* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download heart and head – af and stroke.
Survey
Document related concepts
Heart failure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Artificial heart valve wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Coronary artery disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Jatene procedure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Transcript
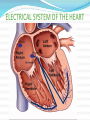
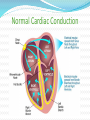
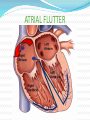
Cardiovascular Care Mark Curnow HASU UCH AIMS OF SESSION Revision Cardiac Anatomy and physiology Electrical Conduction relating to ECG Atrial Fibrillation and stroke Management of Atrial Fibrillation Monitoring on HASU Blood Pressure Management Shock Cardiac Anatomy and Physiology The heart is essentially a sophisticated muscular pump, propelling blood through the vascular system. It is fist sized & lies in the mediastinum between 2nd & 6th ribs. The heart consists of 4 chambers – right & left atria and right & left vent. The chambers are separated by a fibro muscular septum. A series of 4 valves lie between the chambers; between RA & RV - tricuspid valve between RV & pulmonary artery - pulmonary valve between LA & LV - mitral valve between LV & aorta - aortic valve. HEART ANATOMY/BLOOD FLOW HEART ANATOMY/ BLOOD FLOW Cardiac Cycle BLOOD FLOW AROUND THE BODY ELECTRICAL SYSTEM OF THE HEART Normal Cardiac Conduction Cardiac Conduction- Cardiac Cycle SINUS RHYTHM Cardiac Conduction and the ECG DEFINITION OF AF: Abnormal Conduction Most commonly sustained cardiac arrhythmia Atrial fibrillation is a type of arrhythmia in which the upper chambers of the heart (the atria) beat erratically. This erratic beating can be extremely fast (in excess of 300 beats per minute), making it difficult for blood to circulate freely from the atria into the lower chambers of the heart, known as the ventricles. AF is irregularly irregular, having no clear identifiable P waves. Categories: First Episode. Paroxysmal: AF alternating with NSR, spontaneous reversion Persistent: AF alternates with NSR but requires treatment to convert to NSR Permanent: Inability to convert to NSR with therapy DEFINITION OF AF: Abnormal Conduction AF: CAUSES Most cases of AF can be attributed to diseases that affect the structure of the heart over many years. Cardiomegaly: Chronic hypertension – causing enlargement of heart muscle, in particular enlarged atrium. Diseases of the heart valves Pericarditis (swelling) Pericardial effusions (fluid around the heart ) Myocardial Infarction (damage to heart muscle) SSS, (diseases of conduction system) Hyperthyroidism. Emotional stress, Nicotine, High etoh consumption AF AND STROKE: THE PROBLEM AF is very common At least 1.3 % UK population (600,000) have known AF Rising to over 4% in the over 65s and 10.2% in patients over 75 years AF is a major predisposing factor to stroke 16,000 strokes annually in patients with AF in England Of these approx 12,500 are thought to be attributed to AF. AF AND STROKE: THE PROBLEM Incidence of people with AF developing stroke is: 4-6 times higher than a person with no AF. Anticoagulants: Warfarin is superior in stroke prevention in AF. AF strokes tend to be more severe Warfarin reduces stroke risk by 64% Aspirin reduces stroke risk by 22% NICE estimate that approximately 40% of patients in whom warfarin is indicated are not receiving it, amounting to some 166,000 patients nationally HOW AF CAN LEAD TO STROKE HOW AF CAN LEAD TO STROKE Consequence of AF- Thrombus AF: TREATMENTS Dependant on type of AF and treatment aim. Look at history to identify any causes, Echocardiography to look at heart structure. Pharmacological: Digoxin, amiodarone, Flecanide, Beta blockers – Sotolol, Verapamil. Non Pharmacological: Cardioversion, Ablation. Anticoagulation if no contraindication: For prevention of AF related complications. INR 2.o-2.5 People with Disabling ischemic stroke in AF, aspirin 300mg for 2 weeks, then consider warfarin. ATRIAL FLUTTER Atrial flutter, another type of atrial arrythmia originating from a single focus within the atrium (usually the right) creating a rapid atrial rate from 250-400 beats per minute. Due to the impulse being from a single focus, the atrial pattern on the ECG is consistent. As with Atrial Fibrillation, there is an increased risk of stroke. ATRIAL FLUTTER MONITORING ON HASU HASU care provides the patient with 72 hours of acute monitoring. Key element of care for people with acute stroke is the maintenance of cerebral blood flow and oxygenation to prevent further brain damage after stroke (NICE) Cardiac Rhythm (monitor for arrhythmia) Blood Pressure (maintain adequate CPP, the blood pressure gradient across the brain) Respiratory rate/ Oxygen Saturations (detect and treat hypoxia) sats>95% (NICE) Arrhythmia Detection on HASU Bed side monitoring All patients on HASU monitored. All monitors linked to a central station with continuous recording and recall facility. Bedside Monitor vs 24hr Holter Monitor Study (Germany) Sample of 136 patients, 29 were newly diagnosed with PAF . 16 patients diagnosed PAF on bedside monitor prior to commencement of 24hr tape. Of the remaining 13 who were diagnosed PAF from bedside monitor, 24hr tape only picked up 3. Therefore Continuous bedside ECG monitoring is more sensitive than 24-hour Holter ECG for PAF detection in acute stroke/TIA patients Cerebrovasc Dis. 2010;30(4):410-7. BLOOD PRESSURE MANAGEMENT Blood pressure monitoring is critical. Anti-hypertensive treatment in people with acute stroke is recommended only if there is a hypertensive emergency with one of more of the following: hypertensive encephalopathy , hypertensive nephropathy hypertensive cardiac failure/myocardial infarction aortic dissection. Pre-eclampsia/eclampsia Intracerebral haemorrhage with systolic blood pressure over 200 mmHg. (NICE) ESO (2009), Deem Hypertensive emergency as BP > systolic 220 and diastolic >120. BLOOD PRESSURE MANAGEMENT Patients suitable for thrombolysis should have BP no higher than 185/110. (NICE) Avoid drops in blood pressure – maintain an adequate cerebral perfusion pressure. Usually maintained by cerebral blood flow auto regulation. An intracranial event can affect auto regulation, and an increased ICP and a decreased MAP can lower CPP which in turn cause secondary damage to brain. BLOOD PRESSURE TREATMENTS Hypertension: IV GTN: Mainly used in angina/ acute LVF. Causes dilation of smooth muscle within veins and arteries. Leading to reduced myocardial workload and increased myocardial perfusion. Causes hypotension. Can cause throbbing headache. Labetolol Beta Blocker. Blocks beta adrenoreceptors within the body. Reduces blood pressure by altering baroreceptors reflex sensitivity and block peripheral adrenoreceptors. They also cause reduction in heart rate. CHHIPS (2009) SHOCK Types: Cardiogenic: Pump Failure. Diminished cardiac output which severely impairs tissue perfusion. Causes: Myocardial Infarction / Ischemia End stage Cardiomyopathy Signs : Cold, pale clammy skin Hypotension. Tachycardia. Reduced urine output. Confusion. Treatment: Fluid challenge. Inotropes. IABP. Septic Shock Hypovoleamic. CONCLUSION Remember: Close monitoring is essential on HASU Familiarise yourself with the monitor (don't be scared of it) Observe cardiac rhythm for changes, especially irregularities. Monitor Hemodynamics, agree parameters with team and manage changes early. Knowledge leads to empowerment. Always aim to learn from your experiences by questioning, then tell someone else!! THANK YOU