* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Calcium-Handling Abnormalities Underlying Atrial
Survey
Document related concepts
Transcript
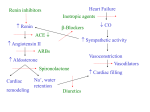
Calcium-Handling Abnormalities Underlying Atrial Arrhythmogenesis and Contractile Dysfunction in Dogs With Congestive Heart Failure Yung-Hsin Yeh, MD;* Reza Wakili, MD;* Xiao-Yan Qi, PhD; Denis Chartier, BSc; Peter Boknik, PhD; Stefan Kääb, MD; Ursula Ravens, MD; Pierre Coutu, PhD; Dobromir Dobrev, MD; Stanley Nattel, MD Downloaded from http://circep.ahajournals.org/ by guest on May 11, 2017 Background—Congestive heart failure (CHF) is a common cause of atrial fibrillation. Focal sources of unknown mechanism have been described in CHF-related atrial fibrillation. The authors hypothesized that abnormal calcium (Ca2⫹) handling contributes to the CHF-related atrial arrhythmogenic substrate. Methods and Results—CHF was induced in dogs by ventricular tachypacing (240 bpm ⫻2 weeks). Cellular Ca2⫹-handling properties and expression/phosphorylation status of key Ca2⫹ handling and myofilament proteins were assessed in control and CHF atria. CHF decreased cell shortening but increased left atrial diastolic intracellular Ca2⫹ concentration ([Ca2⫹]i), [Ca2⫹]i transient amplitude, and sarcoplasmic reticulum (SR) Ca2⫹ load (caffeine-induced [Ca2⫹]i release). SR Ca2⫹ overload was associated with spontaneous Ca2⫹ transient events and triggered ectopic activity, which was suppressed by the inhibition of SR Ca2⫹ release (ryanodine) or Na⫹/Ca2⫹ exchange. Mechanisms underlying abnormal SR Ca2⫹ handling were then studied. CHF increased atrial action potential duration and action potential voltage clamp showed that CHF-like action potentials enhance Ca2⫹i loading. CHF increased calmodulin-dependent protein kinase II phosphorylation of phospholamban by 120%, potentially enhancing SR Ca2⫹ uptake by reducing phospholamban inhibition of SR Ca2⫹ ATPase, but it did not affect phosphorylation of SR Ca2⫹-release channels (RyR2). Total RyR2 and calsequestrin (main SR Ca2⫹-binding protein) expression were significantly reduced, by 65% and 15%, potentially contributing to SR dysfunction. CHF decreased expression of total and protein kinase A–phosphorylated myosin-binding protein C (a key contractile filament regulator) by 27% and 74%, potentially accounting for decreased contractility despite increased Ca2⫹ transients. Complex phosphorylation changes were explained by enhanced calmodulin-dependent protein kinase II␦ expression and function and type-1 protein-phosphatase activity but downregulated regulatory protein kinase A subunits. Conclusions—CHF causes profound changes in Ca2⫹-handling and -regulatory proteins that produce atrial fibrillation– promoting atrial cardiomyocyte Ca2⫹-handling abnormalities, arrhythmogenic triggered activity, and contractile dysfunction. (Circ Arrhythmia Electrophysiol. 2008;1:93-102.) Key Words: atrial fibrillation 䡲 congestive heart failure 䡲 delayed afterdepolarization 䡲 calcium 䡲 sarcoplasmic reticulum C ongestive heart failure (CHF) is a common cause of atrial fibrillation (AF). Both reentrant and triggered mechanisms have been implicated in AF.1 Although CHF induces a substrate for atrial reentry,2 there is also evidence for a role of focal drivers and triggered activity in CHF-related AF.3– 6 Dogs with atrial tachycardia remodeling have calcium (Ca2⫹)-handling abnormalities, reduced Ca2⫹ transients, and cardiac ryanodine receptor (RyR2) dysfunction.7,8 Ca2⫹-handling abnormalities may play a role in CHF-related AF, but there are no published descriptions of atrial Ca2⫹ handling in patients or clinically relevant animal models with CHF-associated AF substrates. Accordingly, the present study was designed to evaluate atrial cardiomyocyte Ca2⫹ handling, and related protein expression and phosphorylation, in a canine CHF model. Editorial see p 77 Clinical Perspective see p 102 Methods A detailed description of materials and methods used in the study is available in the online Data Supplement. Received November 22, 2007; accepted February 29, 2008. From the Department of Medicine and Research Center, Montreal Heart Institute and Université de Montréal (Y.H.Y., R.W., X.Q., D.C., P.C., S.N.), Montreal, Canada; the Department of Pharmacology and Toxicology (R.W., U.R., D.D.), Dresden University of Technology, Dresden, Germany; Chang Gung Memorial Hospital and Chang Gung University (Y.H.Y.), Tao-Yuan, Taiwan; the Department of Pharmacology and Toxicology (P.B.), University of Münster, Münster, Germany; and Ludwig-Maximilians University, Department of Medicine I, Klinikum Grosshadern (R.W., S.K.), Munich, Germany. The online-only Data Supplement can be found at http://circep.ahajournals.org/cgi/content/full/CIRCEP.107.754788/DC1. Correspondence to Stanley Nattel, MD, 5000 Belanger St E, Montreal, Quebec, Canada, H1T 1C8. E-mail [email protected] *Drs Yeh and Wakili contributed equally to this work. Drs Nattel and Dobrev share senior authorship. © 2008 American Heart Association, Inc. Circ Arrhythmia Electrophysiol is available at http://circep.ahajournals.org 93 DOI: 10.1161/CIRCEP.107.754788 94 Circ Arrhythmia Electrophysiol June 2008 Animal Model The animal model was prepared as previously described.9 Forty adult mongrel dogs (22 to 36 kg) were divided into 2 groups: (1) control (n⫽20) and (2) 2-week ventricular tachypacing–induced CHF (n⫽20). CHF dogs had unipolar pacing leads inserted fluoroscopically into the right ventricular apex, which were programmed at 240 bpm for 2 weeks. On the days of study, dogs were anesthetized with morphine (2 mg/kg SC) and ␣-chloralose (120 mg/kg IV, followed by 29.25 mg/kg per hour) and ventilated mechanically. AF (irregular atrial rhythm ⬎400 bpm) was induced by burst pacing. Mean AF duration was determined on the basis of multiple AF inductions in each dog, as an index of the AF-maintaining substrate (for details see the Methods section in the online Data Supplement). AF duration (mean⫾SEM) was then calculated for each experimental group as an indicator of the ability of each group to sustain AF. Hemodynamic data were obtained with fluid-filled catheters and transducers. Table. Hemodynamic Data Control (n⫽20) CHF (n⫽20) Systolic BP, mm Hg 132⫾5 Diastolic BP, mm Hg 82⫾4 114⫾3* 67⫾2* LVSP, mm Hg 131⫾5 113⫾4* LVEDP, mm Hg 4.9⫾0.5 15.3⫾1.0† LAP, mm Hg 4.0⫾0.6 15.4⫾0.9† RAP, mm Hg 2.7⫾0.5 DAF, s 26⫾8 9.6⫾0.4† 1564⫾106* *P⬍0.01, †P⬍0.001 vs control. BP indicates blood pressure; LVSP, LV systolic pressure; LVEDP, LV end-diastolic pressure; LAP and RAP, LA and RA mean pressure; and DAF, duration of AF. Cardiomyocyte Isolation Downloaded from http://circep.ahajournals.org/ by guest on May 11, 2017 Right atrial (RA) and left atrial (LA) preparations were dissected and coronary perfused at ⬇10 mL/min for cardiomyocyte isolation as previously described.9 RA and LA cells were stored separately in Tyrode solution with 200 mol/L Ca2⫹. Measurement of Cell Contraction and Ca2ⴙ Fluorescence Cell-shortening measurements, based on the average of 10 consecutive beats, were obtained from field-stimulated cardiomyocytes with a video edge detector coupled to a charged-coupled device camera. Edge-detection cursors were positioned at both cell ends to measure whole-cell shortening. [Ca2⫹]i transients were recorded with microfluorimetry.10 Cardiomyocytes were incubated with indo-1 AM (5 mol/L) for 4 to 5 minutes. The cells were then superfused with Tyrode solution for 10 minutes to allow intracellular de-esterification. Cardiomyocytes were excited with ultraviolet light (340 nm), and emission ratios (R400/500) were measured through a 10-m aperture focused at the cardiomyocyte center. Ratiometric Ca2⫹i measurements were converted into intracellular Ca2⫹ concentration ([Ca2⫹]i) with the formula [Ca2⫹]i⫽Kd⫻⫻(R400/500 ⫺Rmin)/(Rmax⫺R400/500).10 Experimentally determined Rmin, Rmax, and  averaged 0.43, 2.34, and 1.79, respectively. Sarcoplasmic reticulum (SR) Ca2⫹ content was evaluated with 15-second 10-mmol/L caffeine applications via a rapid-switching perfusion system. For frequency-response measurements, a minimum of 4 Ca2⫹ transients (at 0.1 Hz) or a maximum of 20 Ca2⫹ transients (⬎1.0 Hz) were time-averaged. The decay time constant () was based on a monoexponential fit to the [Ca2⫹]i decay curve. Cellular Electrophysiology LA cells were used for arrhythmogenic action potential (AP) studies and RA tissue for biochemistry. APs were recorded with whole-cell perforated-patch methods. Borosilicate glass electrodes (1.0 mm outer diameter) had tip resistances between 3 and 5 M⍀. Pipette tips were filled with nystatin-containing (60 g/mL) intracellular solution. Junction potentials averaged 15.9 mV and were corrected for APs. For solution contents, see the online Data Supplement Methods section. All recordings were obtained at 35⫾0.5°C. The AP voltage-clamp (whole-cell perforated patch) technique was used to study AP-dependent effects on [Ca2⫹]i transients. [Ca2⫹]i transients were recorded from LA cardiomyocytes subjected to typical AP waveforms from control and CHF cardiomyocytes at 2 Hz for sequential 2-minute periods (in randomized order). Western Blot and Phosphatase Activity Measurements RA tissue homogenates were prepared and protein concentrations determined with Amido-black 10B.11 Proteins were fractionated on SDS-polyacrylamide gels and transferred to nitrocellulose membranes. Western blotting was performed with primary antibodies as previously described.12 A detailed list of antibodies and sources is presented in the online Data Supplement Methods section. Protein bands were visualized by electrochemoluminescence. Phosphatase activity was measured in atrial homogenates.13 Okadaic acid (3 nmol/L) was used to differentiate between PP1 and PP2A activities.13 Data Analysis Group data are presented as mean⫾SEM. Repeated-measures analyses were performed with 2-way analysis of variance (ANOVA), followed by Bonferroni-corrected t tests for statistically significant ANOVAs. Nonpaired t tests were applied for single 2-group comparisons and paired t tests for single repeated measures within one group. Contingency analyses were measured by 2 test. Two-tailed P⬍0.05 was considered statistically significant. The authors had full access to the data and take responsibility for the integrity of the data. All authors have read and agreed to the manuscript as written. Results Hemodynamics and AF Duration Hemodynamic indices and in vivo electrophysiology data are shown in the Table. Arterial pressures were significantly reduced in CHF dogs, whereas left ventricle end-diastolic and LA and RA pressures were increased. CHF significantly prolonged AF duration. APs, Cell Shortening, and Ca2ⴙ Transients CHF cardiomyocytes were enlarged, with a mean capacitance of 120⫾6 pF, versus 91⫾3 pF for control (n⫽25/group, P⬍0.01). APs obtained by averaging all available recordings from each group at 1 Hz are shown in Figure 1A, with mean action potential duration (APD) data provided in the inset. APDs were significantly prolonged by CHF in both LA and RA over a wide range of frequencies (online Data Supplement Figure I). Figure 1B and 1C show recordings of steady-state cell shortening and Ca2⫹ transients. Cell shortening was significantly decreased in CHF cells (Figure 1D), whereas Ca2⫹ transients were larger. Figure 2 shows detailed analyses of LA and RA [Ca2⫹]i transients. CHF increased diastolic [Ca2⫹]i and [Ca2⫹]i transients at all frequencies from 0.1 to 2 Hz (Figure 2A through 2D). The time to peak and decay time constants of [Ca2⫹]i Ca2ⴙ Handling in Failing Atrium A 300 *** *** 150 0 B CHF Control 0 0 20 mV APD90 APD50 Cell shortening (µm) Yeh et al 0 CHF -5 CTL -15 0 C 1000 500 1500 2000 ms 1000 [Ca2+]i (nM) 800 CHF CTL Figure 1. A, AP waveforms obtained by digitally averaging all AP recordings from LA cardiomyocytes at 1 Hz from control (CTL, left) and CHF (right) dogs. Inset: Mean⫾SEM results at 1 Hz (n⫽16, n⫽37 for CTL and CHF, respectively; ***P⬍0.001). B and C, Recordings of cell shortening (B) and Ca2⫹ transients (C) from single control (CTL) and CHF cardiomyocytes. D, Mean⫾SEM cell shortening as a function of pacing frequency (n⫽15 and 12 for control and CHF, respectively; ***P⬍0.001, effect of group: CHF vs control). E, AP-clamp results; left, Ca2⫹ transient recordings obtained with CHF and control waveforms in a control LA cell; right, corresponding mean⫾SEM. Ca2⫹ transient amplitudes (n⫽6 cells, **P⬍0.01). -10 APD (ms) 50 ms 600 1000 CHF-AP 800 [Ca2+]i (nM) 600 [Ca2+]i (nM) 400 AP-clamp 400 300 CTL-AP 200 100 900 800 700 600 500 400 300 200 100 0 ** CHF 200 CTL 0 D CTL-AP CHF-AP 100 ms CHF Control 0 0 14 12 10 8 6 4 2 0 1000 500 1500 CTL 2000 ms CHF *** 0.0 0.5 1.0 1.5 2.0 Hz (LA) and 2F (RA). CHF increased caffeine-induced Ca2⫹ transients by ⬇85% in LA and ⬇50% in RA (Figure 2E and 2F insets). In ventricular cardiomyocytes, [Ca2⫹]i decay depends mainly on Ca2⫹ extrusion by NCX.14 The decay time constant of the caffeine-induced transient was comparable for CHF and control in LA and RA (online Data Supplement Figure IIC and IID). transient were similar for CHF and control (online Data Supplement Figure IIA through IIB). APD prolongation due to CHF could contribute to Ca2⫹i loading, so we performed AP-clamp experiments, imposing the control and CHF waveforms at 2 Hz in control atrial myocytes. [Ca2⫹]i transients obtained in 1 cell with either AP waveform are shown in Figure 1E (left). CHF APs induced a statistically significant increase (⬇18%) in [Ca2⫹]i transient amplitudes (Figure 1E, right). SR Ca2ⴙ Content Spontaneous Ca2ⴙ Transient Events, Delayed Afterdepolarizations, Triggered APs, and Pharmacological Effects To assess changes in SR Ca2⫹ content, we paced cells for 1 minute at 1 Hz and then rapidly applied 10 mmol/L caffeine. Caffeine-induced Ca2⫹ transients are illustrated in Figure 2E The results in Figures 1 and 2 show larger SR Ca2⫹ loads and Ca2⫹ transients in CHF atria versus control, with LA behaving similarly to RA. We therefore determined whether CHF LA 400 600 *** *** 200 0 0.0 0.5 1.0 1.5 400 *** *** 0.5 1.0 1.5 CTL *P<0.05 CHF LA ∆[Ca2+] Caffeine (nM) 2000 1000 500 0 1200 800 RA *** 0 ** 0.0 0.5 CTL 15 20 Caffeine (nM) i ** 1500 400 10 ∆[Ca2+] 2000 CHF 25 30 [Sec] * 1.0 1.5 2.0 600 * ** * * * 400 200 0 0.0 0.5 1.0 1.5 2.0 f (Hz) **P<0.01 i CTL CHF *** f (Hz) F [Ca2+]i (nM) 2000 1600 5 *** 200 2.0 1500 0 * 600 400 Amplitude RA 800 f (Hz) f (Hz) E *** *** 200 0 0.0 2.0 800 *** D Amplitude LA [Ca 2+]i (nM) [Ca 2+ ]i (nM) *** *** C [Ca 2+]i (nM) 600 *** Diastolic [Ca2+]i RA B Diastolic [Ca2+]i LA [Ca 2+ ]i (nM) A [Ca2+]i (nM) Downloaded from http://circep.ahajournals.org/ by guest on May 11, 2017 Cell shortening (µm) E 95 2000 1000 1600 500 0 1200 800 CTL CHF CHF 400 CTL 0 5 10 15 20 25 30 [Sec] Figure 2. Mean⫾SEM. Ca2⫹ transient indices. A and B, [Ca2⫹]i diastolic levels in left (A) and in right atrial (B) cells. C and D, Ca2⫹ transient amplitude in left (C) and right atrial cells (D) (n⫽20 to 24 cells/group; *P⬍0.05, **P⬍0.01, ***P⬍0.001 CHF vs control). E and F, Caffeine-induced Ca2⫹ transients in control and CHF left (E) and right atrial (F) cardiomyocytes. A 10-mmol/L local caffeine concentration was achieved in ⬍500 ms with a laminar-flow rapid solution-switching system, producing Ca2⫹ transients, which are indicated by arrows. Insets: Mean⫾SEM caffeineinduced Ca2-transient amplitudes of LA (E) and RA (F) (n⫽12/group; **P⬍0.01, ***P⬍0.001). 96 Circ Arrhythmia Electrophysiol June 2008 CTL A B CHF Post-pacing follow-up 1 min 2 Hz 30 secs Ca2+ transient events/run 14 ** P<0.003 ** 12 10 8 6 (28) 4 2 (19) 0 CTL CHF CTL D ** 100 2 sec CHF Cells with events (%) Downloaded from http://circep.ahajournals.org/ by guest on May 11, 2017 80 60 40 20 0 -20 -40 -60 -80 80 60 40 20 0 -20 -40 -60 -80 50 mV C 80 23/26 60 40 20 6/24 0 2 Hz 1 min Post-pacing follow-up 30 sec Post-pacing APs Figure 3. A, Spontaneous Ca2⫹ transient events after Ca2⫹ loading by 30 seconds of 2-Hz pacing. B, Mean⫾SEM postpacing Ca2⫹ transient events (cell numbers provided in brackets). C, Triggered APs (vertical arrows), after Ca2⫹ loading by 1 minute of pacing at 2 Hz. D, Percentage of cardiomyocytes showing triggered APs (**P⬍0.003). cardiomyocytes are predisposed to abnormal Ca2⫹ release– associated arrhythmic events. We first recorded spontaneous Ca2⫹ transients after a 30-second period of pacing at 2 Hz. The cessation of cell stimulation was followed by occasional nonstimulated Ca2⫹ transients in control cells (Figure 3A, top). In CHF (bottom), many more spontaneous Ca2⫹ transients were seen. Nonstimulated Ca2⫹ transients were ⬇5-fold more frequent in CHF cells (Figure 3B). Figure 3C shows whole-cell perforated-patch AP recordings immediately after 1-minute stimulation at 2 Hz. In control cells, triggered APs were rare, whereas triggered activity was greatly increased in CHF cells (Figure 3D). Triggered activity was accompanied by prominent diastolic membrane oscillations that sometimes appeared as delayed afterdepolarizations and at other times transitioned smoothly into triggered APs, suggesting abnormal automaticity. To elucidate the basis of diastolic membrane-potential oscillations and triggered APs occurring after the Ca2⫹ loading by rapid pacing, we studied the response to pharmacological manipulations. Figure 4A (top) shows spontaneous AP generation and diastolic oscillatory activity after 2-Hz pacing in a CHF cardiomyocyte. Ryanodine, an SR Ca2⫹ release channel inhibitor, induced quiescence in this and 5 other similar CHF cells. The Na⫹/Ca2⫹-exchanger (NCX) suppression with Na⫹- and Ca2⫹-free medium produced similar responses (Figure 4B). No change in spontaneous activity was seen on If inhibition with 2 mmol/L Cs⫹ (Figure 4C). Some CHF atrial cardiomyocytes presented spontaneous activity and APs without pacing-induced Ca2⫹ loading (online Data Supplement Figure III). These spontaneous events were completely eliminated by 10 mol/L ryanodine (n⫽4 cells), whereas CsCl had no effect (n⫽4 cells). These results indicate that CHF-induced diastolic membrane potential instability leads to triggered activity via mechanisms involving SR Ca2⫹ release through ryanodine receptors and associated arrhythmogenic Na⫹- and Ca2⫹-exchange currents. Ca2ⴙ Handling and Myofilament Proteins To gain insights into potential abnormalities of Ca2⫹ handling and contractile protein systems in CHF atria, we performed Western blots with antibodies that recognize total and phosphorylated forms. Protein-band intensities were normalized to those of GAPDH on the same lanes (GAPDH intensities did not differ between CHF and control atria). The expression of total phospholamban was similar in CHF and control atria (Figure 5A). Phospholamban phosphorylation by protein kinase A (PKA) at Ser16 (Ser16-P) and by CaMKII at Thr17 (Thr17-P) functionally enhances SERCA2a Ca2⫹ uptake. Ser16-P-phospholamban expression was unchanged in CHF, but Thr17-P-phospholamban increased by ⬇85%. Fractional phospholamban PKA phosphorylation (Ser16-P-phospholamban–to–total phospholamban ratio) was unchanged in CHF, Yeh et al Ca2ⴙ Handling in Failing Atrium 97 100 mV A Ryanodine 10 μM B Figure 4. Postpacing diastolic membrane potential oscillations and triggered activity in CHF cells before (left) and after (right) administration of 10 mol/L ryanodine (A), Na⫹- and Ca2⫹-free external solution (Na⫹ replaced by equimolar Li⫹) (B), and 2 mmol/L CsCl (C) (dashed lines represent 0 mV level). Similar results were obtained in 6 experiments of each type. The mean number of triggered APs per run averaged 13.3⫾4.5 before and 13.0⫾3.1 after 2 mmol/L CsCl application (P⫽NS). 2 sec Na+ free Ca2+ free C Cs+ 2 mM post pacing follow-up 3 min post pacing follow-up 3 min 2 Hz 1 min CTL CTL CHF CHF A B PLB-Ser16 7 kDa PLB-Thr17 7 kDa SERCA2a 565 kDa RyR2-Ser2809 565 kDa RyR2-Ser2815 565 kDa CSQ 53 kDa NCX1 120 kDa 37 kDa CTL CHF 200 150 100 * 100 * * 50 50 0 X1 0 C Relative to CTL (A.U.) 150 GAPDH yR 2 P2 80 9 P2 81 5 P2 R 80 yR 9 2 P R 281 yR 5 2 C SQ Se 200 R PL r1 B 6 PL -P L Th B B r1 7PL PL B B LB 7- 6P r1 Th Se r1 PL B a * * * a2 We have shown that atrial Ca2⫹ handling is significantly disturbed in dogs with experimental CHF. Ca2⫹ overload was manifested as increased diastolic Ca2⫹ concentrations, Ca2⫹ Relative to CTL (normalized to GAPDH) * rc Main Findings CTL CTL CHF CHF 37 kDa CTL CHF Se Discussion 105 kDa GAPDH 350 300 250 200 150 100 50 0 of protein function,8,12,13 for a variety of Ca2⫹ handling and contractile proteins. To assess the underlying mechanisms, we analyzed the expression of key protein kinases and protein phosphatases. CHF increased expression and autophosphorylation of the cytosolic CaMKII␦ isoform by 123% and 114%, respectively (Figure 7A). PKA expression was unchanged for PKAC, whereas PKAc (PKA catalytic subunit) and PKAIIa (PKA regulatory subunit) was decreased by 72% (Figure 7B). Because RyR2 and MyBP-C are dephosphorylated primarily by protein phosphatase (PP)1, their reduced PKA phosphorylation may be caused by the increased PP1 activity. Consistent with this notion, total proteinphosphatase activity was 34% higher in CHF, PP1 activity was increased by 83%, and PP2A activity was unchanged (Figure 7C). Protein expression of PP1 and PP2A catalytic subunits was unchanged in CHF (Figure 7D). RyR2-Total 7 kDa PLB-Total Relative to CTL (Normalized to GAPDH) Downloaded from http://circep.ahajournals.org/ by guest on May 11, 2017 whereas fractional CaMKII phospholamban phosphorylation increased by ⬇120%. CHF decreased SERCA2a protein expression (by ⬇35%). CHF resulted in a 65% decrease in total RyR2 protein expression (Figure 5B) and a 73% decrease in PKA-phosphorylated RyR2 (Ser2809-P). Fractional RyR2 phosphorylation (ratios of Ser2809-P-RyR2 and Ser2815-P-RyR2 to total RyR2) was not significantly altered by CHF. Calsequestrin, a major SR Ca2⫹ buffer and regulator of RyR2 function,15 was reduced ⬇15% in CHF. No significant changes were noted for NCX1. Expression values for thin myofilament proteins troponin (Tn)-I and Tn-C are shown in Figure 6A. Total Tn-I expression, PKA-phosphorylated (Ser23/24)–to–total Tn-I ratio, and total Tn-C were unchanged by CHF. However, total thick-myofilament myosin-binding protein C (MyBP-C) and PKA-phosphorylated MyBP-C (Ser282-P) were significantly decreased by ⬇27% and ⬇74%, respectively (Figure 6B). The Ser282-P MyBP-C/total MyBP-C ratio was also reduced by 67% in CHF, and phosphorylated myosin light chain-2a protein (MLC2a) was decreased by 46%. The data in Figures 5 and 6 show potentially important CHF-induced changes in phosphorylation, a critical regulator N 2 Hz 1 min Figure 5. A, Top: Examples of total phospholamban (PLB), Ser16-P PLB, and Thr17-P PLB, SERCA2a, and GAPDH immunoblots. Bottom: Mean⫾SEM protein-band intensities normalized to GAPDH, relative to control (n⫽14 control and 10 CHF atria/analysis, *P⬍0.05 vs control). B, Top: Examples of total RyR2, Ser2809-P RyR2 and Ser2815-P RYR, calsequestrin (CSQ), NCX1, and GAPDH immunoblots. Bottom: Mean⫾SEM protein-band intensities of total RyR2, Ser2809-P RyR2, and Ser2815-P RyR2 relative to control, and CSQ and NCX1 normalized to GAPDH, expressed relative to control (n⫽10 control and 6 CHF atria for RyR2, n⫽14 control and 10 CHF for calsequestrin, n⫽10 control and 8 CHF for NCX1; *P⬍0.05 vs control). 98 Circ Arrhythmia Electrophysiol CTL CTL CHF CHF A June 2008 CTL CTL CHF CHF B MyBP-C 150 kDa Tn-I Ser23/24 30 kDa MyBP-C-P 150 kDa Tn-C-Total 21 kDa MLC2a 21 kDa GAPDH 37 kDa GAPDH 37 kDa 200 Relative to CTL (Normalized to GAPDH) 30 kDa Relative to CTL (Normalized to GAPDH) Tn-I-Total CTL, n=10 CHF, n=8 150 100 50 0 Tn-I 200 CTL, n=14 CHF, n=10 150 100 * 50 * MyBP-C P282 P282 MLC2a-P MyBP-C afterdepolarizations in cardiomyopathic cats. Epicardial mapping suggests focal drivers during AF in CHF dogs,3,5,17 and focal-driver ablation can terminate atrial tachyarrhythmias.3 In vivo pharmacological responses consistent with atrial Ca2⫹-dependent triggered activity have been noted in animals with CHF.4 Although atrial fibrosis favors atrial reentry, reentrant activity is rarely triggered by single atrial extrasystoles, requiring bursts of rapid atrial activation for induction,2 a function that could be fulfilled by Ca2⫹-dependent ectopic firing. Triggered activity could thus contribute to AF in 2 ways: (1) by producing atrial tachycardia bursts that trigger reentrant AF in vulnerable substrates and (2) by providing focal drivers that maintain AF. Our studies have revealed potential mechanisms underlying the Ca2⫹-handling abnormalities that cause atrialtriggered activity in CHF (Figure 8). Changes that we identified in these studies are color coded, with red representing increases, and blue, decreases. The central abnormality Significance for Clinically Relevant Mechanisms AF is very commonly associated with CHF.16 CHF-induced atrial fibrosis impairs intra-atrial conduction and favors AF by promoting atrial reentry. 2 However, focal atrial tachyarrhythmias may also be important in CHF-related AF. Boyden et al6 showed atrial triggered activity due to delayed CaMKIIδδB CTL CHF CTL CHF 58 kDa CTL B 56 kDa PKAIIα GAPDH 37 kDa GAPDH CTL, n=16 CHF, n=8 P 37 kDa 150 125 CTL, n=10 CHF, n=8 100 75 50 25 * 0 PKAc PKAIIα C P C- IIδ K 51 kDa K aM C aM C 54 kDa IIδ C C- K IIδ IIδ aM K aM C C CTL CTL CHF CHF D PP1 Phosphatase activity 300 CTL, n=10 CHF, n=11 * 200 * 100 0 Total PP1 PP2A 37 kDa PP2A Relative to CTL (Normalized to GAPDH) C * * CHF 40 kDa Relative to CTL (normalized to GAPDH) Thr-287-CaMKIIδC Relative to CTL (normalized to GAPDH) 56 kDa 58 kDa 400 350 300 250 200 150 100 50 0 CTL CHF PKAc CaMKIIδC Thr-287-CaMKIIδB Relative to CTL (nmol/mg/min) Downloaded from http://circep.ahajournals.org/ by guest on May 11, 2017 transient amplitudes, and caffeine-releasable SR Ca2⫹. These alterations resulted in a predisposition to spontaneous Ca2⫹ release, abnormal diastolic membrane potential oscillations, and triggered activity. Despite larger Ca2⫹i transients, CHF cells displayed reduced contractility. These findings were accompanied by altered expression and phosphorylation of key Ca2⫹ handling, myofilament, and contractile proteins, as well as changes in crucially important regulatory kinases and phosphatases. CHF increased atrial APD and enhanced CaMKII phospholamban phosphorylation, both of which likely contributed to the Ca2⫹-loaded state. A * * 0 Tn-C Tn-I-P Tn-I-P Tn-I Figure 6. A, Top: Examples of Tn-I, Ser23/24-PTn-I, and Tn-C, along with GAPDH bands on the same lanes. Bottom: Mean⫾SEM protein-band intensities of total Tn-I, Ser23/24-P-Tn-I, and Tn-C normalized to GAPDH, expressed relative to control (n⫽10 control and 8 CHF atria/analysis). B, Top: Examples of total MyBP-C, Ser282-PMyBP-C, and phosphorylated MLC2a bands, along with GAPDH on the same lanes. Bottom: Mean⫾SEM protein-band intensities normalized to GAPDH, expressed relative to control (n⫽14 control, 10 CHF atria/analysis; *P⬍0.05 vs control). 37 kDa 250 200 CTL, n=14 CHF, n=10 150 100 50 0 PP1 PP2A Figure 7. A, Top: Examples of total CaMKII␦, Thr287-CaMKII (autophosphorylated), and GAPDH immunoblots. Top bands (58 kDa) represent CaMKII␦〉 and bottom (56 kDa) CaMKII␦C. Bottom: Mean⫾SEM protein-band intensities normalized to GAPDH, expressed relative to control (n⫽16 control and 8 CHF atria/analysis, *P⬍0.05 vs control). B, Top: Examples of PKAC, PKAII␣, and GAPDH immmunoblots. The PKAII␣ antibody recognized bands at 51 and 54 kDa. Quantification is based on the sum of the bands. Bottom: Mean⫾SEM protein band intensities normalized to GAPDH, expressed relative to control (n⫽10 control and 8 CHF atria/analysis, *P⬍0.05 vs control). C, D, Serine/threonine protein-phosphatase (PP) activity and corresponding protein expression in control and CHF atria. C, PP activity assessed with phosphorylase-A as substrate, quantified as nanomoles of 32Pi released per milligram protein per minute (n⫽10 for control and 11 CHF atria/analysis). D, Representative examples and mean⫾SEM protein-band intensities of PP1 and PP2A normalized to GAPDH, expressed relative to control (n⫽14 control and 10 CHF atria/analysis; *P⬍0.05 vs control). Ca2ⴙ Handling in Failing Atrium Yeh et al Atrial Fibrillation Initiation / maintenance Ectopic focus CHF Na+ ICa,L NCX1 increased increased [Ca2+]i Ca2+- influx CTL [Na+]i ●DADs ●Abnormal automaticity Ca2+ systolic 2+ CHF Ca release APD-prolongation Triggered activity diastolic Ca2+ release Ser2815 P P Ser2809 PP1 Ca2+ RyR Ca2+ increased CaMKII 2+ Ca2+ [Ca ]SR PLB CSQ Ca2+ Ca2+ Ca2+ Sarcoplasmic reticulum SERCA Ser16 P P Thr17 Tn-I P Ser23/24 Tn-C Ca2+ MyBP-C Ca2+ Ca2+ 99 282 P Ser PP1 Ca2+ P Ca2+ MLC-2a Thromboembolism, Stroke Myofilaments Embolus Downloaded from http://circep.ahajournals.org/ by guest on May 11, 2017 Atrial hypocontractility Atrial thrombogenesis that we observed is SR Ca2⫹ overload, likely resulting from 2 primary mechanisms: (1) increased transmembrane Ca2⫹ entry through ICaL during the prolonged CHF-induced AP waveform and (2) increased SERCA2a-mediated SR Ca2⫹ uptake due to the reduced phospholamban inhibition of SERCA2a caused by CaMKII phospholamban hyperphosphorylation. This effect of phospholamban hyperphosphorylation presumably overcomes the CHF downregulation of SERCA2a expression to produce a net increase in SERCAmediated SR Ca2⫹ uptake. In addition, decreased ryanodine receptor expression can promote increased SR Ca2⫹ content by reducing SR Ca2⫹ release.18 SR Ca2⫹ overload increases systolic Ca2⫹ release and also results in spontaneous diastolic Ca2⫹-release events. The NCX responds to diastolic [Ca2⫹]i transients by exchanging Ca2⫹ for Na⫹ in a 1:3 ratio, producing depolarizing inward currents manifesting as delayed afterdepolarizations and abnormal automaticity that cause triggered activity. Triggered activity is a strong candidate to underlie atrial ectopic foci that can initiate or maintain AF. In addition to the increased SR Ca2⫹ loading, we found a significant reduction in calsequestrin expression. Calsequestrin function–impairing mutations are associated with catecholaminergic polymorphic ventricular tachycardia and increased Ca2⫹-spark and -wave generation.19 –21 Calsequestrinknockout mice show spontaneous Ca2⫹-release events that are enhanced by isoproterenol.15 Even moderate downregulation of calsequestrin can increase SR Ca2⫹ leak and arrhythmia susceptibility.22 Therefore, the reduced calsequestrin expression that we observed may contribute to spontaneous SR Ca2⫹-release events independently of absolute Ca2⫹i levels.23 In recent years, there has been a concerted effort to develop novel, mechanistically based approaches to treating AF that avoid the risks of traditional ion channel targets.1 The identification of Ca2⫹-handling abnormalities as an important participant in CHF-related AF opens up interesting possibil- AF Thrombus Figure 8. Schematic representation of our findings and their potential significance. Observed changes in protein expression/phosphorylation or Ca2⫹handling function are indicated in red or blue: Red indicates increases and blue indicates decreases. Vertical solid black arrows represent changes in phosphorylating or dephosphorylating enzyme activity. Increased SR Ca2⫹ loading causes diastolic Ca2⫹ release through SR Ca2⫹-release channels (RyR), producing electrogenic Na⫹,Ca2⫹-exchange currents. The resulting diastolic membrane potential abnormalities may induce triggered activity-mediated ectopic firing that can initiate or maintain AF. Decreased phosphorylation of key contractile element proteins causes atrial cell hypocontractility that promotes stasisrelated thrombogenesis which can lead to thromboembolism and stroke. For further details, see Discussion. ities for novel small molecule – and gene transfer– based therapeutics.24,25 Impaired atrial contractility predisposes to atrial thromboembolism, one of the most significant complications of AF. Our study is the first to analyze atrial myocyte contractility changes and related mechanisms in the CHF setting. Prominent decreases in atrial cardiomyocyte contractility despite enlarged systolic Ca2⫹ transients imply atrial contractile protein dysfunction. We identified dramatically reduced PKA-phosphorylation of MyBP-C at Ser-282 as a potential underlying factor. MyBP-C PKA-phosphorylation is important for maximum force development, stretch-dependent augmentation of force generation, normal cross-bridge cycling kinetics, and diastolic relaxation.26 –29 Reduced phosphorylation of MLC2a, another important regulator of myofilament function,30 may also contribute to contractile dysfunction. Anticoagulant therapy has been the traditional mainstay of AF-related thromboembolism prophylaxis but is complex to maintain and may cause bleeding complications. A better recognition of the molecular basis of atrial hypocontractility could lead to new and potentially safer approaches to combating thromboembolic risk. Comparison With Previous Studies of Ca2ⴙ Handling in Failing Ventricles and AF Early studies of Ca2⫹ handling in ventricular cardiomyocytes from humans31 and rats32 with CHF showed increased diastolic [Ca2⫹]i, reduced Ca2⫹ transients, and slowed Ca2⫹ transient decay. Subsequent work consistently showed reduced and slowed Ca2⫹ transients in failing ventricular cardiomyocytes, with reduced SR Ca2⫹ stores and abnormal Ca2⫹ uptake and release mechanisms.14,33–35 The molecular basis of these ventricular Ca2⫹-handling abnormalities has been studied extensively.33 Decreased SERCA2a expression tends to reduce SR Ca2⫹ stores and slow Ca2⫹ transient decay.34 –36 NCX upregulation attenuates diastolic Ca2⫹ accu- 100 Circ Arrhythmia Electrophysiol June 2008 Downloaded from http://circep.ahajournals.org/ by guest on May 11, 2017 mulation due to the reduced SR Ca2⫹ uptake by SERCA2a and minimizes diastolic dysfunction,36 but it further decreases SR Ca2⫹ stores.33,35 Ca2⫹ release channel dysfunction caused by CaMKII (Ser-2815) and/or PKA (Ser-2809) RyR2 hyperphosphorylation contributes to SR Ca2⫹ depletion and arrhythmogenesis by causing diastolic Ca2⫹ leak.35,37,38 The Ca2⫹-handling abnormalities we identified in atrial cardiomyocytes from CHF dogs differ from previously reported CHF-induced ventricular changes.14,33–35,37 Instead of reduced Ca2⫹ transients and SR Ca2⫹ stores, atrial cells show increases in both. We were concerned by the discrepancies between our atrial Ca2⫹-handling changes and previous reports in ventricular cardiomyocytes. We therefore subjected paired ventricular and atrial cardiomyocytes from 2 dogs to Ca2⫹ transient measurements. As shown in online Data Supplement Figure IV, CHF-induced ventricular Ca2⫹handling changes resembled those in previous reports and differed clearly from Ca2⫹-handling changes in the atria. Several studies have examined the functional abnormalities in Ca2⫹ handling of AF patients, generally without overt CHF. Quantal Ca2⫹-release events and Ca2⫹ waves are more frequent in AF atria.39 PKA hyperphosphorylation of RyR2 promotes FKBP12.6 unbinding and Ca2⫹-release channel opening.8 We observed no significant changes in fractional RyR phosphorylation. This discrepancy may relate to the specific pathophysiological properties of our model, which involved recent-onset CHF, as opposed to clinical series including patients with long-standing AF, a variety of underlying heart diseases, and various cardioactive medications. Studies of atrial Ca2⫹-handling protein biochemistry in AF patients have provided widely varying results, possibly because of variations in patient populations.40 Ca2⫹-handling protein abnormalities in AF subjects reflect the effects of both underlying cardiac diseases and changes induced by the arrhythmia itself. Atrial tachycardia alters atrial cardiomyocyte Ca2⫹ handling, prominently decreasing Ca2⫹ transients.7,41 Mice with tumor necrosis factor-␣ overexpression develop a cardiomyopathic phenotype with atrial fibrosis and atrial reentrant arrhythmias.42 They also display reduced Ca2⫹ transients and caffeine-releasable Ca2⫹ stores in contrast to the increased Ca2⫹ loading and Ca2⫹ release in our canine model. Further studies in well-defined animal models and clinical populations are needed to clarify the factors contributing to abnormal Ca2⫹ handling in AF. Potential Limitations Some of the changes we observed in protein expression and steady-state phosphorylation appear to contradict our functional observations. Decreased SERCA2a protein expression should reduce SR Ca2⫹ loading, yet we noted increased SR Ca2⫹ loads. Increased Ca2⫹ influx due to prolonged atrial APDs, decreased SR Ca2⫹ discharge due to reduced RyR2 expression, and SERCA function enhancement via phospholamban hyperphosphorylation may be sufficient to offset decreased SERCA expression and increase SR Ca2⫹ content. We observed statistically significant ⬇15% decreases in the principal SR Ca2⫹-binding protein calsequestrin, which would be expected to reduce SR Ca 2⫹ storage. However, calsequestrin-knockout mice maintain normal SR Ca2⫹ stores, apparently by increasing SR volume.15 The decreased RyR2 expression that we observed might be expected to reduce [Ca2⫹]i transient amplitude by decreasing SR Ca2⫹ release. Previous studies have shown that decreased RyR2 function initially does decrease [Ca2⫹]i transients but results in SR Ca2⫹ accumulation that eventually restores Ca2⫹ release.18 We observed complex changes in protein phosphorylation, the functional result of which is difficult to predict. Phosphorylating enzymes showed varying changes: unchanged or decreased expression of PKA subunits and unchanged or increased expression of CaMKII components. Dephosphorylating enzyme changes also varied, including unchanged PP2A and enhanced PP1 activity. Thus, for each Ca2⫹handling protein, alterations at specific phosphorylation sites will depend on the net changes in phosphorylating and dephosphorylating enzymes acting on that site. Previous studies have reported varying results with regard to phosphorylation-dependent regulation of RyR2 in CHF, with increased or decreased ventricular RyR2 Ser-2809 phosphorylation having been observed (for review, see George et al43). Ser-2809 is 75% maximally phosphorylated at rest, producing a minimum basal activity level of RyR2 channels.44 Either increased or reduced RyR2 phosphorylation enhances RyR2 channel activity.44 We observed a decrease in total RyR2 phosphorylation but no significant changes in fractional RyR2 phosphorylation because decreased phosphorylated RyR2 expression paralleled decreased total RyR2 levels. Changes in expression and activity of ventricular kinases and phosphatases within local macromolecular complexes do not necessarily follow global changes in these enzymes,23,37 suggesting localized regulation of kinase or phosphatase activity in cellular microdomains. Thus, local changes in atrial macromolecular complexes containing RyR2, phospholamban, MyBP-C, and/or MLC2a may also have contributed to CHF-induced alterations. We found similar Ca2⫹-handling changes in LA and RA free-wall cardiomyocytes, but we cannot be sure that our results extend to other atrial sites. Having shown the similarity of LA and RA Ca2⫹-handling effects of CHF, we optimized the efficiency of dog usage by studying cellular arrhythmias and their response in LA cells and analyzing biochemical changes in RA tissue. We did not perform detailed complementary studies to assess arrhythmogenic changes in RA cells and biochemistry in LA tissue. We estimate that such studies would have required us to euthanize at least 20 additional dogs (10 dogs per group), which we felt was not justified because of very similar Ca2⫹-handling changes with CHF in LA versus RA. We did have frozen LA tissue samples from 6 additional dogs/group, which we subjected to biochemical analyses. The results, shown in Data Supplement Figures V through VIII, indicate that Ca2⫹handling protein changes in LA tissue were qualitatively quite similar to those in RA (which are reproduced beside the LA data for comparison). Conclusions Dogs with ventricular tachypacing–induced dilated cardiomyopathy display important abnormalities in atrial Ca2⫹ handling and in the expression, phosphorylation, and/or Yeh et al activity of key atrial Ca2⫹-handling, contractile, and regulatory proteins. They show signs of cellular Ca2⫹ overload, which results in a predisposition to spontaneous diastolic Ca2⫹ release, arrhythmogenic diastolic membrane potential oscillations, and triggered activity. These abnormalities in Ca 2⫹ homeostasis likely account for focal atrial tachyarrhythmias that contribute to atrial arrhythmogenesis in CHF. Acknowledgments The authors thank Nathalie L’Heureux, Chantal Maltais, Manja Schöne, Annett Opitz, and Sabine Kirsch for technical support and France Thériault for secretarial help with the manuscript. Sources of Funding Downloaded from http://circep.ahajournals.org/ by guest on May 11, 2017 The present study was supported by the Canadian Institutes of Health Research, Quebec Heart and Stroke Foundation, German Federal Ministry of Education and Research (Atrial Fibrillation Competence Network grant 01Gi0204), German Research Foundation (grant BO 1263/9 –1), and a network grant (European-North American AtrialFibrillation Research Alliance) from Fondation Leducq. Disclosures None. References 1. Nattel S. New ideas about atrial fibrillation 50 years on. Nature. 2002; 415:219 –226. 2. Li D, Fareh S, Leung TK, Nattel S. Promotion of atrial fibrillation by heart failure in dogs: atrial remodeling of a different sort. Circulation. 1999;100:87–95. 3. Fenelon G, Shepard RK, Stambler BS. Focal origin of atrial tachycardia in dogs with rapid ventricular pacing-induced heart failure. J Cardiovasc Electrophysiol. 2003;14:1093–1102. 4. Stambler BS, Fenelon G, Shepard RK, Clemo HF, Guiraudon CM. Characterization of sustained atrial tachycardia in dogs with rapid ventricular pacing-induced heart failure. J Cardiovasc Electrophysiol. 2003;14: 499 –507. 5. Ryu K, Schroff SC, Sahadevan J, Martovitz NL, Khrestian CM, Stambler BS. Mapping of atrial activation during sustained atrial fibrillation in dogs with rapid ventricular pacing induced heart failure: evidence for a role of driver regions. J Cardiovasc Electrophysiol. 2005;16:1348 –1358. 6. Boyden PA, Tilley LP, Albala A, Liu SK, Fenoglio JJ Jr, Wit AL. Mechanisms for atrial arrhythmias associated with cardiomyopathy: a study of feline hearts with primary myocardial disease. Circulation. 1984;69:1036 –1047. 7. Sun H, Gaspo R, Leblanc N, Nattel S. Cellular mechanisms of atrial contractile dysfunction caused by sustained atrial tachycardia. Circulation. 1998;98:719 –727. 8. Vest JA, Wehrens XH, Reiken SR, Lehnart SE, Dobrev D, Chandra P, Danilo P, Ravens U, Rosen MR, Marks AR. Defective cardiac ryanodine receptor regulation during atrial fibrillation. Circulation. 2005;111: 2025–2032. 9. Cha TJ, Ehrlich JR, Zhang L, Shi YF, Tardif JC, Leung TK, Nattel S. Dissociation between ionic remodeling and ability to sustain atrial fibrillation during recovery from experimental congestive heart failure. Circulation. 2004;109:412– 418. 10. Coutu P, Chartier D, Nattel S. Comparison of Ca2⫹-handling properties of canine pulmonary vein and left atrial cardiomyocytes. Am J Physiol Heart Circ Physiol. 2006;291:H2290 –H2300. 11. Popov N, Schmitt M, Schulzeck S, Matthies N. Reliable micromethod for determination of the protein content in tissue homogenates. Acta Biol Med Ger. 1975;34:1441–1446. 12. El-Armouche A, Boknik P, Eschenhagen T, Carrier L, Knaut M, Ravens U, Dobrev D. Molecular determinants of altered Ca2⫹ handling in human chronic atrial fibrillation. Circulation. 2006;114:670 – 680. 13. Boknik P, Fockenbrock M, Herzig S, Knapp J, Linck B, Luss H, Muller FU, Muller T, Schmitz W, Schroder F, Neumann J. Protein phosphatase activity is increased in a rat model of long-term beta-adrenergic stimulation. Naunyn Schmiedebergs Arch Pharmacol. 2000;362:222–231. Ca2ⴙ Handling in Failing Atrium 101 14. Hobai IA, O’Rourke B. Enhanced Ca2⫹-activated Na⫹-Ca2⫹ exchange activity in canine pacing-induced heart failure. Circ Res. 2000;87: 690 – 698. 15. Knollmann BC, Chopra N, Hlaing T, Akin B, Yang T, Ettensohn K, Knollmann BE, Horton KD, Weissman NJ, Holinstat I, Zhang W, Roden DM, Jones LR, Franzini-Armstrong C, Pfeifer K. Casq2 deletion causes sarcoplasmic reticulum volume increase, premature Ca2⫹ release, and catecholaminergic polymorphic ventricular tachycardia. J Clin Invest. 2006;116:2510 –2520. 16. Ehrlich JR, Nattel S, Hohnloser SH. Atrial fibrillation and congestive heart failure: specific considerations at the intersection of two common and important cardiac disease sets. J Cardiovasc Electrophysiol. 2002; 13:399 – 405. 17. Okuyama Y, Miyauchi Y, Park AM, Hamabe A, Zhou S, Hayashi H, Miyauchi M, Omichi C, Pak HN, Brodsky LA, Mandel WJ, Fishbein MC, Karagueuzian HS, Chen PS. High resolution mapping of the pulmonary vein and the vein of Marshall during induced atrial fibrillation and atrial tachycardia in a canine model of pacing-induced congestive heart failure. J Am Coll Cardiol. 2003;42:348 –360. 18. Overend CL, O’Neill SC, Eisner DA. The effect of tetracaine on stimulated contractions, sarcoplasmic reticulum Ca2⫹ content and membrane current in isolated rat ventricular myocytes. J Physiol. 1998;507(pt 3):759 –769. 19. Kubalova Z, Gyorke I, Terentyeva R, Viatchenko-Karpinski S, Terentyev D, Williams SC, Gyorke S. Modulation of cytosolic and intrasarcoplasmic reticulum calcium waves by calsequestrin in rat cardiac myocytes. J Physiol. 2004;561(pt 2):515–524. 20. Song L, Alcalai R, Arad M, Wolf CM, Toka O, Conner DA, Berul CI, Eldar M, Seidman CE, Seidman JG. Calsequestrin 2 (CASQ2) mutations increase expression of calreticulin and ryanodine receptors, causing catecholaminergic polymorphic ventricular tachycardia. J Clin Invest. 2007; 117:1814 –1823. 21. Terentyev D, Nori A, Santoro M, Viatchenko-Karpinski S, Kubalova Z, Gyorke I, Terentyeva R, Vedamoorthyrao S, Blom NA, Valle G, Napolitano C, Williams SC, Volpe P, Priori SG, Gyorke S. Abnormal interactions of calsequestrin with the ryanodine receptor calcium release channel complex linked to exercise-induced sudden cardiac death. Circ Res. 2006;98:1151–1158. 22. Chopra N, Kannankeril PJ, Yang T, Hlaing T, Holinstat I, Ettensohn K, Pfeifer K, Akin B, Jones LR, Franzini-Armstrong C, Knollmann BC. Modest reductions of cardiac calsequestrin increase sarcoplasmic reticulum Ca2⫹ leak independent of luminal Ca2⫹ and trigger ventricular arrhythmias in mice. Circ Res. 2007;101:617– 626. 23. Guo T, Zhang T, Mestril R, Bers DM. Ca2⫹/Calmodulin-dependent protein kinase II phosphorylation of ryanodine receptor does affect calcium sparks in mouse ventricular myocytes. Circ Res. 2006;99: 398 – 406. 24. Wehrens XH, Lehnart SE, Marks AR. Ryanodine receptor–targeted antiarrhythmic therapy. Ann N Y Acad Sci. 2005;1047:366 –375. 25. Akar FG, Tomaselli GF. Ion channels as novel therapeutic targets in heart failure. Ann Med. 2005;37:44 –54. 26. Sadayappan S, Gulick J, Osinska H, Martin LA, Hahn HS, Dorn GW II, Klevitsky R, Seidman CE, Seidman JG, Robbins J. Cardiac myosinbinding protein-C phosphorylation and cardiac function. Circ Res. 2005; 97:1156 –1163. 27. Stelzer JE, Patel JR, Moss RL. Protein kinase A-mediated acceleration of the stretch activation response in murine skinned myocardium is eliminated by ablation of cMyBP-C. Circ Res. 2006;99:884 – 890. 28. Pohlmann L, Kroger I, Vignier N, Schlossarek S, Kramer E, Coirault C, Sultan KR, El-Armouche A, Winegrad S, Eschenhagen T, Carrier L. Cardiac myosin-binding protein C is required for complete relaxation in intact myocytes. Circ Res. 2007;101:928 –938. 29. Stelzer JE, Patel JR, Walker JW, Moss RL. Differential roles of cardiac myosin-binding protein C and cardiac troponin I in the myofibrillar force responses to protein kinase A phosphorylation. Circ Res. 2007;101: 503–511. 30. Grimm M, Haas P, Willipinski-Stapelfeldt B, Zimmermann WH, Rau T, Pantel K, Weyand M, Eschenhagen T. Key role of myosin light chain (MLC) kinase–mediated MLC2a phosphorylation in the ␣1-adrenergic positive inotropic effect in human atrium. Cardiovasc Res. 2005;65: 211–220. 31. Beuckelmann DJ, Nabauer M, Erdmann E. Intracellular calcium handling in isolated ventricular myocytes from patients with terminal heart failure. Circulation. 1992;85:1046 –1055. 102 Circ Arrhythmia Electrophysiol June 2008 Downloaded from http://circep.ahajournals.org/ by guest on May 11, 2017 32. Capasso JM, Li P, Anversa P. Cytosolic calcium transients in myocytes isolated from rats with ischemic heart failure. Am J Physiol. 1993;265: H1953–H1964. 33. Bers DM. Altered cardiac myocyte Ca regulation in heart failure. Physiology (Bethesda). 2006;21:380 –387. 34. Hobai IA, O’Rourke B. Decreased sarcoplasmic reticulum calcium content is responsible for defective excitation-contraction coupling in canine heart failure. Circulation. 2001;103:1577–1584. 35. Armoundas AA, Rose J, Aggarwal R, Stuyvers BD, O’rourke B, Kass DA, Marban E, Shorofsky SR, Tomaselli GF, William Balke C. Cellular and molecular determinants of altered Ca2⫹ handling in the failing rabbit heart: primary defects in SR Ca2⫹ uptake and release mechanisms. Am J Physiol Heart Circ Physiol. 2007;292:H1607–H1618. 36. Hasenfuss G, Schillinger W, Lehnart SE, Preuss M, Pieske B, Maier LS, Prestle J, Minami K, Just H. Relationship between Na⫹-Ca2⫹-exchanger protein levels and diastolic function of failing human myocardium. Circulation. 1999;99:641– 648. 37. Ai X, Curran JW, Shannon TR, Bers DM, Pogwizd SM. Ca2⫹/calmodulin-dependent protein kinase modulates cardiac ryanodine receptor phosphorylation and sarcoplasmic reticulum Ca2⫹ leak in heart failure. Circ Res. 2005;97:1314 –1322. 38. Marx SO, Reiken S, Hisamatsu Y, Jayaraman T, Burkhoff D, Rosemblit N, Marks AR. PKA phosphorylation dissociates FKBP12.6 from the calcium release channel (ryanodine receptor): defective regulation in failing hearts. Cell. 2000;101:365–376. 39. Hove-Madsen L, Llach A, Bayes-Genis A, Roura S, Rodriguez Font E, Aris A, Cinca J. Atrial fibrillation is associated with increased spontaneous calcium release from the sarcoplasmic reticulum in human atrial myocytes. Circulation. 2004;110:1358 –1363. 40. Nattel S, Maguy A, Le Bouter S, Yeh YH. Arrhythmogenic ion-channel remodeling in the heart: heart failure, myocardial infarction, and atrial fibrillation. Physiol Rev. 2007;87:425– 456. 41. Schotten U, Greiser M, Benke D, Buerkel K, Ehrenteidt B, Stellbrink C, Vazquez-Jimenez JF, Schoendube F, Hanrath P, Allessie M. Atrial fibrillation–induced atrial contractile dysfunction: a tachycardiomyopathy of a different sort. Cardiovasc Res. 2002;53:192–201. 42. Saba S, Janczewski AM, Baker LC, Shusterman V, Gursoy EC, Feldman AM, Salama G, McTiernan CF, London B. Atrial contractile dysfunction, fibrosis, and arrhythmias in a mouse model of cardiomyopathy secondary to cardiac-specific overexpression of tumor necrosis factor-{alpha}. Am J Physiol Heart Circ Physiol. 2005;289:H1456 –H1467. 43. George CH, Jundi H, Thomas NL, Fry DL, Lai FA. Ryanodine receptors and ventricular arrhythmias: emerging trends in mutations, mechanisms and therapies. J Mol Cell Cardiol. 2007;42:34 –50. 44. Carter S, Colyer J, Sitsapesan R. Maximum phosphorylation of the cardiac ryanodine receptor at serine-2809 by protein kinase a produces unique modifications to channel gating and conductance not observed at lower levels of phosphorylation. Circ Res. 2006;98:1506 –1513. CLINICAL PERSPECTIVE Congestive heart failure (CHF) is a common cause of atrial fibrillation (AF). The therapeutic tools available for AF management are suboptimal, and new insights into fundamental mechanisms underlying AF may permit the development of new treatment approaches. The basis of spontaneous atrial ectopic activity that can trigger or drive AF is poorly understood. This study focused on the potential role of Ca2⫹-handling abnormalities in CHF-related atrial ectopic activity. CHF was induced in dogs by ventricular tachypacing (240 bpm ⫻2 weeks). Cellular Ca2⫹-handling properties and expression/phosphorylation status of key Ca2⫹-handling and myofilament proteins were assessed. CHF increased atrial cell Ca2⫹ loading, leading to spontaneous sarcoplasmic reticulum Ca2⫹ release (especially under Ca2⫹ entry– enhancing conditions like tachycardia), which resulted in diastolic atrial membrane potential oscillation and ectopic firing. Ca2⫹ overload was due to multiple factors: (1) increased action potential duration, which enhanced Ca2⫹ entry during the action potential plateau; (2) increased phosphorylation of phospholamban by Ca2⫹/calmodulin-dependent protein kinase II (CaMKII), which reduces the phospholamban-dependent suppression of sarcoplasmic reticulum Ca2⫹ uptake through the sarcoplasmic reticulum Ca2⫹ transporter (SERCA); and (3) decreased ryanodine receptor expression, which reduces sarcoplasmic reticulum Ca2⫹ egress through Ca2⫹-release channels. Despite increased sarcoplasmic reticulum Ca2⫹ loading, atrial contractility was reduced in CHF, likely because of decreased phosphorylation of 2 important contraction-regulating proteins, myosin-binding protein C and myosin light chain-2a. Phosphorylation abnormalities in CHF were related to altered expression and/or activity of phosphorylation-enhancing (CaMKII expression/activity upregulated) and phosphorylation-suppressing (protein phosphatase-1 activity upregulated) proteins. Thus, CHF causes profound changes in phosphorylation and expression of key Ca2⫹-handling and myofilament regulatory proteins that cause atrial cardiomyocyte Ca2⫹ homeostasis and contractile abnormalities, which in turn contribute to AF-promoting triggered activity and thrombosis-promoting contractile dysfunction. Calcium-Handling Abnormalities Underlying Atrial Arrhythmogenesis and Contractile Dysfunction in Dogs With Congestive Heart Failure Yung-Hsin Yeh, Reza Wakili, Xiao-Yan Qi, Denis Chartier, Peter Boknik, Stefan Kääb, Ursula Ravens, Pierre Coutu, Dobromir Dobrev and Stanley Nattel Downloaded from http://circep.ahajournals.org/ by guest on May 11, 2017 Circ Arrhythm Electrophysiol. 2008;1:93-102; originally published online January 1, 2008; doi: 10.1161/CIRCEP.107.754788 Circulation: Arrhythmia and Electrophysiology is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 2008 American Heart Association, Inc. All rights reserved. Print ISSN: 1941-3149. Online ISSN: 1941-3084 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circep.ahajournals.org/content/1/2/93 Data Supplement (unedited) at: http://circep.ahajournals.org/content/suppl/2008/04/29/CIRCEP.107.754788.DC1 Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Circulation: Arrhythmia and Electrophysiology can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Circulation: Arrhythmia and Electrophysiology is online at: http://circep.ahajournals.org//subscriptions/