* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download SEPTA Anxiety Mental Health Concerns_March 2016
Antisocial personality disorder wikipedia , lookup
Major depressive disorder wikipedia , lookup
Rumination syndrome wikipedia , lookup
Mental health professional wikipedia , lookup
Recovery International wikipedia , lookup
Glossary of psychiatry wikipedia , lookup
Depersonalization disorder wikipedia , lookup
Selective mutism wikipedia , lookup
Mental status examination wikipedia , lookup
Obsessive–compulsive disorder wikipedia , lookup
Emergency psychiatry wikipedia , lookup
Narcissistic personality disorder wikipedia , lookup
Spectrum disorder wikipedia , lookup
Mental disorder wikipedia , lookup
Dissociative identity disorder wikipedia , lookup
Diagnostic and Statistical Manual of Mental Disorders wikipedia , lookup
Controversy surrounding psychiatry wikipedia , lookup
History of psychiatry wikipedia , lookup
Conversion disorder wikipedia , lookup
Classification of mental disorders wikipedia , lookup
Asperger syndrome wikipedia , lookup
Panic disorder wikipedia , lookup
Causes of mental disorders wikipedia , lookup
Child psychopathology wikipedia , lookup
Behavioral theories of depression wikipedia , lookup
History of mental disorders wikipedia , lookup
Anxiety disorder wikipedia , lookup
Claustrophobia wikipedia , lookup
Abnormal psychology wikipedia , lookup
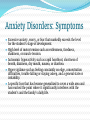
SEPTA Presentation, March 2016 Lynn Rafalik, Executive Director of Pupil Personnel Services Diane Burns-Dobson, Social Worker Ann Constantine, Social Worker Heather Wynne, School Psychologist Prevalence of Mental Health Disorders in Youth1 ● 20% (1 in 5 children 13-18 years old) have had or are still affected by a serious mental health disorder (National Institute of Mental Health) ● In 8-15 year olds, 13% of children had a diagnosable mental disorder (Center for Disease Control) Protective 3 Factors Healthy routines Good self-esteem Practical problem- solving skills Feeling in control, internal locus of control Parental/familial support Feeling close with at least one adult Monitoring of activities Regular school attendance and academic performance Positive social support system Community participation Health recreational activities Mental Health Concerns ● Anxiety ● Depression ● Low Self-Esteem ● School Refusal ● Attention Healthy vs. Unhealthy Anxiety Anxiety helps us get out of harms way and prepares us for important events. It also warns us when we need to take action. Everyday Anxiety Anxiety Disorder Worry about paying bills, landing a job, a romantic breakup, or other important life events Constant and unsubstantiated worry that causes significant distress and interferes with daily life Embarrassment or self-consciousness in an uncomfortable or awkward social situation Avoiding social situations for fear of being judged, embarrassed, or humiliated A case of nerves or sweating before a big test, business presentation, stage performance, or other significant event Seemingly out-of-the-blue panic attacks and the preoccupation with the fear of having another one Realistic fear of a dangerous object, place, or situation Irrational fear or avoidance of an object, place, or situation that poses little or no threat of danger Anxiety, sadness, or difficulty sleeping immediately after a traumatic event Recurring nightmares, flashbacks, or emotional numbing related to a traumatic event that occurred several months or years before Anxiety Disorders: Symptoms ● Excessive anxiety, worry, or fear that markedly exceeds the level for the student’s stage of development. ● High level of motor tension such as restlessness, tiredness, shakiness, or muscle tension. ● Autonomic hyperactivity such as rapid heartbeat, shortness of breath, dizziness, dry mouth, nausea, or diarrhea. ● Hyper vigilance such as feeling constantly on edge, concentration difficulties, trouble falling or staying asleep, and a general state or irritability. ● A specific fear that has become generalized to cover a wide area and has reached the point where it significantly interferes with the student’s and the family’s daily life. Four Dimensions of 2 Anxiety Dimension Description Emotion Feelings of fear, tension, worry, nervousness, panic, terror Physiology Stomach discomfort, muscle tension, rapid breathing, nervous system arousal Cognition Future-oriented thoughts, pessimistic expectations Behavior Avoidance, aggression Note: Researchers are learning that anxiety disorders run in families, and that they have a biological basis, much like allergies or diabetes and other disorders. Anxiety disorders may develop from a complex set of risk factors, including genetics, brain chemistry, personality, and life events. Therapeutic Interventions Cognitive-Behavioral Therapy (85% reduction in symptoms after therapy , Chorpita et al., 2002) Facilitative Strategies: Behavioral Strategies: Relaxation, Systematic Desensitization, Social Skills Cognitive Techniques: Problem-Solving, Self-Monitoring, SelfInstructional, Self-Control Exposure Therapy: incremental exposure to situations or objects with accompanying facilitative strategies Modeling of appropriate behavior Positive Self-Talk Self Awareness and Psychoeducation Identification of feeling, situation, and trigger Identification and application of coping strategies Therapeutic Interventions Acceptance and Commitment Therapy (ACT) Use of metaphors and experiential exercises to associate positive feelings with triggers and upsetting situations Healthy contact with self by noticing and accepting feelings as they occur in daily life ACT: Accept your reactions and be present; Choose a valued direction; Take action Dialectic Behavioral Therapy (DBT) Use of coping skills and relaxation techniques to change patterns of behavior/reaction brought on by emotions, thoughts, feelings, and events Dialectical Behavior Therapy (DBT) Distract with ACCEPTS Activities – positive activities Contribute – help others Comparison – compare yourself to someone else less fortunate Emotions – change situation so you feel a different emotion Push Away – push away emotions or remove yourself from the situation Thoughts – force your mind to think about something else Sensation – change nervous system arousal by changing temperatures, rubbing textured objects IMPROVE the moment Imagery – relaxing and peaceful scenes Meaning – find purpose in what you’re feeling Prayer – meditation Relaxation – Relax your muscles, deep breathing One thing in the moment – focus on one item, mindfulness, iSpy Vacation – Take a break Encouragement – positive self-talk and self-promotion Types of Anxiety Disorders ● Generalized Anxiety Disorder ● Specific Phobia/Social Phobia ● Panic Disorder ● Obsessive-Compulsive Disorder ● Separation Anxiety ● Post-Traumatic Stress Disorder Generalized Anxiety Disorder (GAD): Symptoms Global, free-floating feelings of worry Worries are vague, and flexible toward the environment Feelings of nervousness without a root cause or trigger People may experience restlessness, concentration difficulties, irritability, muscle tension, somatic complaints, sleep difficulties Specific Phobia: Symptoms Intense worry over a concrete object, situation, or event Adolescents tend to avoid the trigger Social Phobia Anxious about being with other people Self-conscious in front of other people Afraid of being embarrassed in front of other people Worry for days or weeks before an event where other people will be ● Stay away from places where there are other people ● Have a hard time making friends and keeping friends ● May have physiological body symptoms when they are with other people (e.g., blushing, heavy sweating, trembling, nausea and having a hard time talking) ● ● ● ● Social/Specific Phobia: Intervention Supports Model appropriate behavior Reduce social demands with systematic desensitization Allow student to eat in alternative place with staff member and/or peers Introduce student to teacher and staff before school starts Flexible seating with teacher and/or student buddy proximity Gradually increase time with peers Reduce demands to triggering events or objects Example: If curriculum includes spiders with a student with agoraphobia, cover pictures or reduce written language Student conference with teacher Parent consultation Panic Attack: Symptoms Sudden onset of fear or worry, with nervous system arousal Attacks occur repeatedly, without a specific trigger (specific triggers would warrant specific phobia) Individuals may avoid situations which increase heart rate and nervous system arousal Panic Attack: Interventions and Supports Have student identify safe places to go to when they are experiencing panic attacks Nurse’s office Related Support Personnel: School Counselor, Social Worker, Psychologist, Speech-Language Pathologist Relaxation techniques Deep breathing Thinking of a peaceful place Meditation Calming thoughts Obsessive-Compulsive Disorder (OCD): Symptoms Obsessive Thoughts Unwanted, repeating thoughts, impulses, or images associated with anxiety Common thoughts: contamination, symmetry/exactness, safety, religious preoccupation Compulsive Behaviors Unwanted, repetitive actions or mental acts that an individual is driven to perform in response to obsessive thoughts Common compulsions: washing, checking, repeating, ordering, counting, hoarding, touching OCD: Intervention Supports Awareness and identification of thoughts and compulsions Parent, staff, and student consultation Monitoring of thoughts and compulsions in the classroom by teacher Teacher-assisted feedback and intervention Breaks Modification of class work Gentle feedback on behaviors Suggestion of calming strategy Separation Anxiety: Symptoms ● Excessive emotional distress and repeated complaints (e.g., crying, ● ● ● ● ● ● regressive behaviors, pleading with parents to stay, temper tantrums) when anticipating separation from home or major attachment figures. Persistent and unrealistic worry about possible harm occurring to major attachment figures or excessive fear that they will leave and not return/be lost kidnapped, killed, or the victim of an accident). Repeated complaints and heightened distress (e.g., pleading to go home, demanding to see or call a parent) after separation from home or the attachment figure has occurred. Persistent fear or avoidance of being alone or refusal to go to sleep as manifested by excessive clinging and shadowing or a major attachment figure. Frequent somatic complaints (e.g., headaches, stomachaches, nausea) when separated from home or the attachment figure is anticipated. Excessive need for reassurance about safety and protection from possible harm or danger Low self-esteem and lack of self-confidence that contributes to the fear of being alone or participating in social activities. Separation Anxiety: Intervention Supports Younger Children Sticker chart in morning where they earn rewards for leaving their parents Adolescents Morning routine/classroom for transition time Behavioral Supports Student check-in with related services personnel Post-Traumatic Stress Disorder (PTSD) Re-experiencing symptoms ● Flashbacks - reliving the trauma over and over, including physical symptoms like racing heart or sweating ● Bad dreams ● Frightening thoughts Avoidance symptoms ● Staying away from places, events, or objects that are reminders of the experience. ● Feeling emotionally numb ● Feeling strong feelings of guilt, depression, or worry ● Losing interest in activities that were enjoyable in the past ● Having trouble remembering the dangerous event Hyperarousal symptoms ● Being easily startled ● Feeling tense or “on edge” ● Having difficulty sleeping, and/or having angry outbursts Anxiety Management Websites for Parents http://www.copingcatparents.com/node/15 http://kidshealth.org/en/parents/anxiety-disorders.html http://www.worrywisekids.org/ http://www.copingcatparents.com/Child_Anxiety_Tales Online parent education program http://www.mdaap.org/Bi_Ped_Brief_Interv_Anxiety.pdf YouTube Videos Teaching Children Deep Relaxation Breathing http://youtu.be/_mZbzDOpylA http://youtu.be/VOnDA6_MAWIk Depression Most common mental health concern in US 1 out of 33 children may have depression 1 out of 8 teens may have depression Depression: Symptoms ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● Sad or flat affect Preoccupation with the subject of death Suicidal thought and/or actions Mood irritability Isolations from family and/or peers Deterioration of academic performance Lack of interest in previously enjoyed activities Refusal to communicate openly Drug use to elevate mood Low energy Little or no eye contact and frequent verbalizations of low self-esteem Reduced appetite Increased sleep Poor concentration and indecision Feelings of unhappiness, worthlessness, or inappropriate guilt Unresolved grief issues Mood-related hallucinations or delusions Depression: Intervention Supports Assess for safety Suicide is the third leading cause of death for young adults aged 10-24 (CDC) Among 9-12th graders, 17% of students seriously considered attempting suicide in the past 12 months, 13.6% made a plan, and 8.0% attempted Columbia-Suicide Severity Rating Scale (C-SSRS): http://www.cssrs.columbia.edu/index.html Lifestyle changes Exercise, Nutrition, Sleep, Social Support, Stress Reduction Coping Skills for Adolescents http://www.yourlifeyourvoice.org/Style%20Library/99%20Coping%20S kills%20Poster.pdf Low Self-Esteem: Symptoms ● Inability to accept compliments ● Verbalization of self-disparaging remarks ● Seeing him/herself as unattractive, worthless, stupid, a loser, a burden, and unimportant; taking blame easily ● Avoiding contact or excessively seeking attention with ● ● ● ● adults and peers Acting out in negative ways that are quite obviously attention seeking Inability to identify or accept his/her positive traits or talents Fear of rejection by others, especially the peer group Difficulty saying no to others; fear of not being liked by peers School Refusal: Symptoms ● Persistent reluctance or refusal to attend school because of a ● ● ● ● ● ● desire to remain at home with parent(s) Marked emotional distress and repeated complaints ● Examples: Crying, regressive behaviors, temper outbursts, pleading with parents(s) not to go to school) Frequent somatic complaints (e.g., headaches, stomachaches, nausea) associated with attending school or in anticipation of school attendance. Excessive clinging or shadowing of parent(s) Frequent negative comments and/or repeated questions about school Low self-esteem and lack of self-confidence that contribute to the fear of attending school and being separated from the parent(s) Verbalization of a fear of failure and anxiety regarding academic achievement accompanying the refusal to attend school School Refusal: Intervention Supports Incrementally expose children to school schedule and situations Identify trigger for school refusal and problem-solve ways to resolve trigger Continual communication with school staff and parents Reward system for attending school Set time to meet with support staff before/after school Attention-Deficit/Hyperactivity Disorder: Symptoms ● Short attention span ● Susceptibility to distraction by extraneous stimuli ● Repeated failure to follow through on instructions or complete school ● ● ● ● ● ● assignments, chores, or job responsibilities in a timely manner Poor organizational skills ● Forgetfulness, inattention to details, and losing things necessary for tasks Hyperactivity ● High energy level, restlessness, difficulty sitting still, or loud/excessive talking. Impulsivity ● Difficulty awaiting his/her turn in group situations, blurting out answers to questions before the questions have been completed, and frequent intrusions into others’ personal business Frequent disruptive, aggressive, or negative attention-seeking behaviors Tendency to engage in careless or potentially dangerous activities Difficulty accepting responsibility for actions, projecting blame for problems onto others, and failing to learn from experience ADHD: Intervention Supports Define and praise appropriate school behavior Ignore inappropriate behavior Remove distracting objects or visuals Visual cues Proximity to teacher Reward systems (Behavior chart, PBIS) Chunk information Organize information (graphic organizers) Sensory/Movement breaks Sensory objects to hold Stretch breaks Accommodations such as a wiggle seat, alternative chair, alternative desk, privacy folder Overview ● There is often comorbidity of symptoms ● There isn’t always a clear cut diagnosis and there can be symptoms that overlap ● Therapeutic techniques can be applied to individual situations ● Consult with school members to determine action plan at school ● If symptoms worsen at home, you may wish to seek individualized assistance through an outside service provider References 1. http://www.nimh.nih.gov/ 2. Shapiro, J., Friedberg, R., & Bardenstein, K. (2006). Child and Adolescent Therapy: Science & Art. 3. Youth Mental Health First Aid USA (2012). Maryland Department of Health and Mental Hygiene, Missouri Dept. of Mental Health, & National Council for Community Behavioral Healthcare Healthguide.org http://kidshealth.org/ http://www.cdc.gov/violenceprevention/pdf/suicid e-datasheet-a.pdf