* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Nephrology Case Presentation IgA Nephropathy
Survey
Document related concepts
Transcript
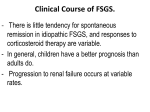
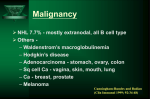
Nephrology Case Presentation Douglas Stahura D.O. Grandview Hospital November 20, 2001 Case Presentation 24 y/o AAF referred by PCP c/o fatigue, periorbital edema, lower extremity edema, hematuria, proteinuria Pt relates a 5 year history of intermittent gross hematuria usually associated with “colds” Over past four months has noticed increasing fatigue, swelling “around my eyes, especially in the morning” and swelling in the ankles and legs Case Presentation PMH – one pregnancy, uncomplicated PSH – none Allergy – none Meds – Lasix 40 mg QD Social – married, nursing student, nonsmoker, EtOH socially, caffeine-2 cpd Family – Father deceased age 50 MVA, Mother DM2 age 56 Case Presentation ROS – Fatigue, Weight gain 10#, No energy, poor – – – – appetite, Swelling in feet/ankles, worse at end of the day, legs “feel heavy” Denies CP/PALP/DOE, Cough/Sputum/SOB Denies N/V/D, +/-Constipation No recent UTI, hematuria Case Presentation Exam: BP 135/85, T-98.6, P-80, R-14 Wt-146, Ht-5’3” NAD, pleasant, cooperative CV,RESP,GI,MS, LYMPH – WNL SKIN – warm/dry, 3+ pitting up to knees B/L, no rash/purpura, Case Presentation Lab data: – Na-133, K-4.1, Cl-103, HCO3-25 – BUN-8, Cr-0.8 – CBC normal – AST-18, ALT-22, ALP-80, ALB-0.6 – UA SG-1.020, pH-5, BLO-2+, PRO-4+, GLU-neg, Ketones-Neg – CXR-normal Differential Diagnosis Hematuria, gross Proteinuria Hypoalbuminuria Nephrotic Syndrome Nephritic Syndrome Clinical Investigation Imaging: Renal Ultrasound Lab: – – – – – ANA, dsDNA ASO titer, ANCA, anti-GBM Ab Serum/Urine Electropheresis HBV, HCV, HIV, C3, C4, CH50 24 hour Urine: Protein, Creatinine Renal Biopsy Clinical Investigation 24 hour urine – 18 grams protein/24 hours – Creatinine Clearance 120 ml/min 00:00 IgA Nephropathy Mesangial proliferative glomerulonephritis characterized by diffuse mesangial deposition of IgA Described by Berger in Paris 1968 Common clinical presentation is gross hematuria provoked by mucosal infection Diagnosis is made by Immunoflorescence IgA Nephropathy Pathogenesis IgA preferentially deposits in glomerulus Abnormality of host IgA immune system – No consistent evidence for a specific antigen Bacterial, viral, food – Possibly autoimmune against mesangium – Antigen-independent mechanism – IgA glycosylation IgA Nephropathy Pathogenesis IgA most abundant Ig in the body and provides mucosal defence Two subclasses: IgA1, IgA2 Mucosal Ag challenge provokes pIgA by plasma cells in MALT Bone marrow derived mIgA1 IgA Nephropathy Pathogenesis In IgA nephropathy – pIgA1 is deposited in mesangium – pIgA1 is downregulated in mucosa and upregulated in the marrow – Tonsillar pIgA1 is increased Mesangial proliferation is a result of cytokines and growth factors (PDGF, TGF-beta) IgA Nephropathy Clinical Presentation Macroscopic Hematuria in 2nd & 3rd decades of life (40-50%) “Synpharingitic” hematuria Microscopic hematuria +- proteinuria Nephrotic Syndrome w/ hematuria(5%) Acute Renal Failure (rare) – Cresentic or tubular occlusion by hematuria Chronic Renal Failure w/HTN IgA Nephropathy Clinical Associations IgA Nephropathy Prognosis Clinical – POOR Increasing Age Duration of symptoms Severity of proteinuria Hypertension Renal impairment – NO IMPACT Gender Serum IgA level Histopathologic – POOR Glomerular sclerosis Tubule atrophy Interstitial fibrosis Vascular wall thickening Capillary loop wall IgA deposits IgA Nephropathy Therapy Reduce IgA production Tonsillectomy Gluten free diet – neither reduce incidence of renal failure Altering Immune and Inflammation In cresentic IgAN – plasmapheresis, steroids, and cyclophosphamide – poor long term results Steroids – alternate day regimen x 2 years Cyclophosphamide only – no good data IgA Nephropathy Therapy Altering Immune and Inflammation Dipyridimole and warfarin – no benefit Cyclosporine – hemodynamic effect only Slowly Progressive Hypertension – Use of ACE-Inhibitor to target 125/75 will reduce proteinuria Fish Oil – 4-8 grams/day provided renal protection from progressive disease, but did not lower proteinuria My Patient Daily Prednisone, then to alternate day therapy – Failed, no decrement of renal function, but no improvement of proteinuria Fish Oil – unable to comply and quit therapy after 3-4 months Cytoxan/Methyprednisolone monthly IV pulses x 6 (Lupus Nephritis regimen) Albumin =4.1 clinical Nephrotic syndrome resolved References Comprehensive Clinical Nephrology, RJ Johnson/J Feehally, Harcourt, 2000 The Kidney, Brenner and Rector, 6th Ed, Saunders, 2000 The long term Outcome of Patients with IgA Nephropathy Treated with Fish Oil in a Controlled Trial, Donadio et al., JASN:10;1772-1777, 1999