* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download sabin vaccine report - Sabin Vaccine Institute
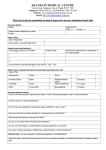
Survey
Document related concepts
Thiomersal controversy wikipedia , lookup
Herd immunity wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Vaccination policy wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Globalization and disease wikipedia , lookup
DNA vaccination wikipedia , lookup
Hepatitis B wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Whooping cough wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Smallpox vaccine wikipedia , lookup
HIV vaccine wikipedia , lookup
Transcript
SABIN VACCINE REPORT the newsletter of the Albert B. Sabin Vaccine Institute at Georgetown University Volume II, Number 2, June 1999 Hepatitis B controversy sparks concern Sabin Vaccine Institute counters anti-vaccine propaganda. 3, 6 Malaria Follow-up Thailand program managers explore future of a malaria vaccine. 3 SPECIAL REPORT: CANCER VACCINES Immunologists develop vaccines to treat cancer. 4, 5 Vaccines combat biological warfare threat Smallpox and Anthrax pose formidable challenges as bioterrorism weapons of choice. 7 Cancer vaccine meeting generates collaborations BY CHARLENE FLASH Thirty-six of the world’s top cancer immunologists, microbiologists, and vaccinologists gathered at the first Walker’s Cay Colloquium on Cancer Vaccines and Immunotherapy to explore the latest research in the molecular immunology of tumor vaccines and to determine how this knowledge can be translated into effective cancer therapies. The Albert B. Sabin Vaccine Institute organized the think tank-style meeting in conjunction with the Lombardi Cancer Center at Georgetown University. The colloquium gathered scientists in fields ranging from statistics to microbiology who specialize in cancer vaccine research and development. The historic setting for the meeting was Walker’s Cay, a small island in the northern Bahamas, where President Nixon was a frequent guest. It was while visiting Walker’s Cay that Nixon decided to make conquering cancer a national priority. The colloquium marked the 28th anniversary of Nixon’s declaColloquium chairs, Drew Pardoll and ration of “war” on Cancer. remarks. James P. Allison, Director of the Cancer Research Laboratory at the Howard Hughes Medical Institute at the University of California Berkeley, and Drew Pardoll of Johns Hopkins University co-chaired the meeting. They set the scientific agenda for the colloquium and oversaw selection of the distinguished participants including John L. Gerin of Georgetown University who proved that hepatitis B vaccine also prevents hepatocellular carcinoma, which affects the liver and is the most common type of cancer in the world. According to Dr. Richard Bucala, head of the medical biochemistry laboratory at the Picower Institute for Medical Research in New York, these research scientists “normally go to meetings with people in their own disciplines, so they rarely get an opportunity to share their ideas and have them constructively challenged by colleagues” who have a different perspective. The unique format of the colloquium was no accident. “We set out to create a meeting that would be very different, to encourage scientists to debate their theories…,” said H. R. Shepherd, chairman of the Sabin Vaccine Institute. The congenial atmosphere and blend of participants served to stimulate a vigorous exchange of ideas and create a sense of collegiality. Dr. Pardoll said the colloquium “stimulated a lot of critical thinking and new ideas about vaccines for cancer.” A. Bennett Jenson, co-developer of a vaccine to prevent human papillomavirus and cervical cancer and a member of the Sabin Vaccine Institute Scientific Advisory Committee, agreed: “It was one of the most intellectually exciting meetings I have ever attended.” Several scientists echoed Dr. Hyam Levitsky of Johns Hopkins University who said, “The intimate setting [promoted] serious exchange of ideas and the establishment of new collaborations.” National Cancer Institute scientist Dr. Suzanne L. Topalian said she left Walker’s Cay with “several new ideas to try in my laboratory.” According to Dr. Carl H. June, Director of Translational Research Programs at the University of Pennsylvania Cancer Center, the Walker’s Cay Colloquium was “one of the best meetings… I have attended in the past fifteen years.” The Sabin Vaccine Institute’s colloquia foster James Allison discuss plenary partnerships between academia, industry and government to stimulate vaccine research and development. Noting author Alexander Benis’ axiom, “None of us is as smart as all of us,” Mr. Shepherd urged participants to consider joining a cancer vaccine consortium. The blueprint for such a partnership is being prepared by Clark McFadden of Dewey Ballantine, LLP, an attorney involved in creating the SEMATECH consortium that revolutionized semiconductor manufacturing in the U.S. A vaccine consortium would encourage ongoing research collaboration and attract more research funding and faster commercialization of new technologies. [See – Government-Industry Partnerships: The Wave of the Future – and the Past, page 2] The Walker’s Cay Colloquium “opened participants’ eyes to the different challenges involved in developing cancer vaccines and will enable them to contribute more to the quest” observed Dr. Pardoll. The colloquium was supported by an unrestricted grant from the Walker’s Cay Corporation. Other co-sponsors included the Richard Nixon Library & Birthplace Foundation and the Sabin Vaccine Institute. v photo by Carol Ruth Shepherd IN THIS ISSUE AIDS vaccine trials offer hope Sabin Vaccine Report Albert B. Sabin Vaccine Institute 58 Pine Street New Canaan, CT 06840 BY ELIZABETH DE LA PAZ “If the 21st century is to be the century of biology, let us make an AIDS vaccine its first great triumph,” President Clinton declared in June 1997. He challenged the United States to develop an AIDS vaccine by 2007. Now, two years later, the question becomes: How close are we to achieving such a goal? There’s no doubt that an HIV vaccine is greatly needed. A study conducted by UNAIDS, the joint United Nations Programme on HIV/AIDS, estimated that 8,500 people are newly infected with HIV every day, and about 5.8 million people worldwide became infected in 1997 alone. At the end of 1997, approximately 30.6 million people were living with the HIV virus. Although retroviral drugs have improved the quality and length of life of HIV-infected people in countries like the United States, no interventions have been available to residents of developing countries, who account for an astonishing 90 percent of new infections. Moreover, the antiviral drugs and therapies cannot be relied on forever, due to drug tolerance and emerging drug-resistant viral strains. The toll that AIDS has taken on the world, through the loss of millions of lives as well as through economic cost, makes finding an HIV vaccine a worldwide public health priority. A safe and effective vaccine would provide protection from HIV infection and eventually end the worldwide epidemic. A vaccine could induce immune responses that attack and destroy any incoming virus and cells that have been infected. If HIV is already well-established in the body, a vaccine might control the replication of the virus and decrease the chance of transmission and disease progression. Various types of vaccines are being used in current HIV vaccine trials. Most of them emphasize the use of the envelope glycoprotein gp160 or gp120 which forms the outer spike projection of the HIV virus. Experiments with live-attenuated vaccines that consist of weakened HIV viruses are also being performed, but not yet on humans for fear that the virus might mutate and become virulent. An advantage to the development of a live-attenuated vaccine is the need for only one immunization, eliminating worries for follow-up for booster shots. Human clinical trials are now under way in the United States and Thailand using recombinant subunit vaccines. This type of vaccine uses pathogen protein derivatives that are purified and combined with vaccine enhancers. Although these vaccines have afforded some protection, the immune response is not very strong. Additional human clinical trials in Uganda are testing vector-type vaccines, using attenuated canarypox viruses to induce HIV-specific immune responses in uninfected people. Other scientists are investigating DNA-type vaccines, in which DNA plasmids encoded with a viral antigen are injected into the muscle of the patient, where they produce HIV proteins that eventually elicit an immune response. The ultimate vaccine Continued on page 6 2 SABIN VACCINE REPORT June 1999 Government-Industry Partnerships: The Wave of the Future - and the Past by Charles Wessner, PhD Charles W. Wessner is the Program Director for Technology and Competitiveness for the National Research Council Board on Science, Technology and Economic Policy. Dr. Wessner directs a project on Government-Industry Partnerships for the Development of New Technologies which directs both U. S. partnerships and international collaboration. Dr. Wessner has served as adviser to the Secretary of Commerce and the Under Secretary of the Technology Administration. SABIN VACCINE REPORT 58 Pine Street New Canaan, CT 06840 phone: 203.972.7907 facsimile: 203.966.4763 email: [email protected] The Albert B. Sabin Vaccine Institute is a non-profit institute dedicated to continuing the work and achieving the vision of Albert B. Sabin: to fully realize the potential of vaccination to prevent disease. Founded in 1994, the Institute strives to prevent disease by promoting the development of new vaccines and delivery systems. Dedicated to Disease Prevention www.sabin.georgetown.edu CHAIRMAN H.R. Shepherd When Americans think of technological innovation, they often visualize a lone inventor. Examples such as Thomas Edison’s light bulb and Alexander Graham Bell’s telephone dominate the view of late-19th-century advances. Today, the garage in Silicon Valley and the university dorm room are the typical settings, and people such as Steve Jobs, Bill Gates, and Michael Dell come to mind. Such images are powerful for a good reason; the relative ease with which an individual can turn an idea into a high-growth company is a unique strength of the U.S. economic system. Less prominent in the popular mind — but equally important to creating new technologies — is the role of government-industry partnerships in stimulating innovation. From the nation’s earliest days, the federal government has frequently played a crucial role in supporting new inventions. For example, in 1842 Congress appropriated $30,000 for Samuel Morse’s telegraph, launching the information economy. In the 1960s, the Department of Defense funded ARPANET, a communications network that linked researchers in universities and government labs. ARPANET evolved into the Internet, which today fuels the burgeoning electronic commerce industry. More recently, the fiercely independent companies of the U.S. semiconductor industry came together to form SEMATECH. From 1988 to 1996, this consortium received half of its $200 million annual budget from the government, and it helped restore U.S. competitiveness. Today, many biotechnology firms and such large biotech companies as Amgen and Genentech can trace their origins to research initially funded by the National Institutes of Health. Government-industry partnerships take many forms. In the Small Business Innovation Research (SBIR) program, a $1.2 billion annual program, government agencies set aside 2.5 percent of their extramural research budgets for R&D grants to small business. Not only do these grants help the government carry out research missions in areas such as public health and defense, but they also accelerate commercialization of innovations from the small business sector. In the Advanced Technology Program (ATP), funded at $220 million per year, the government supplements private-sector funds for developing technologies whose potential benefits broadly accrue to one or more industries. These technologies often cause private investors to hesitate, both because of the technical risk and the diffused nature of the benefits. To advocates of partnerships, these same widely diffused benefits in fact justify public funding because the country as a whole receives the benefits. In an era characterized by rapid technological change, government-industry partnerships are becoming ever more important. One reason is the growing cost and technological complexity of innovations. For instance, the number of circuits on an electronic chip continues to double every 18 to 24 months. But maintaining that pace is expensive — a single fabrication facility for semiconductor chips costs close to $2 billion and has to be retooled every few years. The conversion to the next generation of semiconductor manufacturing (from 200 to 300 mm wafers) will cost the industry $10-20 billion, but larger wafer sizes mean better manufacturing productivity, which is needed to pay for expensive fabrication facilities and R&D. Government support for R&D, through partnerships like SEMATECH and tax policy, has traditionally been an important component to the semiconductor industry’s productivity equation. Similarly, the Human Genome Project (HGP) combines enormous expense — in excess of $2 billion — with incredible complexity as it begins to make exciting medical breakthroughs through genome sequencing. The HGP requires not only scientific breakthroughs but also advances in electronics technology. An important element of the HGP is DNA array technology, in which “gene chips” can quickly gather and analyze DNA sequences, detecting a person’s susceptibility to various diseases or potential reactions to medication. Genometrix, Inc., one company that has developed “gene chip” technology, recently completed a study for the Food and Drug Administration that involved screening the blood of 800 patients for 10,000 genotypes in one week’s time. Without the Genometrix chip, this task would have taken a year. Genometrix developed its technology with the help of an ATP grant. Another reason that partnerships will remain important is global competition. The German government is increasing its support to its biotechnology industry. Japan, notwithstanding its current economic slump, continues to support largescale partnership programs in electronics and other technologies. More generally, the European Union and individual European governments are using partnerships to improve the climate for entrepreneurship. Many markets for high-tech goods tend toward “winner-take-all” outcomes. If other governments can effectively use public funds to support winning partnership programs, they can capture many of the benefits of new, welfare-enhancing, wealth-generating technologies — including jobs, know-how, and economic growth. To succeed, U.S. partnership programs must be appropriate to the technology and the nation’s system. Usually this means they must be industry-led. At the same time, government-supported technologies must be disseminated as widely as possible to ensure the maximum public benefit to taxpayers. We are not certain what technological opportunities we will face in the next century. What we can affirm is that the challenges of today — and tomorrow — will often best be met by industry and government working together. v The Sabin Vaccine Report is published by the Albert B. Sabin Vaccine Institute at Georgetown University. Subscriptions are free. Please direct inquiries to: ALBERT B. SABIN VACCINE INSTITUTE AT GEORGETOWN UNIVERSITY EDITOR Charlene A. Flash WRITERS/STAFF John M. Clymer Elizabeth de la Paz Jane Fox Judith B. Hopkins Gboku Lumbila Robin Netherton Jessica Quinn Erica Seiguer CONTRIBUTORS Valaikanya Plasai, PhD H.R. Shepherd Krongthong Thimasarn, PhD Charles W. Wessner, PhD A scientist who is also a human being cannot rest while knowledge which might be used to reduce suffering sits on the shelf. Albert B. Sabin EXECUTIVE VICE PRESIDENT Edward Neiss MD PhD BOARD OF DIRECTORS Jason S. Berman Zev Braun Kenneth L. Dretchen PhD Robert E. Fuisz MD E. Andrews Grinstead III Jerome Jacobson David J. Meiselman Esq Lewis A. Miller Louis Padovano SJ MD Maj. Gen. Philip K. Russell MD Heloisa Sabin Carol Ruth Shepherd H.R. Shepherd BOARD OF TRUSTEES Ruth Arnon PhD Nancy Gardner Hargrave Joseph L. Melnick PhD Gustav J.V. Nossal MD PhD George C. St. Laurent Jr Andrea Scott Kathryn G. Thompson Donna Twist PhD Stephen G. Valensi Esq James D. Watson PhD Barbara Wilson INTERNATIONAL COUNCIL OF SCIENTIFIC ADVISORS Peter J. Hotez MD PhD Chair Kenneth I. Berns MD PhD Fred Brown PhD FRS Robert M. Chanock MD Stephen N. Chatfield PhD Jonathon M. Fine MD Warren Grundfest MD Ian Furminger PhD Neal A. Halsey MD Maurice R. Hilleman PhD Brian R. Murphy MD Erling Norrby MD PhD MTC Wade P. Parks MD PhD Michael Sela PhD James D. Watson PhD SCIE IN MEMORIAM Mary Lou Clements-Mann MD MPH SCIENTIFIC ADVISORY COMMITTEE Herbert B. Herscowitz PhD Chair Joseph A. Bellanti MD John L. Gerin PhD A. Bennett Jenson MD C. Richard Schlegel MD PhD Joseph G. Timpone Jr MD BOARD OF ADVISORS Mary Alderman Francis E. Andre MD John V. Bennett MD Barry Bloom PhD Betty F. Bumpers Francis Cano PhD Ciro A. de Quadros MD MPH Phyllis Freeman Esq Bruce G. Gellin MD MPH Lance K. Gordon PhD Scott B. Halstead MD Samuel L. Katz MD Stanley M. Lemon MD Sister Collette Mahoney Frederick C. Robbins MD Harvery S. Sadow PhD Ronald J. Saldarini PhD Donald S. Shepard PhD Arnold Stang Patricia Thomas SABIN VACCINE REPORT June 1999 3 Thailand program managers describe challenges of malaria control BY KRONGTHONG T HIMASARN, MD, PHD AND VALAIKANYA PLASAI, DR. PH Although the concept of global eradication of malaria achieved considerable success in reducing morbidity and mortality in certain geographical regions, the eradication campaign has jeopardized the malaria control effort by expending cheap, reliable and relatively safe tools such as DDT and chloroquine which unfortunately gave rise to the insurmountable problems of vector resistance to insecticide and drug resistant malaria parasites. Today, some 50 years since the inception of the malaria eradication effort, malaria is still as rampant as ever, if not worse among developing countries. In Africa alone, an incredible one million deaths per year are reportedly due to malaria. Most of the deaths occurred among children under five: an estimate of one death every 30 seconds. Five decades and millions of dollars after the launch of malaria eradication, the world is still suffering from malaria. Development of malaria control interventions has not been able to keep up with emergence of malaria vector and “Malaria... poses the parasite resistance, and has been outsmarted by malaria paragreatest economic sites and vectors. Advanced knowledge and new technology burden of all tropical available to date such as DNA vaccine technology, new adjudiseases.” vants, and various vaccine delivery systems, have yet to render a new vaccine. Although there are several candidate vaccines based on various antigens at different parasitological stages, none has ever reached an operational utilization level. The SPF66 vaccine, which lit up our hopes in the early 1990s, turned out to take much longer than expected to develop to an operational stage. Mefloquine, the then-promising new antimalarial drug registered for operational use in Southeast Asia in 1985, took a few years to develop, but parasite resistance emerged swiftly in 5-7 years, even before countries in other regions had heard of the drug. Many new insecticides discovered in the last few decades are now facing that same widespread problem of vector resistance. Effective interventions have always been out-paced by emergence of resistance. Those who have been involved in malaria control have learned to accept the fact that controlling malaria is a complex problem. In Southeast Asia, South and Central America, the Middle East and Eastern Europe where 20% of malaria cases occur, malaria epidemiology varies greatly. Problems of insecticide-resistant vectors, drug-resistant parasites, epidemics due to the unstable political situation and massive population movement are all interwoven. They hinder the already weakened efforts of malaria prevention and control. Currently, the situation has become even worse due to the recent economic crisis in Southeast Asia. It seems that there is no light at the end of the tunnel when it comes to planning for malaria control in these areas. Among new tools being developed, a malaria vaccine seems to be the intervention everyone awaits. While we are “waiting for the vaccine”, there are lessons we must learn from past experience. We would certainly hope not to exploit and expend malaria vaccines, once we have them, the way we did other malaria control tools. We must not be naïve and hope that the vaccine is a magic bullet that will solve all problems. Once it becomes available, we must utilize the vaccine wisely, perhaps in combination with other existing measures. Judicious and effective use of the vaccine will ensure that we will be using it for a long time. There are four issues to consider when designing an anti-malaria vaccine. First, the attributes of a malaria vaccine must differ depending on malaria epidemiological features of target regions. Blood-stage malaria vaccines would be ideal for reducing mortality among children under five and pregnant women living in continuous and intense malaria transmission areas such as tropical Africa. In these areas, pre-erythrocytic and transmission blocking vaccines would not be appropriate. These two types of vaccine, on the other hand, would be ideal for non-immune, or semi-immune individuals who remain in partially inhibited malaria transmission areas for short period, if the length of protection is long enough. For example, migrant workers and travelers from non-endemic areas working in, or visiting, intense malaria transmission regions would benefit most from pre-erythrocytic and transmission blocking vaccines. If such vaccines gave protection for a few months, we could observe their impact on the disease incidence. Lastly, anti-TNF vaccines that will prevent malaria disease are an exciting new hope, but we doubt the feasibility, hence their use. We must not aim to produce a ”one-size-fits-all” vaccine for various types of malaria epidemiological paradigms. The next issue to consider when designing a vaccine is its cost: both the cost of the vaccine itself and the cost of the vaccine delivery system. Malaria is a major infectious disease and poses the greatest economic burden of all tropical diseases. Cost-effectiveness is vital to success. A malaria vaccine, once available, needs a delivery system that is not only costeffective, but also inexpensive, simple and easy to maintain. Malaria is endemic in remote areas characterized by lack of health and other facilities. Even chloroquine, the most simple, efficacious, and inexpensive antimalarial drug, does not have any impact on malaria morbidity and mortality in remote areas simply because it cannot reach the target population. The most efficacious vaccine will not bring about desired impact on a target population if it has a complicated and costly delivery system, such as the cold-chain. Thirdly, a malaria vaccine must not disturb, compete or interfere with existing public health systems. The Expanded Programme on Immunization (EPI) program, for example, has established itself firmly in the community. It would be ideal if a malaria vaccine could become part of the existing EPI system. Lastly, a malaria vaccine must take into consideration the culture in which it will be used. Desperate for relief, some people will take advantage of any available antimalarial tools or technologies. A clear example: the use of antimalarial drugs among non-qualified healers. Without understanding social, cultural, and economic forces underpinning malaria transmission and the use of antimalarials by the community, any malaria vaccine could be subject to misuse by the community. A thorough understanding of such factors is necessary to ensure success implementing a malaria vaccine. In 1992 the World Health Organization launched the Global Malaria Control Strategy, a new effort to curb malaria. Abandoning the concept of malaria eradication altogether, the Global Malaria Control Strategy focuses on malaria control, and it recognizes malaria ecology and epidemiology as the foundation of planning for a malaria control effort. It calls for collaborations among private and public health authorities and the affected communities. Therefore, in order to be successful, the Global Malaria Control Strategy calls for strong commitment, full support from all parties, and a greater coordinated effort from both technical and managerial parties. There will be a tendency to search for a “silver bullet” to do away with malaria. We must resist that urge. We must embrace the lessons we have learned during the global eradication campaign period and strive not to repeat mistakes. Today, malaria is in the limelight again with the announcement of the Roll Back Malaria initiative by Dr. Gro Harlem Brundtland, the newly installed Director General of the World Health Organization. The search for a malaria vaccine must not be the search for short cuts to save time and effort in controlling malaria. The battle against malaria is a long process, in which small, incremental but sustainable gains are desirable. Broad sweep and general interventions to be used uniformly in all places must not be encouraged. “Tailor made” malaria control interventions appropriate to each malaria paradigm, however, are the key to success for sustainable malaria intervention. Desirable malaria vaccines used judiciously and appropriately must also follow this logic. v Krongthong Thimasarn, MD, MPH is the director of the Malaria Control Programme and Valaikanya Plasai, Dr. PH is the director of the Malaria Division of Thailand. Editor’s Note: The views expressed are not necessarily those of the Sabin Vaccine Institute, but reflect the opinions of the authors. [For more on malaria vaccines see Volume II, Number 1, March 1999.] France’s medical meddling could cost millions their lives BY H.R. SHEPHERD Some of the world’s top thinkers are debating what to do about smallpox, a disease that ravaged humanity for at least 12,000 years. It struck the mighty and the powerless, from Marcus Aurelius to Ali Maow Maalin, a cook in Somalia who in 1977 was the last person to catch smallpox naturally. The debate now is what to do with the remnants of the virus, whether to destroy them or keep them in secure laboratories for further study. The breathtaking part is that we’re in a position to be holding such a discussion. Thanks to vaccines, smallpox is all but extinct. We’re lucky to have had a 200-year head start on wiping out smallpox because today political road blocks would impede use of the vaccine. Take a look at the status of the vaccine for hepatitis B, one of the most prevalent and deadly infectious diseases in the world. Over 300 million people are chronically infected with hepatitis B, the leading cause of liver cancer. According to the World Health Organization (WHO), hepatitis B leads to more than 1 million deaths a year. Last October, the French government suspended routine hepatitis B immunization of school children because of anecdotal reports that the vaccine caused multiple sclerosis. The French took action without any scientific evidence to back them up. Indeed, since this vaccine became available in 1982, more than 1 billion doses have been administered worldwide. It is 95 percent effective in preventing infection. In countries where 8 percent to 15 percent of children were chronic carriers, vaccination has cut the rate to less than 1 percent. The WHO calls hepatitis B vaccine “one of the safest” vaccines available. Never mind all that. The French government had something more pressing to worry about: politics. Some activists intent on curtailing vaccinations latched onto a combustible accusation — the alleged hepatitis B vaccine- MS connection — and they demanded action. The French government hastily bowed to their demands. In contrast, the WHO turned to science. If the vaccine caused MS, somewhere in a billion doses, something ought to turn up. But an exhaustive search came up empty. The WHO reiterated the vaccine’s safety. This message was reinforced by the Multiple Sclerosis Society of Canada, which cited “the lack of any scientific evidence” of a link between hepatitis B vaccine an d MS. Ironically, the French National Drug Surveillance Committee, a drug safety agency, found lower frequency of neurological diseases, including MS, among those vaccinated against hepatitis B than in the population at large. The international health community is concerned about the French action because it could erode confidence in vaccines. France’s announcement resulted in a 20 percent drop in hepatitis B immunization rates. Activists are trying to raise similar concerns in the United States. They have launched Internet sites that attack universal vaccination, a principle widely advocated by public health experts and medical practitioners. A recent television news magazine reported that since 1991, when the Centers for Disease Control and Prevention endorsed hepatitis B vaccination of infants, 274 deaths have been reported. For most, the cause of death was listed as sudden infant death syndrome (SIDS). In contrast, 140,000 unvaccinated Americans become chronically infected with hepatitis B each year. Does this mean some people might be considered expendable for the common good? No, of course not. It means we cannot precisely forecast the future. We don’t know who is going to catch a disease, or who may have a reaction to a vaccine, or who will get sick from something completely unrelated right after getting vaccinated. But we do know this: Vaccination prevents millions of deaths every year. Thanks to vaccines, diseases that once struck fear in every town in every nation have been eradicated in every corner of the world (smallpox) or nearly eradicated (polio). Without universal vaccination, we would not be arguing over whether to preserve the last remnants of the smallpox virus. Instead, in the case of smallpox, we’d be digging graves — about 40 million of them in the last 20 years by the WHO’s reckoning. v H. R. Shepherd is chairman of the Albert B. Sabin Vaccine Institute at Georgetown University. 4 SABIN VACCINE REPORT June 1999 Cancer Vaccines activate immune response Vaccines are most often considered solely prophylactic, however, cancer vaccines may be used to treat existing tumors as well. An Historical Note… William Coley, a surgeon in New York during the late 19th century, vaccinated patients against bacterial infections using what have been coined as “Coley’s toxins.” Coley noticed that immune response to certain bacterial infections seemed to create a general systemic response that inhibits tumor development and sends cancers such as soft-tissue sarcoma and lymphomas into remission. Decades later, scientists revisit these discoveries trying to develop vaccines to activate the immune system and both prevent and treat cancer. Photo by Carol Ruth Shepherd Bacillus Calmette Guerin (BCG) and Corynebacterium parvum are adjuvants, additives that enhance activity, that may be added to antigen-based vaccines. Antigenics, L.L.C. uses heat shock proteins (HSPs), the body’s natural adjuvants, to modulate the immune system to respond against multiple antigens in a given cell in vaccine trials against renal cell carcinoma, melanoma and gastric and colorectal cancer. Vaccines may be composed of whole tumor cells that Cancer defies medical sensibility as our own cells betray us, senting cells), or impede the generation of tolerance and block- have been irradiated so they can no longer reproduce or lygrowing uncontrollably and developing into tumors. ing inhibitory pathways such as the CTLA-4 pathway so an sates, i.e. particles remaining after a cell is destroyed. Tumor Damaged genes within the human genome cause defects appropriate immune response can take place. An example of vaccines may also be composed of synthetic tumor antigens. leading to tumor development. Tumors flourish when activating T-cells is seen in AVAX ovarian and malignant mela- Tumor cells may be genetically modified to emit proteins growth-controlling genes such as oncogenes are activated noma cancer vaccine trials where a process known as that stimulate an immune response, or they may be adulterand tumor-suppressor genes ated with a gene that will are deactivated. Generally, cause emission of a foreign the human immune system antigen which when exwould respond to antigen pressed will elicit an immune molecular markers on the response. The ras oncogene tumor surface by activating is a potential tumor antigen antibodies or immune cells as is her-2/neu, another proagainst them, however, in the tein that encourages tumor case of cancer, tumor growth. antigens are tolerated by the These techniques are immune system. The meant to yield a T-cell immune system may tolerate response that is antigenantigens rather than specific. combatting them if it is not Peptides that mimic activated properly by the activity of certain antisurrounding circumstances (Top row)Andrews Grinstead, Stan Riddell, Suzanne Topalian, Nicholas Restifo, Jeffrey Schlom, Richard Bucala, Hyam Levitsky, Victor gens may be synthesized. For such as damage to Engelhard, Allesandro Sette, Linda Sherman, Sharon Hammer, John Clymer, (Middle row) Ronald Germain, Richard Simon, Eli Gilboa, example, a person’s antigens Edward Neiss, Charlene Flash, Philip Russell, A. Bennett Jenson, Carl June, John Gerin, and Ephriam Fuchs (Bottom row) H. R. Shepherd, surrounding tissue or Steven Piantadosi, Lee Nadler, Philip Greenberg, Marc Lippman, James Allison, Drew Pardoll, Jay Berzofsky, Ralph Reisfeld, Larry Kwak, may be cloned, manipulated inflammation or if the Mitchell Cairo, David Liebowitz, Herbert Herscowitz, Kenneth Meehan, and Tom Gajewski gather outside conference room at Walker’s Cay so that the immune system is Cancer Vaccine and Immunotherapy Colloquium. appropriate T-cell cobetter able to respond, or stimullatory molecules, such simply multiplied and then as B7, are not present. ‘haptenization” is applied to an individual’s tumor cells; reintroduced to the patient. Compilations of multiple tuAccording to Dr. Drew Pardoll of Johns Hopkins Uni- haptenization enables the patient’s immune system to recog- mor antigens have been attempted as well to create a versity, cancer inhibits a normal immune response because nize the cells as foreign entities and attack. generalizable tumor antigen preparation. tumors prevent appropriate antigen expression, generating Although helping T-cells respond is arguably the Robert Weinberg in his book, One Renegade Cell, inhibitory molecules such as tumor necrosis factor B and fas most common tactic for tumor vaccine development, there predicts, “The big decreases in cancer deaths will … come ligand, or impeding the cellular machinery that delivers for- are various other techniques. Some involve manipulation from preventing disease rather than discovering new eign proteins to T-cells for action (the major histocompatibility of antigen presenting cells such as dendritic cells and cures.” (Weinberg, 153) Tumor vaccines will respond to complex (MHC)) and processes antigens. fibrocytes [See To Present or Not to Present, page 5], regulatory both needs by preventing as well as treating cancer. The goal therefore is for tumor vaccines to stimulate agents of the immune system, or vectors that express mol- Although tumor vaccines may not replace current the immune system to recognize tumor antigens. They ecules such as cytokines, growth factors, and tumor antigens. therapies, they have been and may more effectively be must activate T-cells normally insensitive to tumor anti- Retroviral vectors may be used to insert cytokine genes into used in the future to encourage regression of existing gens, stimulate or augment presentation of antigens by white blood cells from cancer patients to elicit immune re- tumors and to inhibit the appearance of future micromanipulation of the antigen itself (or of the antigen pre- sponse against tumor cells. tumors. v Gerin, Jenson and Schlegel prevent virus-based cancers Photo by Carol Ruth Shepherd Initially, tumor vaccines were only considered for strains of cancer associated with viral infections. If a vaccine could eliminate the causal virus, scientists reasoned, then the cancer would not take hold. Although not all cancers are associated with a specific virus, the two most common cancers — hepatocellular carcinoma (liver cancer) and cervical cancer — are. Hepatoma is associated with the hepatitis B virus (HBV), and cervical cancer with the human papillomavirus (HPV). Other viruses associated with cancer include Epstein-Barr virus (EBV), which has been linked to Burkitt’s lym- Hepatitis B and liver cancer expert, John Gerin arrives at phoma and nasopharyngeal carcinoma, and certain retroviruses — such as HTLV-1, which is associated with a form of lymphoma. Until the path by which cancer develops becomes clear, a vaccine against the causative element is the best approach for preventing virus-associated cancer; eliminating the harmful effects of the offending microorganism reduces the risk of cancer. Unlike many other cancer vaccines, which strive to provide therapies for cancer, vaccines for virus-associated cancers have been designed primarily to be preventive; they prevent chronic infection with the virus, not the actual development of the tumor. However, current research is exploring the therapeutic applications of this type of vaccine for treatment of the viral infection itself. Hepatitis B and liver cancer In the 1970’s, John L. Gerin, now the director of the Division of Molecular Virology in the Department of Microbiology and Immunology at Georgetown University and a scientific advisor to the Sabin Vaccine Institute, developed what is known as the “NIH Vaccine” against hepatitis B. At that time, infant trials in Beijing demonstrated that the hepatitis B vaccine was very effective in preventing HBV. Little did they know that it would soon be determined that hepatitis B caused liver cancer. Years later, Gerin’s animal model work using the woodchuck and human studies in Taiwan would show a strong indication of the preventive benefits of hepatitis B vaccine for liver cancer. Above and beyond the 40 percent lifetime risk of liver cancer associated with hepatitis B, HBV also causes chronic liver disease, a progressive illness that becomes increasingly severe with time, as well as cirrhosis of the liver. Currently, the hepa- “... the hepatitis B titis B vaccine is the only vaccine is the only vaccine that has vaccine that has been definitively proven to prevent cancer. Still, the in- been definitively cubation period proven to prevent for development of HBV cancer.” into chronic liver cancer can be anywhere from 20 to 50 years, creating challenges for those who seek to do human clinical trials. Current research in Gerin’s lab involves a therapeutic approach; antivirals suppress a host’s HBV viral load, and subsequent vaccination triggers an immune response that enables the host to eradicate the virus. Merck & Co., Inc. and SmithKline Beecham markets hepatitis B vaccines; the one Gerin’s lab is working on is more experimental in nature. [See, Sabin counters vaccine campaign, page 8] Humanpapillomavirus and cervical cancer Cervical cancer attacks 500,000 people each year and causes 300,000 deaths. Although Pap smear screening and treatment make a big difference, the death toll is still staggering. Cervical cancer has been directly linked to the human papillomavirus (HPV). This virus causes lesions in the cervix that, over a period of up to 20 years, may develop into cancerous tumors. Aside from being directly associated with cervical cancer, HPV may also play a causative role in cancers of the vulva, vagina, penis, anus, head, and neck. Alfred Bennett Jenson, a member of the Sabin Vaccine Institute Advisory Committee and a professor at Georgetown University, and Richard Schlegel of Georgetown University have developed a vaccine against HPV and cervical cancer. The vaccine is a genetically engineered virus-like particle based on the major protein of the virus’s capsid coat. Because these particles contain no DNA, they are not infectious and cannot cause cancer. The vaccine has been licensed to MedImmune which is jointly developing it with Smith Kline Beecham. Currently the Sabin Vaccine Institute is funding research by the lab of Arthur Weissenger at North Carolina State University to produce Jenson’s papillomavirus vaccine in transgenic tobacco plants. This technology will enable inexpensive production of the vaccine in large quantities. v SABIN VACCINE REPORT June 1999 5 To present or not to present Fibrocytes and dendritic cells deliver antigen for immune attack photo by Charlene Flash Scientists have appreciated for many years that a patient’s proteins that stimulate the immune response into the tumor immune system can be activated against a variety of differ- cells, or by-passing normal processing pathways by loading ent tumors but that the immune response may not be suf- empty major histocompatibility complex (MHC) molecules ficient to actually destroy the cancer. Recently, an on antigen-presenting cells. Twenty-five years ago, Ralph Steinman and Zanvil understanding as to why this might occur has spurred new C o h e n interest in the reported that development dendritic cells of an immucan act as nological apantigenproach to the presenting cells treatment that can initiate and/or prei m m u n e vention of responses in cancer. One white blood reason for the cells, known as lack of an eft-cells, that are fective imresponsible for m u n e cell-mediated response cytotoxicity. against a tu- Antigen presentation proponents, Herbert Herscowitz and Richard Bucala greet each other at According to mor is that Walker’s Cay as Institute chairman, H. R. Shepherd, and Bennett Jenson look on. Francisco tumors express self-antigens to which the patient is immunologically Bracho of the Lombardi Cancer Center at Georgetown tolerant, that is, the patient does not respond to his or her University, dendritic cells “…capture antigen in the periphery, own antigens. The question then becomes, how does one get migrate to the lymphoid areas, and present the antigen in the around the problem of self-tolerance. One approach is to context of major histocompatibility complexes along with increase the level of antigen presentation, the process that co-stimulatory molecules.” In November of 1998, the Sabin Vaccine Institute initiates an immune response. Recently, some cancer vaccines have attempted to target and the Immunex Corporation hosted a mini-symposium at antigens that can be recognized by the immune system to Georgetown University on the role of dendritic cells in the appropriate antigen-presenting cells. This can be immunology. Michael Lotze of the University of Pittsburgh accomplished in a number of ways including: adjusting the Comprehensive Cancer Center presented data demonstrating adjuvant given together with the tumor antigen, transducing tumor regression in cancer patients treated with dendritic or inserting specific genes such as GM-CSF that encode cells pulsed with a tumor-derived synthetic peptide. Patients in his clinical trials were also less susceptible to future tumor development. Synthetic peptides, proteins, DNA, tumor lysates, or apoptotic cells serve as a source of tumor antigen for dendritic cells. Alternatively dendritic cells can be introduced to the intact tumor itself. Dendritic cells are found in all tissues except the brain and can be cultured from a patient’s blood and then “activated” by exposure to an offending protein. When the “activated” dendritic cells are reintroduced into the patient the immune system is better able to recognize the offending antigen and attacks. Her-2/neu, which is expressed on a number of human tumors including human breast cancer for example, is a tumor-associated antigen that is currently being targeted for immunotherapy. Vaccines using dendritic cells also show promise against prostate cancer, lymphoma and malignant melanoma. The new antigen-presenting cell The fibrocyte is a recently-described type of circulating cell, a leukocyte, that was discovered only five years ago at the Picower Institute for Medical Research in New York. Like dendritic cells, fibrocytes can play an active role in antigen presentation. These potent antigen-presenting cells are easy to isolate and to expand. Fibrocytes can be activated by exposure to a particular patient’s cancer antigens by exposure to tumor tissue in the lab, fusion with tumor cells, or via gene therapy. Researchers at the Picower Institute have carried out extensive research on fibrocytes. Currently Richard Bucala, Director of the Medical Biochemistry Lab at the Picower Institute, is collaborating with Cytokine Networks Inc. to explore fibrocytes as a cancer therapy. According to Bucala, antigen-presenting cells such as the fibrocyte “could yield excellent results in the development of tumor vaccines.” v Tissue-specific cancer vaccines offer hope Restifo, Allison find pigment loss coincides with tumor regression Cancer immunologists take advantage of the tenuous balance between cancer immunity and autoimmunity, attack of one’s own cells by the immune system. Many cancers, such as melanoma, prostate cancer, breast cancer and ovarian cancer occur in tissues that if lost or removed would not compromise survival. Vaccine therapies that successfully attack a patient’s tumors may also attack the patient’s cells, “...antigens found causing disorders such as on the surface of a vitiligo. (An autoimmune skin disorder in which tumor may not be patches of skin lose pigthe foreign body ment.) Relevant tissuesome may specific antigens envision...” harvested from the “dispensable” tissues of the skin, breast, ovaries, or penis may successfully act as tumorspecific antigens in tumor vaccines to elicit an immune response against tumors. [See Cancer vaccines activate immune response, page 4] Two examples of this technique were discussed during the Walker’s Cay Colloquium on Cancer Vaccines and Cancer Immunotherapy. [See cover story, Colloquium generates collaborations.] James Allison, director of the Cancer Research Laboratory at the Howard Hughes Medical Institute at the University of California Berkeley, found that our immune system’s T-cells need a signal supplementary to the antigen itself (co-stimulatory signal) in order to recognize and subsequently attack tumors. The CD28 co-stimulatory receptor on the surface of T-cells needs stimulation by a substance known as B7, the ligand that transmits signals to antigen presenting cells. Because tumor antigens don’t of themselves give an appropriate signal to the immune system, antigen presentation gains importance. [See To present or not to present] Vaccination techniques with antigens containing B7 could be used to “jump start” the immune system. Allison found that he could improve the immune system’s response to antigens beyond causing an interaction between CD28 and B7. Allison’s researchers found a substance homologue having a different function to CD28 called CTLA-4. CTLA-4 hinders the interaction between B7 and CD28. If antibodies are used to block the activities of CTLA-4, one can obtain much better results in the attack of tumors by T-cells. In fact tumors treated with a “CTLA-4 blockade” and with vaccines expressing the B7 necessary to bind the antigen presenting cell receptor CD28, regress. Allison’s lab combines an irradiated cell vaccine with the CTLA-4 blockade. (The blockade acts as an adjuvant for a GM-CSF tumor cell vaccine.) The trade-off is vitiligo. Vitiligo is an autoimmune disorder in which T-cells kill normal melanin-producing cells (melanocytes). This proves a theory held among immunologists that tumor antigens are more “self ” than “foreign.” Researchers in Allison’s lab are now applying the CTLA-4 blockade and co-stimulation techniques to prostate cancer. Nicholas Restifo, M.D., of the National Cancer Institute is also working with tissue-specific cancer vaccines. Restifo treats humans with the growth factor interleukin-2 (IL-2) to enhance the immune system’s response to cancer. He noticed that some of his patients, developing vitiligo, lost pigment in patches of their skin. This occurred because the cancer treatment induced an immune response against the patient’s own cells. Researchers in Restifo’s group created a panel of recombinant vaccinia viruses that encoded the mouse homologues (versions) of human melanoma associated antigens. They found that vaccines containing tyrosinase related protein-one (TRP-1) triggered the anti-tumor effects as well as the vitiligo. TRP-1 is an enzyme that helps in the production of eumelanin. Eumelanin is responsible for giving the skin, as well as malignant melanoma cells their dark color. Currently Restifo, together with researchers at the NCI surgery branch, collaborate with Therion Biologics Corporation of Cambridge, Massachusetts to test the hypothesis that autoimmune disease is linked with tumor destruction in humans. Tissue-specific vaccines concentrate on particular tissues for immune attack and as a result yield fewer negative side effects. While other researchers seek out tumor-specific antigens to be used in vaccines, researchers exploring tissuespecific vaccines find that the antigens found on the surface of a tumor may not be the foreign body some may envision. Radiation therapy and surgical procedures provide localized therapy for tumors. Tissue-specific vaccine therapy yields an overall or systemic response, especially useful in that cancerous tumors often form satellite microtumors known as metastases that are not readily combated by localized treatment. v This report on cancer vaccine research was written by Charlene Flash, editor of the Sabin Vaccine Report and research fellow at the Sabin Vaccine Institute. Special thanks to James Allison, Herbert Herscowitz, Nicholas Restifo, Drew Pardoll, John Gerin, and A. Bennett Jenson for their assistance with this feature. Cancer vaccine research in phase-III trials Brand/Code Indication Company OncoVax-CL M-Vax GMK Vaccine OVAREX BEC2 Lung Colorectal Cancer Malignant Melanoma Malignant Melanoma Ovarian Cancer Small cell lung cancer Bionetics BMS Avax Technologies Biomira ImClone System source: Datamonitor, 1998 6 SABIN VACCINE REPORT June 1999 Conference shows hidden costs associated with needle and syringe BY CHARLENE FLASH According to John Lloyd of the World Health Organization (WHO), more than 12 billion skin injections are given each year. Nearly all of these use needles and syringes. Although these injections often save lives or prevent disease, the conventional needle-and-syringe method of delivery poses substantial problems. The strongest arguments for finding alternatives to needle-and-syringe delivery are the frequency of needle“Improper handling stick accidents, which can can cause injections transmit disease from pato carry unintended tient to provider. Also, each injection exposes the padisease.” tient, health professionals, auxiliary staff, and the community to sharps waste and contaminated products. Improper handling can cause injections to carry unintended disease: Offering a conservative estimate, Lloyd says that 30 percent of all injections are not sterilely administered, and in 11 out of 14 developing nations, 50 percent of injections pose the risk of transmitting hepatitis B and C, HIV, ebola, or lassa virus. These issues were among those raised at the Conference on Needle-free Injection Technology, held March 31 through April 1 in Bethesda, Md., on the heels of the National Foundation for Infectious Diseases Second Annual Conference. Sponsors of the Needle-Free Conference were the Centers for Disease Control and Prevention (CDC), the U.S. Agency for International Development (USAID), the World Health Organization (WHO), the Program for Appropriate Technology in Health (PATH), and the Association of Needle-free Injection Manufacturers (ANFIM). The conference enabled participants from both the public and private sectors — including representatives of public health agencies, nonprofit organizations, and manufacturers of needle-free injectors — to discuss the status and future of needle-free injection technology. Speakers presented cost-benefit analyses and examined the effectiveness of using needle-free injection to overcome the Aids trials Continued from page 1 would be one that would elicit simultaneous immune responses by B lymphocytes (humoral immunity) and T lymphocytes (cell-mediated immunity). The AIDS vaccine candidate farthest along in clinical trials is VaxGen’s AIDSVAX, which uses recombinant gp120 envelope antigens and an aluminum adjuvant that enhances immune response. This vaccine has already proven to stimulate an immune response and to be safe for use in humans. Now it is in Phase III clinical trials to test how well it fights off HIV infection, to determine side effects, and to see if prior immunization decreases viral progression in the blood and reduces viral load. AIDSVAX is being tested in the United States and began trials in Thailand in February against HIV strains found in Asia. The Thailand trials mark the first time that an HIV vaccine is being tested for efficacy outside the United States. Although many people are excited to see an HIVpreventive vaccine reach Phase III trials, many doubt that AIDSVAX will be effective, since it is not made with a live-attenuated virus. Such concern is only one of several challenges that must be faced in the development of a successful vaccine. Jeffrey P. Kahn, director of the Center for Bioethics at the University of Minnesota, worries that testing the vaccines in humans could lead study subjects to engage in high-risk behavior in the belief they are safe from contracting the HIV virus. Another concern, Kahn notes, is that any true test of the efficacy of a vaccine must involve exposing individuals to the virus. Other recognized challenges in finding an effective vaccine against HIV are the variations among strains of the virus and the complexity of transmission of HIV. Despite these challenges, hope remains for developing an HIV vaccine. Whether the vaccines currently being tested will be the long-awaited answer to the AIDS epidemic is still not known. But collaborative efforts of both industrialized and developing countries will increase the likelihood of finding a safe, efficient, and cost-effective measure to protect people around the world from the HIV virus. v Elizabeth de la Paz is a graduate student at Georgetown’s School of Nursing. drawbacks of needle-and-syringe administration. They also addressed the use of needle-free injection as an alternative delivery system for insulin and other medications as well as vaccines. Given the chance to communicate with representatives of the commercial sector, public health proponents encouraged manufacturers to accelerate the development of needle-free injection technology. Participants also offered recommendations for improving delivery systems. Steve Landry of USAID, stressed the importance of “increased partnership between the public sector and commercial groups.” Meanwhile, manufacturers must consider ergonomic challenges, performance standards, and cost. The few million syringes purchased by WHO for emergency use do not create enough economic incentive for manufacturers to invest in developing needle-free technology. Organizations like UNICEF have the purchasing power to create incentive, but before they as a public health organization can “... public health make a substantive commitproponents ment, the private sector needs to invest in getting the encouraged technology up to proper manufacturers to standards. Todd Calendar accelerate of Genesis Medical Techthe development of nologies spoke up for manufacturers, stating needle-free injection that government support technology.” would create a profit motive for the private sector to consider a greater investment. According to Bruce Weniger, PhD of CDC, the U.S. government spent $600 million in 1998 to buy CDC discount-price contracts from the vaccine manufacturers for vaccines used in childhood immunizations. While needle-free technology poses far less of a contamination risk than conventional methods, it is not completely risk-free. Experiments done by Ram Abuknesha at Kings College in London showed that even if the nozzle of a needle-free delivery device did not contact the skin, at times there was still contamination evident. (Studies have shown that possibly as little as 10 picoliters may transmit hepatitis B.) In response to this challenge, compliancy measures were developed in which the head of the nozzle was wiped off. Nevertheless, enforcing compliant usage is difficult. Colonel Charles Hoke, Director of the Infectious Disease Division of the U.S. Army Medical Research and Material Command, noted that there is definitely a need for a new delivery device, but suggested that advances in needle-free injection technology seem to have slowed in recent years. Needle-free devices are being developed and or manufactured by American Jet Injector, Inc., Bioject, Inc., Equidyne Systems, Inc., National Medical Products, Inc., and PowderJect, Inc, among others. . Various types of devices were presented, each posing different advantages — and different concerns. A standardized design, according to Dr. Weniger, would create a larger market that ought to benefit all companies; the manufacturer that initially chose to pursue standardization would incur all the associated risk and cost, but would reap great benefit. Another design possibility involves simultaneous injections with multiple cartridges. Needle-free injections would minimize occupational risks, disease transmission, and reuse problems created by improper use of syringes and needles. Donatus Enkwueme, PhD Bruce Weniger, PhD and Robert Chen, PhDof the National Immunization Program of the Centers for Disease Control spearheaded a study of the hidden costs of needles and syringes in Africa and concluded that needles and syringes “carry a much greater risk and cost burden than other vaccine delivery technologies that may cost more to purchase or to maintain.” When one considers the cost of treating someone who contracts hepatitis B from a needle-stick injury, the benefits of developing needle-free methods of delivery become more appealing. The use and development of alternative delivery systems will revolutionize administration techniques for vaccines and other medicaments, according to Julia Mendez, MD and Joseph Bellanti, MD of the Georgetown Immunology Center. v Special thanks to Bruce Weniger, PhD, Julia Mendez, MD, and Joseph A. Bellanti, MD. Sabin counters anti-vaccine campaign B Y JOHN M. C LYMER A concerted public relations campaign by anti-vaccine activists is gaining media coverage and spawning legislation that would weaken immunization programs in several states. The Sabin Vaccine Institute and several other groups and agencies that protect public health are countering this campaign. The campaign led by the National Vaccine Information Center is intended to undermine public confidence in vaccines. Activists allege causal links between vaccines and various diseases such as multiple sclerosis, diabetes and autism. ABC’s “20/20” and numerous newspapers have reported the activists’ charge that hepatitis B vaccine may sometimes cause multiple sclerosis. Despite overwhelming evidence disproving the allegation, some media afford the misinformation as much time or space as they give to public health experts who refute it. The World Health Organization, Centers for Disease Control and the National Multiple Sclerosis Society have studied the allegation and found no evidence to support it. They have issued statements affirming the safety of hepatitis B vaccines and urging the public to take advantage of the vaccines to gain protection against this highly infectious form of liver disease. But even as medical and public health experts have disproved the alleged vaccine-MS link, NVIC and its allies have politicians’ attention. In Washington last month a “Hepatitis B is 100 House subcommittee held a times more hearing on “Hepatitis B Vaccontagious than cine: Helping or Hurting HIV.” Public Health.” Subcommittee Chairman John Mica (R-Fla.) publicly acknowledged NVIC’s role in staging the hearing. Several state legislatures considered bills during their 1999 sessions to suspend hepatitis B vaccination requirements and measures that would reduce immunization rates. Illinois, Indiana, Louisiana and Ohio were among the states where such proposals were debated. The Sabin Vaccine Institute submitted testimony to the congressional hearing and wrote state lawmakers to give them the facts about the hepatitis B vaccine and the importance of mass immunization to public and individual health. Newspapers published Institute Chairman H. R. Shepherd’s op-ed article containing the same message. [See France’s medical meddling could cost millions their lives, page 3] “Hepatitis B is 100 times more contagious than “... hepatitis B HIV, the virus that causes leads to more than AIDS,” Mr. Shepherd told 1 million deaths a legislators. “Many people year.” chronically infected with hepatitis B do not know they have it, so they unknowingly spread it to others.” The WHO reports that hepatitis B leads to more than 1 million deaths a year. “Fortunately, the hepatitis B vaccine is 95% effective in preventing both the viral infection and the liver disease and cancer to which the infection lead,” Mr. Shepherd wrote. [See Gerin, Jenson and Schlegel prevent virus-based cancers, page 4] He cited a comprehensive study by a French drug safety monitoring agency, the Na“Fortunately, the tional Drug Surveillance hepatitis B vaccine Committee, that found lower is 95% effective in incidence of MS symptoms preventing both the among people vaccinated against hepatitis B than in the viral infection and population at-large. the liver disease The American Acadand cancer to which emy of Pediatrics, Infectious the infection lead.” Disease Society of America (IDSA), American Liver Foundation, Hepatitis Foundation International (HFI), Immunization Action Coalition, Parents of Kids with Infectious Diseases (P-KIDS) and other organizations also are engaged in countering the anti-vaccine campaign. Representatives of HFI, IDSA and P-KIDS testified at the congressional hearing, along with officials from the CDC and Food and Drug Administration, that vaccination against hepatitis B is safe and should continue to be required. v John M. Clymer is director of external affairs for the Sabin Vaccine Institute. SABIN VACCINE REPORT June 1999 Vaccines combat biological warfare threat B Y ERICA SEIGUER Recent revelations of the bioterrorist capabilities of nations such as Iraq and Russia, as well as a 1995 gas attack in the Tokyo subway that killed 12 people and injured 5,000, have revealed the vulnerability of the United States to bioterrorist attacks. A terrorist attack with a biological agent is fundamentally different from a chemical or explosive attack. And it requires a completely different response — a response the United States cannot yet provide. And that worries D.A. Henderson, director of the newly inaugurated Center for Civilian Biodefense Studies at Johns Hopkins University in Baltimore. Henderson, a lifelong vaccine scientist, led the World Health Organization’s global smallpox eradication campaign in the 1960s and 1970s and earned a 1994 Sabin Gold Medal Award. He became involved in developing strategies to defend the United States from the threat of bioterrorism as Associate Director for Life Sciences at the White House Office of Science and Technology Policy. It was there that he became aware that biological warfare, or “BW,” was more of a problem than previously anticipated — yet scientists and policy-makers were concerned primarily with chemical and nuclear attack. The United States has been complacent in the face of an increasing possibility of attack with agents such as smallpox, anthrax, or plague, Henderson says. With no immediate, visible threat, however, the urgency needed to mobilize the resources and political will to mount an adequate biodefense plan has not materialized. Until now. U.S. pledges millions for defense Through the Department of Health and Human Services (HHS), the U.S. government has pledged $158 million for FY1999 to develop a bioterrorism defense. The funds will be allocated to improving surveillance, preparing emergency response teams, and stockpiling vaccines and antibiotics. These are currently in such short supply that experts agree an attack tomorrow would find almost any city, state, or locality completely overwhelmed — once physicians and public health officials figure out what happened. The budget President Clinton proposed in January 1999 included about $2.8 billion to be divided among developing defense strategies against biological, chemical, and computer terrorism. Clinton commented that scientific research leading to the development of vaccines to protect citizens would be one of our best defenses. At the February 1999 national symposium on “Medical and Public Health Response to Biological Terrorism,” HHS Secretary Donna Shalala stressed the importance of creating a sense of urgency and opening the national dialogue on the topic. The symposium, the first nonmilitary public meeting on the subject, was organized by the new Center for Civilian Biodefense Studies and cosponsored by 13 other agencies and organizations. Clearly, the level of coordination necessary to address the issue of BW is a significant hurdle. According to Rockefeller University’s Joshua Lederberg, preparing for BW and mounting an appropriate response requires collaboration between very different sectors of society. As he writes in Biological Weapons: Limiting the Threat (MIT Press, 1999), “The transcendence of BW over medicine and public health, private criminal acts, terrorism, interstate warfare, and international law directed at the elimination of BW, makes this one of the most intricate topics of discourse, poses very difficult security problems, and opens some novel challenges in the ethical domain.” Lederberg continues, “[H]ealth authorities will need to negotiate with the military, with law enforcement, with environmental managers. And all will have to cope with how to enhance security without imposing intolerable stresses on personal liberties and on freedom of travel and of commerce.” Challenges of war Two aspects of BW are particularly disturbing. One is the delay that may occur before health officials realize that an act of terrorism has been perpetrated. In contrast to explosive or chemical attacks, a biological attack such as a minuscule amount of anthrax dumped from a plane might take days to be recognized for what it is. Most physicians have never seen, much less diagnosed, a case of smallpox, anthrax, or plague, and so early intervention would be unlikely. Second, even if we were able to figure out early on what had happened, an appropriate response would be difficult. The supply of vaccines and biologicals needed to contain an epidemic is insufficient. Also, hospitals are not set up to deal with large numbers of affected individuals, and facilities for quarantine and isolation are inadequate. Vaccines and other antibiologicals needed Henderson cites smallpox, anthrax, and plague as the top three BW threats today. Given that we already have a smallpox vaccine, why is smallpox considered a threat? There are several reasons. Since the United States stopped vaccinating against smallpox, the amount of vaccine we stockpile would never meet the needs of citizens during a bioterrorist attack. A second-generation smallpox vaccine is in the works, says Henderson, but it is not available yet; nor is it clear that mass vaccination of Americans would be feasible. “In general,” he says, “preventive measures are adopted with great difficulty.” Lacking the urgency that normally comes with a crisis such as an epidemic, vaccination rates are less than desirable. Waiting until a catastrophe occurs, however, will most definitely mean more death and disease. Research and development of vaccines and therapeutics has been conContinued on page 8 Smallpox: Gone for Good?Others, however, see preservation of the smallpox BY JESSICA QUINN As recently as 1967, the smallpox virus ravaged the earth, with 10-15 million cases leading to close to 2 million deaths. In an effort to control this disease, the World Health Organization (WHO) launched a worldwide vaccination campaign against smallpox. Within 13 years, the smallpox virus was declared eradicated, with the only remaining samples stored in research laboratories. In 1981 the WHO recommended that all remaining stocks of the virus be destroyed, except for those held at the Centers for Disease Control (CDC) in Atlanta and at the Institute for Viral Preparations in Moscow. The proposed target date to destroy the last official stocks was June 30, 1999. This proposal brought much debate over the values of these stores and the consequences of destroying them. As a result of the uncertainty, a WHO panel met in Geneva on May 21, 1999 and agreed to postpone the destruction of the virus until at least 2002. Those wishing to eliminate the virus altogether contend that maintaining it has dangerous potential, as it could be used in biological warfare or terrorism and unleashed, could cause another epidemic and result in many lost lives, since — as a result of its eradication — most people are no longer vaccinated against smallpox. virus as important in the advancement of science. As the only virus of its kind unique to humans, smallpox may provide insights into biomedicine that cannot be obtained elsewhere. The DNA sequence of the smallpox virus codes for a unique sequence of proteins that neutralizes human antiviral defense mechanisms. Studying how smallpox accomplishes this may help scientists understand and control HIV, ebola, or other viral illnesses. Preservationists argue that the stores should be maintained for development of a treatment in case of a future smallpox outbreak. They raise several scenarios in which the virus might reemerge — for example, from stocks that are unknowingly stored in non-WHO laboratories, from virus that is somehow preserved in buried smallpox victims, or by resurfacing through a monkeypox variant. Proponents of destruction claim that those situations are highly unlikely and that studies can be done without the live virus. These scientists claimthat genetic sequences mapped from viral plasmids can provide any information that might be needed in the future. However, others argue that the complete virus is necessary, not just plasmid clones, for the greatest understanding of smallpox pathogenesis. The two sides do agree on one thing. If the last stocks are destroyed, smallpox would become the first species deliberately eliminated by man. The bioethics of such an event opens up an entirely new forum for question and debate. v 7 Anthrax threat causes fear BY JESSICA QUINN Anthrax combines many of the properties most feared in disease. It is highly lethal, killing 99 percent of its victims. It can be carried invisibly in the air. And it lies dormant for years before emerging to do its damage. Little wonder, then, that analysts worry that this potent toxin may be used for biological warfare. Anthrax bacteria can survive for many years in the form of spores, thanks to a strong protective coat. Infection occurs when the spores enter a person’s lungs. They move to the lymph nodes, where they reproduce and produce anthrax toxins. Antibiotics may suppress the infection if used before the person develops symptoms. This poses difficulties as there is usually no indication a person has been exposed. The spores do not form a visible cloud, and they have no smell or taste. Twenty-four to 48 hours after exposure, victims suffer from flu-like aches and pains, tightness in the stomach, severe skin infections, fever, fatigue, and difficulty breathing. Shock and death usually occur within 24-36 hours of the onset of these symptoms. Anthrax is seen as a viable biological warfare threat. In the 1980s, U.N. inspectors discovered that Iraq produced 8,000 liters of anthrax spores — an amount that could annihilate the entire human population. Authorities at the Pentagon believe that almost a dozen countries are developing biological weapons, with anthrax a chief candidate. The potential of anthrax as a weapon is compounded by the ability of anthrax spores to remain toxic in water or soil for many years. The Pentagon worries about the possibility of anthrax being made into a dry powder and then stored for later use in war. Fortunately, a vaccine against anthrax is available for people at risk of exposure. The vaccine, developed in the 1950s and 60s and finally approved by the FDA in 1970, is produced by Bioport Corporation of Lansing, Michigan. The vaccine is a cell-free filtrate, meaning it uses dead bacteria rather than live, and the bacteria used are a strain that does not cause disease. It is used primarily by the military. In May 1998, U.S. Secretary of Defense William Cohen approved a plan to vaccinate the entire armed forces. By 2003, nearly 2.4 million men and women will have started the six-shot series of the anthrax vaccine, with those going to Southwest Asia and Korea given top priority. The shots are given over a period of 18 months, with an annual booster shot. The estimated cost of purchase and administration of the anthrax vaccine is $130 million. Despite the Pentagon’s staunch support of the anthrax vaccine, the vaccination program has raised controversy. Some members of the military have refused to be inoculated and face dismissal as a result; they argue that it has not proved effective in humans against airborne anthrax spores and that it may cause side effects. Authorities contend that the vaccine, in use since 1970, has no record of serious side effects, and that although its effectiveness has not been tested in humans, it has proved effective in animal tests, protecting 95 percent of exposed Rhesus monkeys from contracting the disease. Even proponents of vaccine use, however, are concerned about the efficacy of the vaccine against strains of anthrax created specifically to defy the vaccine’s effectiveness. Other objections involve the vaccine’s former manufacturer Michigan Biological Products Institute. FDA reports in February of 1998 cited sloppiness in recordkeeping and testing procedures at the manufacturing plant, raising questions about the sterility of the vaccine. Such reports reached the Internet, causing concern among people required to receive the vaccine. The manufacturer was sold in September 1998, and the FDA and Pentagon state that the current manufacturer, Bioport Corporation, and vaccine are safe. Some military personnel have also raised the issue of the mystery surrounding Gulf War Syndrome. Although no symptomatic link has been established between that illness and the anthrax vaccine administered to over 150,000 of the 500,000 people who served in the Persian Gulf War, some people have suggested that the symptoms of Gulf War Syndrome are side effects from exposure to the vaccine. Authorities and scientists maintain that the current vaccine is both safe and effective. It is seen as a key factor in protecting the world from biological warfare. v SABIN VACCINE REPORT June 1999 8 Sabin encourages next generation of leaders in vaccinology BY JANE FOX Named as 1999 Sabin Hilleman Student Award winners at Intel ISEF were: · Bryan M. Roberts of Pennsylvania for his project examining p53 gene therapy in the human leukemia cell line THP-1. The goal of gene therapy is to replace defective, disease-causing genes with normal genes. His work supported the idea that p53 gene therapy might be effective in treating human leukemia; · Jeet Minocha of California for work to develop a potential live attenuated dysentery vaccine strain against a photo by FocusOne variety, may contain one or more substances capable of inhibiting the growth of human tumor cells. Under the auspices of its Sabin-Hilleman Fellows Program, The students’ research was completed in a variety of the Albert B. Sabin Vaccine Institute honored six students settings and under differing circumstances. For example, for the scientific merit of the projects they presented at the Joseph Markson’s work was undertaken as part of a schoolannual Intel-sponsored International Science and Engineersponsored internship at the University of Maryland Medical ing Fair (ISEF). School while Bryan Roberts’ work was an independent project The Intel ISEF, held in Philadelphia in May, is now in using the laboratories at Dickinson College. Coincidentally, its 50th year and participation is widely recognized as the both these students are also high school baseball players. highest achievement in high school science competitions. The judges were impressed by the students’ work. The ISEF, the only international science project competiRouzer noted that the Sabintion for 9th through 12th Hilleman Award recipients graders, had over 1100 pardid most if not all of this ticipants from more than 30 “very sophisticated” work incountries competing for over dependently. One student $2 million in scholarships and worked with her high school awards. Students attending teacher, without the advanwere top winners from one of tage of guidance from a 500 science fair competitions lab-based scientist that most held world-wide. With about other participants had. Achalf of the participating stucording to Carol Rouzer, dents female and 95% of “The truly outstanding finalists from the public projects were those in which schools, Intel ISEF has been the students themselves took successful at encouraging the initiative.” Laura Kragie participation by traditionally H.R. Shepherd, chairman of the Sabin Vaccine Institute presents awards to Kapualokelanipomaika’i K. Medeiros, Bryan M. Roberts, concurred, noting that stuMaria Carolina Pavan, Carolina Glavao, Joseph S. Markson, and Jeet Minocha at the Intel International Science and Engineering Fair. under-represented groups. dents’ “independence” and Judges are drawn from “self-motivation” were among science, engineering and industry and include Nobel Laure- form of shigella, Shigella flexneri virG SC602, which causes the key factors considered in making the awards decisions. ates and Intel fellows. Judges must have the equivalent of a mild diarrhea in humans; Kragie noted that all the awardees wanted to pursue Ph.D.or M.D. and have eight years of related professional · Joseph S. Markson of Maryland, whose project inves- medicine or graduate study in the biomedical sciences. Stuexperience as the projects are often at the graduate level or tigated potential design improvements in, and the biology dents like these will lead the next generation in the field of higher. of, the genetically deactivated pertussis toxin used as a vector vaccinology. According to H.R. Shepherd, Chairman of the Recognizing the need to help today’s young people for the delivery of HIV antigen peptides (epitopes) into a Institute, “The Albert B. Sabin Vaccine Institute is proud to become tomorrow’s science professionals, the Albert B. Sabin cell in a developmental HIV vaccine; · honor these students, and we look forward to their future Vaccine Institute has become a Special Awards Organiza- · Maria Carolina Pavan and Carolina Glavao of Sao scientific achievement. It is hoped that each of them will tion for the Intel ISEF. Sabin Institute judges included Paulo, Brazil whose project developed a basis for a bovine continue with advanced scientific studies in the area of disHerbert Herscowitz, PhD of Georgetown University —a hybrid vaccine against Escherichia coli and Salmonella ease prevention, and will be as successful in their chosen member of the Institute’s Scientific Advisory Committee, typhimurium to prevent infection in cattle, thereby indirectly career as they have been at the Intel Science Fair.” v Laura Kragie, PhD, President of Biomedworks, and Carol reducing human infection; and · Rouzer, MD, PhD a professor at Western Maryland College. · Kapualokelanipomaika’i K. Medeiros of Hawaii for Jane Fox is a Senior Marketing Consultant for Lubin Lawrence, The six student winners received a classical library of books work examining the effectiveness of papaya seeds, a tradi- Inc. of New York. that include classic treatises as well as modern texts to inspire tional Hawaiian medicine used to treat early stage cancer. the recipients in their scientific endeavors. The seeds of the papaya, especially those of the “Sunrise” Biodefense News from the Institute Continued from page 7 Changing of the Guard Erica Seiguer, editor of the last three issues of the Sabin Vaccine Report, concluded her one-year fellowship with the Sabin Vaccine Institute. She is now doing research in the Washington, DC office of PATH, the Program for Appropriate Technology in Health. She will begin a M.D./Ph.D. program at Harvard University this fall. The Sabin Vaccine Institute is grateful to Erica for greatly improving the quality of the Sabin Vaccine Report. She set it on a new course to provide fresh information and perspective, and news summaries targeted to a broad audience, including laypersons, vaccinologists, public health officials, journalists, policy makers and industry leaders. The new editor is Charlene Flash who, in addition to her publishing responsibilities, is a research fellow at Sabin. As this issue illustrates, Charlene is up to the challenge of continuing the forward momentum. Wearing her research fellow hat, Charlene gave the final presentation at the Sabin Vaccine Institute’s Colloquium on Cancer Vaccines and Immunotherapy at Walker’s Cay in March. She outlined how a consortium involving academia, industry and government could accelerate development of vaccines to treat and prevent cancer. Her discourse drew effusive praise from the prominent scientists, CEOs and others present. Sabin wishes Erica Seiguer well in her promising future and is fortunate to have Charlene Flash contributing talent, energy, and fresh ideas to its programs. v Proposed law spurs vaccine development B Y JOHN CLYMER New federal legislation could create incentives for private sector research and development on vaccines for diseases that kill over 7 million people a year. Rep. Nancy Pelosi (D-CA) introduced the Lifesaving Vaccine Technology Act in Congress this spring. It would establish a tax credit for pharmaceutical and biotechnology companies that do research and development on vaccines to prevent malaria, tuberculosis and HIV/AIDS. The diseases cited by Rep. Pelosi disproportionately affect developing countries that have limited funds for health care. Vaccine research companies face the prospect of investing tens or hundreds of millions of dollars to develop vaccines whose primary markets cannot afford them. The bill provides the special incentives needed to encourage firms to risk capital on research and development of vaccines for these diseases. “Vaccines are our best hope to control the epidemics of TB, malaria and HIV/AIDS, yet there are significant disincentives for investing in private sector research and development of vaccines for these infectious diseases,” said Pelosi. “[My bill] will leverage private sector resources, and encourage the market to work more effectively to address the biggest public health opportunities.” Pelosi’s staff consulted Sabin Vaccine Institute founding president Philip K. Russell, M.D. while drafting the legislation. A white paper issued by her office on the need for vaccines against the most deadly diseases in the world quotes Russell: “Unless there is vigorous investment from the private sector, vaccines won’t get through the [research and development] pipeline.” The Lifesaving Vaccine Technology Act (H. R. 1274) has 18 co-sponsors in the House of Representatives. Gaining Senate sponsors and additional House co-sponsors will increase its chances of passage. Copies of the bill (H. R. 1274) and background information are available from the Sabin Vaccine Institute. Copies of the bill and additional information about developing vaccines to prevent deadly diseases are also available directly from Pelosi’s office (202-225-4965). v ducted mostly in the public sector, through the National Institutes of Health and the U.S. Department of Defense. The pharmaceutical industry has shied away from such research programs. Better late than never Despite the relative state of unpreparedness, public health officials are pleased at interest demonstrated by physicians, nurses, emergency management professionals, and others whose cooperation and insights are crucial for any successful defense. Despite only two months’ advance notice for the February conference at which Shalala spoke, registration surpassed 900 people from 46 states and 10 foreign countries, says Henderson. A great deal of research, strategizing, and implementation is needed to increase BW preparedness, and it is clear that the issue has found an attentive audience. v sabin calendar The Institute is not responsible for non-Institute events listed below. December 2-5, 1999 Cold Spring Harbor, NY MOLECULAR APPROACHES TO VACCINE DESIGN Sessions will include HIV/SIV, Mechanisms of Protective Immunity, Mucosal versus Systemic Immunity, Mechanisms of Immune Memory, Co-stimulation and Dendritic Cells and Delivery Systems. December 5-7, 1999 Cold Spring Harbor, NY FINANCING THE NEXT GENERATION OF VACCINES Sponsored by the Sabin Vaccine Institute and organized by Jeffrey Sachs, M.D. Ph.D. and Peter Hotez, M.D. Ph.D.