
**May be identified as Metallo-Carbapenamase producing or Metallo-beta-lactamase producing
(MBL) Pseudomonas on the lab report.
Note: β=beta
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
200
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Psittacosis (Ornithosis) – (Chlamydia psittaci)
Clinical Presentation
Pneumonia, fever
Infectious Substances
How it is Transmitted
Infected birds
Not person-to-person transmission
Acquired from contact with infected birds
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
7 – 14 days
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
201
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Q
Q Fever (Coxiella burnetii)
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
202
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Q Fever (Coxiella burnetii)
Clinical Presentation
Pneumonia, fever
Infectious Substances
How it is Transmitted
Infected animals, milk
Acquired from contact with infected animals or from
ingestion of raw milk
Not person-to-person transmission
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
14 – 39 days
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
203
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
R
Rabies
Rash, compatible with scabies – (Ectoparasite)
Rash, maculopapular –(Suspected Rubeola virus [Measles])
Rash, petechial or purpuric – (Suspected Neisseria meningitidis)
Rash, vesicular – (Suspected Varicella virus - Chickenpox)
Rat-bite fever – (Streptobacillus moniliformis; Spirillum minus)
Relapsing fever (Borrelia sp.)
Rhinovirus
Rickettsialpox (Rickettsia akari)
Ringworm (Tinea) – (Trichophyton sp., Microsporum sp., Epidermophyton sp.)
Ritters Disease – Staphylococcal scalded skin syndrome (SSSS) See Scalded skin syndrome – Ritter’s Disease
(Staphylococcus aureus)
Rocky Mountain Spotted Fever (Rickettsia rickettsii)
Roseola infantum – Human herpes virus 6
Rotavirus
Roundworm – Ascariasis (Ascaris spp.) See Ascariasis – Round worm (Ascaris lumbricoides)
RSV – Respiratory syncytial virus
Rubella – Acquired
Rubella – Exposed Susceptible Contact
Rubeola – Measles - Known Case See Measles – (Rubeola) – Known Case
Rubeola – (Measles) Exposed Susceptible Contact See Measles – (Rubeola) – Exposed Susceptible Contact
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
204
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Rabies
Clinical Presentation
Acute encephalomyelitis
Infectious Substances
How it is Transmitted
Saliva of infected animals
Not person-to-person transmission
Acquired from saliva or bite of infected animals
Corneal, tissue and organ transplantation
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Highly variable, 5 days to several months
Not person-to-person transmission
Comments
•
Notify Zone Medical Officer of Health of case by fastest means possible.
•
Refer to existing policy re: care of body after death
•
Post-exposure prophylaxis is recommended for percutaneous or mucosal contamination with saliva
of rabid animal
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
205
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Rash, compatible with scabies – (Ectoparasite)
Clinical Presentation
Lesions in skin fold, severe itching, dermatitis, scaling
Infectious Substances
How it is Transmitted
Mite
Direct Contact
Indirect Contact
Precautions Needed*
Contact Precautions
Duration of Precautions
If scabies confirmed, until 24 hours of effective therapy has been received
Incubation Period
Period of Communicability
If scabies:
If scabies: Until mites and eggs are destroyed by
treatment, usually after 1 or 2 courses of treatment,
one week apart.
Initial infestation: 4 – 6 weeks
Reinfestation: 1 – 4 days after re-exposure
Comments
*Precautions required are in addition to Routine Practices
If scabies:
•
Apply scabicide as directed on label.
•
Wash clothing and bedding in hot water, dry-clean or seal in plastic bag for 1 week. Close contacts
should be treated if confirmed; consult IPC or Zone Medical Officer of Health (MOH) or designate as
needed.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
206
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Rash, maculopapular – (Suspected Rubeola virus [Measles])
Clinical Presentation
Fever and one of coryza, maculopapular skin rash, conjunctivitis, cough
Infectious Substances
How it is Transmitted
Respiratory secretions
Airborne
Precautions Needed*
Airborne Precautions
Duration of Precautions
If measles confirmed, until 4 days after start of rash in immunocompetent residents or until all symptoms
have resolved in immunocompromised residents.
Incubation Period
Period of Communicability
7 – 18 days
If measles confirmed, 5 days before start of rash (1 –
2 days before start of other symptoms) and until 4
days after onset of rash (longer in
immunocompromised residents)
Comments
*Precautions required are in addition to Routine Practices
•
If measles confirmed: See Measles – (Rubeola) – Known Case
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
207
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Rash, petechial or purpuric – (Suspected Neisseria meningitidis)
Clinical Presentation
Rash (petechial/purpuric) with fever
Infectious Substances
How it is Transmitted
Respiratory secretions
Large Droplets
Direct Contact
Precautions Needed*
Droplet Precautions if N. meningitidis suspected, otherwise Routine Practices
Duration of Precautions
Discontinue if N. meningitidis ruled out, otherwise maintain until 24 hours of effective antimicrobial
therapy has been received.
Incubation Period
Period of Communicability
If N. meningitides: Usually 2 – 10 days
If N. meningitides: Until 24 hours of effective
antimicrobial therapy has been received
Comments
*Precautions required are in addition to Routine Practices
•
If Neisseria meningitidis confirmed: See Neisseria meningitidis
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
208
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Rash, vesicular – (Suspected Varicella virus - Chickenpox)
Clinical Presentation
Fever, vesicular rash
Infectious Substances
How it is Transmitted
Respiratory secretions
Airborne
Lesion drainage
Direct Contact
Indirect Contact
Precautions Needed*
Airborne and Contact Precautions
Duration of Precautions
If Chickenpox is confirmed: until all lesions have crusted and dried.
Incubation Period
Period of Communicability
See Chickenpox
See Chickenpox
Comments
*Precautions required are in addition to Routine Practices
•
If Chickenpox confirmed: See Chickenpox - Known Case (Varicella zoster virus)
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
209
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Rat-bite fever – (Streptobacillus moniliformis; Spirillum minus)
Clinical Presentation
Fever, arthralgia
Infectious Substances
How it is Transmitted
Saliva of infected rodents
Not person-to-person transmission
Contaminated milk
Acquired from saliva or bite of infected animals or
ingestion of contaminated milk
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
3 – 10 days for Streptobacillus moniliformis
Not person-to-person transmission
7 – 21 days for Spirillum minus
Comments
•
Streptobacillus moniliformis: acquired from rats and other animals, contaminated milk
•
Spirillum minus: acquired from rats, mice only
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
210
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Relapsing fever (Borrelia sp.)
Clinical Presentation
Fever comes (2 – 7 days duration) and goes (4 – 14 days), transitory petechial rashes
Infectious Substances
How it is Transmitted
Louse, ticks
Not person-to-person transmission
Acquired by bite of louse or ticks
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
2 – 18 days
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
211
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Rhinovirus
Clinical Presentation
Respiratory tract infection, common cold
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Indirect Contact
Large Droplets
Precautions Needed*
Droplet and Contact Precautions
Duration of Precautions
Until symptoms have resolved
For immunocompromised hosts (i.e. oncology, transplant residents), isolation precautions need to be
maintained for a longer duration due to prolonged viral shedding. Contact IPC or Zone Medical Officer
of Health (MOH) or designate for discontinuation of precautions.
Incubation Period
Period of Communicability
2 – 3 days
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
•
May cohort individuals infected with the same virus.
•
Resident should not share room with high-risk roommates (e.g. immunosuppressed).
•
Refer to the AHS Guidelines for Outbreak Prevention, Control and Management in Acute Care and
Facility Living Sites, OR the AHS Guidelines for Outbreak Prevention, Control and Management in
Supportive Living and Home Living Sites.
If the respiratory viral panel test has a combined Enterovirus-Rhinovirus positive result; manage as
for Rhinovirus.
•
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
212
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Rickettsialpox (Rickettsia akari)
Clinical Presentation
Fever, rash
Infectious Substances
How it is Transmitted
Mouse mite
Not person-to-person transmission
Acquired by bite of mouse mite
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
9 – 14 days
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
213
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Ringworm (Tinea) – (Trichophyton sp., Microsporum sp.,
Epidermophyton sp.)
Clinical Presentation
Ringworm(skin, beard, scalp, groin, perineal region); athletes foot; pityriasis versicolor
Infectious Substances
How it is Transmitted
Organism in skin or hair
Direct or indirect contact with skin or scalp lesions of
infected people/animals; or with shared brushes,
combs, barber clippers, clothing, hats, shower stalls,
contaminated floors and other articles used by
infected people
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
4 – 10 days
While lesion(s) are present
Comments
•
While under treatment for Trichophyton, resident should be excluded from swimming pools and
activities likely to lead to exposure of others.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
214
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Ritter’s Disease – Staphylococcal scalded skin syndrome (SSSS)
See Scalded skin syndrome – Ritter’s Disease (Staphylococcus aureus)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
215
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Rocky Mountain Spotted Fever (Rickettsia rickettsii)
Clinical Presentation
Fever, petechial rash, encephalitis
Infectious Substances
How it is Transmitted
Tick
Not person-to-person transmission, except rarely
through transfusion
Acquired by bite of infected tick
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
2 – 14 days
Not person-to-person transmission except rarely
through transfusion
Comments
•
Infection in humans is incidental and is acquired most frequently during blood feeding by the infected
tick, rarely through transfusion.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
216
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Roseola infantum – Human herpes virus 6
Clinical Presentation
Rash, fever
Infectious Substances
How it is Transmitted
Saliva (presumed)
Direct contact
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
9 – 10 days
Unknown
Comments
•
Transmission requires close direct personal contact
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
217
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Rotavirus
Clinical Presentation
Fever, Vomitting, Diarrhea
Infectious Substances
How it is Transmitted
Feces
Direct Contact (fecal/oral)
Indirect Contact (fecal/oral)
Precautions Needed*
Contact Precautions
Duration of Precautions
Until symptoms have resolved
Incubation Period
Period of Communicability
1 – 3 days
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
•
Symptomatic residents must not participate in food handling activities.
•
Prolonged fecal shedding may occur in immunocompromised residents after diarrhea has ceased;
Contact Precautions should be maintained until laboratory results are negative.
•
For outbreaks: Refer to the AHS Guidelines for Outbreak Prevention, Control and Management in
Acute Care and Facility Living Sites, OR the AHS Guidelines for Outbreak Prevention, Control and
Management in Supportive Living and Home Living Sites
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
218
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Roundworm – Ascariasis (Ascaris spp.)
See Ascariasis – Roundworm (Ascaris lumbricoides)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
219
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
RSV – Respiratory syncytial virus
Clinical Presentation
Respiratory tract infection
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Indirect Contact
Large Droplets
Precautions Needed*
Droplet and Contact Precautions
Duration of Precautions
Until symptoms have resolved
For immunocompromised hosts (i.e. oncology, transplant residents), isolation precautions need to be
maintained for a longer duration due to prolonged viral shedding. Contact IPC or Zone Medical Officer
of Health (MOH) or designate for discontinuation of precautions.
Incubation Period
Period of Communicability
2 – 8 days
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
•
May cohort with others of same confirmed virus. Minimize exposure of immunocompromised
residents.
•
For outbreaks: Refer to the AHS Guidelines for Outbreak Prevention, Control and Management in
Acute Care and Facility Living Sites, OR the AHS Guidelines for Outbreak Prevention, Control and
Management in Supportive Living and Home Living Sites
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
220
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Rubella virus: German measles – Acquired
Clinical Presentation
Fever, maculopapular rash
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Large Droplets
Precautions Needed*
Droplet Precautions
Duration of Precautions
Until 7 days after onset of rash
Incubation Period
Period of Communicability
14 – 21 days
One week before to 7 days after onset of rash, can be
contagious up to 14 days after rash appears
Comments
*Precautions required are in addition to Routine Practices
•
Defer non-urgent admission if rubella is present. May admit after rash has resolved.
•
Only immune HCWs, caretakers and visitors should enter the room. If it is essential for a nonimmune person to enter the room, a procedure mask must be worn.
•
If immunity is unknown, assume person is non-immune
•
Pregnant staff should not care for residents with rubella, regardless of their immune status.
•
Droplet Precautions should be maintained for exposed susceptible residents for 7 days after first
contact through to 21 days after last contact.
•
Refer exposed susceptible non-pregnant persons to facility’s workplace health and safety or to Zone
Medical Officer of Health or designate for vaccine administration within 3 days of exposure
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
221
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Rubella virus (German measles) - Exposed Susceptible Contact
Clinical Presentation
Susceptible contact. Asymptomatic - may develop Rubella
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Large Droplets
Precautions Needed*
Droplet Precautions
Duration of Precautions
Droplet Precautions should be maintained for exposed susceptible residents for 7 days after first
contact through to 21 days after last contact.
If rubella rash develops: Until 7 days after onset of rash
Incubation Period
Period of Communicability
14 – 21 days
One week before to 7 days after onset of rash; can be
contagious up to 14 days after rash appears
Comments
*Precautions required are in addition to Routine Practices
•
Defer non-urgent admission if a non-immune person is incubating the disease.
•
Only immune HCWs, caretakers and visitors should enter the room. If it is essential for a nonimmune person to enter the room, a procedure mask must be worn.
•
If immunity is unknown, assume person is non-immune
•
Pregnant staff should not care for residents with rubella, regardless of their immune status.
•
Refer exposed susceptible non-pregnant persons to facility’s workplace health and safety or to Zone
Medical Officer of Health for vaccine administration within 3 days of exposure
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
222
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Rubeola – (Measles) – Known Case
See Measles – (Rubeola) – Known Case
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
223
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Rubeola – (Measles) - Exposed Susceptible Contact
See Measles – (Rubeola) – Exposed Susceptible Contact
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
224
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
S
Salmonella (Salmonella sp.)
Salmonella spp. (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing)
SARS – (Severe Acute Respiratory Syndrome; Coronavirus) See Coronavirus – Severe Acute Respiratory Syndrome
(SARS-CoV), Middle Eastern Respiratory Syndrome (MERS-CoV)
Scabies (Sarcoptes scabiei)
Scalded skin syndrome – (Staphylococcus aureus)
Scarlet Fever –Streptococcus pyogenes [Group A] See Streptococcus [Group A] (Streptococcus pyogenes) – Scarlet
Fever, Pharyngitis
Schistosomiasis (Schistosoma sp.)
Septic arthritis – (Haemophilus influenza type B [HIB] [possible in non-immune child <5 years of age], Streptococcus
[Group A], Staphylococcus aureus, many other bacteria)
Serratia spp. (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing) See
Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing)
Shigella (Shigella sp.)
Shingles: (Herpes zoster) Varicella zoster virus – Disseminated
Shingles: (Herpes zoster) Varicella zoster virus –Exposed Susceptible Contact
Shingles: (Herpes zoster) Varicella zoster virus – Immunocompromised Host WITH Localized Lesions(1 or 2
dermatomes)
Shingles: (Herpes zoster) Varicella zoster virus – Normal Host With Localized Lesions(1 or 2 dermatomes) AND
lesions that CAN be covered with dressings or clothing
Shingles: (Herpes zoster) Varicella zoster virus – Normal Host With Localized Lesions (1 or 2 dermatomes) AND
lesions that CANNOT be covered with dressings or clothing
Skin Infection – (Staphylococcus aureus, Streptococcus [Group A], many other bacteria) See Cellulitis –
(Staphylococcus aureus, Streptococcus [Group A], many other bacteria)
Smallpox (Variola major virus, Variola minor virus)
Sporotrichosis (Sporothrix schenckii)
Staphylococcus aureus – MRSA See Methicillin Resistant Staphylococcus aureus (MRSA)
Staphylococcus aureus – pneumonia (not MRSA)
Staphylococcus aureus – skin infection (not MRSA)
Staphylococcus aureus – toxic shock syndrome
Stenotrophomonas maltophilia
Streptococcus, [Group A] (Streptococcus pyogenes) – Invasive
Streptococcus, [Group A] (Streptococcus pyogenes) – Scarlet fever, pharyngitis
Streptococcus, [Group A] (Streptococcus pyogenes) Skin Infection
Streptococcus pneumoniae
Stronglyoidiasis (Stronglyoides stercoralis)
Syphilis (Treponema pallidum)
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
225
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Salmonella (Salmonella sp.)
Clinical Presentation
Diarrhea, enteric fever, typhoid fever, food poisoning
Infectious Substances
How it is Transmitted
Feces
Direct Contact (fecal/oral)
Indirect Contact (fecal/oral)
Foodborne
Precautions Needed*
Adults: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions
Duration of Precautions
Until symptoms have resolved and stools are normal
Incubation Period
Period of Communicability
6 – 72 hours for diarrhea; 3 – 60 days for enteric
fever
Variable
Comments
*Precautions required are in addition to Routine Practices
•
Symptomatic residents must not participate in food handling activities.
•
For Salmonella spp. (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C producing)
also see Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE]; ESBL or Amp-C
producing)
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
226
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Salmonella spp. (Multi-Drug Resistant; Carbapenem resistant
[CRE]; ESBL or Amp-C producing)
E. coli, Klebsiella spp., Serratia spp., Providencia spp., Proteus spp., Citrobacter spp.,
Enterobacter spp., Morganella spp., Salmonella spp., Hafnia spp.
See Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE];
ESBL or Amp-C producing
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
227
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
SARS – (Severe Acute Respiratory Syndrome; Coronavirus)
See Coronavirus – Severe Acute Respiratory Syndrome (SARS-CoV), Middle
Eastern Respiratory Syndrome (MERS-CoV)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
228
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Scabies (Sarcoptes scabiei)
Clinical Presentation
Lesions in skin fold, severe itching, dermatitis, scaling
Infectious Substances
How it is Transmitted
Mite
Direct Contact
Indirect Contact
Precautions Needed*
Contact Precautions
Duration of Precautions
Until 24 hours of effective therapy has been received
Incubation Period
Period of Communicability
Initial infestation: 2 – 6 weeks
Until mites and eggs are destroyed by treatment,
usually after 1 or 2 courses of treatment, one week
apart.
Re-infestation: 1 – 4 days after re-exposure
Comments
*Precautions required are in addition to Routine Practices
•
Apply scabicide as directed on label.
•
Wash clothes and bedding in hot water, dry clean or seal in a plastic bag and store for 1 week.
•
Close contacts should be treated if confirmed; consult IPC or Zone Medical Officer of Health (MOH)
or designate as needed.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
229
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Scalded skin syndrome – Ritter’s Disease (Staphylococcus
aureus)
Clinical Presentation
Painful, rash with thick white/brown flakes
Infectious Substances
How it is Transmitted
Skin exudates/drainage
Direct Contact
Indirect Contact
Precautions Needed*
Major drainage not contained: Contact Precautions
Minor drainage contained: Routine Practices
Duration of Precautions
Until drainage has resolved or can be contained
Incubation Period
Period of Communicability
Variable
While organism is present in drainage
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
230
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Scarlet Fever –Streptococcus pyogenes [Group A]
See Streptococcus [Group A] (Streptococcus pyogenes) – Scarlet Fever,
Pharyngitis
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
231
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Schistosomiasis (Schistosoma sp.)
Clinical Presentation
Diarrhea, fever, itchy rash, Hepatosplenomegaly, hematuria
Infectious Substances
How it is Transmitted
Larvae in contaminated water
Not person-to-person transmission
Acquired by contact with larvae in contaminated
water
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Unknown
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
232
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Septic arthritis – (Haemophilus influenza type B [HIB] [possible in
non-immune child <5 years of age], Streptococcus [Group A],
Staphylococcus aureus, many other bacteria)
Clinical Presentation
Inability to move the limb with the infected joint (pseudoparalysis), intense joint pain, joint swelling, joint
redness, low fever
Infectious Substances
How it is Transmitted
Respiratory secretions if HIB
Direct Contact if HIB
Large droplets if HIB
Precautions Needed*
Adults: Routine Practices
Children: Droplet Precautions if HIB, otherwise Routine Practices
Duration of Precautions
If HIB: Until 24 hours of effective antimicrobial therapy has been received
Incubation Period
Period of Communicability
Not applicable
Not applicable
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
233
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Serratia spp. (Multi-Drug Resistant; Carbapenem resistant [CRE];
ESBL or Amp-C producing)
E. coli, Klebsiella spp., Serratia spp., Providencia spp., Proteus spp., Citrobacter spp.,
Enterobacter spp., Morganella spp., Salmonella spp., Hafnia spp.
See Enterobacteriaceae (Multi-Drug Resistant; Carbapenem resistant [CRE];
ESBL or Amp-C producing)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
234
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Shigella (Shigella sp.)
Clinical Presentation
Diarrhea
Infectious Substances
How it is Transmitted
Feces
Direct Contact (fecal/oral)
Indirect Contact (fecal/oral)
Precautions Needed*
Adults: Routine Practices
For incontinent residents if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Children: Contact Precautions
Duration of Precautions
Until symptoms have resolved and stools are normal
Incubation Period
Period of Communicability
1 – 3 days
Usually 4 weeks unless treated
Comments
*Precautions required are in addition to Routine Practices
•
Symptomatic residents must not participate in food handling activities
•
Treatment with effective antibiotic shortens period of infectivity
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
235
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Shingles: (Herpes zoster) Varicella zoster virus – Disseminated
Clinical Presentation
Vesicular lesions that involve multiple areas (more than 2 dermatomes) with possible visceral
complications. Refer to Dermatome Chart
Infectious Substances
How it is Transmitted
Vesicular fluid
Respiratory secretions
Airborne
Direct Contact
Indirect Contact (articles freshly soiled by drainage
from lesions)*
Precautions Needed*
Airborne and Contact Precautions
Duration of Precautions
Until all lesions have crusted and dried
Incubation Period
Period of Communicability
Not applicable
Until all lesions have crusted and dried
Comments
*Precautions required are in addition to Routine Practices
• Individuals with known immunity to chicken pox (history of past illness or vaccination with 2
appropriately timed doses of varicella vaccine) are not required to wear the N95 respirator when
entering the room.
• Susceptible HCWs should not enter the room if immune staff are available. If they must enter the
room, an N95 respirator must be worn. Other non-immune persons should not enter except in urgent
or compassionate circumstances
• If immunity is unknown, assume person is non-immune
• Susceptible high-risk contacts should be given VZIG as soon as possible within 96 hours of
exposure. Consult Zone Medical Officer of Health or designate for advice.
• For susceptible contacts, Airborne Precautions should begin 8 days after first exposure to rash and
continue until 21 days after last exposure (28 days if VZIG given).
Discharge Settle Time
Non-negative pressure rooms:
• Do not admit a new resident into this room for at least 4 hours. If staff must enter room before 4
hours and non-immune to chicken pox, wear an N95 respirator.
Negative pressure rooms:
• Do not admit a new resident into this room for at least 45 minutes. If staff must enter room before 45
minutes, and non-immune to chicken pox wear an N95 respirator
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
236
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Shingles: (Herpes zoster) Varicella zoster virus – Exposed
Susceptible Contact**
Clinical Presentation
**Susceptible contact with exposure to a person with a case of disseminated shingles or to an
immunocompromised person with localized shingles. Asymptomatic. May develop chicken pox***
Infectious Substances
How it is Transmitted
If chicken pox lesions develop then lesion
drainage, respiratory secretions
Airborne
Direct Contact
Indirect Contact (articles
freshly soiled by drainage from lesions)*
Precautions Needed*
8 days after first contact and until 21 days after last contact with person with active disease (or 28 days if
given ZVIG): Airborne Precautions. If chickenpox lesions develop: Airborne and Contact Precautions
Duration of Precautions
From 8 days after first contact until 21 days after last contact (or 28 days if given VZIG).
If chicken pox develops – If treated: Until 72 hours of effective anti-viral treatment has been received AND
no new lesions AND Existing lesions have crusted and dried. If untreated, Until all lesions have crusted and
dried
Incubation Period
Period of Communicability
10 – 21 days
2 days before rash starts and until all skin lesion have
crusted and dried
Comments
*Precautions required are in addition to Routine Practices
• ***Exposure to shingles does not cause shingles. However, a person who has never had chicken pox or
was never vaccinated for chicken pox may develop chickenpox if the shingles vesicle fluid comes into
contact with their mucous membranes. In the immunocompromised person and persons with
disseminated shingles the virus may also be spread by the airborne route.
• Susceptible high-risk contacts should receive varicella zoster immunoglobulin as soon as possible, latest
within 96 hours of exposure. Consult Zone Medical Officer of Health or designate for advice
• Individuals with known immunity to chicken pox (history of past illness or vaccination with 2
appropriately timed doses of varicella vaccine) are not required to wear the N95 respirator when entering
the room.
• Susceptible HCWs should not enter the room if immune staff are available. If they must enter the room,
an N95 respirator must be worn. Other non-immune persons should not enter except in urgent or
compassionate circumstances. If immunity is unknown, assume person is non-immune
Discharge Settle Time
• Non-negative pressure rooms: Do not admit a new resident into this room for at least 4 hours. If staff
must enter room before 4 hours and non-immune to chicken pox, wear an N95 respirator.
• Negative pressure rooms: Do not admit a new resident into this room for at least 45 minutes. If staff must
enter room before 45 minutes, and non-immune to chicken pox, wear an N95 respirator.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
237
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Shingles: (Herpes zoster) Varicella zoster virus –
Immunocompromised Host With Localized Lesions (1 or 2
dermatomes)
Clinical Presentation
Vesicular lesions in a dermatomal distribution. Refer to Dermatome Chart
Infectious Substances
How it is Transmitted
Vesicular fluid, possibly respiratory secretions
Airborne
Direct Contact
Indirect Contact
(articles freshly soiled by drainage from lesions)*
Precautions Needed*
Airborne and Contact Precautions
Duration of Precautions
Until 24 hours of effective antimicrobial therapy has been received; then as for localized zoster in normal
host.
Incubation Period
Period of Communicability
Not applicable
Until all lesions have crusted and dried
Comments
*Precautions required are in addition to Routine Practices
• Individuals with known immunity to chicken pox (history of past illness or vaccination with 2
appropriately timed doses of varicella vaccine) are not required to wear the N95 respirator when
entering the room.
• Susceptible HCWs should not enter the room if immune staff are available. If they must enter the
room, an N95 respirator must be worn. Other non-immune persons should not enter except in urgent
or compassionate circumstances
• If immunity is unknown, assume person is non-immune
• Susceptible high-risk contacts should be given VZIG as soon as possible within 96 hours of
exposure. Consult Zone Medical Officer of Health or designate for advice.
• For susceptible contacts, Airborne Precautions* should begin 8 days after first exposure to rash
and continue until 21 days after last exposure (28 days if VZIG given).
Discharge Settle Time
Non-negative pressure rooms:
• Do not admit a new resident into this room for at least 4 hours. If staff must enter room before 4
hours and non-immune to chicken pox, wear an N95 respirator.
Negative pressure rooms:
• Do not admit a new resident into this room for at least 45 minutes. If staff must enter room before 45
minutes, and non-immune to chicken pox wear an N95 respirator
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
238
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Shingles: (Herpes zoster) Varicella zoster virus – Normal Host
With Localized Lesions (1 or 2 dermatomes) AND lesions that CAN
be covered with dressings or clothing
Clinical Presentation
Vesicular lesions in a dermatomal distribution. Refer to Dermatome Chart
Infectious Substances
How it is Transmitted
Vesicular fluid
Direct Contact
Indirect Contact (articles freshly soiled by drainage
from lesions)*
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Not applicable
Until all lesions have crusted and dried
Comments
*Exercise care when handling dressings, clothing or other materials that may be contaminated with
vesicular fluid
•
Consider Contact Precautions in addition to Routine Practices for cases of extensive localized
zoster that cannot be covered.
•
Consider Airborne and Contact Precautions in addition to Routine Practices for cases of
extensive localized zoster that cannot be covered and in situations where there are varicella
susceptible residents.
•
HCWs, roommates and caregivers should be immune to chickenpox
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
239
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Shingles: (Herpes zoster) Varicella zoster virus – Normal Host
With Localized Lesions (1 or 2 dermatomes) AND lesions that
CANNOT be covered with dressings or clothing
Clinical Presentation
Vesicular lesions in a dermatomal distribution. Refer to Dermatome Chart
Infectious Substances
How it is Transmitted
Vesicular fluid
Direct contact
Indirect contact (articles freshly soiled by drainage
from lesions)**
Precautions Needed*
Contact Precautions
Duration of Precautions
Until all lesions have crusted and dried
Incubation Period
Period of Communicability
Variable
Until all lesions have crusted and dried
Comments
*Precautions required are in addition to Routine Practices
**Exercise care when handling materials that may be contaminated with vesicular fluid
•
Consider Airborne and Contact Precautions* for cases of extensive localized zoster that cannot be
covered and in situations where there are varicella susceptible residents.
•
HCWs, roommates and caregivers should be immune to chickenpox.
•
Non-immune persons should not enter except in urgent or compassionate circumstances. If immunity
is unknown, assume person is non-immune.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
240
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Skin Infection – (Staphylococcus aureus, Streptococcus [Group
A], many other bacteria)
See Cellulitis – (Staphylococcus aureus, Streptococcus [Group A], many
other bacteria)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
241
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Smallpox (Variola major virus, Variola minor virus)
Clinical Presentation
Fever, vesicular/pustule in appropriate epidemiological context
Infectious Substances
How it is Transmitted
Skin lesion exudate
Oropharyngeal secretions
Airborne
Direct Contact
Indirect Contact
Precautions Needed*
Airborne Precautions and Droplet and Contact Precautions
Duration of Precautions
Until all scabs have crusted and separated (3 – 4 weeks)
Incubation Period
Period of Communicability
7 – 17 days
From onset of mucosal lesions until all skin lesions
have crusted and separated
Comments
*Precautions required are in addition to Routine Practices
•
•
•
•
•
•
May be Bioterrorism related
Notify Zone Medical Officer of Health of case by fastest means possible.
Refer to your facility’s policy for care of body after death.
See Public Health Act – Bodies of Deceased Persons Regulation
Immunization of health care workers (HCWs) was stopped in 1977. Care preferably should be
provided by immune HCWs; non-vaccinated HCWs should not provide care if immune HCWs are
available.
N95 respirator required for all staff regardless of vaccination status
Discharge Settle Time
Non-negative pressure rooms:
• Do not admit a new resident into this room for at least 4 hours. If staff must enter room before 4
hours and non-immune to chicken pox, wear an N95 respirator.
Negative pressure rooms:
• Do not admit a new resident into this room for at least 45 minutes. If staff must enter room before 45
minutes, and non-immune to chicken pox wear an N95 respirator
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
242
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Sporotrichosis (Sporothrix schenckii)
Clinical Presentation
Skin lesions
Infectious Substances
How it is Transmitted
Spores in contaminated soil, on vegetation
Not person-to-person transmission
Acquired from spores in soil or vegetation
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Variable
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
243
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Staphylococcus aureus – MRSA
See Methicillin Resistant Staphylococcus aureus (MRSA)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
244
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Staphylococcus aureus – pneumonia (not MRSA)
Clinical Presentation
Pneumonia
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Indirect Contact
Large Droplets
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Variable
Variable
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
245
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Staphylococcus aureus – skin infection (not MRSA)
Clinical Presentation
Wound or burn infections, skin infection, furuncles, impetigo, scalded skin syndrome
Infectious Substances
How it is Transmitted
Skin exudates and drainage
Direct contact
Indirect contact
Precautions Needed*
Major drainage not contained: Contact Precautions
Minor drainage contained: Routine Practices
Duration of Precautions
Until drainage has resolved or can be contained
Incubation Period
Period of Communicability
Variable
While organism present in drainage
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
246
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Staphylococcus aureus – toxic shock syndrome
Clinical Presentation
High fever, diffuse macular rash, hypotension, multisystem organ involvement
Infectious Substances
How it is Transmitted
Skin exudates and drainage if wounds or skin
lesions present
Direct Contact
Indirect Contact
Precautions Needed*
If draining wounds or lesions present:
Major drainage not contained: Contact Precautions
Minor drainage contained: Routine Practices
Duration of Precautions
Until drainage has resolved or can be contained
Incubation Period
Period of Communicability
Variable
Variable
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
247
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Stenotrophomonas maltophilia
Clinical Presentation
Colonization or infection of respiratory tract
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Indirect Contact
Precautions Needed*
Routine Practices
Contact Precautions for residents with tracheostomies who share a room with residents who are
ventilated or with tracheostomies
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Unknown
While organism is in respiratory secretions
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
248
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Streptococcus [Group A] (Streptococcus pyogenes) – Invasive
disease – iGAS, Toxic Shock
Clinical Presentation
Toxic shock, invasive disease including: necrotizing fasciitis, myositis, meningitis, pneumonia.
Infectious Substances
How it is Transmitted
Respiratory secretions
Direct Contact
Infected body fluids
Indirect Contact
Wound drainage
Large Droplets
Precautions Needed*
Droplet and Contact Precautions
Duration of Precautions
Until 24 hours of effective antimicrobial therapy has been received
Incubation Period
Period of Communicability
Variable
While organism in respiratory secretions, infected
body fluids or wound drainage
Comments
*Precautions required are in addition to Routine Practices
•
•
•
•
Notify Zone Medical Officer of Health of case by fastest means possible
Refer to your facility’s policy for care of body after death.
See Public Health Act – Bodies of Deceased Persons Regulation
Close contacts of invasive disease may require prophylaxis
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
249
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Streptococcus [Group A] (Streptococcus pyogenes) – Scarlet
Fever, Pharyngitis
Clinical Presentation
Scarlet fever, Pharyngitis
Infectious Substances
How it is Transmitted
Respiratory secretions
Large Droplets
Precautions Needed*
Adults: Routine Practices
Children: Droplet and Contact Precautions
Duration of Precautions
Children: Until 24 hours of effective antimicrobial therapy has been received
Incubation Period
Period of Communicability
2 – 5 days
While organism in respiratory secretions, 10 – 21
days if not treated
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
250
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Streptococcus [Group A] – (Streptococcus pyogenes) Skin
Infection
Clinical Presentation
Erysipelas, wound or burn infection, skin infection, impetigo, cellulitis.
Infectious Substances
How it is Transmitted
Drainage, skin exudates
Direct Contact
Indirect Contact
Precautions Needed*
Major drainage not contained: Contact Precautions**
Minor drainage contained: Routine Practices
Duration of Precautions
Until 24 hours of effective antimicrobial therapy has been received and drainage has resolved or can be
contained
Incubation Period
Period of Communicability
Variable
As long as organism is in the exudates or drainage
Comments
*Precautions required are in addition to Routine Practices
** Droplet and Contact Precautions until 24 hours of effective antimicrobial therapy has been received
If invasive group A streptococcal infection suspected
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
251
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Streptococcus pneumoniae
Clinical Presentation
Pneumonia, meningitis, bacteremia, epiglottitis,
Infectious Substances
How it is Transmitted
Respiratory secretions
Large Droplets
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Unknown, infection is thought to be preceded by
asymptomatic colonization
As long as sufficient numbers of pneumococci are in
respiratory secretions
Comments
•
Streptococcus pneumoniae is commonly found in the upper respiratory tract of healthy people and is
the most common bacterial cause of community-acquired pneumonia among all ages
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
252
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Stronglyoidiasis (Stronglyoides stercoralis)
Clinical Presentation
Usually asymptomatic
Infectious Substances
How it is Transmitted
Larvae in feces
Penetration of skin by larvae in soil*
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Unknown
Rarely person-to-person transmission
Comments
*Although usual route of transmission is through skin contact of contaminated soil, fecal/oral
transmission can occur. May cause disseminated disease in immunocompromised resident.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
253
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Syphilis (Treponema pallidum)
Clinical Presentation
Genital, skin or mucosal lesions, disseminated disease, neurological or cardiac disease, latent infection
Infectious Substances
How it is Transmitted
Genital secretions
Mom to newborn or fetus
Lesion exudates
Sexual contact
Direct contact with infectious exudates or lesions
Precautions Needed*
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
10 – 90 days
When moist mucocutaneous lesions of primary and
secondary syphilis are present
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
254
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
T
Tapeworm (Taenia saginata, Taenia solium, Diphyllobothrium latum, Hymenolepsis nana)
Tetanus (Clostridium tetani)
Tinea (Ringworm) – (Trichophyton sp., Microsporum sp., Epidermophyton sp., Malazzezia sp.) See Ringworm (Tinea)
– (Trichophyton sp., Microsporum sp., Epidermophyton sp., Malassezia furfur)
Toxic shock syndrome – (Streptococcus pyogenes [Group A], Staphylococcus aureus)
Toxocariasis (Toxocara canis, Toxocara cati)
Toxoplasmosis (Toxoplasma gondii)
Trachoma (Chlamydia trachomatis) See Chlamydia (Chlamydia trachomatis)
Trench Fever (Bartonella quintana)
Trichinosis (Trichinella spiralis)
Trichomoniasis (Trichomonas vaginalis)
Trichuriasis – Whipworm (Trichuris trichiura)
Tuberculosis – non-respiratory or extrapulmonary (Mycobacterium tuberculosis) See Mycobacterium tuberculosis
(TB) – extrapulmonary disease or not respiratory
Tuberculosis – respiratory or pulmonary (Mycobacterium tuberculosis) See Mycobacterium tuberculosis (TB) –
respiratory or pulmonary disease;
Tularemia (Francisella tularenis)
Typhoid or Paratyphoid fever (Salmonella typhi, Salmonella paratyphi) See Salmonella (Salmonella sp.)
Typhus fever (Rickettsia typhi, Rickettsia prowazekii)
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
255
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Tapeworm (Taenia saginata, Taenia solium, Diphyllobothrium
latum, Hymenolepsis nana)
Clinical Presentation
Usually asymptomatic
Infectious Substances
How it is Transmitted
Ova in feces
Direct Contact with infected feces (fecal/oral)
Larvae in food
Foodborne (Consumption of larvae in raw or
undercooked beef, pork or raw fish)
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Variable when foodborne, 2 – 4 weeks if contact
with feces
T. saginata is not direct person-to-person
transmission, however T. solium can be. Eggs may
be viable in the environment for months.
Comments
•
Larvae develop into adult tapeworms in gastrointestinal tract
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
256
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Tetanus (Clostridium tetani)
Clinical Presentation
Tetanus
Infectious Substances
How it is Transmitted
Spores in soil
Not person-to-person transmission.
Fomites contaminated with animal and human
feces
Tetanus spores are usually introduced through a
puncture wound contaminated with soil or feces.
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
2 days to 2 months
No person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
257
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Tinea (Ringworm) – (Trichophyton sp., Microsporum sp.,
Epidermophyton sp., Malassezia sp.)
See Ringworm (Tinea) – (Trichophyton sp., Microsporum sp.,
Epidermophyton sp., Malassezia furfur)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
258
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Toxic shock syndrome – (Streptococcus pyogenes [Group A],
Staphylococcus aureus)
Clinical Presentation
Toxic shock syndrome
Infectious Substances
How it is Transmitted
Wound drainage (if wound or skin lesions
present)
Direct Contact
Indirect Contact
Precautions Needed
See specific organism
Duration of Precautions
Dependent on organism
Incubation Period
Period of Communicability
Variable
Variable
Comments
•
Notify Zone Medical Officer of Health of case by fastest means possible.
•
Close contacts of invasive disease may require prophylaxis
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
259
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Toxocariasis (Toxocara canis, Toxocara cati)
Clinical Presentation
Fever, wheeze, rash, eosinophilia
Infectious Substances
How it is Transmitted
Ova in dog or cat feces
Not person-to-person transmission
Acquired from contact with infected dogs, cats
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Unknown
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
260
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Toxoplasmosis (Toxoplasma gondii)
Clinical Presentation
Asymptomatic or fever, lymphadenopathy, retinitis, encephalitis in immunocompromised host, congenital
infection
Infectious Substances
How it is Transmitted
Oocysts in cat feces, contaminated soil
Acquired by contact with infected cat feces or soil
contaminated by cats, consumption of raw meat,
contaminated raw vegetables or contaminated water
Intrauterine transmission from mother-to-fetus
Transplantation of stem cells or organs
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
5 – 23 days
Not person-to-person transmission except mother to
fetus.
Oocysts shed by cats become infective 1 – 5 days
later and can remain viable in the soil for a year.
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
261
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Trachoma (Chlamydia trachomatis)
See Chlamydia (Chlamydia trachomatis)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
262
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Trench Fever (Bartonella quintana)
Clinical Presentation
Headache, malaise, pain and tender shins, splenomegaly, rash
Infectious Substances
How it is Transmitted
Organism in feces of human body lice
Vector borne- by inoculation of the organism in louse
feces through a break in the skin
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Not applicable
Not person-to-person transmission in the absence of
lice
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
263
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Trichinosis (Trichinella spiralis)
Clinical Presentation
Fever, rash, diarrhea
Infectious Substances
How it is Transmitted
Organism in infected meat
Not person-to-person transmission
Acquired from consumption of infected meat
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
5 – 45 days
Not person-to-person transmission
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
264
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Trichomoniasis (Trichomonas vaginalis)
Clinical Presentation
Vaginitis, Urethritis
Infectious Substances
How it is Transmitted
Vaginal secretions
Sexual contact
Urethral discharges
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
4 – 28
As long as organism present in secretions
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
265
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Trichuriasis – Whipworm (Trichuris trichiura)
Clinical Presentation
Abdominal pain, diarrhea
Infectious Substances
How it is Transmitted
Ova in soil
Not person-to-person transmission
Acquired from ingestion of contaminated soil or
contaminated vegetables
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Unknown
Not person-to-person transmission
Comments
•
Ova must hatch in soil to be infective.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
266
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Tuberculosis – Extrapulmonary or Not Respiratory
(Mycobacterium tuberculosis)
See Mycobacterium tuberculosis (TB) – extrapulmonary disease or not
respiratory; (also M. africanum, M. bovis, M. caprae, M. microti, M.
pinnipedii)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
267
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Tuberculosis – Respiratory or Pulmonary disease (Mycobacterium
tuberculosis)
See Mycobacterium tuberculosis (TB) – extrapulmonary disease or not
respiratory; (also M. africanum, M. bovis, M. caprae, M. microti, M.
pinnipedii)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
268
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Tularemia (Francisella tularenis)
Clinical Presentation
Fever, lymphadenopathy, pneumonia
Infectious Substances
How it is Transmitted
Organism in infected animals, ticks
Not person-to-person transmission
Acquired from contact with infected animals
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
1 – 14 days
Not person-to-person transmission
Comments
•
May be Bioterrorism related
•
Notify Zone Medical Officer of Health of case by fastest means possible.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
269
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Typhoid or Paratyphoid fever (Salmonella typhi, Salmonella
paratyphi)
See Salmonella (Salmonella sp.)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
270
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Typhus fever (Rickettsia typhi, Rickettsia prowazekii)
Clinical Presentation
Fever, rash
Infectious Substances
How it is Transmitted
Fleas, lice
Not person-to-person transmission
Acquired from bite of fleas or lice
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
6 – 14 days
Not person-to-person transmission
Comments
•
Notify Zone Medical Officer of Health of case by fastest means possible.
•
Refer to your facility’s policy for care of body after death.
•
See Public Health Act – Bodies of Deceased Persons Regulation
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
271
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
U
Urinary tract infection
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
272
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Urinary tract infection
Clinical Presentation
Urinary Tract Infection
Infectious Substances
How it is Transmitted
Many bacteria, viruses, fungi
See specific organism
Precautions Needed*
See specific organism, otherwise: Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Variable
Variable
Comments
*Additional precautions not required unless infection caused by a multi-drug resistant organism or
required by a specific organism
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
273
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
V
Vancomycin-intermediate Staphylococcus aureus (VISA)
Vancomycin-resistant Enterococcus (VRE)
Vancomycin-resistant Staphylococcus aureus (VRSA)
Varicella zoster virus: Chickenpox – Exposed Susceptible Contact See Chickenpox – Exposed Susceptible Contact
(Varicella zoster virus)
Varicella zoster virus: Chickenpox – Known Case See Chickenpox – Known Case (Varicella zoster virus)
Varicella zoster virus: Herpes zoster (Shingles) – Disseminated See Shingles: (Herpes zoster) Varicella zoster virus –
Disseminated
Varicella zoster virus: Herpes zoster (Shingles) – Exposed Susceptible Contact See Shingles: (Herpes zoster)
Varicella zoster virus – Exposed Susceptible Contact
Varicella zoster virus: Herpes zoster (Shingles) – Immunocompromised Host With Localized Lesions(1 or 2
dermatomes) See Shingles: (Herpes zoster) Varicella zoster virus – Immunocompromised Host With Localized
lesions (1 or 2 dermatomes)
Varicella zoster virus: Herpes zoster (Shingles) – Normal Host With Localized Lesions(1 or 2 dermatomes) AND
lesions that CAN be covered with dressings or clothing See Shingles: (Herpes zoster) Varicella zoster virus – Normal
Host With Localized Lesions (1 or 2 dermatomes) AND lesions that CAN be covered with dressings or clothing
Varicella zoster virus: Herpes zoster (Shingles) – Normal Host With Localized Lesions (1 or 2 dermatomes) AND
lesions that CANNOT be covered with dressings or clothing See Shingles: (Herpes zoster) Varicella zoster virus –
Normal Host With Localized Lesions (1 or 2 dermatomes) AND lesions that CANNOT be covered with dressings or
clothing
Vibrio parahaemolyticus Enteritis
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
274
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Vancomycin-intermediate Staphylococcus aureus (VISA)
Clinical Presentation
Colonization or infection of any body site
Infectious Substances
How it is Transmitted
Colonized or infected skin, secretions or
excretions
Direct Contact
Indirect Contact
Large Droplets if symptoms of acute respiratory tract
infection
Precautions Needed*
See Additional Precautions for ARO Positive Residents in Continuing Care information sheet
Duration of Precautions
Residents must be reassessed regularly and as conditions and behaviours change
Additional precautions for ARO positive residents in continuing care may be discontinued when resident
is cooperative with hygiene practices and drainage and body fluids are contained.
If needed, consult IPC or Zone Medical Officer of Health (MOH) or designate for assistance determining
when to discontinue additional precautions for ARO positive resident
Incubation Period
Period of Communicability
Variable
While organism is present in secretions or excretions
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
275
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Vancomycin-resistant Enterococcus (VRE)
Clinical Presentation
Colonization or infection of any body site
Infectious Substances
How it is Transmitted
Colonized or infected skin, secretions or
excretions
Direct Contact
Indirect Contact
Precautions Needed*
See Additional Precautions for ARO Positive Residents in Continuing Care information sheet
Duration of Precautions
Residents must be reassessed regularly and as conditions and behaviours change
Additional precautions for ARO positive residents in continuing care may be discontinued when resident
is cooperative with hygiene practices and drainage and body fluids are contained.
If needed, consult IPC or Zone Medical Officer of Health (MOH) or designate for assistance determining
when to discontinue additional precautions for ARO positive resident
Incubation Period
Period of Communicability
Variable
While organism is present in secretions orexcretions
Comments
*Precautions required are in addition to Routine Practices
•
Enterococcus persists in the environment, ensure thorough cleaning of the resident’s environment
particularly toileting equipment, e.g. commodes, toilet grab rails. Careful discharge cleaning is
required.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
276
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Vancomycin-resistant Staphylococcus aureus (VRSA)
Clinical Presentation
Colonization or infection of any body site
Infectious Substances
How it is Transmitted
Colonized or infected skin, secretions or
excretions
Direct Contact
Indirect Contact
Large Droplets if symptoms of acute respiratory tract
infection
Precautions Needed*
See Additional Precautions for ARO Positive Residents in Continuing Care information sheet
Duration of Precautions
Residents must be reassessed regularly and as conditions and behaviours change
Additional precautions for ARO positive residents in continuing care may be discontinued when resident
is cooperative with hygiene practices and drainage and body fluids are contained.
If needed, consult IPC or Zone Medical Officer of Health (MOH) or designate for assistance determining
when to discontinue additional precautions for ARO positive resident
Incubation Period
Period of Communicability
Variable
While organism is present in secretions or excretions
Comments
*Precautions required are in addition to Routine Practices
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
277
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Varicella zoster virus: Chickenpox – Exposed Susceptible Contact
See Chickenpox – Exposed Susceptible Contact (Varicella zoster virus)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
278
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Varicella zoster virus: Chickenpox – Known Case
See Chickenpox – Known Case (Varicella zoster virus)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
279
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Varicella zoster virus: Herpes zoster (Shingles) – Disseminated
See Shingles: (Herpes zoster) Varicella zoster virus – Disseminated
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
280
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Varicella zoster virus: Herpes zoster (Shingles) – Exposed
Susceptible Contact
See Shingles: (Herpes zoster) Varicella zoster virus – Exposed Susceptible
Contact
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
281
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Varicella zoster virus: Herpes zoster (Shingles) –
Immunocompromised Host With Localized Lesions (1 or 2
dermatomes)
See Shingles: (Herpes zoster) Varicella zoster virus – Immunocompromised
Host With Localized Lesions (1 or 2 dermatomes)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
282
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Varicella zoster virus: Herpes zoster (Shingles) – Normal Host
With Localized Lesions(1 or 2 dermatomes) AND lesions that CAN
be covered with dressings or clothing
See Shingles: (Herpes zoster) Varicella zoster virus – Normal Host With
Localized Lesions (1 or 2 dermatomes) AND lesions that CAN be covered
with dressings or clothing
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
283
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Varicella zoster virus: Herpes zoster (Shingles) – Normal Host
With Localized Lesions (1 or 2 dermatomes) AND lesions that
CANNOT be covered with dressings or clothing
See Shingles: (Herpes zoster) Varicella zoster virus – Normal Host With
Localized Lesions (1 or 2 dermatomes) AND lesions that CANNOT be
covered with dressings or clothing
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
284
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Vibrio parahaemolyticus Enteritis
Clinical Presentation
Diarrhea, food poisoning
Infectious Substances
How it is Transmitted
Contaminated food, particularly seafood
Not person-to-person transmission
Foodborne
Precautions Needed
Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment: Contact Precautions
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
4 – 30 hours
Not person-to-person transmission
Comments
*Precautions required are in addition to Routine Practices
•
Symptomatic residents must not participate in food handling activities.
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
285
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
W
West Nile (West Nile Virus)
Western Equine Encephalitis
Whipworm (Trichuris trichiura) See Trichuriasis – Whipworm (Trichuris trichiura)
Whooping cough – Pertussis (Bordetella pertussis) See Pertussis – Whooping Cough (Bordetella pertussis)
Wound infection – (Staphylococcus aureus, Streptococcus [Group A], many other bacteria) See Draining Wounds
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
286
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
West Nile (West Nile Virus)
Clinical Presentation
Sudden onset fever, headache, muscle pain and weakness, abdominal pain, nausea, vomiting and
diarrhea, may have rash
Infectious Substances
How it is Transmitted
Culex mosquito
Vector borne: Mosquito bite
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
Variable, usually 3 – 21 days
Not person-to-person transmission except rarely by
blood transfusion or organ transplantation, and
extremely rarely by breast milk or transplacentally
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
287
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Western Equine Encephalitis
Clinical Presentation
Fever, encephalomyelitis
Infectious Substances
How it is Transmitted
Aedes and Culex mosquito
Not person-to-person transmission
Vector borne: Mosquito bite
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
5 – 15 days
Not person-to-person transmission
Comments
•
Virus found in birds, bats, and possible rodents
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
288
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Whipworm (Trichuris trichiura)
See Trichuriasis – Whipworm (Trichuris trichiura)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
289
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Whooping cough – Pertussis (Bordetella pertussis)
See Pertussis – Whooping Cough (Bordetella pertussis)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
290
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Wound infection – (Staphylococcus aureus, Streptococcus [Group
A], many other bacteria)
See Draining Wounds
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed*
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
291
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
X
No organisms at this time
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
292
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Y
Yaws (Treponema pallidum)
Yellow Fever
Yersinia enterocolitica; Yersinia pseudotuberculosis
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
293
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Yaws (Treponema pallidum)
Clinical Presentation
Cutaneous lesions, late stage destructive lesions of skin and bone
Infectious Substances
How it is Transmitted
Exudates from skin lesions
Direct contact
Indirect contact
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
2 weeks to 3 months
Variable
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
294
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Yellow Fever
Clinical Presentation
Sudden fever, chills, headache, back and muscle aches, nausea, vomiting, prostration
Infectious Substances
How it is Transmitted
Infected mosquitoes
Not person-to-person transmission
Vector borne: Mosquito bite
Precautions Needed
Routine Practices
Duration of Precautions
Not applicable
Incubation Period
Period of Communicability
3 – 6 days
Not person-to-person transmission
Comments
•
Refer to your facility’s policy for care of body after death.
•
See Public Health Act – Bodies of Deceased Persons Regulation
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
295
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Yersinia enterocolitica; Yersinia pseudotuberculosis
Clinical Presentation
Diarrhea
Infectious Substances
How it is Transmitted
Feces
Direct Contact
Indirect Contact
Foodborne
Precautions Needed*
Adults: Routine Practices
For incontinent residents, if stool cannot be contained or for residents with poor hygiene who soil the
environment Contact Precautions
Children: Contact Precautions
Duration of Precautions
Until symptoms have been resolved for at least 48 hours and stools are normal
Incubation Period
Period of Communicability
1 – 14 days
Until symptoms have resolved
Comments
*Precautions required are in addition to Routine Practices
•
Symptomatic residents must not participate in food handling activities
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
296
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Z
Zygomycosis (Phycomycosis, Mucormycosis) – (Mucor sp., Zygomycetes sp., Rhizopus sp.) See Mucormycosis
(phycomycosis, zygomycosis) – (Mucor sp., Zygomycetes sp., Rhizopus sp.)
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
297
IPC Diseases and Conditions Table:
Recommendations for Management of Continuing Care Residents
Zygomycosis (Phycomycosis, Mucormycosis) – (Mucor sp.,
Zygomycetes sp., Rhizopus sp.)
See Mucormycosis (phycomycosis, zygomycosis) – (Mucor sp.,
Zygomycetes sp., Rhizopus sp.)
Clinical Presentation
Infectious Substances
How it is Transmitted
Precautions Needed
Duration of Precautions
Incubation Period
Period of Communicability
Comments
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z HOME
298