* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Medication Safety Alert - missed doses
Survey
Document related concepts
Transcript
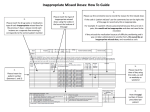
Safe Medicines Practice Group Medication Safety Alert 2 MISSED DOSES - the how’s, the whys and the what’s We felt it timely to re-issue this alert as missed doses continues to be one of the common themes in the Datix reports of medication incidents. Although this is usually classed as an administration error, the causes may occur at any stage in the multi-disciplinary medication process. Risk management needs to be built in at every step. It may occur for outpatients or inpatients and is relevant to all Service Delivery Groups. The majority of missed or delayed doses are not harmful but there may be potentially serious consequences. This alert looks at how doses are missed, why it is important and what we can do to reduce these incidents. How does it happen? Causes can be related to systems, documentation, personnel and environment Poorly hand-written or incomplete prescriptionShort courses section not checked on each medication roundItem not transferred to new prescriptionPatient off the ward at routine medication roundDrug history incompleteStaffing levelsPrescription card not available, in pharmacy or in ward roundMedicine not given at usual time due to blood tests being required, then missedInadequate or inappropriate labelsInterruptions during administration roundOmitted for a reason but not documented, eg patient refusingMedicine not available in pharmacyMedicine not available on the wardMedicine available but cannot be locatedMedicine supplied in unfamiliar packagingMedicine stored in unexpected place eg tablets in fridgeGiven but not recordedPrescribed outside of pharmacy opening hoursNon-formulary drug prescribedItem missed from admission medication history and not prescribed. Why is it important? Can lead to treatment failure. This may not have immediate consequences but can have longer-term problems. May only occur if several doses are missed.Patient may suffer withdrawal or discontinuation symptomsMay lead to concordance issues. Patient may get the message that to miss a few doses is not important.May lead to disruption of therapeutic drug monitoring and cause misinterpretation of levels. Incomplete courses, return of symptoms.Side effects may occur on recommencement of treatment.Re-titration of dose may be required. Which medicines are of particular concern?Antibiotics. Missed doses may lead to infection returning or not being treated. More importantly the microorganism may become resistant to antibiotics. Oral contraceptive pill. Loss of contraceptive cover and pregnancySome antidepressants. Discontinuation symptoms may manifest when one or more doses are missed, in particular paroxetine and venlafaxine.Benzodiazepines. One or more missed doses may lead to withdrawal effects. Lithium. Missed doses can lead to low serum levels and problems with level interpretation and dose adjustments.Anticonvulsants. Missing a dose of medication may lead to a seizure. This is more likely if several doses are missed.Preventative treatments for angina or asthma. Missed doses may cause an angina or asthma attack.Insulin or oral hypoglycaemics. A missed dose may have immediate effects on blood glucose levels several missed doses can lead to poor diabetic control and longer-term consequences on healthClozapine. Missing more than 48 hours of treatment requires re-titration of the dose and consequent reduction in antipsychotic treatment. Risperidone long acting injection and depots antipsychotics. If one dose is missed or delayed the effects will be long term and but not necessarily immediate. TURN OVER TO FIND OUT WHAT WE CAN DO TO REDUCE THE INCIDENCE OF MISSED DOSES What can be done to reduce the risks? – Individuals and units Pharmacists should promptly clarify unclear or inappropriate prescriptions The wards and units should have information about the visiting times of the pharmacists, perhaps by means of a communication book. Visiting times must remain consistent whenever possible. Prescription cards should be left on the ward or unit wherever possible. If the pharmacist is due before the medication is required, wait for them to come rather than sending the card to pharmacy. Aim for the chart to travel as little as possible (this helps prevent them getting lost as well). Units may wish to review conventional method of storage eg types of trolley used. Safe and secure handling of medication should be part of the induction and CPD of all levels of staff who handle medication or prescriptions. Pharmacy should indicate on the prescription whether an item is stock (S) on the unit or dispensed individual for the service user, termed non-stock (NS) and initial and date to show if an item is available on the ward. The person administering the medication must confirm with the prescriber or the pharmacist any prescription that is unclear. The person administering the medication must document the administration, using the appropriate code if medicines are not administered for a reason. If you find it is not possible to administer the medication at the routine round eg if the service user is off the ward it is your responsibility to follow this up and ensure it is given or otherwise document the reasons for not giving. Store medication in an agreed and logical order in the cupboards and the trolleys. Consider labelling the shelves and doors. Ensure supplies are put away promptly and correctly on delivery. Ensure medication no longer required is removed from the trolley. If appropriate the pharmacy can “ring when ready” so that charts and medication do not sit in pigeonholes awaiting delivery when they are needed on the ward. If an item is not available when you come to administer it out of pharmacy opening hours ensure this is followed up by the following shift or leave a message for the pharmacy. If a critical medicine is not available this should be acted on immediately, if out of hours- by using patient’s own medicines, accessing the emergency cupboard or on call pharmacist. If you are taking a medication history on admission consider all sources of information, service user, their GP or their own medication. The community pharmacist can usually tell you if something has been dispensed recently ie is still current. Read all sections of the chart on each administration round. Something new may have been written up and not handed over to you. Start date – treatment will start at the next administration round that day. Treatment will continue until midnight on the stated stop date. What can be done to reduce the risk? – Organisation The Trust wide Medicines Code is available on the intranet and all wards have copiesTraining in medicines management for staffRe-consider conventional methods of supply, for example using patients’ own medication or the one- stop dispensing service used in some areasSupply wherever possible in manufacturers original packs which makes things more recognisable however these have contributed to dose and drug selection errors. Safe Medicines Practice Group – September 2012 Originally produced April 2005 Would you like to join us? We meet every two months at various locations. Please contact Kate Dewhirst, Deputy Chief Pharmacist, email [email protected] for details.