* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Non-Psychotic Chaotic and Challenging Disorders
Survey
Document related concepts
Transcript
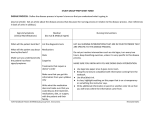
Cluster 8 Non-Psychotic Chaotic and Challenging Disorders This group will have a wide range of symptoms and chaotic and challenging lifestyles. They are characterised by moderate to very severe repeat deliberate self-harm and/or other impulsive behaviour and chaotic, over dependent engagement and often hostile engagement with services. Diagnoses: Likely to include F60 Personality Disorder Structured Assessment CORE Personalised multi- disciplinary assessment including physical, social, mental health and risk assessment with due consideration given to safeguarding and vulnerability issues. (Using Morgan risk assessment tool) An assessment with the service user to consider whether a psychological intervention may be appropriate Assessment to identify current coping strategies and strengths for managing distress. SUPPLEMENTARY As appropriate, for women consider issues around sexual health and pregnancy. Carers views considered and carers assessment offered if appropriate Services provided by LPT Services provided by Mental Health Social Care Team Services provided by 3rd Sector agencies Services provided by primary health care Enabling & Therapeutic Interventions CORE interventions will include: Providing information about cluster, diagnosis, pathway & services. - Provide patient information leaflets Supportive & empathic relationships. Personalised care, All patients should have crisis plan in place Physical healthcare needs resulting from self-harm needs to be re-assessed on each contact following self-harm. Initial risk management plan for crisis resolution & reducing acute aggravating factors. Treatment plans should take note of best practice and be evidence based. SUPPLEMENTARY Assessment will have identified if the service user can benefit from psychological approaches A range of psychological interventions should be considered (see notes) Interventions aim to reduce impulsivity, improve interpersonal difficulties and/or offending behaviours or improve distress tolerance. This could involve weekly therapy or day programmes Drug treatment - should not be used specifically for borderline personality disorder or for the individual symptoms or behaviour associated with the disorder. (See notes) Advise/signpost/access self-help (e.g. groups), self-monitoring (e.g. triggers, early warning signs), health promotion. Consider referral to third sector for early intervention for parental guidance and family focused interventions such as brief or strategic family therapy Possible employment, voluntary work or education/ training/ volunteering support to those wishing it Locality teams should assess current situation and accommodation needs. (see notes) Advice/advocacy/link to other specialist advice/support as necessary Review CORE Care plans are agreed with the service user Mental and physical wellbeing, role functioning, treatment should be regularly reviewed to inform ongoing care Review clustering and care plan at 6 months, or more frequently if needed Contingency & crisis plans need to be in place and regularly reviewed. SUPPLEMENTARY Use short, self-completion questionnaires to monitor when possible Review drug treatment for co-morbid conditions particularly initiation and adherence in depression that is not responding. Relapse prevention: monitor those on long term medications and consider reduction programs Review after 12 months Sustained Improvement Discharge to primary care with care plan and relapse prevention strategies appropriate to clients’ needs Encourage use of self-help resources Average duration of episode is 26+ months Detailed Notes Assessment CORE • All assessments will be individualised and multidisciplinary. • Assess whether the service user is likely to benefit from psychological therapies and at what level these need to be accessed. Seek consultation or assessment from specialist service where appropriate. • Consideration to be given to extra assessment for co-morbid conditions e.g. Learning Disabilities, Deliberate Self-harm, substance abuse etc. SUPPLEMENTARY • Anti-social personality disorder: a structured assessment; thorough multi-agency risk assessment and management plan. If assessed within forensic services use such tools as PCL-R or PCL-SV and HHCR-20 • Borderline Personality Disorder: assess by multidisciplinary teams; possible extra assessment for co-morbid conditions (e.g. LD/DSH) plus possible associated auxiliary interventions. • Special consideration to be given to assessing safeguarding issues for the vulnerable patient and children and vulnerable adults in contact with the patient. Special consideration also needs to be made for assessing safeguarding issues in pregnancy for women and their partners. • Special consideration needs to be made for assessing safeguarding issues in pregnancy for women and their partners and the impact of the service user’s personality upon children and vulnerable adults. • Where appropriate discuss smoking and offer smoking cessation plans. • Use specific assessment tools appropriate to the patient group and treatment approach. These may include Recovery star/ HoNos, Enabling and Therapeutic Interventions The purpose of interventions will be to encourage stability and relapse prevention, maximise role functioning and maintain or enhance current social role functioning, reduce risk of self-harm and promote better adjustment to situation. Interventions will help the patient to take as much responsibility for themselves as they are able to at the time. These interventions will involve on-going assessments, enabling and monitoring by lead professional, medical staff, nursing, psychological therapists, clinical psychology, and support staff as guided by the principles of Care Programme Approach (CPA). CORE ENABLING INTERVENTIONS • • • • • • • • • • Under CPA provisions provide, information about cluster, diagnosis, pathway and services. Initial risk management plan for crisis resolution & reducing acute aggravating factors. Personalised care, good communication within care team and with service user in partnership to promote autonomy & choice; involvement in finding solutions & recovery Coordination is crucial to holistic care that fits with individual needs and makes efficient and effective use of local resources. Promote development of patient centred aims for recovery. Develop contingency and crisis plans. Physical healthcare needs resulting from self-harm should be re-assessed on each contact following self-harm and the care plan reviewed focusing on preventative interventions. Emphasis should be given to the patient working with responsibility for his /her own self care. Positive risk management relies upon good communications, responsibility held jointly across services/clinicians, and the use of appropriate measuring tools. Where different services are involved in different aspects of the care package good communications between members of the care team are essential. It is important that the care team as a whole work to understand and contain the re-creation of aspects of the patients unconscious dynamics within the team. Assess accommodation needs. Provide on-going accommodation monitoring/support as necessary. SUPPLEMENTARY ENABLING INTERVENTIONS • • • • • • • Medication for the overall treatment of co-morbid conditions can be considered ,for borderline personality disorder the cautious short term use of sedative medication or use of drug treatments in crisis. (Ref NICE guidance 2009) Locality teams in conjunction with social care should assess current accommodation needs linking with other agencies as necessary. Due to the demanding nature of the more intensive psychological therapies secure accommodation needs to be in place prior to referral to these programmes. Provide specific gender, ethnic or communication support as needed, .e.g provide interpreter, sexual health advice/ support.. As appropriate advise on and signpost to self-help (eg groups & web based resources), self-monitoring (eg triggers,& signs), health promotion (eg smoking cessation, exercise, activity scheduling, diet, sleep, social support, work patterns, coping strategies, and activities of daily living etc) Signpost to specialist advice on finance, benefits and debt Consider use of befriending and training volunteers. If support to carer’s, friends and family of service users is required consideration should be given about which member of the care team is best placed to offer this and care taken to support the confidentiality boundary necessary to some psychological interventions. Provide information about self-help support groups. Consider family interventions e.g. psycho education, family therapy, offer carer’s assessment. • The care team should signpost to 3rd Sector agencies to address socio-economic needs. (eg REMIT). • Encourage Personalization of budgets with the help of social care. • Advice/advocacy/link to other specialist advice/support as necessary Specific Therapeutic Interventions: • CORE • • • • A detailed assessment will have already identified whether the service user is able to benefit from psychological approaches and whether this necessitates the referral to, or consultation with specialist services. All psychological interventions should be offered by competent trained staff with appropriate supervision arrangements in place. Treatment plans should take note of best practice and be evidence based. If the service user is unable to benefit from psychological interventions due to current mental state the focus should be upon coherent care planning with consultation between secondary and specialist services. SUPPLEMENTARY • Consultation, professionals meetings, supervision and joint assessments are recommended and particularly for patients in crisis who present significant risk of self-harm, harm to others or suicide risk • If the person would benefit from supportive interventions or specific psychological treatments this may be provided within primary care, the locality team or necessitate referral on to a level 4 service, or secondary care service. • Specific interventions may include group work, or group CBT that aims to reduce impulsivity (impulsivity can lead to acting out, deliberate self-harm and the use of crisis services) , improve interpersonal functioning and /or offending behaviours; psychoeducation: stop and think groups or other groups that aim to improve distress tolerance. • Consider activity based groups and combined day therapy has also been shown to beneficial. • Where it has been assessed that the service user can benefit from a talking therapy and has a wish to explore internal and interpersonal difficulties, and some willingness to recognise the contribution one has made/is making to one’s own difficulties; and the capacity to bear the distress this may bring individual or group psychotherapy may be considered. • The therapeutic community or women’s day programme may be appropriate for service users who are insufficiently contained within other programmes. • If there is also substance/alcohol abuse consider psychosocial interventions and specialist substance misuse service support as appropriate. Review CORE • Care plans are agreed with the service user and actions planned and implemented to achieve it’s aims • Mental and physical wellbeing, role functioning, treatment should be regularly reviewed to inform ongoing care • The care plan must be suitable to the level of need and fit the needs & therapeutic & recovery aims for the person • Contingency & crisis plans need to be in place and regularly reviewed. • Ensure information from an annual physical health check (from within service or primary care) is used in care planning. • Review clustering and care plan at 6 months, or more frequently if need/circumstances appear to make this necessary. SUPPLEMENTARY • Use short, self-completion questionnaires to monitor when possible, such as CORE, PROMs and specific CBT measures to assess whether the service user has a better understanding of symptoms and increased ability to manage; a greater understanding of self and the part they play in their difficulties and as improved capacity to bear distress without recourse to self-harm; plus stabilization of symptoms. • Specific therapist measures will be used that are coherent with the treatment approach • Review drug treatment, for co-morbid conditions particularly initiation and adherence especially in depression that is not responding due to suicide risk. • Relapse prevention: monitor those on long term medications and consider reduction programmes • In case of deterioration consider re-clustering or referral on to more intensive treatment programme . Sustained improvement Consider discharge to primary care with relapse prevention strategies appropriate to clients’ needs Encourage use of self-help resources