* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download ACTIVE AND PASSIVE MANAGEMENT OF H1N1 FLU
Transmission (medicine) wikipedia , lookup
Globalization and disease wikipedia , lookup
Neonatal infection wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Hepatitis B wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Common cold wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Management of multiple sclerosis wikipedia , lookup
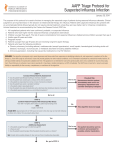
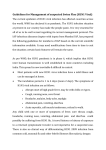
SWINE FLU AWARENESS BY Dr. Mohit Bhutani Dr. D. Himanshu M.D Influenza pandemics & emerging new pandemic threats exist since 1900! 1918 Spanish 1957 Asian 1968 Hong Kong 1977 Russian 1997 Hong Kong 1999 Hong Kong 2003 Dutch 20032008 Global 2009 Global H1N1 H2N2 H3N2 H1N1 H5N1 H9N2 H7N7 H5N1 H1N1 18 cases 2 cases 82 cases 387 cases ~30,000 cases One death 245 deaths 145 deaths 2008 2009 >50 million deaths ~2 million deaths ~1 million deaths <1 million deaths 1918 1957 1968 1977 Pandemic outbreaks Six deaths 2000 Recent outbreaks of influenza The emergence of H1N1 has demonstrated the difficulty in predicting pandemics Nicholson KG, Wood JM, Zambon M. Lancet 2003; 362:1733-1745; WHO, Cumulative number of confirmed human cases of avian influenza A/(H5N1), available at: http://www.who.int/csr/disease/avian_influenza/country/cases_table_2008_09_10/en/index.html (accessed 5 November 2008); CDC, Avian Influenza, available at: http://www.cdc.gov/flu/avian/outbreak.htm (accessed 5 November 2008). Pandemic The guiding principles are:* Early implementation of infection control precautions to minimize nosocomical / household spread of disease Prompt treatment to prevent severe illness & death. Early identification and follow up of persons at risk. *Pandemic Influenza A H1N1 Clinical management Protocol and Infection Control Guidelines Directorate Infrastructure / manpower / material support * Isolation facilities: if dedicated isolation room is not available then patients can be cohorted in a well ventilated isolation ward with beds kept one meter apart. Manpower: Dedicated doctors, nurses, paramedical workers. Equipment: Portable X Ray machine, ventilators, large oxygen cylinders, pulse oxymeters Supplies: Adequate quantities of Personal Protection Equipments (PPE), disinfectants and medications (Oseltamivir, antibiotics and other medicines) *Pandemic Influenza A H1N1 Clinical management Protocol and Infection Control Guidelines Directorate Standard Operating Procedures * Reinforce standard infection control precautions oall those entering the room must use high efficiency N95 masks, gowns, goggles, gloves, cap and shoe cover. Restrict number of visitors and provide them with PPE. Provide antiviral prophylaxis to health care personnel managing the case and ask them to monitor their own health twice a day. Dispose waste properly by placing it in sealed impermeable bags labeled as Bio- Hazard *Pandemic Influenza A H1N1 Clinical management Protocol and Infection Control Guidelines Directorate MANAGEMENT The first thing is to differentiate between a flu and a cold CATEGORISATION OF CASES* MILD OR UNCOMPLICATED ILLNESS PROGRESSIVE ILLNESS SEVERE OR COMPLICATED ILLNESS *Updated Interim Recommendations for the Use of Antiviral Medications in the Treatment and Prevention of Influenza for the 2009-2010 Season Mild or Uncomplicated illness – Fever – Cough – Sore throat – Rhinorrhea – Muscle pain – Headache – Chills – Malaise – Diarrhea and vomiting • These patients do not require treatment with anti-viral drugs as they do not need hospitalization. TREATMENT ALGORITHM FOR MILD DISEASE HIGH RISK GROUP* Children younger than 2 years old Adults 65 years of age or older Pregnant women and women up to 2 weeks postpartum (regardless of how the pregnancy ended) Persons with certain medical conditions: asthma, chronic lung disease, heart disease, blood disorders, kidney and liver disease, diabetes mellitus, immunocompromised and obese *Updated Interim Recommendations for the Use of Antiviral Medications in the Treatment and Prevention of Influenza for the 2009-2010 Season Progressive illness Typical symptoms plus – Chest pain – Tachypnea i.e. respiratory rate > 30 – Hypoxia i.e. SpO2 < 94% at room air – Labored breathing in children – Low blood pressure i.e. SBP < 90mmHg – Confusion – Severe dehydration – Exacerbations of chronic conditions These patients require urgent hospitalization and treatment. Severe or Complicated Illness • Abnormal CXR • Requiring mechanical ventilation • Encephalitis • Encephalopathy • Organ failure • Myocarditis • Rhabdomyolysis • Invasive secondary bacterial infection based on laboratory testing or clinical signs (e.g. persistent high fever and other symptoms beyond three days) These patients require prompt admission and treatment with anti-viral drugs. Whom to test The following people should receive influenza diagnostic testing – people who are hospitalized with suspected flu i.e. patients with progressive or severe/complicated disease – Symptomatic patients in high risk group – Additional people may be recommended for testing based on the clinical judgment of their health care provider • During 2009 H1N1 CDC considered that most people with flu symptoms would not require testing because the test results usually do not change the way one is treated. *Updated Interim Recommendations for the Use of Antiviral Medications in the Treatment and Prevention of Influenza for the 2009-2010 Season How to treat !!! • Antiviral drugs: oseltamivir (oral), zanamivir (inhaled) • Initiate treatment as early as possible after onset of symptoms • Treat empirically before diagnostic test results are reported *Updated Interim Recommendations for the Use of Antiviral Medications in the Treatment and Prevention of Influenza for the 2009-2010 Season • OSELTAMIVIR : oral (cap/suspension) Oseltamivir is the recommended drug both for prophylaxis and treatment. Neuraminidase inhibitor Pregnancy category ‘c’ SCHEDULE ADVERSE EFFECTS(oseltamivir) • >10%- gastrointestinal- vomiting, nausea , pain abdomen • 1%- conjuctivitis • 1%- epistaxis • <1%- anaphylactic reaction, pseudomembranous colitis, SJS/TEN, abnormal LFT, neuropsychiatric events • Zanamivir – inhalational .(Relenza®) FDA-approved for the treatment of influenza in patients 7 years of age and older Caution Bronchospasm in asthma patients SINGLE DOSE Peramivir A third neuraminidase inhibitor formulated for intravenous (IV) administration for 18yrs and older pt. • Treatment approved only if: (1) the patient has not responded to either oral or inhaled antiviral therapy; (2) drug delivery by a route other than IV is not expected to be dependable or is not feasible • AMANTADINE • RIMANATADINE Not recommended due to widespread resistance in 2009 H1N1 strain Duration of antiviral therapy* Recommended duration: 5 days Hospitalized patients with severe infections might require longer treatment courses Treatment is most effective when started in the first 48 hours of illness Limited data from observational studies suggests, treatment started 48 hours after onset of illness also reduced mortality/ duration of hospitalization *Updated Interim Recommendations for the Use of Antiviral Medications in the Treatment and Prevention of Influenza for the 2009-2010 Season Supportive therapy • IV Fluids. • Oxygen therapy/ ventilatory support • Antibiotics for secondary infection • Vasopressors for shock • Paracetamol or ibuprofen for fever, myalgia and headache. • Avoid smoking. • For sore throat, short course of topical decongestants, saline nasal drops, throat lozenges and steam inhalation. • Salicylate / aspirin is strictly contra-indicated in any influenza patient due to its potential to cause Reye’s syndrome. Discharge Policy • Patients responded within 2-3 days can be discharged after 5 days of treatment. No need for a repeat test. • Patients who continue to have symptoms of fever, sore throat etc. even on the 5th day should continue treatment for 5 more days. • If symptomatic even after 10th day of treatment in the absence of secondary infection, retest • If positive, do check for resistance • While discharging, educate family on personal hygiene and infection control measures at home ACTIVE PREVENTION Antiviral Chemoprophylaxis of exposed individuals INFECTIOUS PERIOD One day before fever begins until 24 hours after fever ends or 7 days after onset of symptoms. Children may spread the virus for a longer period Mode of exposure • Droplet exposure of mucosal surfaces (e.g. nose, mouth, and eyes) by respiratory secretions from coughing or sneezing • Contact, usually of hands, with an infectious patient or fomites followed by self-inoculation of virus onto mucosal surfaces such as those of the nose, mouth, and eyes • Small particle aerosols in the vicinity of the infectious individual. Who may be considered for antiviral chemoprophylaxis • The following persons who are a close contact of a person with suspected or confirmed H1N1 influenza during the infectious period: – Persons at high risk for complications of influenza; – Health care workers and emergency medical personnel; – Pregnant women. Whom not to treat chemoprophylactically • Groups of healthy children or adults based on potential exposures in the community, workplace, school, camp or other settings; • If >48 hours have elapsed since the last close contact • The close contact did not occur during the infectious period Oseltamivir AND Zanamivir drug of choice • Prophylaxis should be provided till 10 days after last exposure Use of the Pandemic (H1N1) 2009 vaccines 1. Inactivated – killed • Produced by growing virus in chicken eggs • Given by injection into the upper arm. In infants and younger children the thigh is the preferred site for the vaccine shot. TYPES: • Trivalent VAXIGRIP (flu shot: A/H1N1, A/H3N2, and B) • 50-80% protection • Can be given in pregnancy • Single dose in adults • Immunosuppressed and in children < 10 yr two doses 4 wks apart • S/E: fever ; GBS 1 in 1 lac . C/I – ALLERGIC pts. 2.LIVE ATTENUATED • administered by nasal spray. • healthy individuals 2-49 yr of age • Contraindicated in – – pregnancy immunosuppresed • 90% protection rate • Not advised for health care professionals Influenza vaccines only become effective about 14 days after vaccination Who will receive priority for vaccination? • WHO recommend that health workers be given first priority for early vaccination to protect themselves and their patients • Those caring for high risk individuals who cannot receive vaccination • Other groups at higher risk for severe illness o pregnant women o aged above 6 months with one of several chronic medical conditions, o healthy adults of 65 years of age and above PASSIVE PREVENTION Guidelines on Infection control Measures • FOR HEALTH CARE INDIVIDUALS Personal Protection Equipments reduces the risk of infection if used correctly • Gloves (nonsterile), • Mask (high-efficiency mask) / Three layered surgical mask, • Long-sleeved cuffed gown, • Protective eyewear (goggles/visors/face shields), • Cap (may be used in high risk situations where there may be increased aerosols), • Plastic apron if splashing of blood, body fluids, excretions and secretions is anticipated N95 Respirator • Filters 95% of airborne particulates *NIOSH- National Institute for Occupational Safety and Health. Agency under CDC. During Hospital Care o The patient should be admitted directly to the isolation facility and continue to wear a three layer surgical mask O The identified medical, nursing and paramedical personnel attending the suspect/ probable / confirmed case should wear full complement of PPE . o If splashing with blood or other body fluids is anticipated, a water proof apron should be worn over the PPE • Perform hand hygiene before and after patient contact and following contact with contaminated items, whether or not gloves are worn. Hand washing and Hand rub • The virus is inactivated by – 70% ethanol, – 5% benzalkonium chloride (Lysol) and 10% sodium hypochlorite. • Patient rooms/areas should be cleaned at least daily and finally after discharge of patient. To avoid possible aerosolization of the virus, damp sweeping should be performed. • Recommended bed to bed distance should be at least 1m • All waste generated from influenza patients is infectious clinical waste and should be treated and disposed in accordance with national regulations. Guidelines on Infection control Measures FOR GENERAL POPULATION IN COMMUNITY • Wash hands frequently with soap and water. If soap and water are not available, use an alcohol-based hand rub • Cover your mouth and nose with a tissue when coughing or sneezing • Avoid touching your eyes, nose and mouth • People who are sick with an influenza-like illness should stay home for at least 24 hours after fever is gone except to get medical care or for other necessities • Avoid close contact (i.e. being within about 6 feet) with persons with Influenza like illness THANK YOU