* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
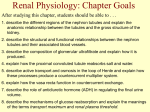
Download Chapter 14 The Kidneys and Regulation of Water and Inorganic Ions
Urethroplasty wikipedia , lookup
Urinary tract infection wikipedia , lookup
Interstitial cystitis wikipedia , lookup
Kidney stone disease wikipedia , lookup
Kidney transplantation wikipedia , lookup
Renal angina wikipedia , lookup
Chronic kidney disease wikipedia , lookup
IgA nephropathy wikipedia , lookup
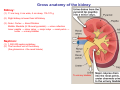
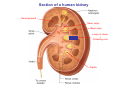
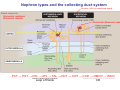
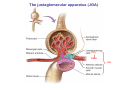
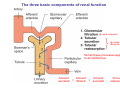
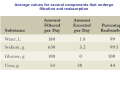
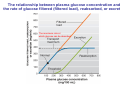
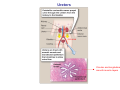
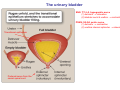
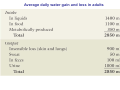
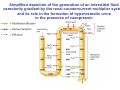
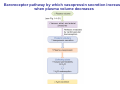
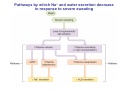
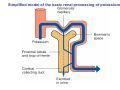
Autosomal dominant polycystic kidney disease wikipedia , lookup
Chapter 14 The Kidneys and Regulation of Water and Inorganic Ions Functions of the kidneys Urea, uric acid, creatinine Drugs, pesticides, food additives Amino acids → glucose Urinary system in a women Gross anatomy of the kidney Kidney: (1) 11 cm long, 6 cm wide, 4 cm deep, 115-170 g (2) Right kidney is lower than left kidney (3) Outer: Cortex → blood filtration Middle: Medulla (8-18 renal pyramids) → urine collection Inner: papilla → minor calyx → major calyx → renal pelvis → ureter → urinary bladder Nephron: (1) 1,000,000 nephrons/kidney (2) The functionl unit of the kidney (the glomerulus + the renal tubule) To urinary bladder Section of a human kidney Renal pyramid Minor calyx Major calyx Loops of Henle + Collecting ucts Papilla Basic structure of a nephron 106 nephrons/kidney Part of thick segment of ascending limb 10-15% 80-85% Nephron types and the collecting duct system Receive 90% of renal blood supply Renal corpuscle; Glomerular capillaries Glomerular capsule Glomerular (Bowman) capsule PCT → PST → DTL → ATL → TAL → DCT → CNT → CCD → OMCD → IMCD Loop of Henle CD Basic structure of a nephron Nephron Anatomy of the renal corpuscle JGA Thick segment of ascending limb Glomerular filtrate Cell-free, protein-free (20% of the plasma) Mesangial cells The glomerulus and its filtration barrier Pore size 70 nm GFR (glomerular filtration rate) = Kf [(PGC-PBS) - (GC-BS)] Hydrostatic pressure Colloid osmotic pressure GC: glomerular capillary BS: Bowmen space < 5,000 Da (1) (2) (3) Lamina rara interna Lamina densa Lamina rara externa TEM of a glomerular capillary and the glomerular membranes Podocytes (fltration slits) Basement membrane Endothelia (fenestrae) The juxtaglomerular apparatus (JGA) (JG) Renin JGA The three basic components of renal function @ renal corpuscle @ varies sites along the tubule Not all these processes apply to all substances Amount Amount Amount = + excreted filtered secreted Amount reabsorbed Renal handling of three hypothetical filtered substrances Forces involved in glomerular filtration Forces favoring glomerular ultrafiltration PBS: Bowman space PGC: glomerular capillary hydrostatic pressure GC: glomerular capillary colloid osmotic pressure + 20 mm Hg + 8 mm Hg Forces controlling fluid reabsorption by peritubular capillaries PC 25 mm Hg in all other regions of the body PC 35 mm Hg 20 mm Hg Other systemic capillary beds 35 mm Hg Control of GFR by constriction or dilation of afferent aRterioles (AA) or efferent arterioles (EA) GFR (glomerular filtration rate) AA: afferent arteriole EA: efferent arteriole Average values for several components that undergo filtration and reabsorption Diagrammatic representation of tubular epithelium Transcellular route (by transporters) Paracellular route (by diffusion) Apical Pathways for reabsorption from the tubule lumen Determined by tight junction structure Requires the assistance of channels or transporters ATP-dependent pumps The relationship between plasma glucose concentration and the rate of glucose filtered (filtered load), reabsorbed, or excreted The maximum rate at which glucose can be absorbed Example of renal handling of inulin The clearance of inulin is equal to the glomerular filtration rate Ureters 2-6 cm/s Circular and longitudinal smooth muscle layers The urinary bladder SNS: T11-L2, hypogastric nerve (1) detrusor relaxation (2) bladder neck & urethra contraction PSNS: S2-S4, pelvic nerve (1) detrusor contraction (2) urethra internal sphincter relaxation Transitional epithelium Pudenal nerve from the sacral spinal cord Intravascular ureteral valve preventing urine reflex Control of the bladder Average daily water gain and loss in adults Daily sodium chloride intake and loss Mechanism of Na+ reabsorption in the proximal tubule and cortical collecting duct Coupling of water and Na+ reabsorption The regulation and function of aquaporins (AQPs) in the medullary-collecting-duct cells to increase water reabsorption ADH receptor ADH Vasopressin-sensitive Vasopressin-insensitive Diabetes insipidus caused by the failure to release vasopressin or non-respond to vasopressin 25 L/day Generating a hyperosmolar medullary renal interstitium Countercurrent multiplier system Impermeable tp H2O Simplified depiction of the generation of an interstitial fluid osmolarity gradient by the renal countercurrent multiplier system and its role in the formation of hyperosmotic urine in the presence of vasopressin Functions of the vasa recta to maintain the hypertonic interstitial renal medulla Urea recycling Direct and neurally mediated reflex pathways when plasma volume decreases Summary of the renin-angiotensin system and the stimulation of aldosterone secretion by angiotensin II RASS (renin-angiotensin-aldosterone system) ACE @ cortical collecting ducts Pathways by which decreased plasma volume leads to increased Na+ reabsorption Atrial natriuretic peptide (ANP) increases Na+ excretion Osmoreceptor pathway that decreases vasopressin secretion and increases water excretion when excess water is ingested Baroreceptor pathway by which vasopressin secretion increases when plasma volume decreases Pathways by which Na+ and water excretion decrease in response to severe sweating Inputs controlling thirst Simplified model of the basic renal processing of potassium Pathways by which an increased potassium intake induces greater K+ excretion Summary of the control of aldosterone and its effects on Na+ absorption and K+ secretion Summary of “Division of labor” in the renal tubules Sources of hydrogen ion gain and loss Reabsorption of HCO3- H+-ATPase or Na+/H+ countertransporters H+/K+-ATPase pumps Renal contribution of new HCO3- to the plasma as achieved by tubular secretion of H+ H+-ATPase or Na+/H+ countertransporters H+/K+-ATPase pumps Renal contribution of new HCO3- to the plasma as achieved by renal metabolism of glutamine and excretion of ammonium (NH4+) Proximal tubule Renal responses to acidosis and alkalosis Changes in the arterial concentrations of H+, HCO3-, and carbon dioxide in acid-base disorders Simplified diagram of hemodialysis 400 mL/min 1000 mL/min