* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Irregular Astigmatism Management
Survey
Document related concepts
Transcript
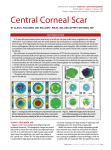
In: Astigmatism Editor: Reuben Buckley ISBN: 978-1-63321-978-6 © 2014 Nova Science Publishers, Inc. No part of this digital document may be reproduced, stored in a retrieval system or transmitted commercially in any form or by any means. The publisher has taken reasonable care in the preparation of this digital document, but makes no expressed or implied warranty of any kind and assumes no responsibility for any errors or omissions. No liability is assumed for incidental or consequential damages in connection with or arising out of information contained herein. This digital document is sold with the clear understanding that the publisher is not engaged in rendering legal, medical or any other professional services. Chapter IV Irregular Astigmatism Management Lucero Pedro-Aguilar, Alejandro Navas, and Enrique Graue-Hernandez Department of Cornea and Refractive Surgery, Institute of Ophthalmology “Conde de Valenciana”, México City, Distrito Federal, Mexico Abstract The term irregular astigmatism is often applied to a distorted corneal topography, whereby two major meridians may not even be easily identified; in simple terms, it can be defined as an “unrefractable” eye. As a consequence, visual function can be severely affected. Conventional treatments are often insufficient and/or unsatisfactory. Spectacles may lead to intolerable aniseikonia, and contact lens fitting is usually challenging. Conservative approaches do not always yield maximal visual results leaving the patient unsatisfied. Numerous surgical procedures have been developed trying to improve astigmatism, including relaxing incisions, thermal and conductive keratoplasty, wedge E-mail: [email protected]. 116 L. Pedro-Aguilar, A. Navas, and E. Graue-Hernandez resections, photorefractive procedures, phakic and intraocular lens implantation, among others. Each procedure needs to be evaluated within the patient’s context and chosen accordingly. The purpose of this chapter is to review the most commonly used techniques for the correction of irregular astigmatism. Introduction The term comes from the Greek α- (a-) meaning "without" and στίγμα (stigma), "a mark/spot”. An optical system with astigmatism is one where rays that propagate in two perpendicular planes have different foci. If an optical system with astigmatism is used to form an image of a cross, the vertical and horizontal lines will be in sharp focus at two different distances. The cornea of the normal eye has a uniform curvature, with resulting equal refracting power over its entire surface. In the eye, astigmatism results from the refraction of light through an aspheric or toric cornea or an abnormal crystalline lens. Light rays refracted by this cornea are not focused to a single point, and retinal images from objects both distant and near are blurred and may appear broadened or elongated. The main differences between regular and irregular astigmatism are summarized in Table 1. Table 1. Regular versus irregular astigmatism Regular astigmatism is correctable using a cylindrical spectacle lens. Irregular astigmatism: refraction in different meridians conforms to no geometrical plan and the refracted rays have no planes of symmetry, not correctable by a sphero-cylindrical lens, “unrefractable”. The further distinction of irregular astigmatism includes regularly or irregularly irregular astigmatism and relates to the presence of pattern recognition on corneal topography (see Figure 1). Irregular Astigmatism Management 117 Astigmatism can be originated from any of the surfaces of the eye, thus it can corneal (or keratometric), lenticular, and retinal, but in most instances it is originated from the anterior surface of the cornea. Astigmatism (more than 0.5 diopters) is a commonly encountered refractive error, accounting for about 13 percent of the refractive errors of the human eye. It is commonly encountered with prevalence rates up to 30% or higher depending on the age or ethnic groups. Studies using videokeratoscopy have found that approximately 40% of normal corneas with a toric refractive error as possessing primary irregular astigmatism. [1] In regular astigmatism, which is the more common form, the cornea would resemble a football or rugby ball with the two principal meridians having different curvature radii. The two principal meridians separated by 90 degrees; the best-corrected visual acuity (BCVA) is at least 20/20 and, in the case of corneal astigmatism, corneal topography displays a symmetrical bowtie pattern. The meridian of greatest and least power, the so-called principal meridians, are always located at meridian 90 degrees apart. Irregular astigmatism (IA) is defined as astigmatism where the principal meridians are not 90 degrees apart. Sir William S. Duke-Elder defined IA as follows: “refraction in different meridians conforms to no geometrical plan and the refracted rays have no planes of symmetry”. [2] It may be defined as an astigmatic state not correctable by a sphero-cylindrical lens thus the term “unrefractable”. Irregular astigmatism can be either “regularly irregular” or “irregularly irregular”. In regularly irregular astigmatism, two principal meridians are either asymmetrical or not 90 degrees apart and characterized by either unequal slopes along a single meridian which generates the classical “asymmetric bow-tie” patterns corneal topography maps or hemimeridians of equal slope but not aligned with each other (the “angled bow-tie” or nonorthogonal astigmatism). Irregularly irregular astigmatism does not have identifiable principal meridians (Figure 1). It is commonly present in diseases that alter corneal shape such as keratoconus and other corneal ecstasies, anterior stromal scarring from various corneal conditions basement membrane and stromal dystrophies, post-traumatic corneal distortion and iatrogenic procedures such as lamellar and penetrating keratoplasty, corneal based refractive procedures (e.g. radial keratotomy). In any case, the magnitude and the axis of astigmatism vary from point to point across the entrance pupil and corneal topography cannot demonstrate a recognizable pattern. Main causes of corneal irregular astigmatism are diverse, including keratoconus (KC), pellucid degeneration (PD), keratoglobus (KG), corneal surgery (keratoplasty, photorefractive keratectomy (PRK), laser in situ L. Pedro-Aguilar, A. Navas, and E. Graue-Hernandez 118 60° 90° 0° 60° 12 9mm 5 7 +2 N +4 N -4 0° ° -2 0 30 270° 0 +2 0° 15 5 3 48.2 50.3 24 7 -2 T -4 +4 T -4 3 52.9 53.0 5 7 51.8 51.3 50.6 0° 3 -4 0 0° 54.3 50.8 24 0° -2 33 52.1 3 0° -2 51.2 33 15 0° 0° 55.1 41.0 48.7 45.4 21 33 3 0° ° 00 270° 0 5 21 0° 24 -2 7 54.9 49.2 42.4 45.3 51.8 0° 0 42.5 ° 7 +2 30 5 48.2 0° 46.4 42.3 180° 42.8 42.2 49.1 -4 +4 0° 43.2 3 49.2 T 60° ° 7 5 42.9 3 42.8 180° 42.6 21 -4 +2 90° 0° 12 46.2 0° 180° -2 9mm 30 ° 47.6 48.0 0 +4 46.2 30 +2 90° 0° 12 9mm 0° +4 15 keratomileusis (LASIK), radial keratotomy (RK), arcuate keratotomy), and scars secondary to infections or burns. Lenticonus may cause astigmatism due to abnormality of the lens. Clinical manifestations of irregular astigmatism could be blurred vision, glare, visual disturbances and ghost images. Through retinoscopy we can observe typical patterns including “scissoring reflex” and jumbled or uninterpretable reflexes. By keratometry, irregular mires are presented. The most common topographic values assessed in irregular astigmatism shown in Table 2. 0° 30 270° 0 +2 N +4 Figure 1. Topographic patterns of irregular astigmatism: Regularly irregular: A) the “asymmetric bow-tie” and B) the “angled bow-tie” or nonorthogonal astigmatism. C) Irregularly irregular, topography cannot demonstrate a recognizable pattern. Table 2. Most common values assessed in corneal topography (statistical indices) Simulated keratometry (SimK) provides the power and location of the steepest and flattest meridian analogous to values obtained by a keratometer. Surface asymmetry index (SAI) is a centrally weighted summation of differences in corneal power between corresponding points 180°apart on 128 equally spaced meridians crosing all the mires. Increases as the corneal shape becomes more asymmetrical. The surface regularity index (SRI) reflects local power fluctuations along 256 equally spaced meridians. Correlates with localized surface regularity. Shape Factor (SF) is the measurement of corneal asphericity. Corneal Irregularity Measurement (CIM) represents the irregularity of the corneal surface. Higher the value of CIM predicts more irregularity. Mean Toric Keratometry (MTK) use elevation data to compare the toric reference to the actual cornea. Irregular Astigmatism Management 119 In the past decades, the available treatment options have increased dramatically, however, the debate continues regarding to the systematic approach necessary to achieve an optimal surface of the eye. Treatment of irregular astigmatism is directed toward the rearrange the orientation of the astigmatism by concurrently regularizing and rotating the axes of astigmatism in both hemidivisions so that they are aligned with each other and closer to the vertical or horizontal meridian with a more favorable position. [3] Treatment options have increased in recent years, particularly with the use of combined procedures, however, the discussion continues regarding to the systematic approach necessary to achieve an optimal surface for the eye. Some examples can be seen in Figure 2. Contact Lenses In patients with irregular astigmatism, optical correction with spectacles has limited success, as this may not provide satisfactory visual function to the patient. Therefore, in attempt to improve the anterior refracting surface, contact lens fitting is and should be the first line of treatment to visually rehabilitate this kind of patients. They are also useful diagnostic tools to assess the visual potential and BCVA and thus may assist in the decision of the other treatment modalities. Corneal topography can and should be obtained in patients with irregular astigmatism. The data from the anterior corneal surface can help in fitting the cornea with the contact lens. Currently many lens designs are available. Soft multicurve lens sets (progressively flatter) with parameters designed for keratoconic corneas are often used as they provide comfort and relatively good visual outcomes, however, when the irregularity is significant a rigid anterior surface is needed to correct the refractive error moderate astigmatism. Piggyback fit is a method fitting a rigid gas permeable lens over a soft lens, to be tried in the management of patients with difficulties in adapting. [4, 5] Fluid-ventilated and gas-permeable scleral lens have proved to be a valuable therapeutic tool in the management of irregular astigmatism resulting from several corneal and ocular surface conditions, who had not responded satisfactorily to conventional methods of optical correction and is an alternative to penetrating keratoplasty for patients with corneal ectasia who are contact lens intolerant. [6-8] 120 L. Pedro-Aguilar, A. Navas, and E. Graue-Hernandez The Prosthetic Replacement of Ocular Surface Ecosystem (PROSE), is a gas permeable scleral lens that vaults the cornea and submerges the entire corneal surface in a pool of oxygenated tears, serve as a protective measure in thin and protruding corneas in addition to providing improved vision. [9, 10] Figure 2. Examples of surgical and nonsurgical therapeutic options available for the management of irregular astigmatism. (A) Fluorogram of contact lens fitting in a patient with keratoconus, (B) Compressive sutures and conductive keratoplasty in a case of high astigmatism post-Radial Keratotomy, (C) Arcuate keratotomy for irregular astigmatism after cataract surgery, (D) Intrastromal ring segments, (E) Pseudophakic toric intraocular lens in keratoconus, (F) Combination of intrastromal ring segments and toric implantable collamer lenses, (G) Wedge resection in a patient with history of pellucid marginal degeneration, and (H) Lamellar keratoplasty in a case of ectasia. Irregular Astigmatism Management 121 Previous studies have reported improved visual functions and decreased higher-order aberrations in subjects with irregular cornea fitted with PROSE device. [11] Hence, PROSE fitting in corneas with steeper curvature such as ectatic disorders has to be carefully monitored while dispensing the PROSE device because reduced vault over a period may cause trauma to the cornea leading to corneal scarring. [12] Contact lenses fitting is possible in patients with mild, moderate and severe irregular astigmatism and even in cases with postoperative astigmatism, provides good comfort, improves visual acuity, and therefore, may postpone the need for surgery. [13] Photorefractive Procedures The goal of modern refractive surgery is to achieve emmetropia and to decrease higher order aberrations. Even a mild residual spherical or cylindrical errors may be considered failure, especially when compared to older refractive surgery procedures. Ablation-related complications following refractive surgery such as decentered ablations, small optical zones, or irregular ablations can produce irregularities in the optical system. [14] Topographically customized ablations have been suggested for the treatment of such corneal irregularities. It may be necessary to perform a treatment that does not change the manifest refraction but that improves vision by “regularizing” the corneal surface technique named topography smoothing. Published reports to date have found topography-guided treatment in general to be effective, successfully improving uncorrected visual acuity (UCVA), BCVA in the setting of previous refractive surgery or even improving the corneal shape after corneal transplantation. However, customized ablations including both, topography and wavefront-guided treatments have reported lower effectiveness in reducing irregular astigmatism secondary to scars, postoperative cataract wound gape (incisional), and postkeratotomy irregularities. [15] It is important to consider that most cornea based refractive procedures may increase higher order aberrations while attempting to neutralize high cylinder. Also, the unpredictability of the refractive outcome appears to be the major disadvantage of current laser systems. Complications associated with photoablative surgery are also an important drawback. For example, 122 L. Pedro-Aguilar, A. Navas, and E. Graue-Hernandez photorefractive keratectomy performed over corneal grafts may cause significant haze and associated irregularities and regression; [16] on the other hand, performing LASIK in such cases increases the chance of wound dehiscence as a result of high vacuum pressure with the microkeratome. Also flap-related complications are of concern, as these corneas tend to be either too steep or too flat to be safely severed with a microkeratome blade or even with femtosecond lasers. Laser based surgery in keratoconus is debatable, specifically increasing the risk of disease progression. However, recent evidence suggest that limited ablation performed to improve corneal shape may help in stabilizing the cornea and improve visual function thus giving the ablation. Crosslinking may be used in conjunction to improve corneal biomechanics. [17, 18] Corneal Tuck The basis of the corneal tuck is suture-induced tissue compression. In this procedure an incision is made across the flat meridian, concentric with the limbus and down to Descemet´s membrane and then it is closed with interrupted sutures. However, sutures eventually degrade and loose their tensile strength thereby loosing the effect. Busin and colleagues performed a excision of a part of the diseased tissue and reinforcement of the residual ectatic periphery by means of corneal tuck for the treatment of extremely advanced pellucid marginal corneal degeneration, resulting in a marked reduction of the preoperative irregular astigmatism, thus allowing a BCVA of 20/50 or better. [19] Due to the unpredictability of this technique, it is reserved almost exclusively for those patients in which conventional corneal transplantation has to extend from limbus to limbus to excise the ectatic cornea thus dramatically increasing the risk of rejection. Improvement in contact lens technology and the introduction of intracorneal rings into the refractive armamentarium have limited the use of corneal tuck, however it may still be of use in patients with limited peripheral thinning (Terrien´s or pellucid marginal degeneration) or in graft patients with ectatic peripheral host cornea. Although theoretically simple, this technique may be extremely difficult to perform and may have deleterious effects on visual function. Irregular Astigmatism Management 123 Conductive Keratoplasty Conductive keratoplasty (CK) uses a 450-micron-sized probe that releases a controlled high-frequency radio wave (350 kHz) to predetermined locations on the peripheral cornea. This causes shrinkage of the collagen fibers with a resultant change in corneal curvature. [20] Several studies have shown CK to be a safe and effective treatment of low-to-moderate irregular hyperopic astigmatism after refractive surgery. These studies reported that most of the correction loss occurred during the first postoperative year, with a minimal regression. [21-23] The few published reports of complications include iron ring lines, keratitis and corneal perforation. [24-26] Conductive keratoplasty may be a minimally invasive option for patients with irregular hyperopic astigmatism, however larger series and longer follow-up periods may be needed to assess this especific indications. Semilunar and Wedge Resections Both were used in last decades to correct astigmatism. Lans used deep, double wedge resections, unsutured or sutured, to modified the corneal toricity. In addition, Wiener used elliptical peeling and crescentic resections adjacent to the limbus in patients with keratoconus. [27] The semilunar resection developed by Professor Jose I. Barraquer consisting of a crescentric piece of tissue with perpendicular walls is resected in full thickness from the limbal area, often under a conjunctival flap. [28] Corneal wedge resections were developed by Richard Troutman. [29] In this procedure, a very deep crescentric tissue with various central widths of up to 1.5 mm is resected from the area of the graft across the flat corneal meridian; the length of the resection is approximately 70 to 90º in arc length. The two curvilinear incisions can be made sequentially with a single blade or simultaneously with a doubled-bladed diamond knife and the wound is sutured. In general, the amount of correction obtained is related to the central width of the resection, although the results correlate only mildly and may be somewhat unpredictable. [30, 31] Crescentic lamellar keratoplasty acts tectonically, simply reinforcing the ectatic area of the cornea, usually with poor visual and refractive outcomes. Instead, wedge resection offers the advantage of removing the ectatic tissue 124 L. Pedro-Aguilar, A. Navas, and E. Graue-Hernandez and preserving the recipient cornea, restructured in a shape compatible with useful vision. As in corneal tuck, these procedures are often limited to peripheral thinning disorders. Careful case selection is key to success. During the procedure is often recommended to tighten the sutures so that, the astigmatism is inverted, to allow for suture removal at the slit-lamp and as well generates a reserve for regression as the suture tensile strength decreases. Radial Keratotomy Keratotomies of various types have been proposed for the correction of astigmatism, these include radial, arcuate, transversal and combinations of all. However it is generally accepted that all these techniques are limited to the correction of low degrees of astigmatism. No standard method has been established to perform arcuate keratotomy (AK), and even with mechanical devices, such as the Hanna keratome, results showed a low reliability. [32-34] Femtosecond laser (FSL) is a step forward in the evolution of corneal surgery, aiming to reduce the deviation of depth and size of corneal incisions to a minimum. The use of this technology has several advantages, including improved accuracy and safety, associated with enhanced reproducibility. [35-37] The Alpins method for vector analysis that using refractive, keratometric, and astigmatism data has shown a decrease of 2.56 D for laser AK and 4 D for mechanized AK. [33] Previous reports have variable results, Hjortdal and Ehlers found a 54% reduction in refractive cylinder with paired AKs in 21 post-keratoplasty eyes, and Hovding found a 49% reduction with transverse keratotomies in 12 post-keratoplasty eyes. [38, 39] Limbal relaxing incisions (LRIs) are used to treat low-to-moderate degrees of astigmatism and are either performed at the time of cataract extraction or as an independent procedure. Planning incisions precisely on axis is not critical since it produces lesser effect than corneal incisions and significant over corrections are rare. The forgiving nature of LRIs is due to placement and length of the incision. LRI produces lesser effect than corneal relaxing incision, thus precise alignment of the axis is not as critical. LRIs can be useful in patients with astigmatism outside the range of the toric lenses; in patients with astigmatic eyes that cannot support a toric lens in the capsular bag; in patients with asymmetric and nonorthogonal astigmatic axes, in which each incision can be Irregular Astigmatism Management 125 placed on each arm of the steep axis. [40, 41] Carvalho et al. have shown that LRI´s performed during phacoemulsification surgery are a safe, effective, and stable procedure to reduce pre-existing corneal astigmatism. [42] Author like Belmont et al. described 48.9% of reduction in postoperative refractive astigmatism using wedge resection and relaxing incisions after PK. [43] Complications associated with these techniques include transient glare, fluctuating visual acuity, undercorrection, overcorrection, scarring, perforation, wound leak, and infection. [44] Intrastromal Corneal Ring Segments The concept of intrastromal corneal rings was introduced in 1978, were first implanted in humans in 1991 to correct myopia. [45, 46] ICR´s are space ocupying elements that inserted in the corneal stroma help flatten the steep meridians while the coupling effect steepens the flatter. Multiple arc lengths and thickness and optical zone diameters are available commercially, however none have proven to be superior. The aim of ICRS surgery is to induce a geometric change in the central corneal curvature, thus, reducing the refractive error and the mean keratometry and improving the visual acuity. An improvement in the optical quality of the cornea and a reduction in optical aberrations can also be expected. ICRS have been used for other indications other than primary KC. The results of implant insertion on corneal topography, refraction, and visual acuity in post-LASIK ectasia were similar to those reported for KC. The evidence for this indication, however, only involved case reports and small case series. ICRS were also successfully used to treat recurrent KC after corneal transplant but this was based on only a small case reports. [47] The channels for the insertion of the segments can be created mechanically or with a femtosecond laser. The most common complications associated with the mechanical dissection are: epithelial defects on the insertion site, anterior and posterior perforations, inadequate depth placement of the ring, extrusion, infectious keratitis, stromal thinning, stromal edema, intraepithelial growth in the tunnel, corneal melting and tunnel vascularization. The use of the femtosecond laser reduces the risk of complications in the creation of the tunnels, however it has been reported that the main 126 L. Pedro-Aguilar, A. Navas, and E. Graue-Hernandez complication with this technique is the incomplete formation of the tunnel (up to 2.7% of the cases), among those cited previously for the manual technique. Improvements in visual acuity and refractive error following insertion of ICRS, however, were not noted for all patients. Although improvements were not found to vary across age groups there were differences across stages of disease. Several reports suggested that improvements in visual acuity and refractive outcomes may not be as large or predictable in more advanced stages of KC. [48] Corneal collagen cross-linking (CXL) used in conjunction with ICRS implantation has shown promising results in improving visual acuity and slowing the progression of keratoconus. ICRS, although they flatten the corneal surface, do not prevent the progression of keratoconus. Several longterm follow up studies have demonstrated that the beneficial effects of ICRS regress over time. [49] CXL has the potential to slow or stop the progression of keratoconus by strengthening and stabilizing the collagen in the corneal stroma via rearrangement of corneal lamellae. The combination of the two treatments is potentially synergistic. [50] Toric Intraocular Lenses Corneal astigmatism is usually treated at the corneal plane. Nevertheless, some cases cannot be treated in such a manner, because for example large amount of cylinder or ocular surface disease. In such cases, correction of astigmatism with an intraocular lens may offer better and more stable results. The selection criteria, intraocular lens (IOLs) calculation issues, and surgical techniques for IOL implantation, clinical outcomes including uncorrected visual acuity, residual refractive astigmatism, and spectacle dependency, should be discussed with patients to generate realistic expectations. Emmetropia was not an achievable target for most of the study eyes because of low toric cylindrical powers, even with the expanded range. The safety, efficacy and predictability indexes of all of the studies have demonstrated to be very suitable in cases in which the patient has been selected appropriately, in particular, adequately identifying progression and refractability. Multiple studies with different brands of toric lenses have been employed for the treatment of irregular astigmatism and for the management of residual ametropia following penetrating keratoplasty. [51-55] This technique allows for the appropriate ametropia correction in cases of non- Irregular Astigmatism Management 127 progressive keratoconus, furthermore may be used with additional treatments, for example, combined intraocular lens treatment (piggyback) for the management of residual ametropia in post-keratoplasty patients. The misalignment is the most frequent complication of toric IOLs, however corneal decompensation; graft failure rates, retinal detachment and macular edema have been associated with cataract surgery. Another drawback of this technique is the potential for miscalculation of the lens power. Irregular corneas frequently display not only asymmetrical or irregular cylinder power, but the relationship between the anterior and posterior corneal curvature are lost, thus the IOL formulas are not as precise when compared to unoperated eyes. This raises the potential for a refractive surprise. However, we have shown that toric IOLs implantation in patients with irregular keratoconus (regularly irregular) may be an effective therapeutic option in the optical rehabilitation of patients with stable and nonprogressive keratoconus. [52, 56, 57] Phakic IOLs are based on the patient’s spectacle refraction. The benefits of phakic IOLs are reversibility and preservation of accommodation. The selection criteria for the placement of a phakic lens include a stable refraction or ectatic disorder, correctable refractive error due to the types of phakic lenses available, endothelial count greater than 2500 cells/mm2, anterior chamber depth > 2.8 mm and absence of uveal pathology or glaucoma. [17, 58] Patients undergoing posterior chamber phakic IOLs should be counseled about the risk of cataract and the potential need for further surgical intervention. [59] Furthermore there may be more long-term risks unique to patients with phakic IOLs, such as continued endothelial cell loss and cataract formation. Bioptics The bioptics approach is a sequential combination of different refractive techniques to treat large and complex refractive errors. The use of this approach in the management of refractive errors secondary to keratectasia has been reported previously, combining phakic intraocular lens implantation with intracorneal ring segments or refractive lens exchange combined with keratorefractive surgery. 128 L. Pedro-Aguilar, A. Navas, and E. Graue-Hernandez Performed bioptics procedures with sequential intracorneal ring and IOL implantation allow us to improve the corneal characteristics and visual acuity in eyes with corneal ectasia. Cakir et al. performed sequential intracorneal Keraring segments and Artisan/Artiflex iris-fixated IOL implantation yielded satisfactory visual and refractive results and could be considered as an alternative to penetrating keratoplasty in patients with different corneal ectatic conditions with high myopic refractive errors, they suggest performing intracorneal ring implantation first, which corrects the refractive myopia and astigmatism in a limited manner and are often unpredictable in different stages of the ectatic disease, it is important to wait until the corneal edema disappears and the refractive error stabilizes before proceeding to the next step of the bioptics procedure. [60] Few studies have reported the combined effect of the three procedures; AlTuwairqi et al. reported placement of ICRS followed by combined topography-guided PRK/CXL appears to be safe and an effective option in select patients with keratoconus. [61] Keratoplasty If contact lens fitting is unsuccessful or the above treatments cannot be performed a penetrating or lamellar keratoplasty may be performed to restore corneal anatomy. The penetrating transplant was considered the treatment of choice for keratoconus for many decades; [62] nevertheless, one of the principal disadvantages has to do with the risk of immunological rejection which can occur in up to 20% of the patients with good prognosis, such as the case of keratoconus. [63, 64] This technique continues to be the treatment of choice when there are endothelial scars (secondary scars to hydrops) or low receptor endothelial cell count. The advantages of the lamellar techniques over the penetrating keratoplasty are that these techniques have lower recuperative time periods, earlier management of astigmatism and sutures and lower incidence of postoperative glaucoma and graft rejection. [65-67] The most important limitations of the lamelar techniques continue to be the irregular borders of the corneal surface dissection that are obtained through manual technique. [68, 69] Irregular Astigmatism Management 129 Recommendations The first step to managing corneal astigmatism is to accurately assess the magnitude and axis of astigmatism, also the stability, especially in ectatic diseases. Total refractive astigmatism is best identified by the manifest or the cycloplegic refraction. The total refractive astigmatism is composed of both corneal astigmatism and lenticular astigmatism. It is important to differentiate these two components because the lenticular component will be replacing in the crystalline lens. Regularly irregular astigmatism Myopic Photoablative procedures (topo or wavefrontguided PRK, LASIK) Hyperopic IOLs * ICRS IOLs* CK Compresive sutures PRK: photorefractive keratectomy; ICRS: intrastromal corneal rings segments; IOLs: intraocular lenses.* If the patient < 50 years: toric phakic lens, if > 50 years: posterior chamber intraocular lens. Irregularly irregular astigmatism Myopic (e.g. post-PK) Topo or wavefrontguided PRK, LASIK) Semilunar, Wedge Resections PK Combined procedures: ICRS +IOLs ICRS+PRK/LASIK Hyperopic (e.g. post-RK) PK Compresive sutures PK: penetrating keratoplasty; RK: radial keratotomy; PRK: photorefractive keratectomy ; ICRS: intrastromal corneal rings segments; IOLs: intraocular lenses.* If the patient < 50 years: toric phakic lens, if > 50 years: posterior chamber intraocular lens. Figure 3. Proposed algorithm for management in irregular astigmatism based on spherical refractive error and topographic pattern. 130 L. Pedro-Aguilar, A. Navas, and E. Graue-Hernandez Topographic analysis of the corneal surface, wavefront analysis of ocular refractive aberrations, and vector planning to enable the appropriate balance in emphasis between these two diagnostic modalities. In recent times, a spate of combinations of procedures, such as collagen crosslinking, intracorneal rings, ICLs, and photorefractive keratectomy have been reported, these procedure reduces residual manifest refraction cylinder to predictably low levels with corresponding improvement in UDVA and CDVA. In Figure 3 we suggest a management algorithm for patients with irregular astigmatism, based on the spherical refractive and topographic pattern. By examining the success of each surgical technique, the refractive surgeon may be able to make an informed decision on its indications and limitations, based on the specific patient’s characteristics. References [1] [2] [3] [4] [5] [6] [7] [8] [9] Bogan S. J., Waring G. O., 3rd., Ibrahim O., et al. Classification of normal corneal topography based on computer-assisted videokeratography. Arch. Ophthalmol., 1990;108:945-9. Duke-Elder S. Pathological refractive errors, 1970:363. Alpins N. A. Treatment of irregular astigmatism. J. Cataract Refract. Surg., 1998;24:634-46. Yamazaki E. S., da Silva V. C., Morimitsu V., et al. [Keratoconus special soft contact lens fitting]. Arq. Bras. Oftalmol., 2006;69:557-60. Lim N. and Vogt U. Characteristics and functional outcomes of 130 patients with keratoconus attending a specialist contact lens clinic. Eye (Lond.), 2002;16:54-9. Arumugam A. O., Rajan R., Subramanian M., et al. PROSE for irregular corneas at a tertiary eye care center. Eye Contact Lens, 2014;40:71-3. Rosenthal P. and Cotter J. The Boston Scleral Lens in the management of severe ocular surface disease. Ophthalmol. Clin. North Am., 2003;16: 89-93. Baran I., Bradley J. A., Alipour F., et al. PROSE treatment of corneal ectasia. Cont. Lens Anterior Eye, 2012;35:222-7. Dimit R., Gire A., Pflugfelder S. C., et al. Patient ocular conditions and clinical outcomes using a PROSE scleral device. Cont. Lens Anterior Eye, 2013;36:159-63. Irregular Astigmatism Management 131 [10] Lee J. C., Chiu G. B., Bach D., et al. Functional and visual improvement with prosthetic replacement of the ocular surface ecosystem scleral lenses for irregular corneas. Cornea, 2013;32:1540-3. [11] Gumus K., Gire A. and Pflugfelder S. C. The impact of the Boston ocular surface prosthesis on wavefront higher-order aberrations. Am. J. Ophthalmol., 2011;151:682-690 e2. [12] Mahadevan R., Fathima A., Rajan R., et al. An ocular surface prosthesis for keratoglobus and Terrien's marginal degeneration. Optom. Vis. Sci., 2014;91:S34-9. [13] Moreira L. B., Bardal R. A. and Crisigiovanni L. R. Contact lenses fitting after intracorneal ring segments implantation in keratoconus. Arq. Bras. Oftalmol., 2013;76:215-7. [14] Wilson S. E. Clinical practice. Use of lasers for vision correction of nearsightedness and farsightedness. N. Engl. J. Med., 2004;351:470-5. [15] Reinstein D. Z., Archer T. J. and Gobbe M. Combined corneal topography and corneal wavefront data in the treatment of corneal irregularity and refractive error in LASIK or PRK using the Carl Zeiss Meditec MEL 80 and CRS-Master. J. Refract. Surg., 2009;25:503-15. [16] Lee B. S. and Hardten D. R. Visual and subjective outcomes of phototherapeutic keratectomy after Descemet's stripping endothelial keratoplasty. Clin. Ophthalmol., 2014;8:1011-5. [17] Jaimes M. R.-M. A., Graue-Hernandez E. O., Navas A. Keratoconus therapeutics advances. World Journal of Ophthalmology, 2013;3:20-31. [18] Kanellopoulos A. J. and Binder P. S. Collagen cross-linking (CCL) with sequential topography-guided PRK: a temporizing alternative for keratoconus to penetrating keratoplasty. Cornea, 2007;26:891-5. [19] Busin M., Santorum P. and Barbara R. Combined tissue excision and corneal tuck for the surgical treatment of extremely advanced pellucid marginal corneal degeneration. Cornea, 2013;32:1628-30. [20] Berjano E. J., Saiz J., Alio J. L., et al. Ring electrode for radio-frequency heating of the cornea: modelling and in vitro experiments. Med. Biol. Eng. Comput., 2003;41:630-9. [21] Habibollahi A., Hashemi H., Mehravaran S., et al. Visual Outcomes of Conductive Keratoplasty to Treat Hyperopia and Astigmatism After Laser in situ Keratomileusis and Photorefractive Keratectomy. Middle East Afr. J. Ophthalmol., 2011;18:238-42. [22] Moshirfar M., Anderson E., Hsu M., et al. Comparing the rate of regression after conductive keratoplasty with or without prior laser- 132 [23] [24] [25] [26] [27] [28] [29] [30] [31] [32] [33] [34] [35] [36] L. Pedro-Aguilar, A. Navas, and E. Graue-Hernandez assisted in situ keratomileusis or photorefractive keratectomy. Middle East Afr. J. Ophthalmol., 2012;19:377-81. Esquenazi S., Bui V. and Bibas O. Surgical correction of hyperopia. Surv. Ophthalmol., 2006;51:381-418. Kymionis G. D., Naoumidi T. L., Aslanides I. M., et al. Corneal iron ring after conductive keratoplasty. Am. J. Ophthalmol., 2003;136:378-9. Khalifa Y. M. and Mifflin M. D. Keratitis and corneal melt with ketorolac tromethamine after conductive keratoplasty. Cornea, 2011; 30: 477-8. Pallikaris I. G., Naoumidi T. L. and Astyrakakis N. I. Conductive keratoplasty to correct hyperopic astigmatism. J. Refract. Surg., 2003;19:425-32. Swinger C. A. Postoperative astigmatism. Surv. Ophthalmol., 1987;31: 219-48. Barraquer J. I. Basis of refractive keratoplasty--1967. Refract. Corneal Surg., 1989;5:179-93. Troutman R. C. Control of corneal astigmatism in cataract and corneal surgery. Trans Pac. Coast Otoophthalmol. Soc. Annu. Meet., 1970;51: 217-31. Hoppenreijs V. P., van Rij G., Beekhuis W. H., et al. Long-term results of corneal wedge resections for the correction of high astigmatism. Doc. Ophthalmol., 1990;75:263-73. Maccheron L. J. and Daya S. M. Wedge resection and lamellar dissection for pellucid marginal degeneration. Cornea, 2012;31:708-15. Borderie V. M., Touzeau O., Chastang P. J., et al. Surgical correction of postkeratoplasty astigmatism with the Hanna arcitome. J. Cataract Refract. Surg., 1999;25:205-11. Hoffart L., Touzeau O., Borderie V., et al. Mechanized astigmatic arcuate keratotomy with the Hanna arcitome for astigmatism after keratoplasty. J. Cataract Refract. Surg., 2007;33:862-8. Fares U., Mokashi A. A., Al-Aqaba M. A., et al. Management of postkeratoplasty astigmatism by paired arcuate incisions with compression sutures. Br. J. Ophthalmol., 2013;97:438-43. Hoffart L., Proust H., Matonti F., et al. Correction of postkeratoplasty astigmatism by femtosecond laser compared with mechanized astigmatic keratotomy. Am. J. Ophthalmol., 2009;147:779-87, 787 e1. Ruckl T., Dexl A. K., Bachernegg A., et al. Femtosecond laser-assisted intrastromal arcuate keratotomy to reduce corneal astigmatism. J. Cataract Refract. Surg., 2013;39:528-38. Irregular Astigmatism Management 133 [37] Kumar N. L., Kaiserman I., Shehadeh-Mashor R., et al. IntraLaseenabled astigmatic keratotomy for post-keratoplasty astigmatism: onaxis vector analysis. Ophthalmology, 2010;117:1228-1235 e1. [38] Hjortdal J. O. and Ehlers N. Paired arcuate keratotomy for congenital and post-keratoplasty astigmatism. Acta. Ophthalmol. Scand., 1998;76: 138-41. [39] Hovding G. Transverse keratotomy in postkeratoplasty astigmatism. Acta. Ophthalmol. (Copenh.), 1994;72:464-8. [40] Rubenstein J. B. and Raciti M. Management of astigmatism: LRIs. Int. Ophthalmol. Clin., 2012;52:31-40. [41] Arraes J. C., Cunha F., Arraes T. A., et al. [Limbal relaxing incisions during cataract surgery: one-year follow-up]. Arq. Bras. Oftalmol., 2006; 69:361-4. [42] Carvalho M. J., Suzuki S. H., Freitas L. L., et al. Limbal relaxing incisions to correct corneal astigmatism during phacoemulsification. J. Refract. Surg., 2007;23:499-504. [43] Belmont S. C., Lazzaro D. R., Muller J. W., et al. Combined wedge resection and relaxing incisions for astigmatism after penetrating keratoplasty. J. Refract. Surg., 1995;11:472-6. [44] Rashid E. R. and Waring G. O., 3rd. Complications of radial and transverse keratotomy. Surv. Ophthalmol., 1989;34:73-106. [45] Schanzlin D. J., Asbell P. A., Burris T. E., et al. The intrastromal corneal ring segments. Phase II results for the correction of myopia. Ophthalmology, 1997;104:1067-78. [46] Burris T. E. Intrastromal corneal ring technology: results and indications. Curr. Opin. Ophthalmol., 1998;9:9-14. [47] Park J. and Gritz D. C. Evolution in the use of intrastromal corneal ring segments for corneal ectasia. Curr. Opin. Ophthalmol., 2013;24:296301. [48] Health Quality O. Intrastromal corneal ring implants for corneal thinning disorders: an evidence-based analysis. Ont. Health Technol. Assess Ser., 2009;9:1-90. [49] Pinero D. P., Alio J. L., Barraquer R. I., et al. Corneal biomechanical changes after intracorneal ring segment implantation in keratoconus. Cornea, 2012;31:491-9. [50] Coskunseven E., Jankov M. R., 2nd., Hafezi F., et al. Effect of treatment sequence in combined intrastromal corneal rings and corneal collagen crosslinking for keratoconus. J. Cataract Refract. Surg., 2009;35: 2084-91. 134 L. Pedro-Aguilar, A. Navas, and E. Graue-Hernandez [51] Gills J. P. Sutured piggyback toric intraocular lenses to correct high astigmatism. J. Cataract Refract. Surg., 2003;29:402-4. [52] Navas A. and Suarez R. One-year follow-up of toric intraocular lens implantation in forme fruste keratoconus. J. Cataract Refract. Surg., 2009;35:2024-7. [53] Srinivasan S., Ting D. S. and Lyall D. A. Implantation of a customized toric intraocular lens for correction of post-keratoplasty astigmatism. Eye (Lond.), 2013;27:531-7. [54] Ormonde S. Refractive surgery for keratoconus. Clin. Exp. Optom., 2013; 96:173-82. [55] Colin J. and Velou S. Utilization of refractive surgery technology in keratoconus and corneal transplants. Curr. Opin. Ophthalmol., 2002;13: 230-4. [56] Alio J. L., Pena-Garcia P., Abdulla Guliyeva F., et al. MICS with toric intraocular lenses in keratoconus: outcomes and predictability analysis of postoperative refraction. Br. J. Ophthalmol., 2014;98:365-70. [57] Nanavaty M. A., Lake D. B. and Daya S. M. Outcomes of pseudophakic toric intraocular lens implantation in Keratoconic eyes with cataract. J. Refract. Surg., 2012;28:884-9. [58] Guerin M. B., Treacy M. P. and O'Keeffe M. Twelve-month follow-up of the Artiflex toric phakic intraocular lens. Eur. J. Ophthalmol., 2014;24:10-3. [59] Health Quality O. Phakic intraocular lenses for the treatment of refractive errors: an evidence-based analysis. Ont. Health Technol. Assess Ser., 2009;9:1-120. [60] Cakir H. and Utine C. A. Combined Kerarings and Artisan/Artiflex IOLs in Keratectasia. J. Refract. Surg., 2010;1-8. [61] Al-Tuwairqi W. and Sinjab M. M. Intracorneal ring segments implantation followed by same-day topography-guided PRK and corneal collagen CXL in low to moderate keratoconus. J. Refract. Surg., 2013;29:59-63. [62] Vazirani J. and Basu S. Keratoconus: current perspectives. Clin. Ophthalmol., 2013;7:2019-30. [63] Pramanik S., Musch D. C., Sutphin J. E., et al. Extended long-term outcomes of penetrating keratoplasty for keratoconus. Ophthalmology, 2006;113:1633-8. [64] Choi J. A., Lee M. A. and Kim M. S. Long-term outcomes of penetrating keratoplasty in keratoconus: analysis of the factors associated with final visual acuities. Int. J. Ophthalmol., 2014;7:517-21. Irregular Astigmatism Management 135 [65] Busin M., Zambianchi L. and Arffa R. C. Microkeratome-assisted lamellar keratoplasty for the surgical treatment of keratoconus. Ophthalmology, 2005;112:987-97. [66] Feizi S., Javadi M. A., Jamali H., et al. Deep anterior lamellar keratoplasty in patients with keratoconus: big-bubble technique. Cornea, 2010;29:177-82. [67] Coster D. J., Lowe M. T., Keane M. C., et al. A comparison of lamellar and penetrating keratoplasty outcomes: a registry study. Ophthalmology, 2014;121:979-87. [68] Anwar M. and Teichmann K. D. Deep lamellar keratoplasty: surgical techniques for anterior lamellar keratoplasty with and without baring of Descemet's membrane. Cornea, 2002;21:374-83. [69] Almousa R., Samaras K. E., Khan S., et al. Femtosecond laser-assisted lamellar keratoplasty (FSLK) for anterior corneal stromal diseases. Int. Ophthalmol., 2014;34:49-58.