* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Clinical finding: Infection with HIV-1 is associated with a progressive
Cryptosporidiosis wikipedia , lookup
Henipavirus wikipedia , lookup
Trichinosis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Leptospirosis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Sarcocystis wikipedia , lookup
Marburg virus disease wikipedia , lookup
West Nile fever wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Hepatitis C wikipedia , lookup
Schistosomiasis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Neonatal infection wikipedia , lookup
Oesophagostomum wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Antiviral drug wikipedia , lookup
Epidemiology of HIV/AIDS wikipedia , lookup
Hepatitis B wikipedia , lookup
Microbicides for sexually transmitted diseases wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
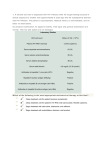
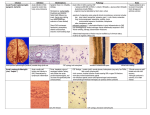
Clinical finding: Infection with HIV-1 is associated with a progressive decrease of the CD4+ T cell count and an increase in viral load (the level of HIV in the blood). The stage of infection can be determined by measuring the patient's CD4+ T cell count and viral load. The clinical picture of HIV infection can be divided into three stages: an acute stage, latent stage, and immunodeficiency stage. Infection with HIV generally occurs by introduction of bodily fluids from an infected person into the body of an uninfected person. A period of rapid viral replication ensues, leading to an abundance of virus in the peripheral blood. During primary infection, the level of HIV may reach several million virus particles per milliliter of blood. This response is accompanied by a marked drop in the numbers of circulating CD4+ T cells. This acute viremia is associated in virtually all patients with the activation of CD8+ T cells, which kill HIV-infected cells, and subsequently with antibody production, or seroconversion. The CD8+ T cell response is thought to be important in controlling virus levels, which peak and then decline, as the CD4+ T cell counts rebound. A good CD8+ T cell response has been linked to slower disease progression and a better prognosis, though it doesn't eliminate the virus. During this period most individuals (80 to 90%) develop an influenza or mononucleosis-like illness called acute HIV infection, the most common symptoms of which may include fever, lymphadenopathy, pharyngitis, rash, myalgia, malaise, mouth and esophageal sores, and may also include, but less commonly, headache, nausea and vomiting, enlarged liver/spleen, weight loss, thrush, and neurological symptoms (figure 3). Infected individuals may experience all, some, or none of these 1 symptoms. The duration of symptoms varies, averaging. This acute stage resolves spontaneously in about 2 weeks. Antibodies to HIV typically appears 3-4 weeks after infection. Because of the nonspecific nature of these symptoms, they are often not recognized as signs of HIV infection. Even if patients go to their doctors or a hospital, they will often be misdiagnosed as having one of the more common infectious diseases with the same symptoms. As a consequence, these primary symptoms are not used to diagnose HIV infection, as they do not develop in all cases and because many are caused by other more common diseases. However, recognizing the syndrome can be important because the patient is much more infectious during this period. Figure(3): the main symptoms of HIV acute infection. In the second stage, a long latent period, measured in years ensues. The patient is asymptomatic, and a large amount of virus is produced by 2 lymph node cells but remains sequestered within the lymph nodes (which typically become persistently swollen, in response to large amounts of virus that become trapped in the follicular dendritic cells (FDC) network). Individuals who are in this phase are still infectious. A syndrome called AIDS-related complex (ARC) can occur during the latent period. The most frequent manifestations are persistent fever, fatigue, weight loss, ad lymphadenopathy. ARC often progress to AIDS. The late stage of HIV infection is AIDS, manifested by a decline in the number of CD4 cells to below 400/mm3 and increase in the frequency and severity of opportunistic infections. Syndrome associated with this period include the following features: 1) Constitutional disease: fever, diarrhea, weight loss, skin rashes. 2) Neurological disease: dementia, peripheral neuropathy. 3) Immunodeficiency: Increased susceptibility to opportunistic infections. 4) Rare malignancies: Kaposi sarcoma, lymphomas. Diagnosis: The diagnosis of HIV infection is made by the detection of antibodies by ELISA. Because there are some false-positive results with this test, the definite diagnosis is made by Western blot analysis. The PCR is very sensitive technique that detect HIV DNA within infected cells. During the first months after infection, antibody tests are frequently negative. In view of this, the diagnosis of acute HIV infection typically cannot be made using serological tests. The presence of HIV can be detected during that period by either viral culture, p24 antigen test, or PCR assay. 3 Treatment: The treatment of choice for advanced disease is a regimen consisting of two nucleoside inhibitors ( Azidothymidine and Lamivudine) and a protease inhibitors ( Indinavir). This combination is known as HAART (highly active antiretroviral therapy). It is effective in prolonging life, improving quality of life, and reducing viral load but doesn't cure the chronic HIV infection. Another regimen especially in children, is the combination of azidothymidine, lamivudine, and non-nucleoside reverse transcritase inhibitor, efavirinez. Azidothymidine (AZT) inhibits HIV replication by interfering with proviral DNA synthesis. Strains of HIV resistant to AZT have been isolated from patient receiving long-term AZT therapy. Dideoxyinosine (ddI) is recommended for patient who are intolerant of AZT or whose disease has progressed while they were taking AZT. Prevention: The risk of contracting HIV increases with the number of sexual partners. A change in the lifestyle would obviously reduce the risk. The spread of HIV through blood transfusion and blood products had virtually been eliminated since the introduction of blood donor screening in many countries. AZT had been shown to be effective in preventing transmission of HIV from the mother to the fetus. The incidence of HIV infection in the baby was reduced by two-thirds. 4