* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Ocular toxicity after intracameral injection of very high
Survey
Document related concepts
Fundus photography wikipedia , lookup
Blast-related ocular trauma wikipedia , lookup
Macular degeneration wikipedia , lookup
Visual impairment due to intracranial pressure wikipedia , lookup
Retinal waves wikipedia , lookup
Retinitis pigmentosa wikipedia , lookup
Transcript
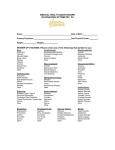
ARTICLE Ocular toxicity after intracameral injection of very high doses of cefuroxime during cataract surgery Marie-No€elle Delyfer, MD, PhD, Marie-Benedicte Rougier, MD, PhD, Sandy Leoni, MD, Qiuhua Zhang, MD, Francis Dalbon, MD, Joseph Colin, MD, Jean-François Korobelnik, MD PURPOSE: To report cases of intraocular inflammation after intracameral injection of a very high dose of cefuroxime at the end of uneventful cataract surgery. SETTING: Department of Ophthalmology, Bordeaux University Hospital, Bordeaux, France. DESIGN: Case series. METHODS: Patients were followed on an outpatient basis and were examined postoperatively at 1 and 5 days and 6 weeks. Central macular thickness, angiography, central corneal thickness (CCT), endothelial cell density (ECD), and electroretinography (ERG) were analyzed to evaluate ocular toxicity. RESULTS: One day postoperatively, the mean corrected distance visual acuity (CDVA) was 0.95 logMAR G 0.40 (SD). All the cases had moderate anterior inflammation. Retinal optical coherence tomography scans systematically showed extensive macular edema (mean 843.2 G 212.7 mm) associated with a large serous retinal detachment. Fluorescein angiograms showed diffuse leakage without abnormal retinal perfusion. At 5 days, the mean CDVA improved significantly to 0.52 G 0.29 logMAR (P<.005), as did the macular edema and serous retinal detachment (mean 339.4 G 138.3 mm) (PZ.005). At 6 weeks, the mean CDVA reached 0.09 G 0.06 logMAR. Modifications in CCT and ECD were similar to those observed after uneventful phacoemulsification. The macular thickness (mean 288.4 G 22.6 mm) and profile returned to normal in all patients, although ERG recordings showed reduced rod photoreceptor cell function (P<.05). CONCLUSIONS: Intracameral injection of high doses of cefuroxime induced anterior and posterior inflammation. Without surgical intervention, the final visual outcome was satisfactory in all cases. Long-term retinal function, however, must be assessed through repeated ERG recordings. Financial Disclosure: No author has a financial or proprietary interest in any material or method mentioned. J Cataract Refract Surg 2011; 37:271–278 Q 2011 ASCRS and ESCRS Cataract extraction is the most commonly performed surgical procedure in elderly people in industrialized countries.1 With the rise of life expectancy, cataract surgical needs will keep increasing, as will the healthy aging population’s expectations of significant improvements in postoperative visual acuity. Bacterial endophthalmitis, although rare, is among the most feared and devastating postoperative complications because it can lead to severe and permanent visual loss.2 Prevention of postoperative endophthalmitis thus represents one of the main challenges facing cataract surgeons. In addition to recommendations to use povidone–iodine preoperatively,3,4 avoid silicone intraocular lenses (IOLs),5 and carefully consider the incision type and location,5–7 the administration of Q 2011 ASCRS and ESCRS Published by Elsevier Inc. prophylactic antibiotic agents has kept the rate of postoperative endophthalmitis at its lowest level.7,8 Of the different antibiotic strategies, the intracameral injection of cefuroxime (0.1 mL of 10.0 mg/mL solution) has been shown to induce a 5-fold reduction in the incidence of postoperative endophthalmitis, a result that is significantly better than with perioperative instillation of topical levofloxacin eyedrops.1,5,9 Cefuroxime is a second-generation bactericidal cephalosporin with an antibacterial spectrum well suited to bacteria implicated in postoperative endophthalmitis.8 Unlike vancomycin, it is not a last-resort antibiotic agent that must be reserved for treatment and not prophylaxis, as recommended by the U.S. Centers for Disease Control and Prevention, Atlanta, Georgia.8,10 Because cefuroxime 0886-3350/$ - see front matter doi:10.1016/j.jcrs.2010.08.047 271 272 OCULAR TOXICITY OF CEFUROXIME is a time-dependent kill agent, it has been debated whether the choice of a concentration-dependent kill antibiotic, such as moxifloxacin, would be more appropriate.11 However, to this day, intracameral cefuroxime remains the most cost-effective way to prevent postoperative endophthalmitis.12 At the recommended dose of 1.0 mg in 0.1 mL, cefuroxime presents no ocular toxicity and is well tolerated.13–16 Intracameral injection of cefuroxime has therefore been proposed as “a standard part of the procedure of modern phacoemulsification cataract surgery.”9 However, no ready-to-use ocular formulations of cefuroxime are available. The 10.0 mg/mL solution is prepared in hospital pharmacies and stored at 4 C for a limited time or reconstituted by the surgeon in the operating room, which risks mistakes during the 2 steps of dilution. Minor dilution errors have occurred in the past without incidence.17 Here, however, we report 6 cases of intraocular inflammation after intracameral injection of a very high dose of cefuroxime secondary to misunderstanding of the dilution protocol at the end of uneventful cataract surgery. PATIENTS AND METHODS This series comprises cases of phacoemulsification cataract surgery performed on January 20, 2010. No perioperative complications were recorded. All patients received a singlepiece AcrySof Natural SN60AT yellow-tinted IOL (Alcon Laboratories, Inc.). It was the first time the eye surgeon used cefuroxime. The surgeon reconstituted the cefuroxime in the operation ward by adding 7.5 mL of a balanced salt solution to a 750.0 mg vial of lyophilized antibiotic powder. The 100.0 mg/mL solution was not rediluted, and a volume containing between 0.4 mL and 0.5 mL was intracamerally injected at the end of the surgical procedure, resulting in an injection of 40.0 to 50.0 mg of cefuroxime instead of the recommended dose of 1.0 mg. The mistake was based on the surgeon’s misunderstanding of the dilution protocol resulting from inattentive study of the literature. The day after surgery, all patients had poor vision and ocular inflammation. They were referred to our department. Patients were examined postoperatively at 1 and 5 days and 6 weeks. No surgical procedure (anterior chamber washout or vitrectomy) was performed. At each clinical evaluation, corrected distance visual acuity (CDVA), slitlamp Submitted: July 11, 2010. Final revision submitted: August 25, 2010. Accepted: August 26, 2010. From the Department of Ophthalmology, Bordeaux University Hospital, Bordeaux, France. Corresponding author: Marie-No€elle Delyfer, MD, PhD, Department of Ophthalmology, Bordeaux University Hospital, Place Amelie Raba-Leon, 33076 Bordeaux Cedex, France. E-mail: marie-noelle. [email protected]. biomicroscopic examination, intraocular pressure (IOP) measurement, and indirect ophthalmoscopy were performed. Fundus autofluorescence imaging, central macular thickness (CMT), and a retinal optical coherence tomography (OCT) profile were assessed by spectral-domain scanning laser ophthalmoscopy OCT (Spectralis Heidelberg Retinal Angiograph/OCT, Heidelberg Engineering GmbH). The OCT mapping software automatically calculated the CMT. Fluorescein angiography was performed 1 day postoperatively. Indocyanine green (ICG) angiography was performed in the initial case with a digital retinal camera (Topcon TRC50IX, Topcon Corp.). Corneal endothelial cell counts (ECCs), expressed as cells/mm2, were taken at 1 day and 6 weeks with a noncontact specular microscope (Noncon Robo, Konan Medical). Anterior segment OCTs (Visante OCT, Carl Zeiss Meditec AG) were performed at 1 day and 6 weeks. The International Society for Clinical Electrophysiology of Vision (ISCEV) standard full-field electroretinograms (ERGs) were recorded 6 weeks postoperatively according to standard protocols (Metrovision).18 Statistical analyses were performed using the Student t test. A P value less than 0.05 was considered statistically significant. RESULTS This case series comprised 6 patients. The mean age of the 4 women and 2 men was 76 years (range 69 to 84 years). Visual Acuity and Symptoms Table 1 shows the details of each case. The mean CDVA was 0.33 logMAR G 0.15 (SD) preoperatively and 0.95 G 0.40 logMAR 1 day postoperatively. By 5 days postoperatively, the mean CDVA had improved to 0.52 G 0.29 logMAR (P!.005). At 6 weeks, the CDVA reached 0.09 G 0.06. Patient 5 was the only one to report persistent halo. The improvement in CDVA from preoperatively to postoperatively was statistically significant (P!.05). Anterior Segment Inflammation and Corneal Changes One day postoperatively, all the patients had moderate anterior inflammation with fibrin formation (Table 1 and Figure 1), 2 patients (5 and 6) had corneal edema, and 2 others (1 and 2) had elevated IOP. All patients were prescribed topical tobramycin 0.3%, dexamethasone 0.1%, and ketorolac tromethamine 0.5% eyedrops. Patients with elevated IOP were also given oral acetazolamide and topical apraclonidine 0.5%. At 5 days, no anterior inflammation or residual high IOP was observed. Ocular hypertension treatment was discontinued in the 2 patients with transient high IOP. The mean central corneal thickness (CCT) was 559.83 G 50.55 mm 1 day postoperatively and 530.33 G 45.60 mm at 6 weeks. The CCT at 1 day was 5.6% J CATARACT REFRACT SURG - VOL 37, FEBRUARY 2011 273 OCULAR TOXICITY OF CEFUROXIME Table 1. Individual patient data over time. Preoperative Age (y) Sex Involved eye CDVA (logMAR) Postoperative 1 day CDVA (logMAR) AC cells AC flare Vitreous haze IOP (mm Hg) CCT (mm) ECC (/mm2) CMT (mm) 5 days CDVA (logMAR) CMT (mm) 6 weeks CDVA (logMAR) CCT (mm) ECC (/mm2) CMT (mm) Contralateral CMT (mm) ERG scotopic b-wave amplitude (mV) Pt 1 Pt 2 Pt 3 Pt 4 Pt 5 Pt 6 74 M R 0.40 82 M R 0.20 70 F L 0.10 77 F R 0.40 84 F R 0.40 69 F R 0.50 0.70 1C 1C 1C 34 503 2198 885 1.60 2C 2C 1C 48 556 2695 996 1.00 1C 0 !1C 20 594 2375 995 1.00 2C 2C !1C 12 580 1980 1008 1.00 1C 1C !1C 12 626 Edema 688 0.40 1C 2C 1C 18 500 Edema 487 0.40 304 1.00 585 0.50 277 0.50 270 MD MD 0.20 261 0.10 470 2008 323 306 104.0 0.10 509 2114 285 308 96.0 0.05 580 2299 296 298 69.4 0.05 574 1550 272 281 56.9 0.20 555 1302 293 286 101.0 0.05 494 1751 266 192 NI AC Z anterior chamber; CCT Z central corneal thickness; CDVA Z corrected distance visual acuity; CMT Z central macular thickness; ECC Z endothelial cell count; ERG Z electroretinography; IOP Z intraocular pressure; MD Z missing data; NI Z not interpretable; Pt Z patient greater than at 6 weeks; the difference in the 2 values was statistically significant (P!.05). Endothelial cell counts could be measured in 4 of 6 patients 1 day postoperatively; the 2 patients in whom the count could not be measured (5 and 6) had corneal edema (Table 1). In the remaining patients, the mean endothelial cell loss between 1 day and 6 weeks postoperatively was 319.25 cells/mm2. This corresponded to a 16% decrease from the initial ECC, although the difference was not statistically Figure 1. Slitlamp images of patient 4 (A) and patient 6 (B) 1 day postoperatively. Patient 4 presented with postoperative inflammatory anterior chamber fibrin formation. Patient 6 also had corneal edema. J CATARACT REFRACT SURG - VOL 37, FEBRUARY 2011 274 OCULAR TOXICITY OF CEFUROXIME significant. The 2 patients in whom an ECC could not be taken were known to have cornea guttata. At 6 weeks, the cornea guttata in patient 5 was more severe in the operated right eye than in the contralateral left eye. No preoperative data were available. The EEC at 6 weeks was 1302 cells/mm2 and 1902 cells/mm2, respectively. Patient 6 had only 1 functional eye because the contralateral eye had several previous surgeries for retinal detachment, preventing comparison between the 2 eyes once the corneal edema resolved. Retinal Findings No patient had previous retinal disease in the operated eye. One day postoperatively, a dilated fundus examination showed slight vitreous haze and significant retinal thickening in all patients. Retinal OCT scans systematically showed extensive macular edema; the mean CMT was 843.2 G 212.7 mm. Macular edema predominated in the outer nuclear layer and was associated with a large serous retinal detachment (Figure 2). Fundus autofluorescence images did not yield additional differences from the contralateral eye. Patient 3 refused to have angiography after reading the consent form. Fluorescein angiograms in the other 5 cases showed diffuse leakage without abnormal retinal perfusion (Figure 3). Indocyanine green angiography was performed only in patient 1, the first to be examined; the angiograph showed no abnormalities (Figure 3). By 5 days postoperatively, the macular edema and serous retinal detachment had improved significantly (PZ.005; data missing for patient 5); the mean CMT was 339.4 G 138.3 mm. By 6 weeks, the profile had returned to normal in all patients; the mean CMT was 288.4 G 22.6 mm. The CMT in the operated eye and the CMT in the contralateral eye (mean 277 G 48.7 mm) were not statistically different (PZ.47). Electroretinographic Analysis Electroretinographic analysis was performed in all cases except patient 6, whose ERGs were not interpretable because of numerous losses of fixation and artifacts. The ISCEV-standard full-field ERGs showed a mean decrease in scotopic b-wave amplitude of 31.6% over the normal values provided by the manufacturer (85.5 G 21 mV, PZ.01), whereas photopic b-wave amplitude remained normal, indicating alteration of the rod photoreceptors. No other abnormalities were seen. DISCUSSION The postoperative inflammation of the anterior chamber that we observed in all 6 patients shared some characteristics with toxic anterior segment syndrome (TASS) 19 as follows: it began within 24 hours after surgery, it was associated with fibrin formation, there was corneal edema, and it improved with topical steroid treatment. However, unlike what usually happens in TASS,19 inflammation was not restricted to the anterior segment, which therefore argues in favor of a diagnosis of mild toxic endophthalmitis. Only patients with elevated IOP reported ocular pain. Transient ocular hypertension in patients 1 and 2 may have been caused by unsolved particles of cefuroxime after reconstitution or inflammatory precipitates on the trabecular meshwork. In TASS, corneal edema is often linked to widespread endothelial cell damages; corneal alterations in our cases were rather limited. There were slight modifications in the ECC between 1 day and 6 weeks postoperatively; the modifications were approximately the same as those observed 6 weeks after standard cataract surgery,20,21 at least in patients 1 to 4. Our findings were not consistent with in vitro observations by Yoeruek et al.,16 who found an increase in endothelial cell loss with cefuroxime concentrations higher than 2.75 mg/mL. Rapid clearance of cefuroxime in the anterior chamber in vivo may explain the discrepancies. In our last 2 patients, preexisting cornea guttata impaired initial measurements and may have represented a susceptibility factor for increased endothelial damages in the presence of high concentrations of cefuroxime, as proposed by € Ozlem et al.22 However, this could not be established. All our patients had an increase in CCT. The 5.6% increase 1 day postoperatively was similar to findings reported in the literature after uneventful phacoemulsification20,23 and therefore was probably not linked to potential cefuroxime toxicity. Retinal vulnerability to cefuroxime has been analyzed at usual doses, and no alteration was observed.13,15 Tolerance has been found to be good after a 1.0 mg and a 3.0 mg intracameral injection of cefuroxime.15,17 Anatomically, the extended macular edema and serous retinal detachment we observed in all 6 patients show that cefuroxime diffusion in the posterior segment was significant. Macular edema predominated in the outer nuclear layer, implying a particular drug susceptibility of the photoreceptors or the retinal pigment epithelium (RPE), as observed in animal models after intravitreal administration of high doses of antibiotic agents (vancomycin24 or aminoglycosides25). Fluorescein angiography showed diffuse leakage from retinal vessels, probably as a result of disruption of the blood–retinal barrier. Because the significant inflammation of the external retina could have been secondary to abnormal choroidal perfusion, we performed an ICG angiogram on our first patient; the angiogram showed no abnormalities. Postoperative fundus autofluorescence images at 1 day, 5 days, J CATARACT REFRACT SURG - VOL 37, FEBRUARY 2011 OCULAR TOXICITY OF CEFUROXIME 275 Figure 2. Postoperative horizontal OCT scans over time. At 1 day, macular edema predominating in the outer nuclear layer was found in all patients and was associated with an extended serous retinal detachment (asterisks). The OCT-based CMT is given for each patient and visit. At 5 days, the macular edema and serous retinal detachment had resolved in patients 1, 3, and 6. In patient 4, a cyst persisted in the retrofoveal area. In patient 2, although decreasing, macular edema and serous retinal detachment (asterisk) were still present. Patient 5 could not been seen at 5 days because of a pneumopathy. By 6 weeks, the macular OCT profile had returned to normal in all the patients. J CATARACT REFRACT SURG - VOL 37, FEBRUARY 2011 276 OCULAR TOXICITY OF CEFUROXIME Figure 3. Fundus image (A) and angiographic findings (B to H) in patient 1. A: Blurred aspect of the fundus was observed due to anterior segment inflammation and to slight vitreous haze. A thickening of the retina predominating at the posterior pole was noticed. The caliber of the retinal blood vessels and the optic nerve was normal. B to E: Fluorescein angiogram images with retinal arterial phase (B), venous laminar phase (C), intermediate phase (D, 4 mn), and late phase (E, 12 mn). Fluorescein angiography showed diffuse leakage without abnormal retinal perfusion. F to H: The ICG angiogram with early (F, 1 mn), intermediate (G, 10 mn), and late (H, 30 mn) phases did not show choroidal perfusion abnormalities. J CATARACT REFRACT SURG - VOL 37, FEBRUARY 2011 OCULAR TOXICITY OF CEFUROXIME and 6 weeks did not show RPE alterations; that is, there were no areas of pigment clumping or atrophy. Functionally, initial retinal dysfunction was assessed by the drop in visual acuity 1 day postoperatively. However, the decrease was transient, as evidenced by the improvement in CDVA at 5 days, which was consistent and significant compared with the CDVA at 1 day (P!.005). Furthermore, at 6 weeks, the improvement in CDVA was significant compared with the preoperative values (P!.05). Still, ERG analyses at 6 weeks showed moderate alterations in rod photoreceptor cell function, confirming a particular drug susceptibility of the outer retina, as observed anatomically on OCT scans and discussed above. With the growing use of intracameral antibiotic administration during cataract surgery, unintended dilution errors have occurred.17,26 However, whenever the errors occur or are discovered, the physician in charge must decide promptly whether additional treatment is required for the benefit of the patient. Should the physician opt in favor of anterior chamber washout? Should one consider vitrectomy to limit retinal damage? Such questions have to be addressed. In this case after reviewing the pharmacokinetic data available and the clinical characteristics of our patients, we decided not to perform surgery. There was no indication for anterior chamber irrigation because intracameral cefuroxime concentration in the aqueous humor has been shown to decrease by 4fold within 60 minutes after injection14; our patients were 24 hours out from surgery and their anterior symptoms were rather moderate. We also carefully weighed the benefits of vitrectomy to decrease the cefuroxime concentration in the vitreous and thus reduce potential retinal toxicity. However, retinal toxicity after intravitreal injection of a high dose of antibiotics in animal models has been shown to be more often related to a peak concentration of the antibiotic agent than to the duration of tissue exposure.24,25 Therefore, we deemed the risks associated with vitrectomy in an inflamed eye too high considering the rapid ocular clearance of the drug and the absence of retinal toxicity observed with cefuroxime in animal experiments.13 Fortunately, the final visual outcome was relatively satisfactory in all 6 patients, arguing against surgical intervention in such cases. Long-term retinal function, however, will have to be assessed through repeated ERG recordings. With the increased use of intracameral cefuroxime at the end of cataract surgery, there is clearly a need for a self-preserved ophthalmic formulation to avoid the important risk of dilution error during extemporaneous compounding. Still, the short-term stability of cefuroxime after reconstitution27 remains a limiting factor that must be overcome. 277 In the meantime, it is the surgeon’s duty to avoid dilution errors when using off-label drugs by performing a careful and comprehensive study of the recommended protocols before using the drugs. In the case of extemporaneous preparation in a hospital pharmacy, multidisciplinary cooperation is essential to preclude similar errors and control of the medication’s labels in advance by the surgeon remains mandatory. REFERENCES 1. Seal DV, Barry P, Gettinby G, Lees F, Peterson M, Revie CW, Wilhelmus KRfor the ESCRS Endophthalmitis Study Group. ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery; case for a European multicenter study. J Cataract Refract Surg 2006; 32:396–406 2. Endophthalmitis Vitrectomy Study Group. Results of the Endophthalmitis Vitrectomy Study; a randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol 1995; 113:1479–1496. Available at: http://archopht.ama-assn.org/cgi/ reprint/113/12/1479. Accessed October 22, 2010 3. Speaker MG, Menikoff JA. Prophylaxis of endophthalmitis with topical povidone–iodine. Ophthalmology 1991; 98:1769–1775 4. Ciulla TA, Starr MB, Masket S. Bacterial endophthalmitis prophylaxis for cataract surgery; an evidence-based update. Ophthalmology 2002; 109:13–24 5. ESCRS Endophthalmitis Study Group. Prophylaxis of postoperative endophthalmitis following cataract surgery: results of the ESCRS multicenter study and identification of risk factors. J Cataract Refract Surg 2007; 33:978–988 €m M, Wejde G, Stenevi U, Thorburn W, Montan P. 6. Lundstro Endophthalmitis after cataract surgery; a nationwide prospective study evaluating incidence in relation to incision type and location. Ophthalmology 2007; 114:866–870 7. Schein OD. Prevention of endophthalmitis after cataract surgery: making the most of the evidence [editorial]. Ophthalmology 2007; 114:831–832; erratum, 1088 8. Montan PG, Wejde G, Koranyi G, Rylander M. Prophylactic intracameral cefuroxime; efficacy in preventing endophthalmitis after cataract surgery. J Cataract Refract Surg 2002; 28:977–981 9. Barry P, Seal DV, Gettinby G, Lees F, Peterson M, Revie CW, for the ESCRS Endophthalmitis Study Group. ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery; preliminary report of principal results from a European multicenter study. J Cataract Refract Surg 2006; 32:407–410 10. Hospital Infection Control Practices Advisory Committee (HICPAC). Recommendations for preventing the spread of vancomycin resistance. Infect Control Hosp Epidemiol 1995; 16:105–113; erratum, 498 11. O’Brien TP, Arshinoff SA, Mah FS. Perspectives on antibiotics for postoperative endophthalmitis prophylaxis: potential role of moxifloxacin. J Cataract Refract Surg 2007; 33:1790–1800 12. Sharifi E, Porco TC, Naseri A. Cost-effectiveness analysis of intracameral cefuroxime use for prophylaxis of endophthalmitis after cataract surgery. Ophthalmology 2009; 116:1887–1896 13. Koul S, Philipson A, Philipson BT, Arvidson S. Intraocular levels of cefuroxime in inflamed rabbit eyes. Eur J Ophthalmol 1993; 3:61–65 €m C. 14. Montan PG, Wejde G, Setterquist H, Rylander M, Zetterstro Prophylactic intracameral cefuroxime; evaluation of safety and kinetics in cataract surgery. J Cataract Refract Surg 2002; 28:982–987 J CATARACT REFRACT SURG - VOL 37, FEBRUARY 2011 278 OCULAR TOXICITY OF CEFUROXIME ~a M, Stewart OG. Macular thick15. Gupta MS, McKee HD, Saldan ness after cataract surgery with intracameral cefuroxime. J Cataract Refract Surg 2005; 31:1163–1166 16. Yoeruek E, Spitzer MS, Saygili O, Tatar O, Biedermann T, Yoeruek E, Bartz-Schmidt KU, Szurman P. Comparison of in vitro safety profiles of vancomycin and cefuroxime on human corneal endothelial cells for intracameral use. J Cataract Refract Surg 2008; 34:2139–2145 17. Sakarya Y, Sakarya R. Cefuroxime dilution error. Eur J Ophthalmol 2010; 20:460–461 18. Marmor MF, Fulton AB, Holder GE, Miyake Y, Brigell M, Bach M (for the International Society for Clinical Electrophysiology of Vision). ISCEV Standard for full-field clinical electroretinography (2008 update). Doc Ophthalmol 2009; 118:69–77. Available at: http://www.iscev.org/standards/pdfs/ERG_standard_2008.pdf. Accessed October 22, 2010 19. Mamalis N, Edelhauser HF, Dawson DG, Chew J, LeBoyer RM, Werner L. Toxic anterior segment syndrome. J Cataract Refract Surg 2006; 32:324–333 20. Mencucci R, Ponchietti C, Virgili G, Giansanti F, Menchini U. Corneal endothelial damage after cataract surgery: microincision versus standard technique. J Cataract Refract Surg 2006; 32:1351–1354 21. Gogate P, Ambardekar P, Kulkarni S, Deshpande R, Joshi S, Deshpande M. Comparison of endothelial cell loss after cataract 22. 23. 24. 25. 26. 27. surgery: phacoemulsification versus manual small-incision cataract surgery; six-week results of a randomized control trial. J Cataract Refract Surg 2010; 36:247–253 € €lsen Y, Ays‚e NB, Ozlem TY, Necati DM, Fatma YM, Gu € Are cefuroxime and vancomycin really safe on the Firdevs O. corneal endothelial cells? Graefes Arch Clin Exp Ophthalmol 2010; 248:415–420. Available at: http://www.springerlink.com/ content/5t2675247v2v14x8/fulltext.pdf Salvi SM, Soong TK, Kumar BV, Hawksworth NR. Central corneal thickness changes after phacoemulsification cataract surgery. J Cataract Refract Surg 2007; 33:1426–1428 ndez E, Fliesler SJ, Alvarez J, Pflugfelder SC, Herna Pflugfelder ME, Forster RK. Intravitreal vancomycin. Retinal toxicity, clearance, and interaction with gentamicin. Arch Ophthalmol 1987; 105:831–837. Available at: http://archopht. ama-assn.org/cgi/reprint/105/6/831. Accessed October 22, 2010 Talamo JH, D’Amico DJ, Hanninen LA, Kenyon KR, Shanks ET. The influence of aphakia and vitrectomy on experimental retinal toxicity of aminoglycoside antibiotics. Am J Ophthalmol 1985; 100:840–847 Fry LL. Vancomycin dilution error. J Cataract Refract Surg 2005; 31:1674 Trissel LA. Handbook on Injectable Drugs, 14th ed. Bethesda, MD, American Society of Health-System Pharmacists, 2007 J CATARACT REFRACT SURG - VOL 37, FEBRUARY 2011