* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Symptomatic Relief Policy
Survey
Document related concepts
Transcript
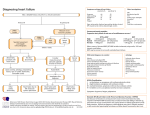
Symptomatic Relief Policy Compiled by: Drug Adminstration Steering Group Date: July 2004 Review Date: July 2006 Drug Administration Steering Group 1 Index Page Introduction 3 Clinical Conditions to which the policy applies. 3 Clinical Criteria for Inclusion 3 Criteria for Exclusion 4 Responsibilities 4 Professional Accountability 5 Prescribing the Symptomatic Relief Policy 5 Administration of Medicines via Symptomatic Relief Policy 5 Recording Keeping for the Symptomatic Relief Policy 6 Symptomatic Relief Products Analgesics Paracetamol Tablets 500mg 8 Paracetamol Suppositories 500mg 9 Antacids Gaviscon Advance 10 Gaviscon Liquid 11 Laxatives -Oral Senna Tablets /Senna Syrup 12 Throat Preparations Simple Linctus 13 Merocet / Strepsil Lozenges 14 Maintenance of Indwelling Urinary Catheter Sodium Chloride 0.9% Catheter Maintenance Solution 15 Anal irritation / Uncomplicated Haemorrhoids Anusol Cream 16 Anusol Suppositories 17 Appendix 1 - Nurse Competence Framework 18 Compiled by: Drug Administration Steering Group 2 Introduction: All medicines must be prescribed by an authorised prescriber before they are administered to a patient. For some patients, it is appropriate to prescribe a number of “as required” medicines, and when that is the case, the prescription of a “Symptomatic Relief Policy” as described below can be very useful. The Symptomatic Relief Policy facilitates the administration of a restricted range of medicines to patients, by registered nursing staff, from an agreed list of products in order to relieve specified symptoms. The policy stipulates the minimum interval and the maximum number of doses of each medicine that can be administered before medical review. Should the patient’s condition persist beyond that stated in the individual drug monograph then a member of medical staff must be notified and the patient examined. Should a patient need more frequent dosing of a particular medicine, this should then be individually prescribed. The policy does not replace the diagnosis and treatment of medical conditions by medical staff and is not intended to treat long-standing/chronic conditions. The medicines contained in this policy may be administered to patients by nursing staff, providing certain criteria are met. The Symptomatic Relief Policy does not contain complete prescribing information. Staff are referred to the BNF and summary of product characteristics for further information. Clinical Conditions to which the policy applies. • • • • • Pain Pyrexia Dyspepsia Constipation Cough • • • • Sore Throat Maintenance of indwelling urinary catheter Flushing an intravenous catheter Anal irritation/haemorrhoids Clinical Criteria for Inclusion Each individual patient must be assessed by a doctor and have the Symptomatic Relief Policy prescribed for them in their medicines prescription form before they can receive treatment under this policy. The doctor may exclude any of the products that in his/her judgement would not be appropriate for that patient. The patient is eligible if he/she is over twelve years of age, is not a pregnant or breastfeeding woman and has no contraindications or known sensitivities to any of the medicines on the Symptomatic Relief policy. Compiled by: Drug Administration Steering Group 3 Criteria for Exclusion The symptomatic relief policy does not apply to children of twelve years of age and under, or to pregnant or breastfeeding women. The patient can be excluded if he/she has any contraindication to any of the medicines listed in the Symptomatic Relief policy, or the policy can be used with those medicines excluded. The patient should be excluded if he/she is unable to communicate relevant symptoms listed above. If a patient is excluded from the Symptomatic Relief Policy, he/she must have all medication individually prescribed on their medicines prescription form. The patient may decline to be included on the Symptomatic Relief Policy. Those patients must not be prescribed the Symptomatic Relief Policy and must have all medication individually prescribed for them on their medicines prescription form. Responsibilities The doctor takes prime responsibility for ensuring that the policy is appropriate for the individual patient and for highlighting any medicine that is contra-indicated and which should not be given. The Nurse identifies the indication and caveats as per the policy; selects and administers the medicine; records and monitors the outcome as per guidelines in respect of Symptomatic Relief Policy. Any suspected adverse drug effects must be recorded in the nursing notes and doctor informed immediately. Only nursing/midwifery staff who have undergone additional training and whose competence has been agreed with their Ward or Department Sister/Charge Nurse, can administer medicines contained in this policy to patients in their care, according to the defined procedures contained within this policy. A competence assessment must be completed for each nurse before he/she can administer symptomatic relief. NHS Lanarkshire Operating Divisions are required to provide suitable training to ensure that all registered nurses have a full understanding of the contents of this list. Any specific areas of education will require to be addressed and ongoing competency evaluated on at least an annual basis. The nurse must have achieved the learning outcomes as detailed in implementation paper associated with the nursing symptomatic relief policy. Compiled by: Drug Administration Steering Group 4 The Sister/Charge Nurse is responsible for identifying appropriate staff for training and competency assessment. Qualified staff of Grade D or above are eligible for consideration. It is required that each ward have a current and maintained staff register which lists those staff who are competent to use the Policy. Only qualified nurses or midwives named in these registers may administer medicines utilising the Symptomatic Relief Policy. Professional Accountability: Each practitioner is accountable for maintenance and development of their professional knowledge and competence. Staff who make use of the Symptomatic Relief Policy must exercise independent judgment and assert their professional expertise. Prescribing the Symptomatic Relief Policy 1. Prescribing and administration must be in accordance with the operating division’s Medicines Code of Practice. 2. The individual patient is identified by the doctor as being a suitable candidate for the policy. 3. The doctor must prescribe the Symptomatic Relief Policy for the individual patient and exclude any of the products that in his/her judgement would not be appropriate and should not be given e.g. ‘Symptomatic Relief Policy Except Laxatives’. 4. Within The Acute Operating Division this should be prescribed in the patient’s Lanarkshire Medicine Prescription Form using the section on the back page of the form i.e. ‘Nurse/Midwife Administration by protocol – Authorised Nurse/Midwives Only’. Within some parts of the Primary Care Operating Division this should be done on the Aberdeen Kardex system. Administration of Medicines via Symptomatic Relief Policy The nurse may only administer in the ward/department where they normally work and only when deemed competent by the Ward Manager. The Ward Manager is required to assess their competency based on their knowledge of the policy content and awareness of the patient’s diagnosis. 1. The patient must be over twelve years of age and must not be pregnant or breastfeeding. Compiled by: Drug Administration Steering Group 5 2. A doctor must have prescribed the policy for that individual patient and detailed in writing any caveats as described above. 3. A registered nurse who has undergone additional training and whose competence has been agreed with their Ward or Department Sister/Charge Nurse may administer medicines from the policy. 4. The nurse must identify the patient by name and as per local procedure, and ensure that this matches the name and other details on the prescription form. 5. The nurse must identify the appropriate medicine for administration and ensure that a dose of the medicine has not already been administered by checking: a) That it has not been prescribed and administered ‘as required’ or regular medication. b) It has not been prescribed and administered in the ‘once only’ section c) That the medicine has not been excluded by the doctor who signed the prescription. d) The administration record to ensure that if this drug has already been administered to the patient via this policy that the maximum dose has not been exceeded. 6. The nurse identifies indication and caveats as per product monograph and administers and records as per guidelines in respect of Symptomatic Relief Policy. 7. The maximum number of doses stated in each drug monograph must not be exceeded. If symptoms persist beyond the recommended time parameters as stated in each protocol, an appropriate medical practitioner must be consulted. 8. Any nurse or midwife unsure of the appropriateness of administering from the Symptomatic Relief Policy should refrain from doing so and consult with a more experienced nursing, midwifery or medical colleague. Recording Keeping for the Symptomatic Relief Policy The nurse will record the administration of the medicine on the prescription form in the normal way i.e. back page of the medicines chart for the Lanarkshire Medicine Prescription form or Medicines Administration Record for the Aberdeen Kardex system which is in use in some parts of the Primary Care operating Division. Compiled by: Drug Administration Steering Group 6 Compiled by: Drug Administration Steering Group May 2004 Signature of Chairperson…………………………………………. ………………… Approved by: Lanarkshire Acute Operating Division Drug and Therapeutics Committee Signature of Chairperson……………………………………….Date………………… Approved by: Lanarkshire Primary Care Operating Division Drugs & Therapeutics Committee Signature of Chairperson: ___________________________ Date: _____________ Approved by: Lanarkshire Area Drug and Therapeutics Committee Signature of Chairperson…………………………………………..Date……………… Review Date………………………………………………………. Compiled by: Drug Administration Steering Group 7 Analgesics Paracetamol Tablets 500mg Description White Scored Tablet 500mg White Soluble Tablet 500mg Indication Mild to moderate pain Pyrexia (Give 2 tablets and advise medical staff) Method of Use / Adult Dose 1g (2 tablets) to be administered orally Frequency of Administration Every 4-6 hours Maximum number of doses that can be administered with authority of the “Symptomatic Relief Policy” prescription 2 doses in 24 hours Precautions/Contraindications • • • • • Known hypersensitivity to paracetamol Hepatic or renal impairment Soluble tablets should not be given to patients with heart failure Avoid use if patient is receiving any other paracetamol containing preparations e.g. coproxamol, co-codamol, benorylate etc. Current admission for paracetamol overdose Drug Interactions Warfarin: do not administer as may enhance anticoagulant effect. Side Effects Occur rarely - rashes, may cause agranulocytosis, thrombocytopenia and pancytopenia. Referral for Medical Advice • • • • • Further information Drug Administration Steering Group Refer if more than two doses are required in 24 hours. Refer if required on successive days In the event of side effects or if symptoms are not alleviated, refer to medical staff. Any suspected adverse drug effects should be recorded in the nursing notes and doctor informed. If symptoms recur within 7 days. Liver damage can occur following overdosage with paracetamol. Seek medical advice immediately if overdosage is suspected. 8 Analgesics Paracetamol Suppositories 500mg - only to be used when patient is unable to take oral preparation. Description Opaque white suppository with a wax-like consistency containing 500mg of paracetamol. Indication Mild to moderate pain. Method of Use / Adult Dose 1g ( 2 x 500mg suppositories) to be inserted into the rectum in accordance with the Nursing Procedure for the administration of Suppositories. Every 4-6 hours Frequency of Administration Maximum number of doses that can be administered with authority of “Symptomatic Relief Policy” prescription 2 doses in 24 hours Precautions/Contraindications • • • • • • • • Drug Interactions Side Effects Referral for Medical Advice Warfarin: do not administer as may enhance anticoagulant effect. Occur rarely - rashes, may cause agranulocytosis, thrombocytopenia and pancytopenia. • • • • • Further information Compiled by: Drug Administration Steering Group For rectal use only. Known hypersensitivity to paracetamol Hepatic or renal impairment. Avoid if patient is receiving any other paracetamol containing preparations. Current admission for paracetamol overdose. Do not administer if the patient has a known bowel obstruction or undiagnosed abdominal symptoms. Do not administer if recent anorectal surgery. Do not administer if rectum is impacted Refer if more than two doses are required in 24 hours. Refer if required on successive days In the event of side effects or if symptoms are not alleviated, refer to medical staff. Any suspected adverse drug effects should be recorded in the nursing notes and doctor informed. If symptoms repeat within 7 days. Liver damage can occur following overdosage with paracetamol. Seek medical advice immediately if overdosage is suspected. 9 Antacids Gaviscon Advance Liquid Description A pink oral suspension - peppermint flavour. Sugar free Indication Gastro-oesophageal reflux such as acid regurgitation, heartburn, indigestion occurring due to the reflux of stomach contents. Method of Use / Adult Dose 5ml – 10ml to be administered orally Frequency of Administration As required after meals and at bedtime. Maximum number of doses that can be administered with authority of “Symptomatic Relief Policy” prescription. Up to 3 doses in 24 hours Precautions/Contraindications Do not administer when a highly restricted salt diet is recommended, e.g. in some cases of congestive cardiac failure and renal impairment or when taking drugs which can increase plasma potassium levels. Each 10 ml dose contains 106mg (4.6 mmol) sodium and 78 mg (2.0 mmol) potassium. Each 10 ml contains 200 mg (2.0 mmol) of calcium carbonate. Care needs to be taken in treating patients with hypercalcaemia, nephrocalcinosis and recurrent calcium containing renal calculi. Contraindicated in patients with hypersensitivity to any ingredients of the product. Drug Interactions None known Side Effects Very rarely patients sensitive to the ingredients may develop allergic manifestations such as urticaria or bronchospasm. Referral for Medical Advice • • Drug Administration Steering Group If symptoms persist for more than 24hrs or increase in severity. If symptoms repeat within 7 days. 10 Antacids Gaviscon Liquid Description A pink oral suspension - aniseed flavour. Sugar free Indication Gastro-oesophageal reflux such as acid regurgitation, heartburn, indigestion occurring due to the reflux of stomach contents. Method of Use / Adult Dose 10ml – 20ml to be administered orally Frequency of Administration As required after meals and at bedtime. Maximum number of doses that can be administered with authority of “Symptomatic Relief Policy” prescription. Precautions/Contraindications Up to 3 doses in 24 hours. Do not administer when a highly restricted salt diet is recommended, e.g. in some cases of congestive cardiac failure and renal impairment or when taking drugs which can increase plasma potassium levels. Each 10 ml dose contains 141mg (6.2 mmol) sodium Contraindicated in patients with hypersensitivity to any ingredients of the product. Drug Interactions None known Side Effects Very rarely patients sensitive to the ingredients may develop allergic manifestations such as urticaria or bronchospasm. Referral for Medical Advice • • Compiled by: Drug Administration Steering Group If symptoms persist for more than 24hrs or increase in severity If symptoms repeat within 7 days. 11 Laxatives Senna Tablet/Senna Syrup Description Brown tablets containing standardised senna equivalent to 7.5 mg sennoside Fruit flavoured syrup containing standardised senna equivalent to 7.5mg sennoside per 5ml Indication Stimulant laxative for constipation Method of Use / Adult Dose Two tablets or 10ml of syrup to be administered orally Frequency of Administration Single dose at bedtime Maximum number of doses that can be administered with authority of “Symptomatic Relief Policy” prescription One dose Precautions/Contraindications Not to be given when any undiagnosed acute or persistent abdominal symptoms are present. Do not administer if the patient is known to have an intestinal obstruction. Do not administer if patient has a chronic gastrointestinal condition including e.g. peptic ulcer, Crohns disease, and ulcerative colitis. Do not administer if patient has had recent GI surgery Drug Interactions None known Side Effects May cause abdominal cramp Referral for Medical Advice Refer if there is no bowel movement within 24hrs Refer if required more than once every two weeks Further information Before administering: • Be aware of patient’s normal bowel function. • Be sure that the patient is constipated and that the constipation is not secondary to an underlying undiagnosed complaint. Document in nursing notes the rationale for administering the laxative. Drug Administration Steering Group 12 Throat Preparations Sugar Free Simple Linctus or Simple Linctus Description Flavoured liquid containing citric acid monohydrate 2.5%w/v Indication Soothing cough linctus. Method of Use / Adult Dose 5ml to be administered orally up to four times daily if required. Frequency of Administration 3 to 4 times daily Maximum number of doses that can be administered with authority of “Symptomatic Relief Policy” prescription. 4 doses in 24 hours Precautions/Contraindications Ensure that sugar free formulation is used if patient is a diabetic. Drug Interactions None known. Side Effects Referral for Medical Advice If symptoms persist for more than 48hrs. If symptoms repeat within 14 days. Drug Administration Steering Group 13 Throat Preparations Lozenges - e.g. Merocet or Strepsil Description Antiseptic throat lozenges Indication For the temporary relief of sore throats Method of Use / Adult Dose One lozenge to be given orally. Allow the lozenge to dissolve slowly in the mouth. Frequency of Administration One lozenge every 2-3 hours, maximum of 8 lozenges in 24 hours. Maximum number of doses that can be administered with authority of “Symptomatic Relief Policy” prescription. 8 lozenges. Precautions/Contraindications If symptoms are accompanied by fever, headache, nausea and vomiting. Caution if sensitivity to any of ingredients is suspected. Drug Interactions None Known Side effects May cause sore lips or tongue Allergic reaction to ingredients are rare but can occur. If symptoms persist for more than 24hrs. Referral for Medical Advice If symptoms repeat within 14 days. Compiled by: Drug Administration Steering Group 14 Maintenance of Indwelling Urinary Catheter Sodium Chloride 0.9% Catheter Maintenance Solution Description Sodium Chloride 0.9% catheter maintenance solution Indication To maintain patency/ flush urinary catheter. Method of Use / Adult Dose To be administered in accordance with the Lanarkshire Nursing Procedure for bladder irrigation. “Scope of Professional Practice: Bladder Maintenance Solution”. Precautions As per nursing procedure Maximum number of doses which can be administered with the authority of “Symptomatic Relief Policy” prescription. One only. Referral for Medical Advice. If there is the perceived need for a repeat flush at any time. Drug Administration Steering Group 15 Anal Irritation / Uncomplicated Haemorrhoids Anusol Cream Description Buff coloured cream. Each 100g contains: Bismuth Oxide 2.14g Balsam Peru 1.8g. Zinc Oxide 10.75 g Indication Symptomatic relief associated with minor anorectal conditions e.g. haemorrhoids, pruritus ani. Method of Use / Adult Dose For rectal use only. Thoroughly cleanse the affected area, dry gently and apply the cream. For internal conditions use the rectal nozzle provided. Clean the nozzle thoroughly after each use. Ensure the tube is clearly labelled with the patient’s name and date of opening. In cold temperatures it may be difficult to squeeze the ointment out of the tube. If this occurs warm the tube in the hand or dip it in warm water taking care not to overheat the cream. Frequency of Administration To be applied to the affected area at night, in the morning and after each evacuation until the condition is controlled Maximum number of doses that can be administered with authority of “Symptomatic Relief Policy” prescription. 4 doses in 24 hours. Precautions/Contraindications For external or rectal use only. Do not administer if the patient is allergic to any of the ingredients. Drug Interactions None known Referral for Medical Advice A transient burning sensation or irritation may occur on application. If this lasts longer than 30 minutes discontinue and seek medical advice. If symptoms persist for longer than 48hrs If symptoms recur within 14 days. Drug Administration Steering Group 16 Anal Irritation / Uncomplicated Haemorrhoids Anusol Suppositories Description White or off-white torpedo shaped suppository. Indication Symptomatic relief associated with minor rectal conditions including internal haemorrhoids. Method of Use / Adult Dose One suppository to be inserted into the anus in accordance with the Nursing Procedure for the administration of Suppositories. Frequency of Administration One suppository to be inserted at night, in the morning and after each evacuation if required. Maximum number of doses that can be administered with authority of “Symptomatic Relief Policy” prescription. Four in 24 hours. Precautions/Contraindications For rectal use only Do not administer if the patient has had recent anorectal surgery. Do not administer to patients with rectal bleeding. Do not administer if rectum is impacted with faeces. Drug Interactions None Known Referral for Medical Advice A transient burning sensation or irritation may occur on application. If this lasts longer than 30 minutes discontinue and seek medical advice. If symptoms persist for more than 48hrs. If symptoms recur within 14 days. Compiled by: Drug Administration Steering Group 17 Appendix 1. Nurse Competence Framework NHS Lanarkshire Symptomatic Relief Policies Before nursing staff can apply the Symptomatic Relief Policy, they must be assessed as having the competences listed below by the ward change nurse. The attached form should be used to record the assessment. Competencies Required. The nurse administering medicines using the authority of the Symptomatic Relief Policy must: • Understand that the Symptomatic Relief Policy must be prescribed by a doctor before a medicine from it can be administered. • Understand the limits of dosing frequency and duration permitted for each medicine within the symptomatic relief policy. • Understand that some patients may have certain medicines within the Symptomatic Relief Policy excluded. • Understand how medicines administered under the authority of a Symptomatic Relief Policy Prescription are to be recorded. Legal, accountability and professionally issues - The registered nurse/midwife must be able to demonstrated their knowledge of: • The rationale for using the Policy • The legal issues relating to admin istration of medicines using the Policy • The Registered nurse/midwife’s responsibility and accountability when assessing a patient for administration of drugs from the Policy • The importance of maintaining accurate records of training and achievement of co mpetence. Using the formulary safely and effectively - The registered nurse/midwife must be able to demonstrated their knowledge of: • The correct use of the Policy • An ability to interpret the signs and symptoms of patient conditions and select appropriate medication utilising the Policy. • Ability to correctly record the process • A knowledge of the action required if the patient’s symptoms persist beyond the recommended time parameters. Pharmacology - The registered nurse/midwife must be able to demonstra ted their knowledge of: • A knowledge of the doses, side effects, contraindications of the drugs within the Policy. Drug Administration Steering Group 18 Name of Nurse Grade Compiled by: Drug Administration Steering Group I confirm that I have understood the policy & procedure for the administration of Symptomatic Relief (Signature) Competence Assessment completed on (date) Approved by: Associate Director of Nursing/Manager or Named Professional (name) Signature of Associate Director of Nursing /Manager or Named Professional 19