* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
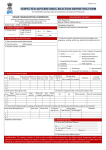
Download Guidance Document For Reporting Individual Case Safety Report
Pharmaceutical marketing wikipedia , lookup
Electronic prescribing wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Drug interaction wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacognosy wikipedia , lookup
Theralizumab wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Guidance Document For Reporting Individual Case Safety Report National Coordination Centre Indian Pharmacopoeia Commission, Ghaziabad is an autonomous institution of the Ministry of Health and Family Welfare, Govt. of India, which sets standards for drugs that are manufactured, sold and consumed in India.IPC is functioning as a National Coordination Centre for Pharmacovigilance Programme of India.The basic function of IPC is to publish official documents for improving quality of medicines by way of adding new and updating existing monographs in the form of Indian Pharmacopoeia. It further promotes rational use of generic medicines by publishing National Formulary of India. IP prescribes standards for identity, purity and strength of drugs essentially required from healthcare perspective of human beings and animals. IPC also provides IP Reference Substances which act as a finger print for identification of an article under test and its purity as prescribed in IP. The IP standards are legally acceptable during quality assurance and at the time of dispute in the court of law. IPC administers the Second Schedule of the Drugs and Cosmetics Act, 1940 (the act) and Rules 1945, applying a risk management approach designed to set standards of drugs in India to meet acceptable standards of quality, safety and efficacy of drugs commonly required for treatment of diseases prevailing in the region. NCC is operating under the supervision of steering committee which recommends procedures and guidelines for regulatory interventions.The main responsibility of NCC is to monitor all the adverse reactions of medicines being observed in the Indian population. It aims to develop and maintain its own Pharmacovigilance database for patient safety with respect to use of medicine. Pharmacovigilance Programme of India Page 1 Guidance Document For Reporting Individual Case Safety Report Introduction Adverse reactions of drugs continue to remain as an important public health issue. Safety monitoring of medicines is the responsibility of all stakeholders of the healthcare system since globally it continues to be an important cause of morbidity and mortality. In some countries adverse drug reactions are among the ten leading causes of mortality. The safety of patients and the safe use of medicines are crucial for health policy development and delivery of the best healthcare. To prevent or reduce harm to patients thereby improving public health, the safety of medicines in clinical use must be monitored and evaluated through specialised systems. This requires a need to establish a well-organised pharmacovigilance system. Thus, a pharmacovigilance system is defined as a system used by an organisation to monitor the safety of authorised medicinal products and detect any change to their risk-benefit balance. A pharmacovigilance system is characterised by its structures, processes and outcomes. To run an effective pharmacovigilance system a protocol is required for reporting adverse reactions associated with drug use. Therefore NCC aims to ensure the systematic and effective functioning of PvPI by publishing its guidance document. This Guidance Document lays down requirements and guidance for reporting of adverse drug reactions and significant safety issues related to drugs regulated by the Central Drugs Standard Control Organization. This document does not establish legally enforceable responsibilities. This has been prepared by the NCC and approved by Working Group. The purpose of this document is to present the importance of pharmacovigilance in India, to record the growth and potential as a significant discipline within medical science, and to describe its impact on patient welfare and public health. This document also highlights the importance of collaboration and communication at local, regional and international levels to ensure that pharmacovigilance delivers its full benefits. It also provides guidance to stakeholders on good pharmacovigilance practices, assessment of data regarding drugs including vaccines, herbal and biological products (blood and blood components) and dietary supplements. Scope of Guidance Document This document helps to expand the role and scope of PvPI to identify, analyse and minimise the risk associated with drugs. Further it promotes better and broader use of existing pharmacovigilance data for patient safety by spontaneous reporting system. Pharmacovigilance Programme of India Page 2 Guidance Document For Reporting Individual Case Safety Report The document is intended for the following wide-ranging readership: Policy makers at all levels of healthcare, particularly those concerned with drug policy Staff and consultants in CDSCO Healthcare practitioners including clinicians, dentists, pharmacists, nurses and other healthcare professionals Pharmaceutical industry and scientists Professional staff at NCC Representatives of Adverse Drug Reaction Monitoring Centre Medical and scientific journals Health epidemiologists Health economists National Health Programs under MoHFW, Government of India Professional staff at poison and drug information centres Health administrators Consumer groups, civil societies and patient support groups Institutes of medical, dental, pharmacy and nursing Pharmacovigilance Programme of India Page 3 Guidance Document For Reporting Individual Case Safety Report Chapter 1: Pharmacovigilance Programme of India 1.0 Background The Pharmacovigilance Programme of India was initiated by the Government of India on 14th July 2010in AIIMS, New Delhi as the NCC for monitoring ADRs in the country for safeguarding public health. The NCC was shifted from AIIMS, New Delhi to IPC, Ghaziabad on 15th April 2011. 1.1 Overview Before registration and marketing of medicine in the country, its safety and efficacy experience is based primarily on the use of the medicine in clinical trials. These trials mainly detect common adverse reactions. Some important reactions, such as those, which take a long time to develop, or those, which occur rarely, may not be detected in clinical trials. In addition, the controlled conditions under which medicines are used in clinical trials do not necessarily reflect the way they will be used in practice. For a medicine to be considered safe, its expected benefits should be greater than any associated risks of harmful reactions. So in order to gain a comprehensive safety profile of medicine, a continuous post-marketing monitoring system is essential. PvPI is to collate the data and use the inferences to recommend regulatory interventions, besides communicating risks to healthcare professionals and the public. The robust database will play a vital role in analysing and detecting new signals and updating the status of existing information on drug profile. The larger is the data for any drug, the higher will be the likelihood of saying with confidence that the conclusions or inferences being drawn from that data are meaningful and significant. The Medical Colleges and hospitals are the corner stone of the PvPI. They act as AMCs which are responsible for collecting the individual case safety reports and performing the follow up with the patient to check completeness of the reports as per SOPs. The ICSRs data is then uploaded in the VigiBase by using VigiFlow software which is sent to NCC. The quality assessment will be performed at NCC and the data is further sent to WHO-UMC which maintains the global drug safety database. Pharmacovigilance Programme of India Page 4 Guidance Document For Reporting Individual Case Safety Report 1.2 Mission Safeguard the health of the Indian population by ensuring that the benefits of use of medicine outweigh the risks associated with its use. 1.3 Vision To improve patient safety and welfare in Indian population by monitoring drug safety and thereby reducing the risk associated with use of medicines. 1.4 Objectives To create a nation-wide system for patient safety reporting To identify and analyse new signal from the reported cases To analyse the benefit - risk ratio of marketed medications To generate evidence based information on safety of medicines To support regulatory agencies in the decision-making process on use of medications To communicate the safety information on use of medicines to various stakeholders to minimise the risk To emerge as a national centre of excellence for pharmacovigilance activities To collaborate with other national centres for the exchange of information and data management To provide training and consultancy support to other national pharmacovigilance centres across globe 1.4.1 Short term goals To develop and implement pharmacovigilance system in India To enrol, initially, all MCI approved medical colleges in the program covering north, south, east and west of India To encourage healthcare professionals in reporting of adverse reaction to drugs, vaccines, medical devices and biological products Collection of case reports and data 1.4.2 Long term goals To expand the pharmacovigilance programme to all hospitals (govt. & private) and centres of public health programs located across India To develop and implement electronic reporting system (e-reporting) To develop reporting culture amongst healthcare professionals To make ADR reporting mandatory for healthcare professionals Pharmacovigilance Programme of India Page 5 Guidance Document For Reporting Individual Case Safety Report 1.5 Organogram under Pharmacovigilance Programme of India 1.5.1 Organogram of NCC Advisor Secretary-CumScientific Director, IPC Senior Scientific Officer Director, National Institute of Biologicals Finance & Account Officer Scientific Assistant Technical Associate 1.5.2 Committees under NCC The following committees and panels are constituted by MoHFW, Government of India to give proper direction for efficient functioning of the programme. Steering Committee PvPI is administered and monitored by Steering Committee to supervise and give proper direction to the programme. PvPI Working Group It is constituted to approve major technical issues related to establishment, implementation of programme and giving technical inputs to CDSCO for regulatory intervention of medicine. Pharmacovigilance Programme of India Page 6 Guidance Document For Reporting Individual Case Safety Report Quality Review Panel It is constituted to review quality, causality assessment and completeness of ICSRs. The panel also makes recommendations to PvPI working group after data analysis and will devise formats and guidance documents for follow up actions after implementation of recommendations. Signal Review Panel It is constituted of experienced scientists and clinical experts affiliated to government and non-government academic institutions, hospitals and pharmaceutical industries to collate and analyze information from ICSRs submitted to NCC. This panel assesses the results of the regular computerized screening of ICSRs in NCC database for the occurrence of signals of possible importance of public health, drug regulation and science. It also defines biostatical methods to be followed for analysis and creates standardized post analytical reports that will help in understanding the information that is derived from ADRs. It is also responsible to decide on actionable indicators. Core Training Panel The Core Training Panel of PvPI identifies trainers and zone wise training centres for imparting training under pharmacovigilance training programme. Core training panel interacts with international agencies for participation and implementation of training programmes related to pharmacovigilance. It organizes training and projects budgetary requirements. Training modules and training schedules are also develop by this panel. 1.6 PvPI - Programme Communication Effective communication channels are the key to successful functioning of PvPI. The following chart depicts the movement of information between the key stakeholders and ensures the continuous transfer of data, information, and knowledge. Pharmacovigilance Programme of India Page 7 Guidance Document For Reporting Individual Case Safety Report PvPI - Programme Communication Pharmacovigilance Programme of India Page 8 Guidance Document For Reporting Individual Case Safety Report Chapter 2: Responsibilities of Stakeholders under PvPI 2.0 Roles and Responsibilities of Personnel at AMC Each AMC under PvPI is assigned with a coordinator and a technical associate responsible for its functioning. Their roles and responsibilities are: The designated coordinator is responsible for the proper functioning of respective AMC. In absence of the coordinator, the designed deputy coordinator is responsible for the smooth functioning of the centre. Other important responsibilities of coordinator checking completeness of a valid case, causality assessment and scrutinizing the ADR reports as per SOPs. The technical associate is responsible for collecting and follows up ICSRs. All the scrutinized and signed ADR reports should be entered in VigiFlow by TA. Every report has to be sent for the central assessment at NCC. The centre coordinator is responsible for sending the monthly reports of their AMC to NCC. The centre coordinator is also responsible for sensitization of the physicians/healthcare professionals/medical students/patient of the catchment hospital for spontaneous ADR reporting by various modes (lectures on ADR reporting, emails, telephone, pamphlets & newsletters). Feedbacks to all healthcare professionals involved in reporting are to be sent by the AMC coordinator. 2.1 Roles and Responsibilities of Personnel at NCC NCC is responsible for: Preparing standard operating procedures, guidance documents &training manuals. Enrolment of new AMC. Reviewing and analyzing ICSRs received from AMCs and commit them to WHOUMC. Organising Continuous Medical Education on pharmacovigilance at various zones. Conducting periodic training and workshops for all enrolled AMCs. Publishing the newsletter (PvPI Newsletter) on timely basis. Reporting all concerned issues to CDSCO Headquarters. Providing procurement, financial and administrative support to all AMCs enrolled under PvPI. Collaborating with WHO-UMC, Sweden. Pharmacovigilance Programme of India Page 9 Guidance Document For Reporting Individual Case Safety Report 2.2 Roles and Responsibilities of Personnel at Zonal/Sub-zonal CDSCO office The Zonal/Sub-zonal is responsible for: Reporting all drug related issues to the CDSCO headquarter. Providing administrative and logistic supports to the AMC at their zone. Auditing/inspecting AMC in their respective zonal and submitting the inspection report to CDSCO HQ. 2.3 Roles and Responsibilities of Personnel at CDSCO HQ The CDSCO HQ is responsible for: Taking appropriate regulatory decision and actions on the basis of recommendations made by NCC. Propagating medicine safety related decisions to stakeholders. Providing administrative support to run PVPI. Pharmacovigilance Programme of India Page 10 Guidance Document For Reporting Individual Case Safety Report Chapter 3: Reporting of Adverse Drug Reactions Monitoring of ADRs in a pharmacovigilance involves both active and passive surveillance system. Passive surveillance means that no active measures are taken to look for adverse effects other than the encouragement of health professionals and others to report safety concerns. Reporting is entirely dependent on the initiative and motivation of the potential reporters. Spontaneous or voluntary reporting is a type of passive surveillance. Active surveillance, in contrast to passive surveillance, seeks to ascertain completely the number of adverse events via a continuous pre-organised process. An example of active surveillance is the follow-up of patients treated with a particular drug through a risk management program. 3.0 Spontaneous Reporting As per WHO definition, a spontaneous report is an unsolicited communication by healthcare professionals or consumers, pharmaceutical company to regulatory authority that describes one or more suspected adverse drug reactions in a patient given one or more medicinal products. Globally spontaneous reporting is adopted as the most common method of passive surveillance since it is easiest to establish and the convenient to run. In spontaneous reporting, reporting rates are generally very low and subject to bias and there is no database of all users or information on overall drug utilization. These problems prevent the accurate assessment of risk, risk factors or comparisons between drugs. Underreporting is also a problem of spontaneous reporting systems for suspected adverse drug reactions. Underreporting may delay signal detection and cause underestimation of a serious problem. Nevertheless spontaneous reporting has played a major role in the identification of safety signals throughout the marketed lifetime of medicines in general. PvPI is following spontaneous reporting system to collect data on drug safety. 3.1 Reporting Form The NCC has designed a Suspected Adverse Drug Reaction Reporting Form to record adverse reactions related to drugs. Separate forms are available to record adverse reactions associated with transfusion of blood and blood products and Adverse Event Following Immunization. A report that contains information describing a suspected adverse drug reaction related to the administration of one or more medicinal products to an individual patient is termed as individual case safety report. An ICSR must contain information on the following items: Pharmacovigilance Programme of India Page 11 Guidance Document For Reporting Individual Case Safety Report A. Patient Information 1. Patient initials: A reporter should only write the initials of a patient instead of full name. For e.g.: Madhu Gupta should be written as MG 2. Age at time of event or date of birth: A reporter must report either the date of birth or age of the patient at the time event or reaction occurred 3. Sex: A reporter must mention the gender of the patient. 4. Weight: The weight of the patient should be in kilograms B. Suspected Adverse Reaction 5. Date of reaction started: A reporter must report the date on which the reaction first observed. 6. Date of recovery: If the reaction recovered, the date on which the reaction recovered should be report. 7. Describe reaction: A reporter must describe the event in terms of nature, localization etc. For e.g.: patient developed erythematous maculopapular rash over upper and lower limp. C. Suspected Medications 8. The details of suspected medication(s) such as drug name (brand or generic name), manufacturer, batch no/lot no, expiry date, dose used, route used, frequency, dates of therapy started and stopped, and indication of use must be provided by the reporter. 9. De-challenge details: A reporter must report the status on de-challenge as: ‘Yes’- if reaction abated after de-challenge ‘Reduced dose’- If dose at which the reaction occurred is reduced Note: Also mention the reduced dose ‘No’- if reaction does not abated after de-challenge ‘Unknown’- if information on de-challenge is not confirmed ‘Not Applicable’ or ‘NA’- if de-challenge is not applicable as in case of vaccines, anaesthesia or where single dose is given 10. Re-challenge details: A reporter must report the status on re-challenge as: ‘Yes’- if reaction reappeared after re-challenge ‘No’- if reaction does not reappeared after re-challenge Pharmacovigilance Programme of India Page 12 Guidance Document For Reporting Individual Case Safety Report ‘Unknown’- if information on re-challenge is not confirmed ‘Re-introduced dose’- If the reduced dose is increased to dose at which adverse ‘Not Applicable’ or ‘NA’- if re-challenge is not applicable as in case of injections. event occurred 11. Concomitant drugs: A reporter should include all the details of concomitant drugs including self-medication, OTC medication, herbal remedies with therapy dates 12. Relevant tests/ laboratory data: The reporter must report any laboratory data (if available) relevant to the event occurred. 13. Other relevant history: A reporter must mention any relevant history persistent to patient including pre-existing medical conditions (e.g. allergies, pregnancy, smoking, alcohol use, hepatic/renal dysfunction). 14. Seriousness of the reaction: If any event is serious in nature, a reporter must tick the appropriate reason for seriousness as: ‘Death’- if the patient died due to adverse event ‘Life-threatening’- if patient was at substantial risk of dying at the time of the adverse event ‘Hospitalisation/prolonged’- if the adverse event cause hospitalisation or increased the hospital stay of the patient ‘Disability’- if adverse event resulted in a substantial disruption of a person's ability to conduct normal life functions ‘Congenital anomaly’- if exposure of drug prior to conception or during pregnancy may have resulted in an adverse outcome in the child. ‘Required intervention to prevent permanent impairment/damage’- if medical or surgical intervention was necessary to preclude permanent impairment of a body function, or prevent permanent damage to a body structure ‘Other’ -when the event does not fit the other outcomes, but the event may put the patient at risk and may require medical or surgical intervention to prevent one of the other outcomes. Examples include serious blood dyscrasias (blood disorders) or seizures/convulsions that do not result in hospitalization, development of drug dependence or drug abuse Pharmacovigilance Programme of India Page 13 Guidance Document For Reporting Individual Case Safety Report 15. Outcomes: The reporter must tick the outcome of the event as: ‘Fatal’- if the patient dies due to adverse event ‘Continuing’- if the patient is continuing with the event occurred ‘Recovering’- if the patient is recovering from the existing event occurred ‘Recovered’- if the patient is recovered from the event occurred ‘Unknown’- if the outcome is not known D. Reporter 16. Name and Professional address: A reporter must mention his/her name and professional address on the form. The identity of the reporter will be maintained confidential 17. Causality assessment: The reporter (if trained) must perform the causality assessment. 18. Date of report: A reporter must mention the date on which he/she reported the adverse event. For quality reporting of ICSRs all the above mentioned fields are essential. In case of incomplete information, the reporter must take care that at least mandatory fields are present. Following are the mandatory fields for a valid case report: Patient information: initials, age at onset of reaction, gender. Suspected adverse reaction: A reaction term(s), date of onset of reaction Suspected medication: Drug(s) name, dose, date of therapy started, indication of use, seriousness, outcome, de-challenge and re-challenge details Reporter: Name and address, causality assessment, date of report Pharmacovigilance Programme of India Page 14 Guidance Document For Reporting Individual Case Safety Report Pharmacovigilance Programme of India Page 15 Guidance Document For Reporting Individual Case Safety Report 3.2 Who can Report? Under PvPI healthcare professionals (clinician, dentist pharmacist nurses and others) can report suspected adverse drug reaction. Pharmaceutical companies can also send ICSRs specific for their product to NCC. 3.3 What to Report? In order to foster the habit of reporting PvPI encourages reporting of all types of suspected ADRs- irrespective of whether they are known or unknown, serious and non-serious, frequent or rare. Although pharmacovigilance is primarily concerned with pharmaceutical medicines, adverse reactions associated with drugs used in traditional medicine (e.g. herbal remedies) should also be considered. Special fields of interest are drug use in pregnancy, lactation, paediatric and geriatric. In addition, the reporting of lack of efficacy and suspected pharmaceutical defects is recommended, especially when there is the possibility of manufacturing problems, counterfeit pharmaceuticals or of the development of resistance e.g. antibiotics. 3.4 Whom to Report? Use the ‘Suspected Adverse Drug Reaction Reporting Form’ which is available on the official website of IPC (www.ipc.gov.in) as well as CDSCO (www.cdsco.nic.in) to report any ADR. A reporter who is not a part of AMC can submit the ICSR to the nearest AMC or directly to the NCC. A reporter can also mail the ICSR at [email protected] or [email protected] Contact details for AMCs under PvPI are included in Annexure I. 3.5 Establishment of an AMC A ‘letter of Intent’ is required to submit by the Heads of the Institutions to participate in this nationwide programme to monitor drug safety. After examining the suitability, the concerned centre may be inducted as AMC under PvPI. Subsequently NCC communicates the AMC details to WHO-Uppsala Monitoring Centre (UMC), Sweden to obtain VigiFlow (WHOUMC owned online software) login details to upload ADRs. Pharmacovigilance Programme of India Page 16 Guidance Document For Reporting Individual Case Safety Report 3.5.1 Data Flow Once the Medical institute enrolled as AMC, the AMC starts reporting ADRs to NCC. Following chart explains the flow of data at regional, national and international level. Following chart explains the flow of data at regional, national and international level. 3.6 Assessment of Individual Case Safety Reports The quality of the ICSR will be assessed for completeness of information and it will be reviewed by: 1. Quality of documentation: e.g. completeness and integrity of data, quality of diagnosis, follow-up. 2. Coding: Drug names should be registered in a systematic way, for example by using the WHO Drug Dictionary (which is based on the ATC classification). For the coding of the adverse events the WHO Adverse Reaction Terminology (WHOART) and internationally recognised terminology (e.g. MedDRA) should be used. 3. Relevance with regard to the detection of new reactions, drug regulation, or scientific or educational value. The following questions especially may be asked: Pharmacovigilance Programme of India Page 17 Guidance Document For Reporting Individual Case Safety Report New drug - a new drug shall continue to be considered as new drug for a period of four years from the date of its first approval or its inclusion in IP, whichever is earlier. Unknown reaction- Not included in the approved Summary of Product Characteristics Serious reaction- Results into either death, life-threatening condition, hospitalisation or prolonged hospitalisation, disability, congenital anomaly, required intervention to prevent permanent impairment/damage or any other medically important condition 4. Identification of duplicate reports: Certain characteristics of a case (sex, age or date of birth, dates of drug exposure, etc.) may be used to identify duplicate reporting. 5. Causality assessment: With few exceptions, case reports describe suspected adverse drug reactions. The likelihood of a causal relationship between drug exposure and adverse events must be validated. 3.7 Utilization of the Data Data collected in pharmacovigilance can be used in a variety of ways. 1. Signal generation and strengthening: A major aim of pharmacovigilance is the early detection of signals with regard to possible adverse reactions. A signal may be strengthened by further analysis can help the regulatory system in performing regulatory activities. 2. Drug regulation: After approval of a medicinal product, all available domestic and international safety information is continuously monitored by the drug regulatory authority and MAH. The PvPI data can be useful in resolving the problems by adaptation of the approved product information (inclusion of new adverse effects and warnings). 3. Education: The information from PvPI data is useful in updating the knowledge of healthcare professionals during continuous medical education programme on Page 18 pharmacovigilance. Pharmacovigilance Programme of India Guidance Document For Reporting Individual Case Safety Report 3.8 Reporting Requirements in Special Population 3.8.1 Pregnancy and Breastfeeding Pregnancy The clinical trial program of a medicinal product under development rarely includes pregnant women, unless the product is intended specifically for use during pregnancy. All pregnant women coming for routine pre-natal check-ups at various categories of health system must be monitored for any suspected ADR by the healthcare professional. They must be followed-up to collect information on the outcome of the pregnancy and development of the child after birth. At present NCC database contains a limited number of ICSRs related to parent-child case. Intensive monitoring is required to draw any conclusion to upgrade/downgrade pregnancy category of drugs use during pregnancy. Breastfeeding All lactating mother exposed to medicinal product should be monitored to collect information on outcome of lactation on neonates and infants. 3.8.2 Paediatric and Geriatrics The collection of safety information in the paediatric and geriatric population is important as ADRs can lead to significant morbidity and death among these populations. Immunisation is one of the most common and widely used public health interventions in paediatric population. On other hand geriatric population is at higher risk of developing ADRs due to factors like polypharmacy and co-morbidities. The paediatric and geriatric population can be considered to be more vulnerable to some adverse reactions. Therefore, data collected from this program will provide a national database for drug safety information in this vulnerable population. To ensure safe and effective medicines for children and elderly, efforts are needed at different levels (governments, drug regulatory agencies, pharmaceutical industries, health care professionals, and parents).NCC database contains ICSRs reported for paediatric population and geriatric population but more number of case reports are required for monitoring drug safety in these populations. Pharmacovigilance Programme of India Page 19 Guidance Document For Reporting Individual Case Safety Report 3.8.3 Reporting in the Event of a Public Health Emergency A public health emergency is a public health threat duly recognised either by the WHO or MoHFW, Government of India. In the event of a public health emergency, regular reporting requirements may be amended. 3.8.4 Reports of overdose, abuse, off-label use, misuse or OTC Reporting of ADRs encountered with overdose, abuse, off-label use, misuse or occupational exposure is not currently included in PvPI, however physician judgement shall be final. Pharmacovigilance Programme of India Page 20 Guidance Document For Reporting Individual Case Safety Report Chapter 4: Haemovigilance 4.0 Introduction Haemovigilance is a process of data collection and analysis of transfusion -related adverse reactions in order to investigate their causes and outcomes, and prevent their occurrence or recurrence. Indian Pharmacopoeia Commission in collaboration with National Institute of Biologicals has launched Haemovigilance across the country under PvPI with following terms of references: 1. To track Adverse Reactions/ Events and incidence associated with Biologicals, Blood transfusion and Blood product administration (Haemovigilance) as well as tissue organ and cell therapy transplantation. 2. To help in identifying trends, recommend best practices and interventions required to improve patient care and safety, while reducing overall cost of the healthcare system. Haemovigilance Programme was launched on 10th Dec 2012 as an integral part of PvPI. NIB is the Coordinating Centre to collate & analyze data for Haemovigilance. Further information on Haemovigilance is available on http://nib.gov.in/haemovigilance. Pharmacovigilance Programme of India Page 21 Guidance Document For Reporting Individual Case Safety Report 4.1 Transfusion Reaction Reporting Form(TRRF) Pharmacovigilance Programme of India Page 22 Guidance Document For Reporting Individual Case Safety Report Chapter 5: Adverse Event following Immunization 5.0 Introduction AEFI is defined as a medical event that takes place after immunization, causes concern and is believed to be caused by immunization. The AEFI should be handled effectively in order to maintain/restore public faith in immunization program. AEFI Surveillance System in India has come a long way since its inception in 1986. To ensure their safety and efficacy, vaccines are subjected to release a lot at Central Research Institute, Kasauli before release for public use. AEFIs may occur due to the intrinsic property of vaccines and constituents like stabilizers, adjuvant, antibiotics, diluents etc. added to the vaccines or hypersensitivity of some individuals to vaccine component(s). Such incidents are rare but may become apparent in terms of number when vaccinating a large cohort. AEFI may also result from programmatic errors as a result of inappropriate storage, improper handling, preparation and administration etc. of vaccines. AEFI surveillance and timely management will build public confidence and prevent additional clustering of cases if they occur due to a programmatic error. AEFI surveillance monitors immunization safety, detects and responds to adverse events; corrects unsafe immunization practices, reduces the negative impact of the event on health and contributes to the quality of immunization activities. Operational Guidelines of AEFI mainly relate to vaccines included in the National Immunization Program and issues of vaccine manufacturing, safety & quality control of AEFI cases are handled by CDSCO headed by DCGI. Intensive efforts are being made by MoHFW, Government of India to strengthen surveillance and monitoring of AEFI in the country. In India, the safety of vaccine is monitored by the division of AEFI, MoHFW, Government of India and PvPI. AEFI cases submitted to PvPI are further coordinated with national level committee AEFI for reporting & investigation. Subsequently AEFI committee will follow with local AEFI team to completely furnish FIR/PIR/DIR to do the causality assessment. Pharmacovigilance Programme of India Page 23 Guidance Document For Reporting Individual Case Safety Report 5.1 Adverse events following immunization- Reporting Form Pharmacovigilance Programme of India Page 24 Guidance Document For Reporting Individual Case Safety Report Pharmacovigilance Programme of India Page 25 Guidance Document For Reporting Individual Case Safety Report Pharmacovigilance Programme of India Page 26 Guidance Document For Reporting Individual Case Safety Report Pharmacovigilance Programme of India Page 27 Guidance Document For Reporting Individual Case Safety Report Pharmacovigilance Programme of India Page 28 Guidance Document For Reporting Individual Case Safety Report Pharmacovigilance Programme of India Page 29 Guidance Document For Reporting Individual Case Safety Report Pharmacovigilance Programme of India Page 30 Guidance Document For Reporting Individual Case Safety Report Pharmacovigilance Programme of India Page 31 Guidance Document For Reporting Individual Case Safety Report Pharmacovigilance Programme of India Page 32 Guidance Document For Reporting Individual Case Safety Report Chapter 6:Causality Assessment of Adverse Event 6.0 Definition Causality Assessment is defined as the evaluation of the likelihood that a medicine was the causative agent of an observed adverse reaction. 6.1 Why causality assessment? An inherent problem in pharmacovigilance is that most case reports concern suspected adverse drug reactions. Adverse reactions are rarely specific for the drug, diagnostic tests are usually absent and a Re-challenge is rarely ethically justified. In practice few adverse reactions are ‘certain’ or ‘unlikely’; most are somewhere in between these extremes, i.e. ‘Possible’ or ‘Probable’. In an attempt to solve this problem many systems have been developed for a structured and harmonised assessment of causality but none of these systems, have shown to produce a precise and reliable quantitative estimation of relationship. Nevertheless, causality assessment has become a common routine procedure in pharmacovigilance. AMC is responsible for performing causality assessment of reports which shall be reviewed at NCC. The PvPI follows WHO-UMC causality assessment scale for establishing the relation between the suspected drug and suspected adverse drug event. The WHO-UMC scale is used as a practical tool for the assessment of case reports. It is basically a combined assessment taking into account the clinical-pharmacological aspects of the case history and the quality of the documentation of the observation. 6.2 Advances and limitations of standardised case causality assessment What causality assessment can do What causality assessment cannot do Decrease disagreement between assessors Give accurate quantitative measurement of Relationship likelihood Classify relationship likelihood Distinguish valid from invalid cases Mark individual case reports Prove the connection between drug and event Improvement of scientific evaluation; Educational Pharmacovigilance Programme of India Quantify the contribution of a drug to the Development of an adverse event Change uncertainty into certainty Page 33 Guidance Document For Reporting Individual Case Safety Report 6.3 WHO-UMC Causality Assessment Scale Causality term Certain Assessment criteria Probable/ Likely Possible Event or laboratory test abnormality, with plausible time relationship to drug intake Cannot be explained by disease or other drugs Response to withdrawal plausible (pharmacologically, pathologically) Event definitive pharmacologically or phenomenological (i.e. an objective and specific medical disorder or a recognised pharmacological phenomenon) Re-challenge satisfactory, if necessary Event or laboratory test abnormality, with reasonable time relationship to drug intake Unlikely to be attributed to disease or other drugs Response to withdrawal clinically reasonable Re-challenge not required Event or laboratory test abnormality, with reasonable time relationship to drug intake Could also be explained by disease or other drugs Information on drug withdrawal may be lacking or unclear Event or laboratory test abnormality, with a time to drug intake that makes a relationship improbable (but not impossible) Disease or other drugs provide plausible explanations Conditional/ Unclassified Event or laboratory test abnormality More data for proper assessment needed, or Additional data under examination Unassessable/ Unclassifiable Report suggesting an adverse reaction Cannot be judged because information is insufficient or contradictory Data cannot be supplemented or verified Unlikely Pharmacovigilance Programme of India Page 34 Guidance Document For Reporting Individual Case Safety Report Chapter 7: Signal Detection and Evaluation Signal detection and its clinical assessment is an important domain of pharmacovigilance. The WHO has defined a Signal as “Reported information on a possible causal relationship between an adverse event and a drug, the relationship being unknown or incompletely documented previously.” It is worth mentioning that a signal does not imply causation but it can only provide preliminary information about postulating a hypothesis and not for testing it. Analysis of any pharmacovigilance database can be used for signal detection but it is reviewed by clinicians and other experts to arrive at decision making. Signal detection process in a spontaneous ADR database is based on different statistical methodology - either the Bayesian or Frequentist statistical approach. Whichever method is employed, basically it involves computation of measures of disproportionality i.e. determination to what extent the number of observed cases differs from the number of expected cases. All disproportionality algorithms despite having operational technique variability actually calculate surrogate observed to expected ratios in which the reporting experience of each reported drug-adverse event combination is compared to the background reporting experience across all drugs and events in the database using an independence model. The WHO UMC uses the BCPNN – (Bayesian Confidence Propagation Neural Network) while US FDA uses the MGPS- (Multi item Gamma Poisson Shrinker) methodologies. Other disproportionality analyses methods are ROR (Reporting Odds Ratio), PRR (Proportional Reporting Ratio) are employed by some national reporting centres (MHRA, UK) and drug safety research units. In the BCPNN methodology computation of the Information Component is based on prior and posterior probabilities. As per the WHO-UMC, the IC measures the disproportionality in the reporting of a drug-ADR pair in an ICSR database, relative to the reporting expected based on the overall reporting of the drug and the ADR. Positive IC values indicate higher reporting than expected. However, review of signals generated by using such tools must be analysed by clinicians and drug safety experts before arriving at a conclusion. Whichever method is used for signal detection, each has its advantages and disadvantages and therefore is no single method which can be considered as the gold standard. The PVPI is Pharmacovigilance Programme of India Page 35 Guidance Document For Reporting Individual Case Safety Report currently analysing its own national database and a signal review panel will shortly formulate its strategy for signal detection and its assessment. Pharmacovigilance Programme of India Page 36 Guidance Document For Reporting Individual Case Safety Report Chapter 8: PvPI and WHO-UMC Collaboration IPC-NCC has free access to the databases provided by WHO-UMC which helps in achieving the objectives of PvPI in a more efficient way. 8.0 VigiFlow VigiFlow is a web-based ICSR management system that is specially designed for use by national centres in the WHO Programme for International Drug Monitoring. VigiFlow is based on and compliant with the ICH E2B standard and is a trademark of the UMC and maintained by the UMC in Uppsala, Sweden. It offers a simple, fast and secure web-based solution that improves all aspects of ADR reporting. ICSR data can be manually entered into VigiFlow with support from the latest versions of terminologies such as the WHO-DD and WHO-ART or MedDRA. Once a report is complete and committed the first version of the ICSR is considered to be finalized. It is easy to retrieve reports to amend the contents or add follow-up information. ICSRs will automatically be flagged for being copied to VigiBase, the WHO Global ICSR database when they are committed. 8.1 VigiMed VigiMed is a web-based forum for those working at national centres in the WHO Programme to have easy access to safety concerns in other countries, to check regulatory status, and to expedite the sharing of drug information. VigiMed is part of the UMC collaboration portal, a web-based platform managed by the UMC. 8.2 VigiSearch VigiSearch is a powerful search tool that provides access to all case reports in VigiBase. VigiSearch allows for report searching across multiple drugs and ADRs simultaneously, as well as incorporating a range of filters. Drugs can be searched on a generic substance level or a specific trade name. VigiSearch also supports browsing the ATC structure. The results can be accessed on an overview level and viewed from a number of aspects (country, year, reaction term) or at the level of individual case report. For members of the WHO Programme, VigiSearch enables an international comparison of national spontaneous reporting data, as well as giving access to ADR information on drugs that are not yet on the national market. Pharmacovigilance Programme of India Page 37 Guidance Document For Reporting Individual Case Safety Report 8.3 VigiLyze VigiLyze is a powerful search and analysis tool that provides access to more than 8 million ICSRs in VigiBase, submitted from over 100 countries. VigiLyze includes data on conventional medicines, traditional medicines as well as biological medicines including vaccines. VigiLyze can be used to have a global, regional or national view of an ADR identify or monitor international patient safety data. It can be useful to find supporting evidence while assessing Indian case reports or to see how Indian data support global pharmacovigilance. VigiLyze enables international comparison with national spontaneous reporting data, as well as giving access to ADR information on drugs that are not yet on our national market. Results from VigiLyze are instantly available as graphics as well as in tabular format. Pharmacovigilance Programme of India Page 38 Guidance Document For Reporting Individual Case Safety Report VigiFlow- Demo Chart User ID Password LOG-IN DETAIL Change Password Retrieve Unsaved Report Language Quick Start Main Menu Mandatory Fields: Report Title, Patient Initials, Patient Age, Gender, Reaction term, Onset Date of Reaction, Drug Name, date of therapy started, indication of use, seriousness, outcome, de-challenge , re-challenge details, reporter details 1 2 Pharmacovigilance Programme of India 3 4 Page 39 Guidance Document For Reporting Individual Case Safety Report 5 6 7 THE CAUSALITY ASSESSMENT SAVE REPORT SEND REPORT TO NCC COMMIT REPORT Pharmacovigilance Programme of India Page 40 Guidance Document For Reporting Individual Case Safety Report Chapter 9: Risk Management, Communication and Publications 9.0 Risk Management Risk management is the identification, assessment, and prioritization of risks followed by coordinated and economical application of resources to minimize, monitor, and control the probability and impact of unfortunate events. It is the discipline within pharmacovigilance that is responsible for signal detection and the monitoring of the risk-benefit profile of drugs. At the time of marketing authorisation, the benefit-risk balance is judged to be positive for the target population. A medicinal product is associated with multiple risks and individual risks will vary in terms of severity, effect on individual patients and public health impact. However, at the time when an initial authorisation is sought all the risks (actual or potential) have not been identified and many of the risks associated with the use of a medicinal product will only be discovered and characterised during post-authorisation. Risk management has three stages which are inter-related as mentioned below: 1. Characterisation of the safety profile of the medicinal product including what is known and not known. 2. Planning of pharmacovigilance activities is to characterise and identify new risks and increase the knowledge in general about the safety profile of the medicinal product. 3. Planning and implementation of risk minimisation, mitigation and assessment of the effectiveness of these activities. Risk management is a global activity. However the benefits and risk of a medicinal product may also vary between regions as they differ in disease prevalence, severity, population genetics (South Indian, North Indian, East Indian and West Indian). The overall aim of risk management is to ensure that the benefits of a particular medicinal product exceed the risks by the greatest achievable margin for the individual patient and for the target population as a whole. 9.1 Communication Communicating safety information to patients and healthcare professionals is a public health responsibility and is essential for achieving the objectives of pharmacovigilance in terms of promoting the rational, safe and effective use of medicine, preventing harm from adverse Pharmacovigilance Programme of India Page 41 Guidance Document For Reporting Individual Case Safety Report reactions and contributing to the protection of public health. Communication in PvPI improves patient care, understanding, promotes transparency and accountability. All the communications with WHO-UMC will be managed by NCC. All the issues associated with drug safety are reported to CDSCO which will further take appropriate regulatory decision and action on the basis of recommendation of NCC. The objective of communication in PvPI aims to provide evidence based information on the safe and effective use of medicine and regulatory status of medicines in India as well as globally. For this PvPI is using different modes of communications as follow: Press communication It includes press release and press briefings which are primarily intended for journalists. The Secretary-Cum-Scientific Director, IPC is the only designated authority to correspond with media, related to all activities and issues of PvPI. Website A website is a key tool for the stakeholders including patients and health professionals. NCC and CSDCO shall ensure that all important safety information should be published on the websites under their control. Newsletter To communicate the findings and regulatory status of medicine in India as well as globally to the stakeholders, IPC-NCC publishes newsletter i.e. “PvPI Newsletter” three issues in a year. This newsletter is for everyone concerned with the issues of pharmacovigilance which provides practical information and advice on drug safety and information about emerging safety issues. The newsletter can also be downloaded from IPC website www.ipc.gov.in under Pharmacovigilance Program of India. 9.2 Publications IPC publishes Indian Pharmacopoeia, a book of standards for drugs in India as per Drugs and Cosmetics Act, 1940 (the act) and Rules 1945. Also IPC publishes National Formulary of India which is a guidance document for rational use of medicines. Pharmacovigilance Programme of India Page 42 Guidance Document For Reporting Individual Case Safety Report Chapter 10: Audit of PvPI To ensure the PvPI operates effectively and achieves its objectives, the center will establish key indicators to measure the efficiency of (i) process (ii) outcome and (iii) impact of the PvPI. The following indicators will be measured: A. Personnel’s details: 1. Personnel prior education and GVP experience. 2. Whether GVP training provided by the Zone/NCC 3. Do personnel know the job descriptions/responsibilities? B. Administrative Responsibility: 1. Whether infrastructure is sufficient for PV? 2. Whether sufficient working place? 3. Whether logistic support provided by NCC such as Computer system, internet connection are work properly? 4. Storage of hard copies as well as soft copies of documents. 5. Whether co-operation by other dept. to PV section? C. Documents Review: 1. Verify version number and effective date of SOPs provided to NCC with AMC’s SOPs. 2. Verify Training Records/Certificates. 3. Randomly verify the data of source documents with entreated ICSRs. D. Quality Assurance: 1. Does the source document mentions Essential Required Item such as patient information/ division/ reaction with date/ suspected drug with date/ outcome and sender information? 2. Determine whether data entry by TA in VigiFlow is same with source documents. 3. Whether all ADRs were reported in Suspected ADR Reporting Form. 4. Verify the timeline for reporting the SAE to NCC and CDSCO. E. Data collection and its security: 1. Use of electronic data capture or data transcription from Suspected ADR Reporting into an electronic record (VigiFlow). 2. Record retention. 3. Data security in case of disasters, e.g., power failure. 4. Contingency plans and backup files. 5. Determine whether personnel has Access methods e.g., User ID/password for the security of electronic data. Pharmacovigilance Programme of India Page 43 Guidance Document For Reporting Individual Case Safety Report F. Competence of Technical Associate: 1. 2. 3. 4. He/She is conversant with the drug for which he/she is sending the report? Is he/she conversant with the Rechallenge and Dechallenge process? Is this a side effect or ADR? Any SAE reported from the centre? How quickly it was forwarded. G. Authenticity of Data: 1. Mechanism of identifying the patient from the registration number of the case report – random check should be done by the inspecting team 2. How many times TA visits various wards. 3. How quickly he/she sends the report to NCC. 4. Is he/she taking interest in reporting drugs of current interest i.e. from CVS, Psychiatry, Oncology and Diabetes? 5. Interaction with coordinator – frequency and documentation for the same. H. Core Structural Indicators: 1. 2. 3. 4. 5. 6. 7. 8. Does the AMC have standard accommodation? Whether NCC has given acceptance letter? A regular financial provision for the AMC? Human resources to carry out its functions properly? A standard ADR reporting form? A process in place for collection, recording and entering of ADRs in VigiFlow? Newsletters/NFI/Information bulletin/website for PV information dissemination? A PV advisory committee or expert committee in the setting? I. Core Process Indicators: 1. 2. 3. 4. 5. 6. Total number of ADR reports reported to NCC last calendar year. Percentage of total annual reports acknowledged by NCC. Percentage of reports subjected to causality assessment in the year. Percentage of reports on therapeutic ineffectiveness. Percentage of reports on medication error. Number of active surveillance activities initiated, on-going or completed, the last 5 years. J. Core Outcome/Impact Indicators: 1. 2. 3. 4. 5. 6. Number of medicine related hospital admissions/1000 admissions. Number of medicine related deaths/1000 persons served by hospital. Number of medicine related deaths/100000 in the population. Average cost of treatment of medicine-related illness. Average duration of extension of medicine-related hospital stay. Average cost of medicine related hospitalization. Pharmacovigilance Programme of India Page 44 Guidance Document For Reporting Individual Case Safety Report Pharmacovigilance Programme of India Page 45 Guidance Document For Reporting Individual Case Safety Report Annexure 1: Contact details of AMC reporting under PvPI LIST OF 90 ADR MONITORING CENTRES UNDER PHARMACOVIGILANCE PROGRAMME OF INDIA (PvPI) S. No 1. 2. 3. 4. 5. State Centre Name Andhra Pradesh Andhra Medical College King George Hospital (KGH), Visakhapatnam Guntur Medical College, Guntur Kakatiya Medical College, Warangal Nizam Institute of Medical Sciences, Hyderabad Department of Pharmacology, Govt. Medical College, Guwahati Silchar Medical College & Hospital, Ghungoor, Silchar Indira Gandhi Institute of Medical Sciences, Shekhpura, Patna Goa Medical College & Hospital, Bambolim Assam 6. 7. Bihar 8. Goa 9. Gujarat 10. SMT NHL Municipal Medical Ahmadabad BJ Medical College, Ahmadabad Coordinator name Dr. J. Sudha [email protected] Dr. Zaheda Bano Dr. Raju Devde Dr. Shobha Udutha Dr. Mangala Lahkar [email protected] [email protected] [email protected] [email protected] Dr.Pinaki Chakravarty [email protected] Dr. Harihar Dikshit [email protected] Dr. Padmanabh V. Rataboli [email protected] m [email protected] College, Dr. Varsha J Patel Dr. R.K. Dikshit 13. Government Medical College, Bhavnagar Dr. C B Tripathi Surat Municipal Institute of Medical Education & Dr. Sachendra Ku. Srivastava Research, Surat M.P. Shah Medical College, Jamnagar Dr. Hiren R. Trivedi 14. PDU Medical College, Rajkot 11. 12. Pharmacovigilance Programme of India Email Dr. S. T. Hotchandani [email protected]/ramdiksh [email protected] [email protected] [email protected]/drarvi [email protected] [email protected]/ [email protected] [email protected] Page 46 Guidance Document For Reporting Individual Case Safety Report Medanta-The Medicity Sector-38, Gurgaon PanditBhagwatDayal Sharma, Post Graduate Institute of Medical Sciences, Rohtak Dr. Himanshu Baweja Dr MC Gupta [email protected] [email protected]/ [email protected] Dr. Vishal Tandon Dr. ZA Wafai [email protected] [email protected] Dr. Janardan Sharma [email protected] Dr. C. R. Jayanthi [email protected] 21. 22. 23. 24. Govt. Medical College, Bakshi Nagar, Jammu Sher-i-Kashmir Institute of Medical Sciences, Srinagar Rajendra Institute of Medical Sciences (RIMS), Ranchi Bangalore Medical College and Research Institute, Bengaluru Belgaum Institute of Medical Sciences, Belgaum Bidar Institute of Medical Sciences, Bidar JSS Medical College Hospital, Mysore Karnataka Institute OF Medical Sciences, Hubli Dr. Basavaraj Kotintot Dr. B.O. Hanumanthappa Dr. Parthasarathi G Dr. Janaki. R. Torvi 25. Kasturba medical College, Manipal Dr. K. L. Bairy 26. Mandya Institute of Medical Sciences (MIMS), Dr. Nagabushan District Hospital Campus, Mandya SDS Tuberculosis Research Centre & Rajiv Dr. Shashidhar Buggi Gandhi Institute of Chest Disease, Bengaluru [email protected] [email protected] [email protected] [email protected]/kims_hubl [email protected] [email protected]/klbairy@yah oo.com [email protected] 15. 16. Haryana 17. 18. J&K 19. Jharkhand 20. Karnataka 27. 28. 29. St. John’s Medical College, Bengaluru Vijaynagar Institute of Medical Sciences, Bellary Dr. Padmini Devi Dr. C. Lakshmi Narayana 30. Vydehi Institute of Medical Sciences Research Centre, Bengaluru Govt. Medical College Kozhikode Dr. P.V. Narayanan 31. 32. Kerala Govt. Medical College, Kottayam Pharmacovigilance Programme of India and Dr. Pratibha Nadig Dr. Kala Kesavan [email protected]/direct [email protected] [email protected] [email protected]/blydrkln @gmail.com [email protected] [email protected] .in [email protected] Page 47 Guidance Document For Reporting Individual Case Safety Report 33. 34. 35. 36. 37. Madhya Pradesh Maharashtra 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. Odisha Pushpagiri Institute of Medical Sciences and Research centre, Pushpagiri Medical College Hospital, Tiruvalla Gandhi Medical College, Bhopal RD Gardi Medical College, Ujjain SAIMS Medical College, Indore BJ Medical College & Sassoon General Hospital, Pune Government Medical College & Hospital, Nagpur Dr. Santosh Pillai [email protected] Dr. Arun Srivastav Dr. S.P. Dhaneria Dr. Chhaya Goyal Dr. Pradeep Deshpande Grant medical college & Sir JJ Group of Hospital, Mumbai Indira Gandhi Government Medical College, Nagpur LokmanyaTilak municipal Medical College & General Hospital, Mumbai Mahatma Gandhi Institute of Medical Sciences, Nagpur MGM Medical College and Hospital, Kalamboli, Navi Mumbai Pd. Dr. D.Y. Patil Medical College, Pimpri, Pune Seth GS Medical College & KEM Hospital, Parel, Mumbai Swami Ramanand Teerth Rural Govt Medical College, Ambajogai TN Medical College &Byl Nair Hospital, Mumbai Central, Mumbai VSS Medical College, Burla M. K. C. G Medical College, Berhampur SCB Medical College and Hospital, Cuttack Dr. S. B. Patel [email protected] [email protected] [email protected] pradeepdeshpande.deshpande69@g mail.com [email protected]/gndakhle @rediffmail.com [email protected]/dr.sbpat [email protected] [email protected],/am1 [email protected] [email protected] Pharmacovigilance Programme of India Dr. Ganesh N. Dakhle Dr. Vandana Avinash Badar Dr. Sudhir R. Pawar Dr. Sushil Kumar Varma Dr. Daniel Joseph Dr. P.S. Worlikar Dr. Urmila Thatte [email protected]/varmasushil9 @gmail.com [email protected] Dr. V.M. Motghare [email protected] [email protected]/urmilathatt [email protected] [email protected] Dr. Renuka Kulkarni-Munshi [email protected] Dr. Sabita Mohapatra Dr. Bandana Rath Dr. Srikanta Mohanty [email protected] [email protected] [email protected]/adr.sc [email protected]/ Page 48 Guidance Document For Reporting Individual Case Safety Report 51. Punjab 52. 53. 54. Rajasthan 55. 56. 57. 58. 59. 60. 61. 62. 63. 64. 65. 66. 67. 68. 69. Christian Medical College and Hospital, Brown Road, Ludhiana Dayanand Medical College and Hospital, Ludhiana Govt. Medical College Patiala Sardar Patel Medical College, Bikaner Dr. Dinesh Kumar Badyal [email protected] [email protected] Dr. Sandeep Kaushal [email protected] Dr. Anita Gupta Dr. Kiran Barar SMS Medical College, Jaipur Dr. Mukul Mathur Dr. Supratim Datta [email protected] [email protected]/kiran [email protected] [email protected]/co [email protected] [email protected] Dr. Dr. J.V. peter Dr. C. Ramachandra Bhat Dr. R Nandini Dr. S. Ramalingam peterjohnvictor @yahoo.com.au [email protected] [email protected] [email protected] Dr. Jamuna Rani [email protected] Dr. Debasis Ray Dr. T.N. Sharma [email protected] [email protected] Dr. P.P. Gupta [email protected] Dr S.P. Singh Dr. B.L. Pandey [email protected] [email protected] Dr. Mohammad Nasiruddin [email protected] Dr.Sadhna Kaushik Dr. Rakesh Chandra Chaurasia [email protected] [email protected] Sikkim Manipal Institute of Medical Sciences, Tadong, Gangtok Tamil Nadu Christian Medical College, Vellore Govt. Kilpauk Medical College, Chennai Madras Medical College, Chennai PSG Institute of Medical Sciences & Research, Coimbatore SRM Medical College Hospital & Research Centre, kattankulathur, Chennai Agartala Govt. Medical College, Agartala Tripura Tripura Medical College & Dr. BRAM Teaching Hospitals, Hapania, Agartala Uttar Pradesh B.R.D Medical College & Nehru Hospital, Gorokhpur GSVM Medical College, Swaroop Nagar, Kanpur Institute of Medical Sciences Banaras Hindu University, Varanasi JN Medical College Aligarh Muslim University , Aligarh M.L.B. Medical College, Jhansi M.L.N Medical College, Allahabad Sikkim Pharmacovigilance Programme of India Page 49 Guidance Document For Reporting Individual Case Safety Report 70. 71. 72. 73. Uttarakhand 74. 75. West Bengal 76. 77. 78. 79. 80. 81. 82. 83. 84. 85. 86. 87. 88. Chandigarh Delhi Santosh Medical University, Santosh Nagar, Ghaziabad U.P Rural Institute of Medical Sciences and Research, Safai, Etwah Govt Medical College, Haldwani Himalayan Institute of Medical Sciences, Dehradun Veer Chandra Singh Garhwali Medical Science and Research Institute, Srinagar, Garhwal School of Tropical Medicine, Chittaranjan Avenue, Kolkata R.G. Kar Medical College, Kolkatta Calcutta National Medical College, Kolkata Institute of Postgraduate Medical Education & Research, Kolkata Burdwan Medical college, Burdwan BankuraSammilani Medical College, Bankura Dr. VC Chopra [email protected] Dr. Asha Pathak [email protected] Dr. Bhavana Srivastava Dr. DC Dhasmana [email protected] [email protected] Dr. Vijay Thawani Dr. Santanu Tripathi [email protected] om/[email protected] [email protected] Dr. Anjan Adhikari Dr. Syed Mohammad Naser Dr. Suparna Chatterjee [email protected] [email protected] [email protected] Dr. Swati Bhattacharyya Dr. Santanu Munshi NilratanSircar Medical College, Kolkata PGIMER, Chandigarh All India Institute of Medical Sciences (AIIMS) Prof. Nina Das Dr. Bikash Medhi Dr. Y.K. Gupta Indraprastha Apollo Hospital Lady Hardinge Medical College (LHMC) University College of Medical Sciences, Dilshad Garden Vallabhbhai Patel Chest Institute (VPCI) University of Delhi VMMC &Safdarjung Hospital Dr. Lalit Kanodia Dr. H.S. Rehan Dr. S. K. Bhattacharya [email protected] [email protected]/ [email protected] [email protected] [email protected] [email protected]/ [email protected] [email protected] [email protected] [email protected] Dr. A. Ray [email protected] Dr. C.D. Tripathi [email protected] Pharmacovigilance Programme of India Page 50 Guidance Document For Reporting Individual Case Safety Report 89. 90. Puduchery Indira Gandhi Medical College & Research Dr. G. Sivagnanam Institute, Kadirkamam. JIPMER, Pondicherry Dr. C Adithan Pharmacovigilance Programme of India [email protected]/adigaisc [email protected] [email protected] Page 51 Guidance Document For Reporting Individual Case Safety Report Annexure 2: Pharmacovigilance Terminologies used in Absolute risk Risk in a population of exposed persons; the probability of an event affecting members of a particular population (e.g. 1 in 1,000). Absolute risk can be measured over time (incidence) or at a given time (prevalence). Adverse event Any untoward medical occurrence that may present during treatment with a pharmaceutical product but which does not necessarily have a causal relationship with this treatment. Adverse (drug) reaction (ADR) A response which is noxious and unintended, and which occurs at doses normally used in humans for the prophylaxis, diagnosis, or therapy of disease, or for the modification of physiological function. (WHO, 1972). An adverse drug reaction, contrary to an adverse event, is characterized by the suspicion of a causal relationship between the drug and the occurrence, i.e. judged as being at least possibly related to treatment by the reporting or a reviewing health professional. Association Events associated in time but not necessarily linked as cause and effect. Attributable risk Difference between the risk in an exposed population (absolute risk) and the risk in an unexposed population (reference risk). Also referred to as excess risk. Attributable risk is the result of an absolute comparison between outcome frequency measurements, such as incidence. Examples: If the exposed persons with a particular outcome are A, the exposed persons without the outcome are B, the unexposed persons with the outcome are C and the unexposed persons with the outcome are D, then the attributable risk is calculated as : [A / (A+B)] - [C / (C+D)]. If, during the same time period, the incidence of rash in a population treated with Pharmacovigilance Programme of India Page 52 Guidance Document For Reporting Individual Case Safety Report medicine X is 20/1,000=0.02, and the incidence of rash in a population not treated with X is 5/2,000=0.0025, the attributable risk is (20/1,000) - (5/2,000) = 0.0175. Benefit An estimated gain for an individual or a population. See also Effectiveness/Risk. Benefit - risk analysis Examination of the favourable (beneficial) and unfavourable results of undertaking a specific course of action. (While this phrase is still commonly used, the more logical pairings of benefit-harm and effectiveness-risk are slowly replacing it). Biological products Medical products prepared from biological material of human, animal or microbiologic origin (such as blood products, vaccines, insulin). Causal relationship A relationship between one phenomenon or event (A) and another (B) in which A precedes and causes B. In pharmacovigilance; a medicine causing an adverse reaction. Causality assessment The evaluation of the likelihood that a medicine was the causative agent of an observed adverse reaction. Causality assessment is usually made according established algorithms. CIOMS The Council for International Organizations of Medical Sciences (CIOMS) is a body set up under World Health Organization and UNESCO. It has developed a series of guidelines on pharmacovigilance, drawn up by a committee of volunteers from Industry, regulatory authorities, WHO and others. The main guidelines concern the international reporting form (CIOMS I); periodic safety update reports (CIOMS II); core data sheets (CIOMS III); benefit-risk assessments (CIOMS IV); practical issues in pharmacovigilance (CIOMS V); clinical trial safety data (CIOMS VI); and development safety update reports (CIOMS VII). Pharmacovigilance Programme of India Page 53 Guidance Document For Reporting Individual Case Safety Report Clinical trial A systematic study on pharmaceutical products in human subjects (including patients and other volunteers) in order to discover or verify the effects of and/or identify any adverse reaction to investigational products, and/or to study the absorption, distribution, metabolism and excretion of the products with the objective of ascertaining their efficacy and safety. Cohort Event Monitoring Cohort Event Monitoring (CEM) is a prospective, observational study of events that occur during the use of medicines, for intensified follow-up of selected medicinal products phase. Patients are monitored from the time they begin treatment, and for a defined period of time. See also Prescription Event Monitoring. Common Epidemiology In pharmacovigilance, an event with a frequency between 1 in 100 and 1 in 10. Co-morbidities Two or more coexisting medical conditions or disease processes that are additional to an initial diagnosis. Compliance Faithful adherence by the patient to the prescriber's instructions. Congenital Anomalies Morphological, functional and/or biochemical developmental disturbance in the embryo or foetus whether detected at birth or not. The term congenital anomaly is broad and includes congenital abnormalities, foetopathies, genetic diseases with early onset, developmental delay, etc. Control group The comparison group in drug-trials not being given the studied drug. Critical terms Some of the terms in WHO-ART are marked as "Critical Terms". These terms either refer to or might be indicative of serious disease states, and warrant special attention, because of their Pharmacovigilance Programme of India Page 54 Guidance Document For Reporting Individual Case Safety Report possible association with the risk of serious illness which may lead to more decisive action than reports on other terms. Data-mining At the UMC, the use of an automated tool, based on Bayesian logic, for the scanning of the WHO database (VigiBase) in the process of detecting drug-adverse reaction associations: the BCPNN. Knowledge-detection is the preferred term for the process. De-challenge The withdrawal of a drug from a patient; the point at which the continuity, reduction or disappearance of adverse effects may be observed. Disproportionality analysis Screening of ICSR databases for reporting rates which are higher than expected. For drugADR pairs, common measures of disproportionality are the Proportional Reporting Ratio (PRR), the Reporting Odds Ratio (ROR), The Information Component (IC), and the Empirical Bayes Geometrical Mean (EBGM). There are also disproportionality measures for drug-drug-ADR triplets, such as Omega (Ω). Drug Abuse It is a patterned use of a drug in which the user consumes the substance in amounts or with methods neither approved nor supervised by medical professionals. Effectiveness/risk The balance between the rate of effectiveness of a medicine versus the risk of harm is a quantitative assessment of the merit of a medicine used in routine clinical practice. Comparative information between therapies is most useful. This is more useful than the efficacy and hazard predictions from pre-marketing information that is limited and based on selected subjects. Efficacy The ability of a drug to produce the intended effect as determined by scientific methods, for example in pre-clinical research conditions (opposite of hazard). Pharmacovigilance Programme of India Page 55 Guidance Document For Reporting Individual Case Safety Report Epidemiology The science concerned with the study of the factors determining and influencing the frequency and distribution of disease, injury and other health-related events and their causes in a defined human population for the purpose of establishing programs to prevent and control their development and spread (Dorland's Illustrated Medical Dictionary). Essential medicines Essential medicines are those that satisfy the priority health care needs of the population. They are selected with due regard to public health relevance, evidence on efficacy and safety, and comparative cost-effectiveness. EVMPD The EudraVigilance Medicinal Product Dictionary (EVMPD) has been developed by the European Medicines Agency in collaboration with the EudraVigilance Joint Implementation Group. The main objective of the EVMPD is to assist the pharmacovigilance activities in the European Economic Area. EUDRAGENE Eudragene is a European collaboration that established a collection of DNA samples as a resource for studying genes which influence serious or adverse drug reactions (ADRs). Identifying genes that influence susceptibility to adverse reactions will advance understanding of the basis of adverse drug reactions and may also lead to the development of tests that can predict individual susceptibility to adverse reactions. Excipients All materials included to make a pharmaceutical formulation (e.g. a tablet) except the active drug substance(s). Formulary A listing of medicinal drugs with their uses, methods of administration, available dose forms, side effects, etc., sometimes including their formulas and methods of preparation. Pharmacovigilance Programme of India Page 56 Guidance Document For Reporting Individual Case Safety Report Generic (multisource product) The term "generic product" has somewhat different meanings in different jurisdictions. Generic products may be marketed either under the non-proprietary approved name or under a new brand (proprietary) name. They are usually intended to be interchangeable with the innovator product, which is usually manufactured without a license from the innovator company and marketed after the expiry of patent or other exclusivity rights. Harm The nature and extent of actual damage that could be caused by a drug. Not to be confused with risk. ICH The International Conference on Harmonization of Technical Requirements for the Registration of Pharmaceuticals. ICD International Classification of Diseases (ICD) is the standard diagnostic tool for epidemiology, health management and clinical purposes. Incidence The extent or rate of occurrence, especially the number of new cases of a disease in a population over a period of time. Individual Case Safety Report A report that contains information describing a suspected adverse drug reaction related to the administration of one or more medicinal products to an individual patient. MedDRA MedDRA or Medical Dictionary for Regulatory Activities is a clinically-validated international medical terminology used by regulatory authorities and the regulated biopharmaceutical industry. The terminology is used through the entire regulatory process, from pre-marketing to post-marketing, and for data entry, retrieval, evaluation, and presentation. Pharmacovigilance Programme of India Page 57 Guidance Document For Reporting Individual Case Safety Report Medical error "An unintended act (either of omission or commission) or one that does not achieve its intended outcomes." Leape, Lucien. Error in Medicine. Journal of the American Medical Association 272(23):1851-57 (Dec. 21, 1994). Over the counter (OTC) Medicines which are available for purchase without prescription. Off-label-use When the medicinal product is intentionally used for a medical purpose not in accordance with the authorised product information. Overdose Administration of a quantity of a medicinal product given per administration or cumulatively, which is above the maximum recommended dose according to the authorised product information. Pharmacoepidemiology Study of the use and effects of drugs in large populations. Pharmacology Pharmacology is the science of drugs (Greek: Pharmacon-drug; logos-discourse in) . In a broad sense, it deals with interaction of exogenously administered chemical molecules (drugs) with living systems. It encompasses all aspects of knowledge about drugs, but most importantly those that are relevant to effective and safe use for medicinal purposes. Pharmacovigilance The science and activities relating to the detection, assessment, understanding and prevention of adverse effects or any other drug-related problem. Phocomelia Characteristic deformity caused by exposure to thalidomide in the womb, also very rarely occurring spontaneously. Meaning: limbs like a seal. Pharmacovigilance Programme of India Page 58 Guidance Document For Reporting Individual Case Safety Report Placebo An inactive substance (often called a sugar pill) given to a group being studied to compare results with the effects of the active drug. Polypharmacy The concomitant use of more than one drug, sometimes prescribed by different practitioners. Post-authorization safety study (PASS) A pharmacoepidemiological study or a clinical trial carried out in accordance with the terms of the Marketing Authorisation, with the aim of identifying or quantifying a safety hazard relating to an authorized medicinal product. Post-marketing The stage when a drug is generally available on the market. Predisposing factors Any aspect of the patient’s history (other than the drug) which might explain reported adverse events (for example, genetic factors, diet, alcohol consumption, disease history, polypharmacy or use of herbal medicines). Pre-marketing The stage before a drug is available for prescription or sale to the public. Prescription event monitoring (PEM) System created to monitor adverse drug events in a population. Prescribers are requested to report all events, regardless of whether they are suspected adverse events, for identified patients receiving a specified drug. Also more accurately named "cohort-event monitoring". Prescription only medicine (POM) Medicinal product available to the public only on prescription. Prophylaxis Prevention or protection. Pharmacovigilance Programme of India Page 59 Guidance Document For Reporting Individual Case Safety Report PSUR The Periodic Safety Update Report (PSUR) is a stand-alone document that allows a periodic but comprehensive assessment of the worldwide safety data of a marketed drug or biological product. QPPV Qualified Person responsible for Pharmacovigilance. Rare In pharmacovigilance an event with a probability between 1 in 10,000 and 1 in 1,000. Rational drug use An ideal of therapeutic practice in which drugs are prescribed and used in exact accordance with the best understanding of their appropriateness for the indication and the particular patient, and of their benefit, harm effectiveness and risk. Re-challenge The point at which a drug is again given to a patient after its previous withdrawal (see dechallenge). Reference risk Risk in a population of unexposed persons. Also called baseline risk. Reference risk can be measured over time (incidence) or at a given time (prevalence). The unexposed population refers to a reference population, as closely comparable to the exposed population as possible, apart from the exposure. Regulatory authority The legal authority in any country with the responsibility of regulating all matters relating to drugs. Relative risk Ratio of the risk in an exposed population (absolute risk) and the risk in an unexposed population (reference risk). Relative risk is the result of a relative comparison between outcome frequency measurements, e.g. incidences. Pharmacovigilance Programme of India Page 60 Guidance Document For Reporting Individual Case Safety Report Example: If the exposed persons with an outcome are A, the exposed persons without the outcome are B, the unexposed persons with the outcome are C, and the unexposed persons without the outcome are D, the relative risk is calculated as [A / (A+B)] / [C / (C+D)]. If the incidence of rash in a population treated with medicine X is 35/1,500=0.023, and the incidence of rash in a population which is not treated with X, during the same time period, is 5/2,000=0.0025, the relative risk is (35/1,500) / (5/2,000) = 9.3. Risk The probability of harm being caused; the probability (chance, odds) of an occurrence. SAEC The International Serious Adverse Events Consortium (SAEC) is a non-profit consortium formed in October 2007 between industry, academia, the Wellcome Trust, and the US Food and Drug Administration to identify genetic variants associated with serious adverse events. Serious Adverse Event or Reaction A serious adverse event or reaction is any untoward medical occurrence that at any dose: results in death results in life-threatening condition requires inpatient hospitalization or prolongation of existing hospitalization results in persistent or significant disability/incapacity causes congenital abnormality requires any intervention to prevent the occurrence of any of the above To ensure no confusion or misunderstanding of the difference between the terms "serious" and "severe", the following note of clarification is provided: The term "severe" is not synonymous with serious. In the English language, "severe" is used to describe the intensity (severity) of a specific event (as in mild, moderate or severe); the event itself, however, may be of relatively minor medical significance (such as severe headache). Seriousness (not severity) which is based on patient/event outcome or action criteria serves as guide for defining regulatory reporting obligations. Pharmacovigilance Programme of India Page 61 Guidance Document For Reporting Individual Case Safety Report Side effect Any unintended effect of a pharmaceutical product occurring at normal dosage which is related to the pharmacological properties of the drug. Signal Reported information on a possible causal relationship between an adverse event and a drug, the relationship being unknown or incompletely documented previously. Usually more than a single report is required to generate a signal, depending upon the seriousness of the event and the quality of the information. The publication of a signal usually implies the need for some kind of review or action. Spontaneous reporting System whereby case reports of adverse drug events are voluntarily submitted from health professionals and pharmaceutical manufacturers to the national regulatory authority. SUSAR (Suspected Unexpected Serious Adverse Drug Reaction) A serious adverse drug reaction whose nature, severity or frequency is not identified previously in the risk information provided to the clinical investigator’s brochure (CIB) or on the drug label. Summary of Product Characteristics A regulatory document attached to the marketing authorization which forms the basis of the product information made available to prescribers and patients. Teratogen Environmental factors which can cause congenital abnormalities. Traditional Medicines Traditional medicine is the sum total of the knowledge, skills, and practices based on the theories, beliefs, and experiences indigenous to different cultures, whether explicable or not, used in the maintenance of health as well as in the prevention, diagnosis, improvement or treatment of physical and mental illness. Uncommon In pharmacovigilance an event with a frequency between 1 in 1.000 and 1 in 100. Pharmacovigilance Programme of India Page 62 Guidance Document For Reporting Individual Case Safety Report Unexpected adverse reaction An adverse reaction, the nature or severity of which is not consistent with domestic labeling or market authorization, or expected from characteristics of the drug. VigiBase The name of the WHO Global ICSR Database. WHO-ART Terminology for coding clinical information in relation to drug therapy. WHO-ART is maintained by UMC. WHO Drug Dictionary (WHO-DD) The WHO Drug Dictionary is an international classification of drugs providing proprietary and on-proprietary names of medicinal products used in different countries, together with all active ingredients. Pharmacovigilance Programme of India Page 63 Guidance Document For Reporting Individual Case Safety Report Annexure 3: Organisations, societies, regulators & useful websites 1. The Central Drugs Standard Control Organisation Headquarters CDSCO is the national regulatory body for Indian pharmaceuticals and medical devices, and serves parallel function to the European Medicines Agency of the European Union, the PMDA of Japan and the Food and Drug Administration of the United States. Within the CDSCO, the DCG (I) regulates pharmaceutical and medical devices. The DCGI is advised by the Drug Technical Advisory Board (DTAB) and the Drug Consultative Committee (DCC). It is divided into zonal offices which do pre-licensing and post-licensing inspections, postmarket surveillance, and recalls when needed. Official website: www.cdsco.nic.in 2. Indian Pharmacopoeia Commission IPC is an autonomous institution of the Ministry of Health and Family Welfare, Government of India. IPC is created to set standards of drugs in the country. Its basic function is to update regularly the standards of drugs commonly required for treatment of diseases prevailing in this region. It publishes official documents for improving quality of medicines by way of adding new and updating existing monographs in the form of IP. It further promotes rational use of generic medicines by publishing NFI. IPC also acts as a NCC for PvPI, thereby coordinating all the activities related to PV in India. Official website: www.ipc.gov.in 3. WHO Collaborating Centre for International Drug Monitoring: The Uppsala Monitoring Centre The WHO is a specialized agency of the UN that is concerned with international public health. The UMC is an independent foundation and a centre for international service and scientific research. The operational responsibility for the ADR monitoring programme rests with the WHO Collaborating Centre for International Drug Monitoring, UMC, in Sweden. The system started with 10 countries that had already established national systems for spontaneous adverse reaction reporting and who agreed to contribute data. For an effective international Pharmacovigilance Programme of India Page 64 Guidance Document For Reporting Individual Case Safety Report system to become operative, a common reporting form was developed, agreed guidelines for entering information formulated, common terminologies and classifications prepared and compatible systems for transmitting, storing and retrieving and disseminating data were created. The ADRs database in Uppsala currently contains over eight million reports of suspected ADRs. Official website: www.who-umc.org 4. WHO Country office for India Envisioning better health for all Indians, Mr Ghulam Nabi Azad, Hon’ble Minister for Health & Family Welfare, Government of India launched WHO’s new Country Cooperation Strategy (CCS), 2012-17with India along with Dr Nata Menabde, WHO representative to India on 29 June 2012. The WHO Country Office for India is headquartered in Delhi with country-wide presence. Its areas of work are enshrined in its new CCS, 2012-2017.The key aim of this pathbreaking strategy is to contribute to improving health and equity in India. It also provides the blueprint for unleashing India’s role on the global health arena alongside the continued pursuit of health improvement in the country. In this context, it distinguishes and addresses the challenges to India’s potential globally as well as impediments in solving long-standing health and health service delivery internally. The WHO Country Office for India also coordinates pharmacovigilance training programmes to the PV professionals, preparation and updating of PV toolkit and other regulatory documents for PvPI. Official website: www.whoindia.org 5. National Institute of Biologicals National Institute of Biologicals is an autonomous institution under the MoHFW, Government of India and is a premier scientific organization and a centre of excellence to ensure quality of biological and vaccines in the country. The institute responsibly assures and reviews the quality of number of biological products available through domestic manufacturers or imports. The operations are carried out in the state of the art facility of the institute and in close coordination with regulatory authorities. Official website: www.nib.gov.in Pharmacovigilance Programme of India Page 65 Guidance Document For Reporting Individual Case Safety Report 6. International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH) ICH is a project that brings together the regulatory authorities of Europe, Japan and the United States and experts from the pharmaceutical industry in the three regions to discuss scientific and technical aspects of pharmaceutical product registration. Official website: www.ich.org Pharmacovigilance Programme of India Page 66 Guidance Document For Reporting Individual Case Safety Report Annexure 4: Literature resources for pharmacovigilance Following literature resources can provides further information to NCC and AMCs under PvPI, regarding drug safety monitoring and other aspects of pharmacovigilance. Books 1. Alesso, L. (2007) Farmacovigilancia: HaciaUna Mayor Seguridad en el Uso de Medicamentos, Los talleresgráficos de Alejandro Graziani S.A. (2nd edition planned) 2. Aronson, JK. (ed.) (2006) Meyler's Side Effects of Drugs, 15th edition, Elsevier Science. 3. Aronson, JK. (ed.) (2010) Side Effects of Drugs Annual (36), Elsevier. 4. Baxter, K. (ed.) (2010) Stockley's Drug Interactions, 9th edition, Pharmaceutical Press. 5. Begaud, B. (2000) Dictionary of Pharmacoepidemiology, John Wiley & Sons Ltd. 6. Bennett, P., Calman, K., Curtis, S. and Fischbacher-Smith, D. (2010) Risk Communication and Public Health, 2nd edition, Oxford University Press, USA. 7. BMJ. (2007) Clinical Evidence Handbook: The International Source of the Best Available Evidence for Effective Healthcare, BMJ Publishing Group. 8. CIOMS. (1999) Benefit-Risk Balance for Marketed Drugs: Evaluating Safety Signals (Report of CIOMS Working Group IV), WHO. 9. CIOMS. (2010) Practical Aspects of Signal Detection in Pharmacovigilance (Report of CIOMS Working Group VIII), WHO. 10. Cobert, B. (2011) Cobert’s Manual of Drug Safety and Pharmacovigilance, 2nd edition, Jones & Bartlett Learning. 11. Cobert, B. and Biron, P. (2008) Practical Drug Safety from A to Z, Jones & Bartlett Publishers. 12. Cohen, MR. (2006) Medication Errors, 2nd edition, American Pharmacists Association. 13. Dukes, G., Mildred, M. and Swartz, B. (1998) Responsibility for Drug-Induced Injury: A Reference Book for Lawyers, the Health Professions and Manufacturers, IOS Press. 14. Gupta, SK. (ed.) (2011) Textbook of Pharmacovigilance, Jaypee Brothers Medical Publishers (P) Ltd. 15. Hugman, B. (2009) Healthcare Communication, Pharmaceutical Press. Pharmacovigilance Programme of India Page 67 Guidance Document For Reporting Individual Case Safety Report 16. Klepper, MJ. andCobert, B. (2010) Drug Safety Data: How to Analyze, Summarize, and Interpret to Determine Risk, Jones & Bartlett Learning. 17. Klincewicz, SL., Yap, YY., Thomas, A. with Taylor, JL. (ed.) (2009) Global Pharmacovigilance: Laws & Regulations, the Food and Drug Law Institute. 18. Mann, RD. and Andrews, EB. (ed.) (2007) Pharmacovigilance, 2nd edition, John Wiley & Sons Ltd. 19. MHRA. (2008) Good Pharmacovigilance Practice Guide, Pharmaceutical Press. 20. Slovic, P. (2000) The Perception of Risk, Earthscan Publications Ltd. 21. Strom, BL. (2005) Pharmacoepidemiology, 4th edition, John Wiley & Sons Ltd. 22. Sweetman, SC. (ed.)(2011) Martindale: The Complete Drug Reference, 37th edition, Pharmaceutical Press. 23. Talbot, J. and Waller, P. (ed.) (2003) Stephen’s Detection of New Adverse Drug Reactions, 5th edition, John Wiley & Sons Ltd. 24. Van Boxtel, CJ.,Santoso, B. and Edwards, IR. (ed.) (2008) Drug Benefits and Risks: International Textbook of Clinical Pharmacology, 2nd edition, IOS Press. 25. Vincent, C. (2010) Patient Safety, 2nd edition, Wiley-Blackwell. 26. Waller, P. (2009) An Introduction to Pharmacovigilance, Wiley-Blackwell. Journals 1. ADR Newsletters from National Centres 2. BMJ (British Medical Journal) 3. Drug Information Journal 4. Drug Safety 5. Indian Heart Journal 6. Indian Journal of Pathology & Microbiology 7. Indian Journal of Cancer 8. Indian Journal of Clinical Medicine 9. Indian Journal of Dentistry 10. Indian Journal of Dermatology 11. Indian Journal of Gastroenterology 12. Indian Journal of Health & Wellbeing 13. Indian Journal of Medicine 14. Indian Journal of Oncology & Radiation Biology Pharmacovigilance Programme of India Page 68 Guidance Document For Reporting Individual Case Safety Report 15. Indian Journal of Ophthalmology 16. Indian Journal of Pharmaceutical Sciences 17. Indian Journal of Pharmacology 18. Indian Journal of Pharmacy Practice 19. Indian Journal of Psychiatry 20. Indian Journal of Public Health 21. Indian Journal of Sexually Transmitted Diseases and AIDS 22. Indian Journal of Transfusion Medicine 23. JAMA (Journal of the American Medical Association) 24. Journal of Indian Medical Association 25. Pharmacoepidemiology & Drug Safety 26. Pharmacoepidemiology and Drug Safety 27. Prescrire 28. Reactions Weekly 29. The Indian Journal of Hospital Pharmacy 30. The Indian Journal of Medical Research 31. The Indian Journal of Paediatrics 32. The International Journal of Risk & Safety in Medicine 33. The Journal of Family Welfare 34. The Lancet 35. The New England Journal of Medicine 36. The Nursing Journal of India Publications 1. PvPI Newsletters 2. Safer Medicines, Safer Use of Medicines, Safer Patients (leaflet) 3. Aide Memoire - For a National Strategy for Safe Drugs and Their Appropriate Use 4. WHO Policy Perspectives on Medicines no. 9 - PV: Ensuring the Safe Use of Medicines 5. Viewpoint (part 1) 6. Viewpoint (part 2) 7. The Importance of Pharmacovigilance - Safety Monitoring of Medicinal Products Pharmacovigilance Programme of India Page 69 Guidance Document For Reporting Individual Case Safety Report 8. Safety Monitoring - Guidelines for Setting Up and Running a Pharmacovigilance Centre 9. Safety of Medicines - A Guide to Detecting and Reporting Adverse Drug Reactions 10. Being a Member of the WHO Programme 11. Uppsala Reports (Newsletter) 12. Vigiflow - when time is crucial (leaflet) 13. VigiSearch/VigiMine (leaflet) 14. CemFlow (leaflet) 15. SIGNAL 16. WHO Pharmaceuticals Newsletter 17. WHO Drug Information 18. WHO: Pharmaceuticals: Restrictions in Use and Availability 19. Effective Communications in Pharmacovigilance - The Erice Report 20. Dialogue in Pharmacovigilance - More Effective Communication 21. Expecting the Worst (2nd Edition 2010) 22. The Safety of Medicines in Public Health Programmes - Pharmacovigilance an Essential Tool 23. A Practical Handbook on the Pharmacovigilance of Antimalarial Medicines 24. A Practical Handbook on the Pharmacovigilance of Antiretroviral Medicines 25. WHO Guidelines on Safety Monitoring of Herbal Medicines 26. Accepted Scientific Names of Therapeutic Plants and their Synonyms 27. Herbal ATC Guide 28. Writings on Pharmacovigilance - Selected articles by David J Finney 29. A Lifetime in Safety - Selected articles by Ed Napke 30. Promoting Safety of Medicines for Children 31. The world medicines situation 2011 –Pharmacovigilance and safety of medicines Pharmacovigilance Programme of India Page 70