* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Lecture 22: Female Pelvic Viscera: Introduction to the Female
Survey
Document related concepts
Transcript
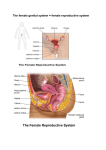
Lecture 22: Female Pelvic Viscera: Introduction to the Female Internal Genital Organs: Hemisection In general, pelvic viscera are arranged in the midline, from front to back Value of hemisection Female Internal Genital Organs The female internal genital organs consist of the ovaries, the uterus, the uterine tubes, and the vagina Function The female internal genitalia produce sex hormones and gametes Like male In addition, the female reproductive system must be able to protect and support a developing embryo Ovaries: Broad Ligament Background The ovaries, uterus, and uterine tubes are all held in position in the pelvic cavity within a common mesentery—the broad ligament The broad ligament is a double-layer of peritoneum that extends from the sides of the uterus to the floor and lateral walls of the pelvis Parts The broad ligament consists of three parts 1. The mesometrium is the largest part Supports uterus 2. The mesosalpinx is the superior free border Supports uterine tubes 3. The mesovarium is a small mesentery along the posterior aspect of the broad ligament Supports ovaries Ovary Introduction The ovaries—small, lumpy, almond-shaped and sized-organs—are the female gonads They produce the female gamete (the ovum) and reproductive hormones The ovaries are not covered with peritoneum, thus the ovulated egg is released into the peritoneal cavity Repeated ovulation gives the ovaries their scarred and distorted appearance Ligaments Two other ligaments—in addition to the broad ligament—are associated with the ovaries The ovarian ligament—the cranial remnant of the gubernaculum—extends from the uterus to the ovary The suspensory ligament is a peritoneal fold that extends from ovary to pelvic wall It contains the vessels and nerves of the ovary Uterine Tubes: Background The uterine tubes/oviducts/fallopian tubes connect the ovaries to the uterus Each tube is ~10 cm long and ~0.7 cm in diameter They conduct the ovum to the uterus and are generally the site of fertilization In the “ideal” disposition the tubes extend laterally and arch superiorly and posteriorly above the ovaries Notes: In reality, in ulstrasound examination, the tubes are often asymmetrical, having varying dispositions. Parts The uterine tubes are divisible into 4 parts 1. Infundibulum Funnel-shaped distal end terminates with fimbriae 2. Ampulla Widest and longest part, and usual site of fertilization 3. Isthmus Part entering uterus 4. Uterine part Within the walls of the uterus Uterus: Background The uterus (womb) is a thick-walled, pear-shaped, hollow muscular organ 7.5 x 5 x 2 cm It is the site of development of embryo and fetus Anatomy The uterus is divided into two main regions The body forms the upper two-thirds Contains slit-like uterine cavity (~6 cm long) The cervix forms the lower third The cervix is cylindrical and ~2.5 cm long The body is demarcated from the cervix by the isthmus (~1 cm wide) Pelvic Fascia Introduction Background The pelvic fascia is connective tissue occupying the space between the peritoneum and the muscular pelvic walls (where viscera is not present) It is a continuation of the endoabdominal (transversalis) fascia Pelvic Fascia Components The pelvic fascia is divided into two components Membranous pelvic fascia Endopelvic fascia Membranous Pelvic Fascia Background The membranous pelvic fascia is further subdivided into parietal and visceral parts The parietal pelvic fascia lines the muscles that make up the muscular walls and floor of the pelvis The visceral pelvic fascia directly ensheaths the pelvic organs Tendinous Arch Where the organs penetrate the pelvic floor, the parietal and visceral layer are continuous At this point, the parietal and visceral layers are thickened to form the tendinous arch of pelvic fascia The tendinous arch fastens prostate or bladder to the pubis, and prostate or vagina to the sacrum Endopelvic Fascia Background The endopelvic fascia varies markedly in density and content, and thus may be subdivided into two basic parts Loose areolar tissue serves as “packing” material and allows the bladder and rectum to expand Other parts of the endopelvic fascia are condensed to form fibrous structures—the hypogastric sheath and its laminae Hypogastric Sheath The hypogastric sheath extends from the lateral wall of the pelvis and divides medially to form ligamentous extensions, which serve as conduits for most neurovasculature—and ureters and ductus deferentes—passing to the pelvic viscera As well, these extensions provide support and are thus also referred to as pelvic ligaments Support of the Uterus Background It is important for the uterus to remain centered in the pelvic cavity (to avoid functional disturbances to the adjacent rectum and bladder), and resist the tendency to be pushed into the vagina (prolapse) This is accomplished in two main ways Natural position of the uterus Ligaments Natural Position The uterus is located posterior to the bladder and anterior to the rectum It is normally positioned such that the cervix is tipped forward relative to the axis of the vagina (anteversion) In addition, the body of the uterus is flexed anteriorly relative to the cervix (anteflexion) Ligaments Ligamentous support of the uterus is primarily provided by the broad ligament, the cardinal (transverse cervical) ligaments, and the uterosacral ligaments The round and ovarian ligaments—remnants of the gubernaculum—offer additional support Position of the Uterus Variation in Position Background The uterus is possibly the most dynamic structure in the human body Several factors can influence the size, proportion, and position of the uterus Rapid physiological changes involving the rectum and bladder Pregnancy Age Age At birth, the uterus has nearly adult proportions (length of body to length of cervix ratio of 2 to 1) Influence of maternal hormones Within weeks postpartum, the childhood ratio of 1:1 is established until puberty (2:1) After menopause the uterus reassumes a 1:1 ratio Pregnancy During pregnancy the uterus grows to occupy most of the abdominopelvic cavity and press against most organs Compression of vena cava in supine position? The uterus becomes very thin-walled (nearly membranous) Multiparous non-gravid uterus may cause slight protrusion of abdominal wall Prolapse When intra-abdominal pressure is increased, the normally anteverted and anteflexed uterus is pressed against the bladder A retroverted uterus is more likely to prolapse through the vagina Prolapse is also more likely in the presence of a disrupted perineal body or other pelvic diaphragm weakness Pouches Peritoneum covers most of the superior and anterior parts of the uterus Anteriorly the peritoneum reflects off the uterus onto the bladder, while posteriorly it reflects onto the rectum, creating pouches (vesicouterine and rectouterine) The rectouterine pouch, in particular, is clinically important as an area where fluid/infection can accumulate Vagina: Background The vagina is a distensible, musculomembranous tube, ~7-9 cm long It is generally collapsed, except at the cervix The vagina ascends posteriorly, at a 90º angle to the axis of the uterus, in-between the bladder and the rectum It passes between the medial margins of levator ani Fornices The vaginal fornix is the circular recess created by the protrusion of the cervix into the vagina The fornix is divided into anterior, posterior, and lateral fornices Of these, the posterior fornix is the deepest and has clinical relevance, in part due to it relation to the rectouterine pouch Note that in this illustration, fluid is accumulating deep to the peritoneum, in the rectouterine pouch. This would likely be due to an abscess on a pelvic organ. Fluid in the peritoneal cavity, such as blood, can also be aspirated using this method. Neurovasculature of Internal Genital Organs: Blood Supply Background Blood supply to the female internal genital organs derives from three main sources Ovarian artery Branch of lumbar aorta Uterine artery Internal pudendal artery Notes: The internal iliac artery has the most variable branching of any artery. Thus, identification of branches must be done by distribution, and not pattern of branching. Uterus and Vagina Arterial blood supply to the uterus derives from the uterine artery Arterial blood supply to the vagina derives from two arteries Vaginal branch of uterine artery Superior and middle parts of vagina Vaginal and internal pudendal artery Middle and inferior parts of vagina Ovaries and Uterine Tube The ovaries and uterine tubes receive blood from ovarian arteries (abdominal source) and ascending branches of uterine arteries (pelvic source) Both arteries bifurcate into tubal and ovarian branches These branches then anastamose with each other Venous Drainage The uterus and vagina drain primarily into the uterovaginal plexus of veins, which drains into the internal iliac veins The uterine tubes and ovaries drain primarily into the ovarian plexus of veins, which drains into the ovarian vein All four organs may drain into either plexus Lymphatics Lymph from female internal genitalia drains via two primary routes Most lymph drainage parallels venous drainage (internal iliac and ovarian veins) and travels to internal iliac and lumbar nodes Structures located superiorly in the anterior portion of the pelvis (mainly the body of the uterus) drain to external iliac nodes via routes that do not parallel venous drainage Innervation Somatic Inferior Vagina Only the inferior quarter of the vagina is sensitive to touch and temperature Somatic innervation is from deep branches of the perineal nerve Branch of pudendal nerve (S2-S4) Autonomic Background Autonomic innervation to female internal genitalia is supplied by two nerve plexuses Ovarian plexus Ovaries and uterine tubes Uterovaginal plexuses Uterus and vagina Sympathetic, parasympathetic, and visceral afferent fibers pass through these plexuses Visceral Afferents The ovaries and uterine tubes are intraperitoneal, thus superior to the pelvic pain line Pain fibers travel with sympathetic motor fibers to T11-L1 Caudal Epidural Anesthesia A caudal epidural block is a popular choice for participatory childbirth The anesthetic agent is injected through the sacral hiatus where it bathes S2-S4 nerve roots Structures inferior to the pelvic pain line—birth canal, pelvic floor, perineum—are anesthetized Structures superior to the line—body of uterus—are not Mother is aware of uterine contractions