* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Library CD Request Processor
Women's health in India wikipedia , lookup
Prenatal development wikipedia , lookup
HIV and pregnancy wikipedia , lookup
Prenatal testing wikipedia , lookup
Maternal health wikipedia , lookup
Prenatal nutrition wikipedia , lookup
Women's medicine in antiquity wikipedia , lookup
Fetal origins hypothesis wikipedia , lookup
Maternal physiological changes in pregnancy wikipedia , lookup
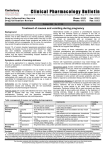
Sacred Heart Medical Center -- Professional Library Services Telephone: (541) 686 - 6837 Requester: Telephone: Deliver By: Address: Search Number: Reference Librarian: FAX: (541) 686 - 7391 Treena Bell 335-2671 In-House E-Mail: LIBRARY Patron Type: SHMC(Dept) Fax: email results 264-08 Bonne Starks 5/9/2017 Topic: Hyperemesis in pregnancy This database search covers literature from 1966 to the present. Unless otherwise noted below, MEDLINE was searched using the OVID CD-ROM system located in the library. This system is also available to staff via modem. MEDLINE is produced by the NATIONAL LIBRARY OF MEDICINE. NOTIFICATION OF COPYRIGHT: Databases, software, journal articles and the other library materials are protected by the Copyright Law (Title 17, U.S. Code). Under certain conditions (referred to as fair use), individuals are authorized to make reproductions. Some of these conditions are: (1) that the copied material is not “used for any purpose other than private study, scholarship, or research” (i.e. for educational use, not for personal profit), (2) that only a small portion of the work is copied, and (3) only a single copy is made. This institution pays royalties on all copying that exceeds these guidelines. The library assumes that users have read and understand the notification and will refuse requests that involve violation of the Copyright Law. Notes: Results include: last 5 years, reviews or what is on site. 1: Am J Obstet Gynecol. 2008 Jan;198(1):71.e1-7. Validity of a modified Pregnancy-Unique Quantification of Emesis and Nausea (PUQE) scoring index to assess severity of nausea and vomiting of pregnancy. Lacasse A, Rey E, Ferreira E, Morin C, Bérard A. Faculty of Pharmacy, University of Montreal, Montreal, QC, Canada. OBJECTIVE: The only validated nausea and vomiting of pregnancy (NVP) severity index is the Motherisk Pregnancy-Unique Quantification of Emesis and Nausea (PUQE) index that covers symptoms in the previous 12 hours. We sought to assess the validity of a modified-PUQE index that covers the entire first trimester of pregnancy by comparing NVP severity scores between the 12-hour PUQE index and our modified-PUQE index and by measuring the extent of the association between the modified-PUQE score and quality-of-life (QOL) score during the first trimester of pregnancy. STUDY DESIGN: A prospective study that included women who attended the Centre Hospitalier Universitaire Sainte-Justine or René-Laennec clinic for their prenatal visits was conducted from 2004-2006. Women were eligible if they were > or = 18 years old and < or = 16 weeks of gestation at the time of their first prenatal visit. Women who reported NVP were asked to fill out the 12-hour PUQE, the modified PUQE index, and the Short-Form Health Survey QOL index simultaneously. Intraclass correlation coefficients were calculated to determine concordance between the 2 scores. Linear regression models were built to measure the association between the modified-PUQE score and Short-Form Health Survey QOL scores. RESULTS: Among participants (n = 287), the mean NVP severity score was 5.7 vs 6.7 on the 12-hour PUQE and modified PUQE, respectively (P < .05). There was substantial concordance between the indices (intraclass correlation coefficient, 0.71). Severity of NVP that was measured by the new modified index was associated with QOL. CONCLUSION: We are confident that, on the basis of the modified-PUQE, the relationship between QOL and severity of NVP justify the use of this new index. Publication Types: Research Support, Non-U.S. Gov't Validation Studies 5/9/2017 Page 1 of 9 Sacred Heart Medical Center -- Professional Library Services Telephone: (541) 686 - 6837 FAX: (541) 686 - 7391 In-House E-Mail: LIBRARY PMID: 18166311 [PubMed - indexed for MEDLINE] 2: Am J Obstet Gynecol. 2008 Jan;198(1):56.e1-4. Hyperemesis in pregnancy: an evaluation of treatment strategies with maternal and neonatal outcomes. Holmgren C, Aagaard-Tillery KM, Silver RM, Porter TF, Varner M. Department of Obstetrics and Gynecology, University of Utah Health Sciences Center, Salt Lake City, UT, USA. [email protected] OBJECTIVE: The objective of the study was to evaluate the use of interventions such as a peripherally inserted central catheters (PICC) line or nasogastric (NG)/nasoduodenal (ND) tube with the use of medications alone in the management of pregnancies with hyperemesis. STUDY DESIGN: Subjects were identified with confirmed intrauterine pregnancy, admitted with hyperemesis gravidarum (HEG) between 1998 and 2004. Medical records were then abstracted for information with regard to therapy. Subjects were assigned on the basis of the management plan: medication alone, PICC line, or NG/ND tube. Outcomes were compared between groups. RESULTS: Ninety-four patients met study criteria and had complete outcome data available. Of those, 33 had a PICC line placed (35.1%), 19 had a NG/ND placed (20.2%), and 42 were managed with medication alone (44.7%). These groups were similar with respect to gestational age at delivery, Apgar score, and mean birthweight. Maternal complications were significantly higher among those with PICC lines. Of patients managed with PICC lines, 66.4% (P < .001) required treatment for infection, thromboembolism, or both. Adjusted odds ratio for a PICC line complication was 34.5 (5.09, 233.73). CONCLUSION: Maternal complications associated with PICC line placement are substantial despite no difference in neonatal outcomes, suggesting that the use of PICC lines for treatment of HEG patients should not be routinely used. PMID: 18166306 [PubMed - indexed for MEDLINE] 3: Dig Dis Sci. 2007 Oct;52(10):2840-3. Epub 2007 Apr 12. Helicobacter pylori stool antigen assay in hyperemesis gravidarum: a risk factor for hyperemesis gravidarum or not? Aytac S, Türkay C, Kanbay M. Department of Gastroenterology, Güven Hospital, Ankara, Turkey. Objective: To test the hypothesis that Helicobacter pylori (H. pylori) infection may cause hyperemesis gravidarum (HG). Materials and methods: A prospective-comparative study was performed on 107 pregnant patients from October 2002 to December 2003 in a university-based prenatal care clinic. Blood and stool samples were obtained from 52 patients diagnosed as HG and 55 matched asymptomatic pregnant women. H. pylori stool antigen (HpSA) status of the participants was evaluated using a commercially available enzyme immunoassay-based kit. Results: The overall prevalence of HpSA positivity appeared as 41.1%. Twenty-two of 52 (42.3%) HG patients and 22 of 55 (40.0%) control subjects were positive for HpSA. The difference was not significant (p>.05). Conclusion: HG seemed to be not associated with H. pylori infection, as indicated by specific stool antigen assay. PMID: 17431779 [PubMed - indexed for MEDLINE] 4: Aust Fam Physician. 2007 Sep;36(9):698-701. Hyperemesis gravidarum--assessment and management. Sheehan P. Maternity Care Program, Royal Women's Hospital, Melbourne, Victoria, Australia. [email protected] BACKGROUND: Nausea and vomiting are common symptoms in early pregnancy. In most 5/9/2017 Page 2 of 9 Sacred Heart Medical Center -- Professional Library Services Telephone: (541) 686 - 6837 FAX: (541) 686 - 7391 In-House E-Mail: LIBRARY women the condition is mild and self limiting. A small percentage of women experience severe nausea and vomiting. This is known as hyperemesis gravidarum. Outcomes have improved with intravenous rehydration therapy. Consequences include decreased quality of life, time off work and secondary depression. OBJECTIVE: This article outlines the aetiology, outcomes, history and examination of women with hyperemesis gravidarum. Treatment modalities are discussed together with evidence regarding use. DISCUSSION: It is important to exclude other causes of nausea and vomiting such as urinary tract infection and thyrotoxicosis. Assessment of severity by checking for ketones is important as severity determines management. Management will include rehydration (intravenous or oral). Evidence is lacking regarding dietary and lifestyle recommendations but some women find them useful. Pyridoxine and metoclopramide (category A) are first line in treatment of hyperemesis gravidarum followed by prochlorperazine (category C), prednisolone (category A), promethazine (category C) and ondansetron (category B1). Benefit has been reported with the use of ginger. Evidence is mixed regarding acupressure and acupuncture. Publication Types: Review PMID: 17885701 [PubMed - indexed for MEDLINE] 5: Obstet Gynecol. 2007 Sep;110(3):695-703. Hyperemesis gravidarum and Helicobacter pylori infection: a systematic review. Golberg D, Szilagyi A, Graves L. Department of Family Medicine, SMBD Jewish General Hospital, McGill University, Montreal, Canada. [email protected] OBJECTIVE: To systematically review studies examining the relationship between hyperemesis gravidarum and Helicobacter pylori (H pylori) infection. DATA SOURCES: A 1966 to January 2007 search using MEDLINE/PubMed, EMBASE, and Web of Science included MeSH terms: "Helicobacter pylori," "Helicobacter infections," "hyperemesis gravidarum," and the text words "nausea," "vomit," "pregnancy," and "Helicobacter." References of selected papers were examined for additional relevant studies. METHODS OF STUDY SELECTION: We evaluated studies investigating a relationship between hyperemesis gravidarum and H pylori infection. Studies were included in which the diagnosis of hyperemesis gravidarum was made at or before entry into the study, and H pylori diagnosis was made by serum antibody sample, gastric biopsy, saliva test, or stool sample. The search produced 169 titles; 22 were reviewed in further detail. TABULATION, INTEGRATION, AND RESULTS: Fourteen case-control studies met established criteria, involving 1,732 participants and controls tested for H pylori infection. Studies were evaluated according to patient demographics and study methodology (case definition, exclusion criteria, H pylori testing). An estimate of the odds ratios with 95% confidence intervals was calculated by using a random effects model for dichotomous variables with review article software. Ten studies showed a significant association between hyperemesis gravidarum and H pylori infection. Odds ratios varied from 0.55 to 109.33; three results were less than 1.0. Tests for heterogeneity applied to several subgroups were considerable with values above 75% for all groups. CONCLUSION: An association between hyperemesis gravidarum and H pylori infection is suggested by this systematic review. However, the considerable heterogeneity among studies highlights study limitations. Publication Types: Review PMID: 17766620 [PubMed - indexed for MEDLINE] 5/9/2017 Page 3 of 9 Sacred Heart Medical Center -- Professional Library Services Telephone: (541) 686 - 6837 FAX: (541) 686 - 7391 In-House E-Mail: LIBRARY 6: Crit Care Med. 2006 Nov;34(11):2781-3. Pulsed steroid therapy is an effective treatment for intractable hyperemesis gravidarum. Bondok RS, El Sharnouby NM, Eid HE, Abd Elmaksoud AM. Department of Anaesthesiology and Intensive Care, Ain-Shams University Hospitals, Cairo, Egypt. OBJECTIVE: Intractable hyperemesis gravidarum remains a serious cause of morbidity among pregnant women. If not controlled, hyperemesis gravidarum can lead to severe disability, electrolyte and acid base imbalance, and even various organ system dysfunctions. From the successful use of steroids for chemotherapy-induced emesis, corticosteroids might prove useful in hyperemesis gravidarum. The purpose of this study was to compare the efficacy of pulsed hydrocortisone therapy with that of metoclopramide for the management of intractable hyperemesis gravidarum. DESIGN: Prospective, double-blind study. SETTING: Intensive care unit of Ain Shams University Maternity Hospital. PATIENTS: Forty patients aged 19-34 yrs having a normal appearing intrauterine pregnancy, of < or =16 wks gestation, admitted to the intensive care unit with intractable hyperemesis meeting the study criteria. INTERVENTIONS: Patients were randomly assigned to receive either intravenous hydrocortisone 300 mg as a daily dose or intravenous metoclopramide 10 mg 3 times daily. After 3 days the hydrocortisone was tapered completely during the course of 1 wk, whereas the metoclopramide was continued without change for 1 wk. Patients were followed up daily during the therapy course and for 2 wks following intensive care unit discharge. MEASUREMENTS AND MAIN RESULTS: There was a significant reduction in vomiting episodes in the hydrocortisone group compared with the metoclopramide group (p < .0001). Within-patient analyses showed a significant reduction in mean vomiting episodes in the hydrocortisone group within the first 3 days (p < .0001). No patients from the hydrocortisone group but six of the patients receiving metoclopramide were readmitted for intractable vomiting within 1 wk from discharge. Five of them showed improvement on intravenous hydrocortisone therapy. CONCLUSIONS: A short course of hydrocortisone is an effective treatment for intractable hyperemesis gravidarum. Publication Types: Comparative Study Randomized Controlled Trial PMID: 16957638 [PubMed - indexed for MEDLINE] 7: Scand J Caring Sci. 2006 Jun;20(2):169-76. Tactile massage and severe nausea and vomiting during pregnancy--women's experiences. Agren A, Berg M. Department of Obstetrics and Gynaecology, Hospital of Skövde, Sweden. [email protected] Nausea and vomiting during pregnancy is a condition with an obscure aetiology. The treatment is symptomatic but there is a lack of alternative treatments. Tactile massage is known to give relaxation and increased well-being in connection with different illnesses, but has never been studied on women with severe nausea and vomiting during pregnancy (SNVP). The aim of this study was to describe hospitalized women's experiences of SNVP and of tactile massage. A phenomenological method was used. Ten hospitalized women with SNVP were included. Each woman was given tactile massage on three separate occasions. After the final massage an open interview was used covering both the experience of severe nausea and vomiting, and of tactile massage. The findings revealed an essential meaning summarizing the experience: to obtain a relieving moment of rest and access to the whole body when nausea rules life. When nausea is experienced as controlling a woman's life, tactile massage is experienced as promoting relaxation and gives 5/9/2017 Page 4 of 9 Sacred Heart Medical Center -- Professional Library Services Telephone: (541) 686 - 6837 FAX: (541) 686 - 7391 In-House E-Mail: LIBRARY her an opportunity to regain access to her body. The findings suggest that tactile massage is a good alternative and complement to traditional treatment of SNVP. Publication Types: Research Support, Non-U.S. Gov't PMID: 16756522 [PubMed - indexed for MEDLINE] 8: Obstet Gynecol Surv. 2006 Apr;61(4):255-68. Hyperemesis gravidarum complicated by Wernicke encephalopathy: background, case report, and review of the literature. Chiossi G, Neri I, Cavazzuti M, Basso G, Facchinetti F. Obstetrics and Gynecology Residency Program, Modena Policlinico Hospital, University of Modena and Reggio Emilia, Modena, Italy. Wernicke encephalopathy (WE) is a rare but known complication of severe hyperemesis gravidarum caused by thiamine deficiency. This article presents an unusual case that occurred at our institution and reviews the 48 previously published cases of WE in pregnancy. Considering all the 49 cases, the mean (+/-standard deviation) patients' age was 26.7 +/- 4.9 years, the mean gestational age when WE manifested was 14.3 +/- 3.4 weeks, and the mean duration of vomiting and feeding difficulties was 7.7 +/- 2.8 weeks. Wernicke's classic triad (confusion, ocular abnormalities, and ataxia) manifested in only 46.9% (23 of 49) of the patients. Confusion affected 63.3% (31 of 49) of the patients, ocular signs 95.9% (47 of 49) and symptoms 57.1% (28 of 49), and ataxia 81.6% (40 of 49). Deterioration of consciousness affected 53.1% (26 of 49) of the subjects and memory impairment 61.2% (30 of 49). Complete remission of the disease occurred in only 14 of 49 cases. Symptom resolution required months and permanent impairments were common. The overall pregnancy loss rate, directly (spontaneous fetal loss) and indirectly (planned abortion) attributable to WE, was 47.9% (23 of 49). The diagnosis of WE is clinical and can be rapidly confirmed by magnetic resonance imaging. We emphasize the importance of thiamine supplementation to women with prolonged vomiting in pregnancy, especially before intravenous or parenteral nutrition. We also underline the necessity to promptly replace vitamin B1 when neurologic symptoms and/or signs develop in a patient with hyperemesis gravidarum. Publication Types: Case Reports Review PMID: 16551377 [PubMed - indexed for MEDLINE] 9: Am J Obstet Gynecol. 2006 Mar;194(3):815-20. Acupressure for the in-patient treatment of nausea and vomiting in early pregnancy: a randomized control trial. Heazell A, Thorneycroft J, Walton V, Etherington I. Maternal and Fetal Health Research Centre, St. Mary's Hospital, Manchester, UK. [email protected] OBJECTIVE: The purpose of this study was to evaluate the efficacy of acupressure at the P6 point for the in-patient treatment of severe nausea and vomiting in early pregnancy. STUDY DESIGN: This was a prospective single-blind randomized control trial that involved 80 patients with nausea and vomiting plus ketonuria before 14 weeks of gestation. RESULTS: There was no difference between length of stay, amount of medication, or fluid required between the acupressure and placebo groups, although acupressure reduced the number of patients who stayed > or =4 nights in the hospital. Acupressure was well tolerated and not associated with an increase in perinatal morbidity or death. CONCLUSION: The use of acupressure at the P6 point does not reduce the amount of antiemetic medication that is required, the requirement for intravenous fluid, and median duration of in-patient stay more than the use of placebo. A small reduction was seen in the 5/9/2017 Page 5 of 9 Sacred Heart Medical Center -- Professional Library Services Telephone: (541) 686 - 6837 FAX: (541) 686 - 7391 In-House E-Mail: LIBRARY number of women who required > or =4 days in the hospital. Publication Types: Randomized Controlled Trial PMID: 16522418 [PubMed - indexed for MEDLINE] 10: J Infus Nurs. 2006 Mar-Apr;29(2):89-100. Hyperemesis gravidarum and the role of the infusion nurse. Lamondy AM. Intravenous Therapy Department, Day Kimball Hospital, Putnam, CT, USA. [email protected] Hyperemesis gravidarum is a potentially serious complication of pregnancy that can result in severe maternal malnutrition, affects the normal growth and development of the fetus, can precipitate preterm birth, and in extreme cases, causes fetal death. The article uses a case study to review the disease process and outline the benefits of a team approach to the care of the pregnant woman and her unborn child. Treatment interventions, from dietary modifications to total parenteral nutrition, are reviewed, with a focus on the effects that normal pregnancy physiology has on infusion device selection and the total parenteral nutrition formula prescribed. Publication Types: Case Reports Review PMID: 16569998 [PubMed - indexed for MEDLINE] 11: Obstet Gynecol. 2006 Feb;107(2 Pt 2):486-90. Wernicke's encephalopathy with hyperemesis and ketoacidosis. Selitsky T, Chandra P, Schiavello HJ. Department of Obstetrics and Gynecology, Wyckoff Heights Medical Center, Brooklyn, New York 11237, USA. BACKGROUND: Avitaminosis can result from the acute malnutrition associated with prolonged pregnancy-related hyperemesis. Serious complications may arise from thiamine deficiency under these circumstances. CASE: We review the relevant literature and describe a case with central nervous system involvement presenting with typical manifestations of Wernicke's encephalopathy, apparently precipitated by a combination of hyperemesis gravidarum, diabetic ketoacidosis, and intravenous glucose administration. CONCLUSION: While this life-threatening complication is rare, it is important for all who care for obstetric patients to be aware of it and alert to its development. Early recognition is critical given the need to treat affected women expeditiously to help avoid potentially fatal adverse consequences. Prophylactic thiamine supplementation should be considered in the care of gravidas with hyperemesis. Publication Types: Case Reports Review PMID: 16449159 [PubMed - indexed for MEDLINE] 12: Obstet Gynecol. 2006 Feb;107(2 Pt 1):285-92. Outcomes of pregnancies complicated by hyperemesis gravidarum. Dodds L, Fell DB, Joseph KS, Allen VM, Butler B. Perinatal Epidemiology Research Unit, Department of Obstetrics and Gynaecology, Dalhousie University, Halifax, Nova Scotia, Canada. [email protected] OBJECTIVE: To evaluate maternal and neonatal outcomes among women with hyperemesis during pregnancy. METHODS: A population-based retrospective cohort study was conducted among women with singleton deliveries between 1988 and 2002. Hyperemetic pregnancies were defined as those requiring one or more antepartum admissions for hyperemesis before 24 weeks of gestation. Severity of hyperemesis was evaluated according to the number of antenatal hospital admissions (1 or 2 versus 3 or more) and according to weight gain during pregnancy (< 7 kg [15.4 lb] versus > or = 7 kg). Maternal outcomes evaluated included weight gain during 5/9/2017 Page 6 of 9 Sacred Heart Medical Center -- Professional Library Services Telephone: (541) 686 - 6837 FAX: (541) 686 - 7391 In-House E-Mail: LIBRARY pregnancy, gestational diabetes, gestational hypertension, labor induction, and cesarean delivery. Neonatal outcomes included 5-minute Apgar score of less than 7, low birth weight, small for gestational age, preterm delivery, and perinatal death. Logistic regression was used to generate adjusted odds ratios for all outcomes, and the odds ratios were converted to relative risks. RESULTS: Of the 156,091 singleton pregnancies, 1,270 had an admission for hyperemesis. Compared to women without hyperemesis, infants born to women with hyperemesis and with low pregnancy weight gain (< 7 kg [15.4 lb]) were more likely to be low birth weight, small for gestational age (SGA), born before 37 weeks of gestation, and have a 5-minute Apgar score of less than 7. Compared with infants born to women without hyperemesis, rates of low birth weight and preterm delivery were substantially higher among infants born to women with hyperemesis and low pregnancy weight gain (4.2% versus 12.5% and 4.9% versus 13.9%, respectively). The outcomes among infants born to women with hyperemesis with pregnancy weight gain of 7 kg (15.4 lb) or more were not different from the outcomes among women without hyperemesis. CONCLUSION: The results of this study suggest that the adverse infant outcomes associated with hyperemesis are a consequence of, and mostly limited to, women with poor maternal weight gain. LEVEL OF EVIDENCE: II-2. PMID: 16449113 [PubMed - indexed for MEDLINE] 13: Obstet Gynecol. 2006 Feb;107(2 Pt 1):277-84. Risk factors for hyperemesis gravidarum requiring hospital admission during pregnancy. Fell DB, Dodds L, Joseph KS, Allen VM, Butler B. Perinatal Epidemiology Research Unit, Department of Obstetrics and Gynaecology, Dalhousie University, Halifax, Nova Scotia, Canada. OBJECTIVE: To identify risk factors for hyperemesis requiring hospital admission during pregnancy. METHODS: Data from a population-based cohort of all deliveries in Nova Scotia, Canada between 1988 and 2002 were obtained from the Nova Scotia Atlee Perinatal Database. Women with 1 or more antepartum admissions for hyperemesis were compared with women with no admissions for hyperemesis. Relative risks (RRs) and 95% confidence intervals (CIs) were estimated using logistic regression and used to determine a set of independent risk factors for hyperemesis. RESULTS: The overall rate of admission for hyperemesis was 0.8% (n = 1,301) among 157,922 deliveries. In the adjusted analysis, hyperthyroid disorders (RR 4.5, 95% CI 1.8-11.1), psychiatric illness (RR 4.1, 95% CI 3.0-5.7), previous molar pregnancy (RR 3.3, 95% CI 1.6-6.8), preexisting diabetes (RR 2.6, 95% CI 1.5-4.7), gastrointestinal disorders (RR 2.5, 95% CI 1.8-3.6), and asthma (RR 1.5, 95% CI 1.2-1.9) were all statistically significant risk factors for hyperemesis, whereas maternal smoking and maternal age older than 30 were associated with decreased risk. Compared with singleton male pregnancies, singleton female pregnancies, pregnancies with multiple male fetuses, and male and female combinations were associated with statistically significant increased risk of hyperemesis. CONCLUSION: Although hospitalization for hyperemesis occurs in less than 1% of pregnant women, this translates to a large number of hospital admissions. The factors associated with hyperemesis are primarily medical and fetal factors that are not easily modifiable, but identification of these factors may be useful in determining those women at high risk for developing hyperemesis. LEVEL OF EVIDENCE: II-2. PMID: 16449112 [PubMed - indexed for MEDLINE] 5/9/2017 Page 7 of 9 Sacred Heart Medical Center -- Professional Library Services Telephone: (541) 686 - 6837 FAX: (541) 686 - 7391 In-House E-Mail: LIBRARY 14: Ann Pharmacother. 2005 Oct;39(10):1710-3. Epub 2005 Aug 30. Treating pregnancy-related nausea and vomiting with ginger. Boone SA, Shields KM. Raabe College of Pharmacy, Ohio Northern University, Ada, OH 45810-1078, USA. OBJECTIVE: To review literature assessing the safety and efficacy of the use of ginger to treat nausea and vomiting in pregnancy. DATA SOURCES: Iowa Drug Information Service (1966-September 2004), International Pharmaceutical AB: s (1971-September 2004), MEDLINE (1966-September 2004), and EMBASE (1966-September 2004) were searched. Key terms included ginger, nausea, vomiting, emesis, and pregnancy. DATA SYNTHESIS: Studies evaluating the safety and efficacy of ginger in the management of nausea and vomiting in pregnancy were reviewed. Various doses and forms of ginger were used to treat women during their first and second trimesters of pregnancy. Ginger has been shown to improve the symptoms of nausea and vomiting compared with placebo in pregnant women. CONCLUSIONS: While data are insufficient to recommend ginger universally and there are concerns with product quality due to limited regulation of dietary supplements, ginger appears to be a fairly low-risk and effective treatment for nausea and vomiting associated with pregnancy. In low doses, this may be appropriate for patients not responding to traditional first-line therapies. Publication Types: Review PMID: 16131535 [PubMed - indexed for MEDLINE] 15: Hum Reprod Update. 2005 Sep-Oct;11(5):527-39. Epub 2005 Jul 8. Erratum in: Hum Reprod Update. 2007 Mar-Apr;13(2):207. Hyperemesis gravidarum, a literature review. Verberg MF, Gillott DJ, Al-Fardan N, Grudzinskas JG. Academic Unit of Reproductive Physiology, Obstetrics and Gynaecology, St. Bartholomew's Hospital, West Smithfield, London, UK. Hyperemesis gravidarum (HG) is a condition causing severe nausea and vomiting in early pregnancy often resulting in hospital admission. The incidence of HG is approximately 0.5% of live births, said to be higher in multiple pregnancies, hydatidiform mole and other conditions associated with increased pregnancy hormone levels. Both the aetiology and pathogenesis of HG remain unknown. We conducted a literature review (1966-now) to summarize the current evidence on the aetiology and pathogenesis of HG. The potential role of pregnancy-related hormones such as progesterone, estrogen and HCG has been widely studied; however, various other hormones such as leptin, placental growth hormone, prolactin, thyroid and adrenal cortical hormones have been implicated in the aetiology of HG. In addition to endocrinological hypotheses, the rationale and evidence considering infectious, immunological, psychological, metabolic and anatomical causes for HG have been analysed here. Many studies suffer from the low number of patients included, the variable definition used for HG and varying assay methodology used in studies of hormone measurement. This review highlights the need for more extensive studies addressing the pathogenesis and aetiology of HG. Publication Types: Review PMID: 16006438 [PubMed - indexed for MEDLINE] 16: Obstet Gynecol. 2005 Apr;105(4):849-56. Comment in: Obstet Gynecol. 2005 Sep;106(3):640; author reply 640-1. Effectiveness and safety of ginger in the treatment of pregnancy-induced nausea and vomiting. Borrelli F, Capasso R, Aviello G, Pittler MH, Izzo AA. Department of Experimental Pharmacology, University of Naples Federico II, Naples, Italy. [email protected] 5/9/2017 Page 8 of 9 Sacred Heart Medical Center -- Professional Library Services Telephone: (541) 686 - 6837 FAX: (541) 686 - 7391 In-House E-Mail: LIBRARY OBJECTIVE: Conventional antiemetics are burdened with the potential of teratogenic effects during the critical embryogenic period of pregnancy. Thus, a safe and effective medication would be a welcome addition to the therapeutic repertoire. This systematic review was aimed at assessing the evidence for or against the efficacy and safety of ginger (Zingiber officinale) therapy for nausea and vomiting during pregnancy. DATA SOURCES: Systematic literature searches were conducted in 3 computerized databases (MEDLINE, EMBASE, and Cochrane Library), and the reference lists of all papers located were checked for further relevant publications. METHODS OF STUDY SELECTION: For the evaluation of efficacy, only double-blind, randomized controlled trials (RCTs) were included. All retrieved clinical data, including uncontrolled trials, case reports, observational studies, and RCTs, were included in the review of safety. TABULATION, INTEGRATION, AND RESULTS: Six double-blind RCTs with a total of 675 participants and a prospective observational cohort study (n = 187) met all inclusion criteria. The methodological quality of 4 of 5 RCTs was high. Four of the 6 RCTs (n = 246) showed superiority of ginger over placebo; the other 2 RCTs (n = 429) indicated that ginger was as effective as the reference drug (vitamin B6) in relieving the severity of nausea and vomiting episodes. The observational study retrieved and RCTs (including follow-up periods) showed the absence of significant side effects or adverse effects on pregnancy outcomes. There were no spontaneous or case reports of adverse events during ginger treatment in pregnancy. CONCLUSION: Ginger may be an effective treatment for nausea and vomiting in pregnancy. However, more observational studies, with a larger sample size, are needed to confirm the encouraging preliminary data on ginger safety. LEVEL OF EVIDENCE: I. Publication Types: Review PMID: 15802416 [PubMed - indexed for MEDLINE] 5/9/2017 Page 9 of 9