* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download b. Ventricular stroke volume decrease
Survey
Document related concepts
Transcript
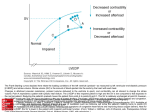
b. Ventricular stroke volume decrease Stroke volume is the amount of blood being pumped out the left ventricle (to the body) per heartbeat. Cardiac output is the total volume leaving the left ventricle per minute (or SV * HRM). The mechanical performance of the ventricle is due to the FrankStarling mechanism. This mechanism shows that stroke volume increases as the preload (or End Diastolic Volume) increases. As we know from the first point, blood volume decreases in microgravity. With this decreased volume the preload is not as great in the left ventricle (Kotovskaya & Fomina, 2010). With this reduction in preload the stretch of the ventricle is not as large, and the force of contraction is not as great. Therefore, the stroke volume is reduced. With the reduction in stroke volume comes the reduction in cardiac output (Carter & West, 2013). The reduction of preload has been seen to decrease by 3-6% within the first month of flight. This number increases to 8-10% by month 5-6 (Kotovskaya & Fomina, 2010). A decrease in stroke volume of 17% has been seen after 31 days of flight. This percentage increased to 36% in a study after 171 days of flight (Antonutto & di Prampero, 2003). It is important to note that although preload and stroke volume decreased, the left ventricular ejection fraction (SV/EDV) stayed within a normal range (Kotovskaya & Fomina, 2010). (Thigh cuffs are used as a way to reduce the change in stroke volume). The function and myocardial contractility (pumping function) also remained within normal limits (Kotovskaya & Fomina, 2010; Schneider & Convertino). After return from flight the reduction in stroke volume is still apparent (Carter & West, 2013). In bed rest, cardiac compliance (the change in intraventricular pressure for a change in preload) was shown to increase during the first few days of rest by showing that stroke volume remained higher at any given filling pressure (Schneider & Convertino). Cardiac compliance is used as a defense mechanism to maintain stroke volume even with a reduction in preload. Even with this change during bed rest, after about two weeks ventricular remodeling was noted and cardiac compliance and preload decreased (Schneider & Convertino). The reduction of blood volume, stroke volume, and cardiac output all play a part in the reduced baroreflex function and the ability for blood vessels to constrict in the lower extremity (Carter & West, 2013). When the blood vessels are not as able to constrict, the blood flow is not as strong, and the venous return (to the heart) is reduced. The reduction of blood getting to the heart also plays a part in the decrease of stroke volume. There is a greater capacity for blood to pool due to the impaired constriction and also the reduction in leg muscle mass (Schneider & Convertino). (The tissue mass normally provides structural 1 b. Ventricular stroke volume decrease support, but with the decreased size this may also play a part in the reduced ability to constrict). These changes contribute to orthostatic intolerance (Hargens et al., 2013), hypovolemia (Schneider & Convertino), and reduced aerobic capacity (Hargens et al., 2013). To next Physiological Change: c. The Carotid Baroreceptor resets Or back to home: 1. Introduction 2