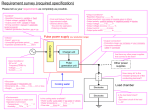
* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Physics of pacing - Cardiac and Stroke Networks in Lancashire
Survey
Document related concepts
Stepper motor wikipedia , lookup
Electrical ballast wikipedia , lookup
Mercury-arc valve wikipedia , lookup
Skin effect wikipedia , lookup
Switched-mode power supply wikipedia , lookup
Nominal impedance wikipedia , lookup
Voltage optimisation wikipedia , lookup
Buck converter wikipedia , lookup
Surge protector wikipedia , lookup
Mains electricity wikipedia , lookup
Stray voltage wikipedia , lookup
Resistive opto-isolator wikipedia , lookup
Current source wikipedia , lookup
Power MOSFET wikipedia , lookup
Transcript
PHYSICS OF PACING NASPE TRAINING Lauren Butler Lancashire & South Cumbria Cardiac Network Objectives Pacing stimulation Variations stimulation threshold Sensing Lead design Pulse generators Calculations !! Strength–Duration Threshold Curve Stimulation threshold definition Minimum amount of energy required to produce depolarisation of the myocardium Exponential relationship exists between pulse duration and stimulus amplitude – strengthduration threshold curve Strength-Duration Curve Threshold (v) 5 4 3 2 1 Rheobase 0 0 0.2 0.4 0.6 0.8 1.0 chronaxie Pulse width (ms) 1.5 Rheobase – smallest voltage amplitude that stimulates the myocardium at an infinitely long pulse duration Chronaxie – threshold pulse duration at twice the stimulus amplitude which is twice the rheobase voltage The chronaxie approximates the lowest stimulation energy (microjoules) required for myocardial deploarisation Strength-Duration Curve Threshold 5 Energy (uJ) 4 3 2 1 Rheobase 0 0 0.2 0.4 0.6 0.8 1.0 chronaxie Pulse width 1.5 Energy Relationship between Energy, voltage, current and pulse duration Minimum threshold energy (chronaxie) Charge E = V2 x t energy R volts current Units uC, uJ, v, mA 0.03 0.5 5 Constant voltage vs Constant current All pacing systems – now operate constant voltage Strength duration curves of constant current are similar in shape but the current decline is more gradual Hence chronaxie tends to be at a higher pulse width ∴ lowest energy requirements are greater in a constant current device Constant voltage – programmed to deliver 5 volts, resultant current is unknown What is that resultant current dependant upon? Impedance (resistance) of the system V=IxR Impedance & Resistance Impedance describes the impediment to current flow of electrons within the entire pacing system All factors that contribute to impedance include Lead conductor resistance Electrode resistance Polarisation resistance In constant voltage systems the higher the pacing impedance the lower the current flow Constant current stimulation ! Calculation to calculate threshold current I = Ir x (1 + tc/t) I = threshold current at pulse duration t Ir = rheobase current tc = chronaxie pulse duration Ideally Lead conductor material – low resistance (to minimize heat wastage and therefore energy loss) Electrode – high resistance (to minimize current flow) Polarisation – low Polarisation Layers of oppositely charged ions that surround the electrode during the pulse stimulus + + + + + + NA+ & H3O+ IONS Polarisation Layers ++- - ++ + ++++ ++ + ++ -- HPO4- & OHnegative ions rush towards the positive ion layer Polarisation impedes the movement of charge from electrode to myocardium, thus requiring a greater voltage to stimulate and depolarise myocardial tissue Polarisation = increase voltage threshold Polarisation layers build up as the pulse stimulus is present and reaches a peak torwards the end of the stimulus The longer the stimulus is present the greater the polarisation To reduce polarisation Reduce pulse width and Use materials which discourage polarisation (platinum black, irridium oxide, titanium nitride, activated carbon) Ideally Lead conductor material – low resistance (to minimize heat wastage and therefore energy loss) Electrode – high resistance (to minimize current flow) Polarisation – low Ideal electrode tip High resistance & ∴ low current drain Small radius – increases current density and in doing so reduces voltage threshold Large surface area – which reduces polarisation Finally Polarisation is inversely related to surface area To maximize surface area (to reduce polarisation) and minimize the radius (to increase electrode impedance) construction of electrodes consist of a small radius with an irregular surface made out of porous, polarisation reducing material Ideal electrode tip Target Tip Wire filament mesh (lazer bullet holes) Coating microspheres Microscopic pores Uneven surface creates hot spots of increased current density whilst keeping the surface area high and the overall radius low Summary – pacing impedance Low resistance conductor coil High resistance at electrode / myocardial interface Small radius High surface area High current density Low polarisation Short pulse width materials Threshold Variations Acute changes Typically rises rapidly within the first 24 hours and then gradually increases to a peak at 1 week over the ensuing 6-8 weeks gradually declines - reach level – chronic threshold Chronic threshold will be higher than the implantation measurement but less than the peak Threshold Variations Magnitude & duration of increase in threshold may be due to Lead electrode size Shape Design Interface between lead & myocardium Individual variation Stable electrode-myocardial interface Passive Vs Active Active leads have higher threshold at implant but frequently reduces between 15 – 30 minutes post placement Due to hyperacute injury due to advancement of screw Cortico-Steroid eluting electrodes reduce acute & chronic thresholds (available passive and active leads) Cellular changes Acute injury to cellular membranes Development myocardial oedema Electrode surface coated with platelets & fibrin Subsequent release chemotactic factors Acute inflammatory reaction – mononuclear cells & polymorphonuclear leukocytes Following acute response – accelerated cellular injury due to release of proteolytic enzymes & oxygen free radicals by invading macrophages Finally – fibroblasts within myocardium produce collagen creating fibrous capsule around electrode tip Fibrous capsule – increase in electrode radius with a possible decrease in electrode surface area Other factors Increase threshold during sleep, reduces during day Increases with hyperglycemia, hypoxia, acute viral illness, after eating, electrolyte fluctuations, drugs Remember the threshold may also increase at fast pacing rates (short cycle lengths) as the pacing stimulus encroaches into the refractory period of the preceeding beat Exit Block Progressive rise in threshold over time Despite initial satisfactory placement Often occurs in parallel within atria and ventricles Often recurs with further placement of new leads Steroid-eluting electrodes prevent exit block in most but not all patients (type steroid – usually 1mg dexamethasone sodium) Sensing Wavefront electrical activity approaches electrode – which creates a positive deflection on IEGM as electrode tip becomes positive in relation to negative region of depolarisation As wavefront passes tip - large negative deflection (called intrinsic deflection) Smaller waveforms pre & post intrinsic deflection due to depolarisation of surrounding myocardium Ventricular IEGM’s are larger than Atrial IEGM’s – muscle mass Fourier transformation determines frequency density Atrial 80 – 100 Hz Ventricular 10 – 30 Hz This allows filter systems to be incorporated into sensing circuits of pacemakers to enhance sensing – myopotentials overlap 10 – 200Hz (Unipolar sensing!) Blanking & refractory periods have helped IEGM – Slew rate Time (Δt) Voltage (ΔV) Slew rate = ΔV/ Δt (Volts/second) R wave amplitude chronic = 85% R wave amplitude acute Slew rate (V) chronic = 50%–60% slew rate (V) acute IEGM – slew rate Peak slope of developing EGM Represents maximal rate of change of the electrical potential between the two sensing electrodes What should the slew rate be? Slew rate > 0.5 v/sec in both chambers High slew = high frequency content = increased chance sensing Slow broad signals (T waves) low slew rate, low frequency content = less likely to be sensed Polarisation again! After termination of pacing stimulus – an excess of positive charge surrounds the cathode which gradually decays until neutral – Afterpotentials Afterpotentials if sensed – inhibition or delay subsequent pacing stimulus Amplitude afterpotentials – related to size and pulse duration of pulse High PW, High Output, Maximum sensitivivity = not good Blanking periods reduce this – if not cross talk (highlighted in unipolar sensing systems) Constant voltage pulse with leading & trailing edge Afterpotential – opposite polarity to stimulus Leading Trailing edge edge Remember – devices with autocapture may be at risk of inappropriate sensing Acute Vs Chronic sensing Amplitude & slew rate may abruptly decline within the 1st week post implant After 6 – 8 weeks, approach implant levels Active fixation leads – marked decrease immediately after implant which increases within 20 – 30 minutes Cortico-steroid eluting leads have little effect on measurements Source and Input impedances Source impedance? The sensing circuit of the system also has impedance Source impedance – voltage drop that occurs from origin of IEGM to proximal portion of lead Electrode myocardial resistance Lead conductor resistance Effects of polarisation Source & Input impedances Input Impedance? Impedance of sensing amplifier itself EGM actually seen by pacer – determined by ratio between sensing amplifier (input impedance) and the lead (source impedance) The bigger the difference/ratio the less attenuation of signal occurs Input impedances are large Source impedances – typically 400 - 1500Ω Impedance mismatch – clinically due to insulation or conductor failure – under or oversensing Lead Design Components Electrode, conductor, insulator, connector pin Mechanically stable & flexible in vivo Satisfactory electrical conductive and resistive properties Durable insulation with low friction coefficient but high tensile strength Good mechanical contact/grip between electrode & myocardium Sensing circuitry Incorporates noise reversion circuits Reverts to fixed rate pacing when rate of noise exceeds the noise reversion rate Incorporate Zener diode – protects circuitry from high voltage sources e.g. defibrillation If voltage exceeds zener voltage, the excess is shuntedback through the leads to the myocardium and is dissipated Electrode Small radius, large surface area Electrode shape, surface composition Also – biologically inert, resist degradation, do not elicit marked tissue reaction at myocardial interface Materials – reduce polarisation whilst achieving the above Metals for electrode use (or not) Toxic reactions Zinc, copper, mercury, nickel, lead, silver Susceptible to corrosion Stainless steel alloys Surface coating oxides impedes current transfer Titanium & tantalium Metals for electrode use In use today Platinum-iridium Elgiloy (alloy cobalt, nickel, chromium, molybdenum, iron & manganese) ! Platinised titanium coated platinum Pyrolytic carbon coated titanium Pyrolytic carbon coated graphite Iridium oxide platinum Activated carbon – least susceptible to erosion, the activation process increases surface area and allows for tissue ingrowth * Lead fixation Passive types Fins, fines, tines Most active fixation screws are now electrically active forming the cathode itself, although some are inactive Steroid eluting – both passive & active Active fixation Distorted anatomy, congenital defects, post surgical (A lead), high right sided pressures, septal placement Active fixation mechanisms Retractable – easier passage down vasculature but mechanism has higher rate of failure Fixed active screws – difficult to pass down veins, apply torque as the lead passes down vein and through tricuspid valve Remember different types Screws, hooks, barbs Lead conductor Multifilament design – to facilitate high tensile strength and reduce metal fatigue Other types include – unifilar and cable designs Bipolar leads – parallel, co-axial (most common), individually coated wires wrapped in a single multifilar arrangement, mixture Bipolar and Unipolar leads Unipolar – smaller diameter lead body Bipolar - Co-axial design Conductor materials Alloy MP35N Cobalt, nickel, chronium, molybdenum Elgiloy Susceptible to corrosion as a lead, OK as an electrode material Nickel-silver – Drawn Brazed Strand (DBS) has 6 nickel alloy wires drawn together with heated silver breaks down polyurethane due to MIO (Metal Ion Oxidation) process – seen in Medtronic 6972 leads Lead Insulation Polyurethane Vs Silicone Polyurethane polymers with widest use Pellathane 80A and Pellathane 55d BUT ** Pellathane 80A had a high failure rate due to small insulation cracks appearing after heating and cooling processes during manufacture. With environmental stresses the cracks deepened – insulation failure In contact with silver chloride conductors – oxidative stress may occur causing failure of insulation from inside Polyurethane – easier to move Advantages polyurethane High tear strength High cut resistance Low friction in blood High abrasion resistance Less thrombogenic Superior compressive properties Advantages Silicone Flexible Good performance record > 30 yrs Easy fabrication & moulding Disadvantages Polyurethane Relatively stiff Sensitive to manufacturing processes Potential – environmental stress cracking (Pellathane 80A) Potential MIO (Pellathane 80A & 55D) Disadvantages Silicone Tears easily Cuts Easily Higher friction in blood More thrombogenic Some leads have silicone body with poyurethane coating (Fast pass coating) When implanting 2 leads – same vein – use same material for easier use Lead connector Standardized IS1 3.2 mm diameter In-line bipolar configuration (not bifurcated) Pulse Generator Power source Output circuitry (pacing) Input circuitry (sensing) Timing circuit Header block RR sensor Telemetry Microprocessor (storage diagnostics) Power source Previously Nuclear, photoelectric cell, rechargeable nickelcadmium cell & biogalvanic energy Now Lithium-Iodine Lithium – anode & provides electrons Iodine – cathode & recieves the electrons Anode & cathode separated by electrolyte which serves as a conductor of ionic movement but as a barrier to electron transfer Circuit completed by external load (leads & myocardium) Battery Voltage Battery voltage depends on chemical composition Lithium Iodine BOL = 2.8v ERI = 2.4v (90 % has been used) Exponentially decreases until EOL is reached EOL = 1.8v Longevity – contributing factors Chemical composition of battery Size of battery External load Pulse amplitude, duration, stimulation frequency, total pacing lead impedance, amount current required to operate circuitry & store diagnostics Amount – internal discharge Voltage decay characteristics Longevity Longevity (years) = Ampere-hours x 114 current drain Finally - calculations Ohms Law V= I x R Energy E = V2/R x t Constant current stimulation (Rheobase/chronaxie) Slew Rate = Δv/Δt Longevity = ampere-hrs/current drain x 114 TO DO Other energy equations Noise sampling equation And Finally ! E = V2/R x t E = VIT E = I2RT Noise sampling Period (NSP) – Convert to Hz (frequency per second) to enable trigger response Hz = 1/t (ms) eg.NSP = 125ms, Hz = 1000/125 = 8Hz