* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Typical antipsychotic drugs
Pharmacogenomics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Polysubstance dependence wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Prescription costs wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
Toxicodynamics wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug interaction wikipedia , lookup
Serotonin syndrome wikipedia , lookup
Norepinephrine wikipedia , lookup
Chlorpromazine wikipedia , lookup
Atypical antipsychotic wikipedia , lookup
Antipsychotic wikipedia , lookup
Neuropharmacology wikipedia , lookup
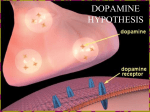
Major Psychiatric Disorders Psychoses eg schizophrenia Affective disorders eg depression and mania Psychoses False perceptions (Hallucinations) False beliefs (Delusions) Affective Disorders Emotional disturbances: Mood is very low (Depression) Mood is very high (Mania) Schizophrenia Most common form of psychosis (1% of world population) Most typical features are : -Delusions -Hallucinations -Disorganised thinking -Emotional abnormalities Types of Schizophrenia Paranoid Disorganised Catatonic forms Symptoms Positive symptoms: agitation, delusions, insomnia, disorganised speech, hallucinations disorganised thinking Result from excessive neuronal activity in mesolimbic neuronal pathways Negative symptoms: apathy, lack of motivation,lack of pleasure, social isolation, poverty of speech Result from insufficient activity in mesocortical neuronal pathways Aetiology and pathogenesis Children of two schizophrenic parents have about 40% risk of disease So heredity appears to have a major role Dopamine hypothesis or= phamacocentric hypothesis Hypofrontality hypothesis Linked hypothesis Antipsychotic Drugs Mechanisms of action -competitive blockade of dopamine receptors and serotonin receptors -adverse effect result from blockade of different receptors Typical antipsychotic drugs They have an equal or greater affinity for D2 receptors than for 5-HT2 receptors Antagonism of D2 receptors in mesolimbic pathways suppress the positive symptoms of SCh Blockade of D2 receptors in the basal ganglia is responsible for parkinsonian and other extrapyramidal side effects of anti psychotic drugs Atypical antipsychotic drugs eg clozapine have a greater affinity for 5-HT2 receptors than for D2 receptors Some atypical drugs have increased affinity for D3 or D4 receptors Three time-dependent changes in dopamine neuroteransmission Compensatory response (increase in dopamine synthesis and release) to acute blockade of postsynaptic dopamine receptors Continued dopamine receptor blockade Inactivation of dopaminergic neurons reduced dopamine release from mesolimbic and nigrostriatal neurons, So, alleviate positive symptoms of schizophrenia and cause extrapyramidal side effects. Continued Dopamine reduction causes dopamine upregulation and super sensitivity to dopamine agonists and then delayed extrapyramidal side effect called tardive dyskinesia. In mesocortical and nigrostriatal pathways, 5HT2 receptors mediate presynaptic inhibition of dopamine release. Blockade of 5-HT2 receptors by atypical drugs increase dopamine release in these pathways. Continued In mesocortical pathway, this action alleviate negative symptoms of Sch. In nigrostriatal pathway, increased dopamine release counteracts the extrapyramidal side effects caused by D2 receptor blockade. Drug Classification Typical antipsychotic drugs -Phenothiazines -Thioxanthenes -Butyrophenones - some Azepines (eg loxapine) Atypical antipsychotic drugs -other Azepines (clozapine, olanzapine) -Benzisoxasole (risperidone) Phenothiazines Chlorpromazine, Fluphenazine, Thioridazine, Trifluoperazine Similar therapeutic effects Different potency and side effect Chlo. And Thio. lower potency, more autonomic side effects and fewer extrapyramidal side effects than high potency Flu. Higher potency Mechanisms of therapeutic effects Blockade of D2 receptors Positive symptoms of Sch. Decrease in 1-3 weeks Less agitated, fewer auditory hallucinations, disappear of paranoid delusions Behavioural improvement Adverse effects 1- Extrapyramidal side effects -Acute: 1- Akathisia 2- Pseudoparkinsonism 3- Dystonias -Chronic: Tardive dyskinesia continued 2- neuroleptic malignant syndrome 3-increase serum prolactin levels 4-impair thermoregulation cause poikilothermy Treatment of adverse side effects Acute extrapyramidal side effects Decrease dose Change to atypical drug Counteract with benztropine, diphenhydramine, amantadine Chronic extrapyramidal side effects Decrease dose Drug treatment Continued Neuroleptic malignant syndrome Supportive care Discontinuing of drug Administration of bromocryptine Change to atypical Indication of Phenothiazines Schizophrenia Drug-induced psychosis Psychosis associated with the manic phase of bipolar disorder. Dementia Severe mental retardation Some of them for management of nausea and vomiting Chlorpromazine and thioridazine Thioridazine causes greater antichloinergic activity And so fewer extrapyramidal side effect High doses of thioridazine cause pigmentary retinopathy and cardiac arrythmia Fluphenazine and trifluoperazine In compare with thioridazine, cause fewer autonomic side effect and more extrapyramidal side effects Fluphenazine is available in long-term depot preparation Thioxanthenes Thiothixene has pharmacological effects similar to trifluoperazine It is used for schizophrenia (Other thiothixenes in BNF are flupentixol [depixol] zuclopentixol [clopixol]. Butyrophenones Haloperidol has pharmacological effects similar to fluphenazine. It is available in a long-acting depot. It is used for schizophrenia and Tourette’s syndrome (corprolalia and echolalia). Azepines Loxapine (typical), clozapine, olanzapine (atypical) Loxapine properties are similar to phenothiazines Clozapine has fewer extrapyramidal side effect and greater activity against negative symptoms and its use is with 1.3% first year incidence of potentially fatal agranulocytosis. Other atypical drugs are amisulpride, quetiapine, risperidone and zotepine. continued Olanzapine is: As effective as haloperidol in alleviating of positive symptoms. Superior to haloperidol in alleviating of negative symptoms. Fewer extrapyramidal side effects At high doses may cause akathisia, pseudoparkinsonism, and dystonias. Risperidone Its pharmacological effects are similar to olanzapine. But less sedation more orthostatic hypotension, higher incidence of extrapyramidal side effcts. Antidepressant drugs 1. 2. 3. 4. Tricyclic antidepressants Selective serotonin reuptake inhibitors (SSRI) Monamine oxidase inhibitors (MAOI) Others Tricyclic antidepressants Amitriptyline, nortriptyline, imipramine, clomipramine, desipramine They block neuronal reuptake of NE and serotonin, but at different degrees Side effects: Autonomic side effects by blocking muscarinic and a-adrenergic receptors, sedation, induce seizure, orthostatic hypotension Overdose cause life-threatening cardiac arrythmia. Indications Depression Phobic, panic and obsessive compulsive disorder. Sleep disorder (sleepwalking, night terrors, enuresis). Chronic pain syndrome Selective serotonin reuptake inhibitors (SSRI) Fluoxetine, fluvoxamine, paroxetine, sertraline. Most widely used drugs for depression and anxiety disorders (panic & obsessive compulsive disorders) As effective as TCAs But cause fewer autonomic side effects and less sedation. Following overdose, seldom cause cardiac arrhythmia and less likely to induce seizure. Mechanism and pharmacological effects They selectively block reuptake of serotonin. (citalopram and escitalopram are newer SSRI drugs) Adverse effects Fewer sedative, autonomic, cardiovascular side effects. They tend to increase alertness in patients. Most common adverse effects are: nervousness, dizziness, insomnia. Should be used with caution in patients with seizure and hepatic disorders, diabetes, bipolar disorders. Should not be used with MAOI, cause serotonin syndrome. Indications Depression Eating disorders (bulimia nervosa, anorexia nervosa). Panic, phobic and obsessive compulsive disorders. Monoamine oxidase inhibitors They were among the first to be introduced clinically as ADS. They were replaced by TCAs and others whose clinical efficacies were better and whose clinical side effects were less than MAOI. The main examples are Phenelzine, iproniazid and tranylcypramine. They cause irreversible inhibition of the enzyme and do not distinguish between the two main isozymes. Meclobamate acts as a specific inhibitor of MAOA. Others (Atypical) 1. 2. 3. 4. The main claims are: Fewer side effects (sedation and anticholinergic effects) Lower acute toxicity in overdose Action with less delay Efficacy in patients non-responsive to TCA or MAOI Continued 1. 2. They can be divided into two categories: Non-tricyclic structures with similar noradrenaline uptake blocking effects to TCA such as nomifensine and maprotiline Drugs that do not affect amine reuptake such as mianserin, trazodone and bupropion Great minds discuss ideas. Average minds discuss events. Small minds discuss people. THANK YOU!