* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Urinary Interleukin-18 level as an Early Biomarker in Acute Kidney
Survey
Document related concepts
Transcript
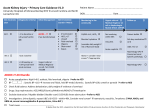
Urinary Interleukin-18 level as an Early Biomarker in Acute Kidney Injury in Critically Ill children. Abd El-Hameed. A. Abd El-Hameed a , Shaheen. A. Dabour , Soha. A. Ibrahim a, Eman. R. Abd ElGwad b, Eman. R. A bd-Almonaema, Effat. H. Assara and Wesam. E. Afifi a.. a The Pediatric Department, Faculty of Medicine, Benha University, Egypt. b Clinical Chemical Pathology Department, Faculty of Medicine, Benha University, Egypt. Correspondence to Wesam. E. Afifi, email Abstract Background: Interleukin-18 is a protein which in humans which encoded by the IL18 gene .The protein encoded by this gene is a pro inflammatory cytokine which is a mediator of renal ischemia–reperfusion injury, causing acute tubular necrosis, and neutrophil and monocyte infiltration of the renal parenchyma, so urinary IL-18 level has been shown a good biomarker in predicting AKI . Aim The aim of this work is to study of urinary interleukin -18 as an earlier predictor of AKI in critically ill children. Methodology: Fifty critically ill patients were included in our study (22 males, 28 females), patients collected from the Pediatrics ICU, Pediatric Department, Benha University Hospital. During the period from January 2015 to January 2016. The following investigations were done for all patients: CBC, CRP, urea, creatinine, blood culture, Na, K, glucose, albumin, ABG, bleeding profile & urinary IL-18, urinary IL-18 were measured on admission & after 48 hours. Results: the incidence of AKI was 44%, 3 patients from them were received dialysis, the most common admission diagnosis was infectious causes (44.8%), Urinary interleukin 18 has higher both sensitivity (90.9%) & specificity (92.9%) & has both better positive predictive value & negative predictive value. Serum creatinine has higher specificity (100%) & lower sensitivity (68.2%) & has good negative predictive value, but low in positive predictive value. Urinary interleukin 18 is better in predication of AKI than serum creatinine, as we can see from ROC curve that interleukin 18 has higher area under the curve (0.947) than creatinine (0.908). The best cut values for urinary interleukin 18 & serum creatinine from ROC curve, for creatinine the best cut value is 0.35 with sensitivity 95.5% & specificity 75% while for urinary interleukin 18 we can see that the best cut value was 80 with high both sensitivity (95.5%) & specificity (92.9%) which con firms that interleukin 18 is a better in predication of AKI than serum creatinine. Conclusion: urinary interleukin -18 as an earlier predictor of AKI in critically ill children prior to rise serum creatinine. Keywords: urinary Interleukin-18, Acute kidney injury, Systemic review, Predictive value. Introduction: Acute kidney injury (AKI) is characterized by a sudden and generally revertible renal function impairment, involving inability to maintain the normal homeostasis, and may or not be accompanied by reduced diuresis. Usually, AKI is categorized as pre-renal, related to reduced renal blood flow for inappropriate cardiac output or intravascular volume; intrinsic renal disease, from an insult to the renal parenchyma including ischemic , tubular, vascular or glomerular disorders; and post renal , due to urinary tract obstruction either in single kidney or both kidneys(1). During the childhood, the main AKI causes are sepsis, renal ischemia, and nephrotoxic drugs in critically ill patients (1). These patients, particularly those staying in intensive care units, are exposed to a number of conditions which may lead to renal impairment, thus significantly increasing the morbity & mortality rate. (2) Acute kidney injury occurs in approximately 30% of patients admitted to the intensive care unit and is commonly associated with multiple organ dysfunction syndromes. It is now known that acute kidney injury has a negative impact on patient morbidity and mortality that is caused mainly by non-renal organ failure (3). Although regarded as the standard indicators of kidney function loss, serum creatinine (sCr) level and urine output are recognized as having limitations. On the one hand, sCr cannot accurately reflect the GFR in a patient with unsteady state, and urine output is easily affected by water intake and the primary fluid state of the body (4). On the other hand, sCr and urine output have limited sensitivity and specificity, and a delayed response to kidney impairment. All these factors suggest that sCr and urine output are not appropriate markers in the early detection of AKI. Thus, an accurate and timely biomarker to predict AKI onset or progression after renal insult is urgently needed. Interleukin-18 is an eighteen pro-inflammatory cytokine up-regulated during endogenous inflammatory processes, and also it plays an important role in the pathophysiology of sepsis (5). it is necessary to evaluate the utility of urinary interleukin-18 as an AKI biomarker to clarify the relation between AKI, sepsis & mortality in critically ill patients with varying degree of underlying infection (6). The advances in new biomarkers that increases early clinical diagnosis capacity and the implementation of possible early treatment have promoted the study of AKI in children. Despite these advances and new technologies in renal replacement therapies, the mortality rate from AKI is still elevated. (7) Patient & methods: This study was conducted on patients collected from the Pediatrics ICU, Pediatric Department, Benha University Hospital. During the period from January, 2015 to January, 2016. Informed consents were taken from parents of included patients. The study was approved by the ethical committee of Benha University Then the cases were be further subdivided into two groups according to pRIFLE . Patient: 50 critically ill patients admitted to our ICU were divided into groups: Group (I): PICU cases without acute kidney injury (28 cases). Group (II): PICU cases with acute kidney injury (22 cases).The group (II) cases were classified into subgroups according to pediatric RIFLE maximum (pRIFLE max) which refer to the worst GFR during PICU stay period. Into 3 subgroups (R: Risk , I: Injury& F: Failure ) .The patient’s normal baseline GFR value of 100ml/1.73m2/24h was considered as a reference(8). Our cases are selected according to the following inclusion and exclusion criteria: Inclusion criteria: Both sex were included, Requirement for mechanical ventilation And / or More than one system failure (e.g. shock, respiratory failure, coma, IEM, DIC). Exclusion criteria: less than one month of age, more than 18 years of age, less than 24 hours stay in PICU, brain death at admission and chronic kidney disease which defined as GFR is less than 60ml/min1.73m2, for 3 months or more(9), end stage renal disease on regular hemodialysis, patients need medication of nephrotoxic drugs. Methodes: All our subject were submitted to the following: Full history ( Age and sex, History of the presenting problem, History of other systems affection (renal and non-renal), Administration of any medication), General examination including (Blood Pressure , weight, height, respiratoy distress, conscious level, UOP), Systemic examination (chest , heart , abdominal and neurological examination), and Laboratory investigations ( CBC, CRP, urea, creatinine, blood culture, Na, K, glucose, ABG, liver profile, bleeding profile, urinary interleukin18) GFR Glomerular filtration rate (GFR) was estimated using the following equation The original Schwartz formula is: crCl = k* height / serum creatinine (10). Height is measured in cm. Serum creatinine is measured in mg/dl. (National Kidney Disease Education Program recommendation). Two Urine samples were taken for measurement of interleukin -18 (one on admission & second sample 24 hours after admission), with Normal range: 5ng/ L– 100ng /L. Statistical methods: Data management and statistical analysis were performed using the Statistical Package for Social Sciences (SPSS) vs. 22. Numerical data were summarized using means and standard deviations or median and ranges (if non parametric). Categorical data were summarized as numbers and percentages. Comparisons between the 2 groups with respect to normally distributed numeric variables were done using the independent t-test or Mann Whitney’s U test (if non parametric). For categorical variables, differences were analyzed with 2 (chi square) test or Fisher’s exact test when appropriate. Spearman Correlation between variables was done, “rs” (Spearman correlation coefficient) ranges from +1 to -1, a value of 0 indicates that there is no association between the two variables; a value greater than 0 indicates a positive association; a value less than 0 indicates a negative association. Standard diagnostic indices including sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) were calculated for IL18 and Creatinine. Receiver operator characteristics (ROC curve) was used to determine the best cut off point of IL18 and Creatinine for prediction of acute kidney injury. All p-values are two-sided. P-values < 0.05 were considered significant. RESULTS: Our results will be demonstrated in the following tables & figures: Table (1): Study profile regarding incidence of AKI & its class Classification N % Normal 28 56.0 Risk 3 6.0 Injury 9 18.0 Failure 10 20.0 Table (2): Statistical comparison between AKI and non AKI cases regarding to least UOP & renal functions parameters: Non AKI cases(I) AKI Cases(II) P value Median 1.4 0.9 <0.001 Minimum 0.9 0.1 Maximum 2.5 1.9 Highest urea Mean 30.6 131.8 (mg/dl) ±SD 3.9 61.5 Least UOP (ml/kg h) Highest creatinine (mg/dl) Lowest GFR (ml∕min∕1.73m2) Minimum 25 35 Maximum 38 305 Median 0.4 1.2 Minimum 0.2 0.7 Maximum 0.6 6 Median 97.47 32.13 Minimum 75 10.4 Maximum 137.5 75.71 <0.001 <0.001 <0.001 Table (3): Statistical comparison between AKI and non AKI cases regarding urinary interleukin 18 on admission & after 48 hours: IL18 on admission (ng/ L) IL18 at 48h (ng/L) Non AKI cases(I) AKI Cases(II) P value Median 40 190 <0.001 Minimum 14 40 Maximum 70 230 Median 50 310 Minimum 20 40 Maximum 80 440 <0.001 Table (4): Statistical comparison between AKI and non AKI cases regarding serum creatinine on admission & after 48 hours: Non AKI Cases(I) AKI Cases(II) P value Creatinine on admission (mg/dl) Creatinine at 48h (mg/dl) Median 0.3 0.5 Minimum 0.2 0.3 Maximum 0.5 0.9 Median 0.3 0.9 Minimum 0.2 0.4 Maximum 0.6 1.3 <0.001 <0.001 Table (5): Standard diagnostic indices for urinary interleukin 18: RIFLE Positive (N=22) Negative (n=28) N % N % Positive 20 90.9 2 7.1 IL18 Negative 2 9.1 26 92.9 Sensitivity= 90.9 % , Specificity= 92.9 %, PPV= 90.9 %, NPV= 92.9 % Table (6): Standard diagnostic indices for serum creatinine: RIFLE Positive (N=22) Negative (28) n % N % 15 68.2 0 0.0 Creatinine Positive Negative 7 31.8 28 100.0 Sensitivity= 68.2 %, Specificity= 100 % , PPV= 100 %, NPV= 80 % Total 22 28 Total 15 35 Fig. (1): Receiver operating characteristic (ROC) curve to detect the sensitivity and specificity of urinary interleukin-18 on admission versus serum creatinine in predicting acute kidney injury. Table (7): comparison of the area under ROC curve (AUC) between urinary interleukin18 and serum creatinine: IL18 AUC 0.947 Std. Error 0.037 P value < 0.001 95% C.I. 0.875 – 1 Creatinine 0.908 0.04 < 0.001 0.83 - 0.987 Table (8): best cut-off values for urinary Interleukin18 and serum creatinine: IL18 Creatinine Cutoff value 80 0.35 Sensitivity 95.5 95.5 Specificity 92.9 75.0 DICUSSION: The critically ill patients, particularly those staying in intensive care units, are exposed to a number of conditions which may lead to renal impairment, thus significantly increasing the morbidity & mortality rate (2). Infectious causes were most common causes of admission in our study (44.8%), followed by heart failure (11.7%) & neurological causes (11.7%) denoting that infection was the most significant causes of PICU admission. Our study includes 50 critically patients 22 males (44%) and 28 females (56%) with median value of age was 0.67 year in non AKI cases and 2.75 year in AKI cases which shows statistically significant difference (p value 0.02). The incidence of AKI in this study was (44%), representing (22) cases, out of (50) cases admitted to the PICU admission. As regard to the incidence of AKI in various studies, the incidence was variable as Hoste et al., 2006 (11) reported incidence of 67.2%. while Ostermann &Chang,2007(2) reported AKI incidence of 35.8%. Bagshaw et al.,2008 (12) reported incidence of 36.1 %. Plotz et al.,2008 (13) reported incidence of 58 %. Keina et al.,2010 (14) reported that the incidence of AKI was 82%. This variation can be explained by specific epidemiological characteristics according to the area of study. The group II was subdivided into 3 subgroups representing the classes of AKI (severity) according to pRIFLE : Class (R) Risk, Class (I) injury & Class (F) failure In this study the different AKI classes incidences at maximal RIFLE were as the followings : 3 cases R (13.65%), 9 cases I (40.9%) & 10 cases F (45.45%). The AKI level incidence was different in other studies as keina et al.,2010 (14) reported that the maximal RIFLE score found during the patients stay was 39.1% for class (R), 37.2% for class ( I ) and 21.8% for class (F) while Akcan et al.,2007 (8) found 48.8%, 26% and 25.2%,respectively. Plotz et al .,2008 (13) reported incidences of 52%, 37% and11%, respectively .This variability of incidences can be explained by keina et al., 2010 (14) who reported that the cause of this variability was due to different populations studied, and the different ICU characteristics. Dialysis was needed in 3 patients (13.6 %) who were classified as RIFLE III stage of AKI (failure) having massively increased levels of serum creatinine of the 2nd samples in relation to the 1st samples and prolonged duration of oliguria. 2 of them were improved & one died, the patient of AKI group received conservative management. Blood pressure significantly decreased in group I (53.6 %) of cases compared to group II (36.4),while increased in group II (45.5%) of cases compared to group I (3.6%) & normal blood pressure level is higher in group I (42.9%) compared to group II (18.2%). As regards to sepsis there significant difference between two groups as sepsis was (72.7%) in group II compared to group I (42.9%). This agree with some studies which referred to sepsis as a cause and a consequence of AKI (Zapitelli, 2011 (15) and Mehta et al., 2002 (16), another American study referred to sepsis as a less important cause of AKI, being replaced by other causes such as oncologic and hematological causes in addition to respiratory failure (Williams et al., 2002(17). In addition, our study showed that dehydration was significantly associated with development of AKI as severe dehydration are common in group II (22.7%) than group I (3.6%), bad perfusion is common in group II (68.3%) than group I (39.3%) and that was in agreement with a Turkish study which showed that, according to the acute kidney injury network (AKIN) definitions and classifications, dehydration is considered one of the important AKI risk factors (Ozçakar et al.,2009 (18). It is also in agreement with Lameire et al.,2005 (19) who reported that shock was one of the risk factors for AKI and had been implicated in the pathophysiology of AKI, as during these periods (hypoperfusion), as a result of either cardiovascular shock or the vasoconstrictive auto regulatory process, as the metabolically active tubular epithelium is placed under hypoxic/ischemic stress. In group I, urinary interleukin on admission ranged from (14-70 ng / L) the median value is 40 ng/ L, urinary interleukin at 48 h ranged from (20- 80 ng / L) the median value is 50 ng/ L. While in group II, urinary interleukin on admission ranged from (40-230 ng/ L) the median value is 190 ng/ L, urinary interleukin at 48h ranged from(40-440 ng/ L) the median value is 310 ng/ L. There is highly statistical significant differance in urinary interleukin -18 on admission & at 48hours after admission between group II and group I with p value<0.001, it was higher in group II on admission & after 48hours. In group I, serum creatinine on admission ranged from (0.2- 0.5 mg/dl) the median value is 0.3 mg/dl , serum creatinine at 48h ranged from(0.2 -0.6 mg/ dl) the median value is 0.3 mg/ dl. While in group II, serum creatinine on admission ranged from (0.3- 0.9 mg/dl) the median value is 0.5 mg/dl , serum creatinine at 48h ranged from(0.4 -1.3 mg/ dl) the median value is 0.9 mg/ dl. There is highly statistical significant differance in serum creatinine on admission & at 48hours after admission between group II and group I with p value<0.001. it was higher in group II 48h after admission. but this difference in serum creatinine on admission clinically insignificant as the level is in normal range in both group. Regarding patients' laboratory results, the 1st serum creatinine sample taken upon enrollment showed no clinical significant difference between patients with AKI and those with no AKI, while the 2nd sample that was taken 48 hours later was significantly higher in patients with AKI. These results were in agreement with multiple studies that serum creatinine can be used as a late marker for diagnosis of AKI (Honore et al.,2007 (20)and Melnikov and Molitoris,2008 (21). While the 1st serum creatinine sample was not an indicator of evident AKI, the 1st urinary interleukin-18 sample taken at the same time was significantly higher in patients with AKI and subsequently, the 2nd urinary interleukin-18 sample that was taken 48 hours later, in addition to the interleukin-18 rise in both samples which showed the same significant rise in patients with AKI. This was in accordance with many other studies which proved that interleukin-18 contributes to renal damage after ischemia-reperfusion injury and that ischemic kidney tissue damage initiates production of interleukin-18 (Wu et al.,2008 (22) and also proved that interleukin18 is increased in the glomeruli of patients with autoimmune lupus nephritis (LN) (Calvani et al.,2004(23). All of the previous results confirm that rise of urinary interleukin-18 level preceded rise of serum creatinine level by 48 hours in critically ill children who developed AKI which was in agreement with many other studies that showed the same fact (Parikh et al,2006 (24) , Devarajan,2008 (25), and Washburn et al.,2008 (6). However, a single recent American study showed that urinary interleukin-18 did not reliably predict AKI development, but did predict only poor clinical outcomes, but we have to clarify that this study was different for being performed on adults, not children (Siew et al., 2010(26). Urinary interleukin 18 showed highly statistical significant positive correlation with highest urea, highest creatinine & serum K, and show highly statistical significant negative correlation between urinary interleukin 18 & lowest UOP, GFR, PH &bicarbonate with p value<0.001 There was significant negative correlation between interleukin 18 & HB, platelet , CRP & serum albumin with p value =0.002, and there were no significant correlation between interleukin 18 & other parameters. Serum creatinine showed highly statistical significant positive correlation with highest urea, highest creatinine & serum K, and show highly statistical significant negative correlation between serum creatinine & lowest UOP, GFR, PH &bicarbonate with p value<0.001 There was significant negative correlation between serum creatinine & HB& platelet with p value =0.02, and there are no significant correlation between interleukin 18 & other parameters. Urinary interleukin 18 has higher both sensitivity (90.9%) & specificity (92.9%) & has both better positive predictive value & negative predictive value. Serum creatinine has higher specificity (100%) & lower sensitivity ( 68.2%) & has good negative predictive value , but low in positive predictive value. Urinary interleukin 18 is better in predication of AKI than serum creatinine, as we can see from ROC curve that interleukin 18 has higher area under the curve (0.947) than creatinine (0.908). The best cutoff values for urinary interleukin 18 & serum creatinine from ROC curve, for creatinine the best cut value is 0.35mg/dl with sensitivity 95.5% & specificity 75% while for urinary interleukin 18 we can see that the best cut value was 80 ng/L with high both sensitivity (95.5%)& specificity(92.9%) which confirms that interleukin 18 is a better in predication of AKI than serum creatinine. Somewhat different cut off levels were reported by (Washburn et al,(8) who found that interleukin-18 concentration in critically ill children at cut off level of 100 ng /l had the best specificity (81%) to predict AKI development upon enrollment, while at cut off level 200 ng /l, interleukin-18 had the highest specificity (93%) and to predict AKI after 48 hours after admission. This might suggest that the test needs further standardization and layer scale study to be used routinely for detecting AKI in different populations in the critical care setting. Conclusion: Our study showed that elevation of urinary interleukin-18 level preceded rise in serum creatinine level in critically ill patients who developed AKI by 48 hours, making the urinary interleukin-18 is an early AKI biomarker in this category of children. Recommendation: Frequent monitoring and observation of critically ill children admitted to pediatric intensive care unit which is extremely important to prevent AKI that represents a significant but under-recognized problem in clinical medicine, with serious immediate and long-term consequences, Further researches should continue to identify new risk factors that could be responsible for occurrence of AKI in PICU, Further studies have to be done in order to confirm and properly utilize the urinary interleukin-18 as an early acute kidney injury biomarker in critically ill children. Conflict of interest: None declared. Acknowledgement: We like to thank all the doctors who participated in the study, the parents of the patients and the nursing staff. References: 1- Liberato Bresolin N & Toporovski J. (2005): Insuficiência renal agudana sepse. Arch Latinoam Nefrol Pediatr.;5(3):164-72. 2- Ostermann M & Chang RW. (2007): Acute kidney injury in the intensive care unit according RIFLE. Crit Care Med.;35(8):1837-43; quiz 185 3- Fauble S.(2009): Acute kidney injury and multiple organ dysfunction syndrome, Minerva Urol Nefrol (61):171-188. 4- Herget-Rosenthal S, Marggraf G, Hüsing J, et al.,(2004): Early detection of acute renal failure by serum cystatin C. Kidney Int.;66(3):1115–1122. doi: 10.1111/j.1523-1755.2004.00861.x. 2. 5- Tschoeke SK,Oberholzer A, Moldawer LL.(2006): interleukin-18: a novel prognostic cytokine in bacteria-induced sepsis. Crit Care M ed 34:1225-1233. 6- Washburn K, Zappitelli M, Arikan A et al., (2008):. Urinary interleukin-18 is an acute kidney injury biomarker in critically ill children. Nephrol Dial Transplant 2008; 23: 566-572 7- Lenihan C, Montez-Rath M, Mangano C et al., (2013): trends in acute kidney injury, associated use of dialysis, and mortality after cardiac surgy, 1999-2008, Annals of thoracic Surgery, 95, 1, 2028. 8- Akcan-Arikan A, Zappitelli M, Loftis LL et al., (2007): Washburn KK, Jefferson LS, Goldstein SL. Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int.; 71(10):1028-35. 9- Hogg RJ, Furths, Lemley KV et al., (2003): National kidney foundations kidney disease out comes quality initative clinical practice guidelines for kidney disease in children and adolescents ,evaluation ,classification and stratification pediatric (111):146-21. 10- Schwartz GJ, Brion LP & Spitzer A. (1987): The use of plasma creati-nine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr. Clin. NorthAm.;34(3):571-90. 11- Hoste EA,Clermont G, Kersten A et al., (2006): RIFLE criteria for a cute kidney injury are associated with hospital mortality incritically ill patients: A cohort analysis. Crit Care 10: R73. 12- Bagshaw SM, George C, Dinu I et al., (2008): A multi-centre evaluation of the RIFLE criteria for early acute kidney injury in critically ill patients. Nephrol Dial Transplant.;23(4):1203-10. 13- Plötz FB, Bouma AB, van Wijk JA et al., (2008): Pediatric acute kidney injury in the ICU: an independent evaluation of pRIFLE criteria. Intensive Care Med.; 34(9):1713-7. 14- Kenia Machado , Souza Freire , Nilzete Liberato et al., (2010): Acute kidney injury in children: incidence and prognostic factors in critically ill patients Rev Bras Ter Intensiva.; 22(2):166-174. 15- Zappitelli M.(2008). Epidemiology and diagnosis of acute kidney injury. Semin Nephrol 2008; 28(5): 436-46 16- Mehta RL, Bouchard J, Soroko SB et al., (2011): Program to Improve Care in Acute Renal Disease (PICARD) Study Group. Sepsis as a cause and consequence of acute kidney injury: Program to Improve Care in Acute Renal Disease. Intensive Care Med 2011; 37(2): 241-8 17- Williams DM, Sreedhar SS, Mickell JJ et al., (2002):. Acute kidney failure: a pediatric experience over 20 years. Arch Pediatr Adolesc Med ; 156(9): 893-900. 18- Ozçakar ZB, Yalçinkaya F, Altas B et al.,(2009): Application of the new classification criteria of the Acute Kidney Injury Network: a pilot study in a pediatric population. Pediatr Nephrol. ; 24(7): 1379-84 19- Lameire N, Van Biesen W & Vanholder R. (2005): Acute renal failure. Lancet 365: 417–430. 20- Honore PM, Joannes-Boyau O, Boer W et al., (2007): Acute kidney injury in the ICU: time has come for an early biomarker kit. Acta Clin Belg Suppl ; (2): 318-21. 21- Melnikov VY & Molitoris BA. (2008): Improvements in the diagnosis of acute kidney injury. Saudi J Kidney Dis Transpl ; 19(4): 537-44. 22- Wu H, Craft ML, Wang P et al., (2008): IL-18 contributes to renal damage after ischemiareperfusion. J Am Soc Nephrol ; 19(12): 2331-41 23- Calvani N, Richards HB, Tucci M et al.,(2004): Up-regulation of IL-18 and predominance of a Th1 immune response is a hallmark of lupus nephritis. Clin Exp Immunol ; 138: 171-178. 24- Parikh CR, Mishra J, Thiessen-Philbrook H, et al., (2006): Urinary IL-18 is an early predictive biomarker of acute kidney injury after cardiac surgery. Kidney Int. 2006;70(1):199–203. doi: 10.1038/sj.ki.5001527. 25- Devarajan P.(2008): The future of pediatric acute kidney injury management--biomarkers. Semin Nephrol ; 28(5): 493-8. 26- Siew ED, Ikizler TA, Gebretsadik T et al., (2010):. Elevated urinary IL-18 levels at the time of ICU admission predict adverse clinical outcomes. Clin J Am Soc Nephrol 2010; 5(8): 1497-505.