* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Mul Ma ltiple M anagin Myelo g Rela oma: C apse an Current nd Ref
Survey
Document related concepts
Transcript
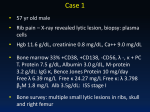
Mulltiple M Myelo oma: C Currentt Apprroachees to Maanaging Relaapse an nd Reffractory Diseease Pressented ass a Live W Webinar Tuesday, A August 20 0, 2013 and W Wednesd day, Septeember 18 8, 2013 Planned d and conducte ed by ASHP Advvantage and su upported by ed ducational grants from Millennium m: The Takeda O Oncology Company and Onyxx Pharmaceuticals, Inc. Multiple Myeloma: Current Approaches to Managing Relapse and Refractory Disease WEBINAR INFORMATION How do I register? Go to www.ashpadvantage.com/myeloma/relapse and click on the Register Now button. After you submit your information, you will be e-mailed computer and audio information. What is a live webinar? A live webinar brings the presentation to you – at your work place, in your home, through a staff in-service program. You listen to the speaker presentation in “real time” as you watch the slides on the screen. You will have the opportunity to ask the speaker questions at the end of the program. Please join the conference at least 5 minutes before the scheduled start time for important announcements. How do I process my Continuing Education (CE) credit? Continuing pharmacy education for this activity will be processed on ASHP’s eLearning system and reported directly to CPE Monitor. After completion of the live webinar, you can process your CPE credit and print your statement of credit online at http://elearning.ashp.org/my-activities. To process your CPE credit, you will need the enrollment code that will be announced at the end of the webinar. Full CE processing instructions can be found on the last page of this handout as well as at http://www.ashp.org/claimce. What if I would like to arrange for my colleagues to participate in this webinar as a group? One person serving as the group coordinator should register for the webinar. That group coordinator will receive an e-mail confirmation with instructions for joining the webinar. A few minutes before the webinar begins, the group coordinator should launch the webinar link. Once the webinar has been activated, the coordinator will have the option to open the audio via VoIP (Voice Over IP) on the webinar toolbar or use a touch tone phone with the provided dial-in information. At the conclusion of the activity, the group coordinator will complete a brief online evaluation and report the number of participants at that site. Each participant will process his or her individual continuing education statement online. What do I need in order to participate in the webinar? 1. Computer with internet access and basic system requirements. When you register, the webinar system will assess your system to ensure compatibility. 2. Telephone to dial the toll-free number and listen to the presentation (if you choose not to use Voice Over IP [VoIP] via your computer). Webinar System Requirements Be sure to view the webinar system requirements for Windows, Mac, iOS, and Android prior to the activity. 1 Multiple Myeloma: Current Approaches to Managing Relapse and Refractory Disease ACTIVITY FACULTY Christopher A. Fausel, Pharm.D., M.H.A., BCOP Clinical Manager of Oncology Pharmacy Indiana University Simon Cancer Center Indiana University Health Indianapolis, Indiana Christopher A. Fausel, Pharm.D., M.H.A, BCOP, is Clinical Manager of Oncology Pharmacy at Indiana University Simon Cancer Center (IUSCC) in Indianapolis, Indiana. He oversees the clinical and dispensing pharmacy services at the IUSCC ambulatory infusion center and six satellite infusion clinics. Dr. Fausel holds academic appointments at the Department of Medicine at Indiana University School of Medicine, Purdue University School of Pharmacy and Pharmaceutical Sciences, and Butler University College of Pharmacy. He is the founding Residency Program Director for the postgraduate year two (PGY-2) oncology pharmacy residency at Indiana University Health. He serves on the Indiana University Purdue University at Indianapolis Institutional Review Board and Indiana University Simon Cancer Center Scientific Review Committee. Dr. Fausel received his Bachelor of Science degree in pharmacy and Doctor of Pharmacy degree from Albany College of Pharmacy in Albany, New York. He completed a pharmacy practice residency accredited by the American Society of Health-System Pharmacists (ASHP) at the Samuel S. Stratton VA Medical Center in Albany, New York. More recently, he earned a Master of Health Administration degree from Simmons College in Boston, Massachusetts. Dr. Fausel is a board-certified oncology pharmacist (BCOP), and he is certified in basic life support by the American Red Cross. He is a member of the Hoosier Oncology Group Board of Directors and a long-standing member of ASHP, American Society of Clinical Oncology, and Hematology/Oncology Pharmacy Association. 2 Multiple Myeloma: Current Approaches to Managing Relapse and Refractory Disease DISCLOSURE STATEMENT In accordance with the Accreditation Council for Continuing Medical Education’s Standards for Commercial Support and the Accreditation Council for Pharmacy Education’s Guidelines for Standards for Commercial Support, ASHP Advantage requires that all individuals involved in the development of activity content disclose their relevant financial relationships. A person has a relevant financial relationship if the individual or his or her spouse/partner has a financial relationship (e.g., employee, consultant, research grant recipient, speakers bureau, or stockholder) in any amount occurring in the last 12 months with a commercial interest whose products or services may be discussed in the educational activity content over which the individual has control. The existence of these relationships is provided for the information of participants and should not be assumed to have an adverse impact on presentations. All faculty and planners for ASHP Advantage education activities are qualified and selected by ASHP Advantage and required to disclose any relevant financial relationships with commercial interests. ASHP Advantage identifies and resolves conflicts of interest prior to an individual’s participation in development of content for an educational activity. The following faculty and planners report no relationships pertinent to this activity: - Christopher A. Fausel, Pharm.D., M.H.A., BCOP Tippu Khan, Pharm.D., BCOP, CPP Gerald M. Higa, Pharm.D. James Aubrey Waddell, Pharm.D., BCOP, FAPhA Jill A. Sellers, Pharm.D. Carla J. Brink, M.S., B.S.Pharm. ASHP staff has no relevant financial relationships to disclose. 3 Multiple Myeloma: Current Approaches to Managing Relapse and Refractory Disease ACTIVITY OVERVIEW Among the many challenges of managing patients with multiple myeloma is the fact that most patients eventually develop resistance to therapy. Several new treatment options have emerged over the past few years for managing relapse and refractory disease. This educational activity will review current options to address this challenge. Time for questions and answers from the webinar audience will be provided at the end of the presentation. LEARNING OBJECTIVES At the conclusion of this application-based educational activity, participants should be able to • Review current and emerging treatment strategies for the management of patients with relapsed and refractory multiple myeloma. • Apply evidence-based approaches to managing the challenges in treating relapsed and refractory multiple myeloma. • Describe appropriate supportive care measures for patients receiving active treatment for multiple myeloma. LIST OF ABBREVIATIONS For a list of abbreviations used in this activity, please see page 18. CONTINUING EDUCATION ACCREDITATION The American Society of Health-System Pharmacists is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. This activity provides 1 hour (0.1 CEU) of continuing pharmacy education credit (ACPE activity # 0204-0000-13-460-L01-P). Attendees must complete a Continuing Pharmacy Education Request online and may print their official ASHP statements of continuing pharmacy education credit at the ASHP eLearning site (elearning.ashp.org) immediately following this activity. Complete instructions for processing CE can be found on the last page of this handout. 4 Which of these represents true progressive disease in multiple myeloma (MM)? Multiple Myeloma: Current Approaches to Managing Relapse and Refractory Disease A. Less than 50% reduction in serum M-component B. Less than 25% reduction in serum M-component C. Incomplete resolution of plasmacytoma D. New-onset hypercalcemia that may be secondary to MM Christopher A. Fausel, Pharm.D., M.H.A., BCOP Indiana University Health Indianapolis, Indiana Enlarged version on page 13 Enlarged version on page 13 Salvage Therapy Options Definition of Progression Progression Increase in 25% or more from lowest response value in any one or more of the following: Serum M-component (absolute increase must be ≥ 0.5 g/dL) Urine M-component (absolute increase must be ≥ 200 mg per 24 hours) Only in patients without measureable serum and urine M-protein levels: the difference between involved and uninvolved free light chains levels (absolute increase must be > 10 mg/L) Bone marrow plasma cell percentage (absolute percentage must be ≥ 10%) Definite development of new bone lesions or soft tissue plasmacytomas or definite increase in the size of existing bone lesions or soft tissue plasmacytomas Development of hypercalcemia (corrected serum calcium > 11.5 mg/dL) that can be attributed solely to the plasma cell proliferative disorder Preferred regimens Other regimens Repeat primary induction (if relapse at > 6 months) Bortezomib Bortezomib, dexamethasone Bortezomib, lenalidomide, dexamethasone Bortezomib, liposomal doxorubicin Bortezomib, thalidomide, dexamethasone Carfilzomib Cyclophosphamide, bortezomib, dexamethasone Dexamethasone, cyclophosphamide, etoposide, cisplatin Dexamethasone, thalidomide, cisplatin, doxorubicin, cyclophosphamide, etoposide ± bortezomib High-dose cyclophosphamide Lenalidomide, dexamethasone Pomalidomide, dexamethasone Thalidomide, dexamethasone Bendamustine Bortezomib, vorinostat Lenalidomide, bendamustine, dexamethasone NCCN Guidelines Version 2.2013 Multiple Myeloma. www.nccn.org Durie BGM et al. Leukemia. 2006; 20:1467-73. Which of these is an appropriate supportive care measure with patients receiving treatment with bortezomib? ? Bortezomib vs. Dexamethasone: Phase III in Refractory Disease ? A. Pre-emptive therapy with gabapentin B. Pre-emptive therapy with romiplostim C. Pre-medication with palonosetron, dexamethasone, aprepitant D. Prophylaxis with acyclovir Response rate Median time to progression Median overall survival Bortezomib (n = 313) 43% 6 months 29.8 months Dexamethasone (n = 312) 19% 3.5 months 23.7 months P value <0.001 <0.001 0.027 Richardson PG et al. N Engl J Med. 2005; 352:2487-92. Richardson PG et al. Blood. 2007; 110:3557-60. 5 Grade III/IV Toxicity Toxicity Bortezomib Retreatment Bortezomib Dexamethasone (n = 313) (n = 312) Anemia 10% 11% Constipation 2% 1% Diarrhea 7% 2% Dyspepsia 6% 4% Fatigue 6% 4% Nausea/vomiting 5% 1% Neutropenia 14% 1% Peripheral neuropathy 8% 1% Pyrexia 2% 2% Thrombocytopenia 30% 6% • Phase II study of 130 patients with a median of two lines of prior treatment • Regimen – Bortezomib 1 or 1.3 mg/m2 (last tolerated dose with first treatment) IV on days 1, 4, 8, 11 in a 21-day cycle • Primary endpoint: best confirmed response at retreatment Richardson PG et al. N Engl J Med. 2005; 352:2487-92. Richardson PG et al. Blood. 2007; 110:3557-60. Petrucci MT et al. Br J Haematol. 2013; 160:649-59. Results Efficacy Prior exposure to bortezomib N = 130 (total) Patients receiving ≥ 4 treatment cycles 90% Single-agent bortezomib 37% Bortezomib with another agent 63% Last tolerated dose – 1.3 mg/m2 Last tolerated dose – 1 mg/m2 29% 62% Median duration of therapy Median time from prior bortezomib treatment Response parameter N = 126 Overall response 40% Complete response 1% 39% 4.9 months Very good partial response/partial response Median response duration 6.5 months 13.9 months Progression free survival 8.4 months Petrucci MT et al. Br J Haematol. 2013; 160:649-59. Petrucci MT et al. Br J Haematol. 2013; 160:649-59. Bortezomib + Liposomal Doxorubicin: Phase III Results Grade III/IV Toxicity Toxicity N = 130 Thrombocytopenia 35% Diarrhea 7% Neutropenia 7% Pneumonia 6% Bortezomib 41 2 Progression Overall free survival survival at 15 (months) months (%) 6.5 65 5% Bortezomib 44 + liposomal doxorubicin 4 9.3 Anemia Neuropathy 0% Any Grade III/IV 60% Regimen Response Complete rate (%) response (%) *p = 0.03 Orlowski RZ et al. J Clin Oncol. 2007; 25:3892-901. Petrucci MT et al. Br J Haematol. 2013; 160:649-59. 6 76* Cyclophosphamide, Bortezomib, Dexamethasone Efficacy Parameter • Phase II trial with 54 patients receiving – Bortezomib 1.3 mg/m2 IV on days 1, 4, 8, 11 – Dexamethasone 20 mg PO on days 1, 2, 4, 5, 8, 9, 11, 12 – Cyclophosphamide 50 mg PO daily – Cycle repeated every 21 days • Primary endpoint – Response rate Kropff M et al. Br J Haematol. 2007; 138:330-7. Overall response Evaluable patients (n = 50) 82% Complete response 16% Partial response 66% Minor response 8% Median event free survival Overall survival 12 months 22 months Kropff M et al. Br J Haematol. 2007; 138:330-7. Which of these represents the most reasonable therapy choice for a patient with refractory MM and cirrhosis? Grade III/IV Toxicity Toxicity Grade III/IV (n = 53) Anemia Bleeding 9% 2% Dyspnea 4% Fatigue 15% Herpes zoster 15% Infection 23% Leukocytopenia 20% Neuropathy Thrombocytopenia 21% 53% ? A. Bortezomib and dexamethasone B. Bortezomib, cyclophosphamide, dexamethasone C. Dexamethasone, cyclophosphamide, etoposide, cisplatin D. Lenalidomide and dexamethasone Kropff M et al. Br J Haematol. 2007; 138:330-7. Lenalidomide + Dexamethasone: Phase III results (combined) Regimen Response Complete rate (%) response (%) Time to progression (months) Overall survival (months) Dexamethasone 19 (n = 352) 1-3.4 4.7 20.1 Lenalidomide + 61 dexamethasone (n = 352) 14-16 11.2 29.6 Carfilzomib: Phase II Trial • Phase II study evaluated 266 patients with relapsed/refractory MM previously treated with bortezomib • Regimen – Carfilzomib 20 mg/m2 IV on days 1, 2, 8, 9, 15, 16 repeated every 28 days x cycle 1 – Then carfilzomib 27 mg/m2 IV on days 1, 2, 8, 9, 15, 16 repeated every 28 days – Plus dexamethasone 4 mg PO or IV prior to each carfilzomib dose • Primary endpoint – Response rate Dimopoulos M et al. N Engl J Med. 2007; 357:2123-32. Weber DM et al. N Engl J Med. 2007; 357:2133-42. Siegel DS et al. Blood. 2012; 120:2817-25. 7 Grade III/IV Toxicity Efficacy Parameter N = 257 Thrombocytopenia 29% Parameter N = 257 Response rate 24% Anemia 24% Complete response 0.4% Lymphopenia 20% Very good partial response 5% Neutropenia 11% Pneumonia 9% Time to progression 7.8 months Overall survival 15.6 months All patients had received prior bortezomib (except one). Fatigue 8% Hyponatremia 8% Leukopenia 7% Hypophosphatemia 6% Upper respiratory infection 5% Siegel DS et al. Blood. 2012; 120:2817-25. Siegel DS et al. Blood. 2012; 120:2817-25. Results Pomalidomide • Phase II study evaluated 84 patients with relapsed/refractory myeloma previously treated with bortezomib and lenalidomide with two dosing regimens for pomalidomide • Dosing – Pomalidomide 4 mg PO daily on days 1 through 21 of a 28-day cycle or continuously for a 28-day cycle with dexamethasone 40 mg PO once weekly • Primary endpoint – Response rate Parameter 21 of 28-day P 28 of 28-day P dosing (n = 43) dosing (n = 41) Response rate (%) 35 34 Complete response (%) 2 5 Very good partial response (%) 2 2 Time to progression (months) 5.5 4.6 Overall survival at 18 months (%) 49 39 P = Pomalidomide Leleu X et al. Blood. 2013; 121:1968-75. Leleu X et al. Blood. 2013; 121:1968-75. Carfilzomib, Lenalidomide, Dexamethasone (CLD) – Refractory MM Grade III/IV Toxicity Toxicity N = 84 Neutropenia 62% Anemia 36% Thrombocytopenia General disorders 27% 24% Musculoskeletal and connective tissue disorders 20% Pneumonia 13% Dyspnea 12% Bone pain 11% Renal failure 11% • Phase I trial to establish maximum tolerated dose (MTD) of CLD in a refractory cohort of 40 patients – Prior treatments – 75% bortezomib, 70% lenalidomide, 75% transplant • MTD – – – – Carfilzomib 27 mg/m2 IV days 1, 2, 8, 9, 15, 16 Lenalidomide 25 mg PO daily days 1 through 21 Dexamethasone 40 mg PO weekly Repeat cycle every 28 days Niesvizky R et al. Clin Cancer Res. 2013; 19:2248-56. Leleu X et al. Blood. 2013; 121:1968-75. 8 Efficacy Toxicity – Grade III/IV Parameter Outcome (n = 40) Toxicity Event Grade III/IV (n = 40) Overall response rate 62.5% Neutropenia 43% Stringent complete response 2.5% Thrombocytopenia Lymphopenia 33% 28% Hyperglycemia 23% Very good partial response 32.5% Partial response 27.5% Median duration of response 11.8 months Median progression free survival 10.2 months Anemia 20% Hypophosphatemia 20% Leukopenia 18% Hyponatremia 15% Hypokalemia 10% Niesvizky R et al. Clin Cancer Res. 2013; 19:2248-56. Niesvizky R et al. Clin Cancer Res. 2013; 19:2248-56. Future Drug Targets in MM Monoclonal Antibody Therapy Cell surface targets Cytokines CD40 FGFR3 CS1 BAFF-R VEGF-R IL-6 VEGF IGF-1 SDF-1α BAFF APRIL BSF-3 1. Induction of apoptosis Monoclonal antibody Intact C1 Plasma cell Target antigen Fc receptor 2. Activation of complement Bone marrow stroma NF-κB Smad ERK Killer cell Anderson KC. J Clin Oncol. 2012; 30:445-52. 3. ADCC Investigational Agents (MoAb) Agent BHQ880 Dacetuzumab Daratumumab Elotuzumab huN901-DM1 RAP-011 1339 Target DKK1 CD40 CD38 CS1 CD56 Activin A IL-6 Supportive Care Anderson KC. J Natl Compr Canc Netw. 2013; 11(5 Suppl):676-9. 9 Adhesion molecules ICAM-1 VCAM-1 Fibronectin LFA-1 MUC-1 VLA-4 Which of the following would be the most likely cause of mortality in a patient with MM? Adjunctive Therapy for MM ? • Bone disease – All patients receiving primary MM therapy should be given bisphosphonates – Use of bisphosphonates in smoldering or stage I disease should preferably be in the context of a clinical trial A. Lytic lesions of bone B. Hypercalcemia of malignancy C. Anemia D. Infection • Conduct bone surveys annually and if symptomatic – Monitor for renal dysfunction with use of bisphosphonates – Monitor for osteonecrosis of the jaw NCCN Guidelines Version 2.2013 Multiple Myeloma. www.nccn.org Adjunctive Therapy for MM Adjunctive Therapy for MM • Radiation therapy • Hypercalcemia – Low-dose radiation (10-30Gy) can be used as palliative treatment for uncontrolled pain, impending pathologic fracture, or impending cord compression – Limited involved fields should be used to limit the impact of irradiation on stem-cell harvest or impact on potential future treatments – Hydration/furosemide, bisphosphonates, (zoledronic acid preferred), steroids +/- calcitonin • Hyperviscosity – Plasmapheresis should be used for symptomatic hyperviscosity • Surgery • Anemia – Orthopedic consultation for long bone fractures, spinal cord compression, or vertebral column instability – Vertebroplasty or kyphoplasty for symptomatic vertebral compression fractures – Consider erythropoietin for anemic patients (guideline-based prescribing) NCCN Guidelines Version 2.2013 Multiple Myeloma. www.nccn.org NCCN Guidelines Version 2.2013 Multiple Myeloma. www.nccn.org Adjunctive Therapy for MM Adjunctive Therapy for MM • Infection • Renal dysfunction – Intravenous immunoglobulin consideration in the setting of recurrent life-threatening infections – Consider pneumococcal and influenza vaccines – Pneumocystis, herpes, and antifungal prophylaxis if high-dose dexamethasone therapy – Herpes zoster prophylaxis for patient treated with bortezomib – Maintain hydration to avoid renal failure – Avoid use of NSAIDs – Avoid IV contrast – Plasmapheresis – Not a contraindication to transplant – Monitor for renal dysfunction with chronic use of bisphosphonates NCCN Guidelines Version 2.2013 Multiple Myeloma. www.nccn.org NCCN Guidelines Version 2.2013 Multiple Myeloma. www.nccn.org 10 Adjunctive Therapy for MM Phase III Thromboprophylaxis • Thromboembolism – Prophylactic anticoagulation recommended for patients receiving thalidomide-based or lenalidomide with dexamethasone therapy • MM patients receiving a thalidomide-based regimen (n=667) • Regimen-specific risk • Primary endpoint: Rate of thromboembolic/ acute cardiac events or sudden death in first 6 months of treatment – Thalidomide 200 mg/day with Dex 40 mg daily days 1-4, 9-12, 17-20 (high dose Dex) – 17% – Lenalidomide 25 mg/day days 1-21 of 28 with high dose Dex – 26% – Lenalidomide 25 mg/day days 1-21 of 28 with Dex 40 mg PO weekly – 12% Rajukumar SV et al. J Clin Oncol. 2006; 24:431-6. Rajukumar SV et al. Lancet Oncol. 2010; 11:29-37. NCCN Guidelines Version 2.2013 Multiple Myeloma. www.nccn.org Aspirin 100 mg/day Warfarin 1.25 mg/day Enoxaparin 40 mg/day Palumbo A et al. J Clin Oncol. 2011; 29:986-93. Efficacy First 6 months Entire follow-up R A N D O M I Z E Skeletal-related Events Aspirin (n = 220) Warfarin (n = 220) Enoxaparin (n = 219) 6.4% 8.2% 5% 8.6% 10% 7.8% • • • • • • Differences were not statistically different. Median follow up was 24.9 months Palumbo A et al. J Clin Oncol. 2011; 29:986-93. Which of these is most appropriate for a patient with MM taking monthly bisphosphonates who requires a tooth extraction? Hypercalcemia of malignancy Pathologic fracture Bone pain Spinal cord compression Radiation therapy to the bone Bone surgery Body JJ. Support Care Cancer. 2006; 14:408-18. Osteonecrosis of the Jaw ? • Resembles “osteoradionecrosis” • Consistent with localized vascular insufficiency • Associated with use of higher-potency bisphosphonates A. Continue monthly bisphosphonate uninterrupted B. Discontinue bisphosphonate permanently C. Switch to alternate bisphosphonate D. Hold bisphosphonate for several months – Especially zoledronic acid Woo SB et al. Ann Intern Med. 2006; 144:753-61. 11 Osteonecrosis of the Jaw: Risk Factors Associated comorbidities Cancer Corticosteroid use Hypercoagulability Diabetes Osteonecrosis of the Jaw: Treatment • Dental care before or during bisphosphonate therapy • Antibiotics • Surgical debridement • Pain control • Discontinuation of bisphosphonate Common risk factors Bisphosphonate type Bisphosphonate total dose Dental disease Dunstan CR et al. Nat Clin Pract Oncol. 2007; 4:42-55. Woo SB et al. Ann Intern Med. 2006; 144:753-61. Migliorati CA et al. Cancer. 2005; 104:83-93. Enlarged version on page 14 Enlarged version on page 14 Adjusting Therapy for End-organ Dysfunction Secondary Primary Malignancies 2nd Study N % with second malignancy Median time to malignancy Retrospective single site 589 3 35 months Randomized, phase III, lenalidomide vs. placebo maintenance post HSCT 614 5.5 - L 1 - placebo 44 months Randomized, phase III, lenalidomide vs. placebo maintenance post HSCT 460 6.5 - L 2 - placebo 17.5 months post HSCT Randomized, phase III, lenalidomide vs. placebo maintenance post MPL 459 3.9 - L 1.3 - placebo 25 months Retrospective single site 279 3.5 354 days (Imid) 415 days (no Imid) Hasskarl et al. Leuk Lymphoma. 2011; 52:247-59; Attal M et al. Blood. 2010; 116:310; McCarthy PL et al. Blood. 2010; 116:37; Palumbo A et al. Blood. 2010; 116:310; Ormerod A et al. Clin Lymphoma Myeloma Leuk. 2012; 12:113-7. Conclusion • Acceptable treatment options are available for patients with refractory MM • Factors such as response with prior therapy and medical comorbidities should be weighed when selecting a salvage regimen for MM • Patients with MM require supportive care during active treatment that can be managed by experienced pharmacists 12 Drug Primary route of metabolism Recommendations for dosage modification Melphalan Hydrolysis Yes – reduce dose in HSCT conditioning to 140 mg/m2 Thalidomide Renal None Lenalidomide Renal Adjust dose with CrCl < 60 mL/min Pomalidomide Hepatic None (not well studied in hepatic and renal dysfunction) Bortezomib Hepatic Yes – reduce for elevated bilirubin Carfilzomib Peptidase cleavage None and epoxide hydrolysis Bisphosphonates Renal Yes - renal Definition of Progression Progression Increase in 25% or more from lowest response value in any one or more of the following: Serum M-component (absolute increase must be ≥ 0.5 g/dL) Urine M-component (absolute increase must be ≥ 200 mg per 24 hours) Only in patients without measureable serum and urine M-protein levels: the difference between involved and uninvolved free light chains levels (absolute increase must be > 10 mg/L) Bone marrow plasma cell percentage (absolute percentage must be ≥ 10%) Definite development of new bone lesions or soft tissue plasmacytomas or definite increase in the size of existing bone lesions or soft tissue plasmacytomas Development of hypercalcemia (corrected serum calcium > 11.5 mg/dL) that can be attributed solely to the plasma cell proliferative disorder Durie BGM et al. Leukemia. 2006; 20:1467-73. Salvage Therapy Options Preferred regimens Other regimens Repeat primary induction (if relapse at > 6 months) Bortezomib Bortezomib, dexamethasone Bortezomib, lenalidomide, dexamethasone Bortezomib, liposomal doxorubicin Bortezomib, thalidomide, dexamethasone Carfilzomib Cyclophosphamide, bortezomib, dexamethasone Dexamethasone, cyclophosphamide, etoposide, cisplatin Dexamethasone, thalidomide, cisplatin, doxorubicin, cyclophosphamide, etoposide ± bortezomib High-dose cyclophosphamide Lenalidomide, dexamethasone Pomalidomide, dexamethasone Thalidomide, dexamethasone Bendamustine Bortezomib, vorinostat Lenalidomide, bendamustine, dexamethasone NCCN Guidelines Version 2.2013 Multiple Myeloma. www.nccn.org 13 Secondary Primary Malignancies Study N % with second malignancy Median time to 2nd malignancy Retrospective single site 589 3 35 months Randomized, phase III, lenalidomide vs. placebo maintenance post HSCT 614 5.5 - L 1 - placebo 44 months Randomized, phase III, lenalidomide vs. placebo maintenance post HSCT 460 6.5 - L 2 - placebo 17.5 months post HSCT Randomized, phase III, lenalidomide vs. placebo maintenance post MPL 459 3.9 - L 1.3 - placebo 25 months Retrospective single site 279 3.5 354 days (Imid) 415 days (no Imid) Hasskarl et al. Leuk Lymphoma. 2011; 52:247-59; Attal M et al. Blood. 2010; 116:310; McCarthy PL et al. Blood. 2010; 116:37; Palumbo A et al. Blood. 2010; 116:310; Ormerod A et al. Clin Lymphoma Myeloma Leuk. 2012; 12:113-7. Adjusting Therapy for End-organ Dysfunction Drug Primary route of metabolism Recommendations for dosage modification Melphalan Hydrolysis Yes – reduce dose in HSCT conditioning to 140 mg/m2 Thalidomide Renal None Lenalidomide Renal Adjust dose with CrCl < 60 mL/min Pomalidomide Hepatic None (not well studied in hepatic and renal dysfunction) Bortezomib Hepatic Yes – reduce for elevated bilirubin Carfilzomib Peptidase cleavage None and epoxide hydrolysis Bisphosphonates Renal Yes - renal 14 Multiple Myeloma: Current Approaches to Managing Relapse and Refractory Disease SELECTED REFERENCES 1. Anderson KC. Therapeutic advances in relapsed or refractory multiple myeloma. J Natl Compr Canc Netw. 2013; 11:676-9. 2. Anderson KC. The 39th David A. Karnofsky lecture: bench-to-bedside translation of targeted therapies in multiple myeloma. J Clin Oncol. 2012; 30:445-52. 3. Attal M, Lauwers-Cances V, Marit G et al. Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. N Engl J Med. 2012; 366:1782-91. 4. Body JJ. Bisphosphonates for malignancy-related bone disease: current status, future developments. Support Care Cancer. 2006; 14:408-18. 5. Dimopoulos M, Spencer A, Attal M et al. Lenalidomide plus dexamethasone for relapsed or refractory multiple myeloma. N Engl J Med. 2007; 357:2123-32. 6. Dunstan CR, Felsenberg D, Seibel MJ. Therapy insight: the risk and benefits of bisphosphonates for the treatment of tumor-induced bone disease. Nat Clin Pract Oncol. 2007; 4:42-55. 7. Durie BGM, Harousseau JL, Miguel JS et al. International uniform response criteria for multiple myeloma. Leukemia. 2006; 20:1467-73. 8. Hasskarl J, Ihorst G, De Pasquale D et al. Association of multiple myeloma with different neoplasms: systemic analysis in consecutive patients with myeloma. Leuk Lymphoma. 2011; 52:247-59. 9. Kropff M, Bisping G, Schuck E et al. Bortezomib in combination with intermediate dose dexamethasone and continuous low-dose oral cyclophosphamide for relapsed multiple myeloma. Br J Haematol. 2007; 138:3307. 10. Leleu X, Attal M, Arnulf B et al. Pomalidomide plus low-dose dexamethasone is active and well tolerated in bortezomib and lenalidomide-refractory multiple myeloma: Intergroupe Francophone du Myelome 2009-02. Blood. 2013; 121:1968-75. 11. McCarthy PL, Owzar K, Hofmeister CC et al. Lenalidomide after stem cell transplantation for multiple myeloma. N Engl J Med. 2012; 366:1770-81. 12. Migliorati CA, Schubert MM, Peterson DE et al. Bisphosphonate-associated osteonecrosis of mandibular and maxillary bone: an emerging oral complication of supportive care cancer therapy. Cancer. 2005; 104:83-93. 13. National Comprehensive Cancer Network. Recent Updates to NCCN Clinical Practice Guidelines in Oncology Version 2. 2013. http://www.nccn.org/professionals/physician_gls/recently_updated.asp (accessed 9 Aug 2013). 14. Niesvizky R, Martin TG III, Bensinger WI et al. Phase Ib dose-escalation study of carfilzomib, lenalidomide, and low-dose dexamethasone in relapsed or progressive multiple myeloma. Clin Cancer Res. 2013; 19:224856. 15. Orlowoski RZ, Nagler A, Sonneveld P et al. Randomized phase III study of pegylated liposomal doxorubicin plus bortezomib compared to bortezomib alone in relapsed, refractory multiple myeloma: combination therapy improves time to progression. J Clin Oncol. 2007; 25:3892-901. 16. Ormerod A, Fausel CA, Abonour R et al. Observations of second primary malignancy in patients with multiple myeloma. Clin Lymphoma Myeloma Leuk. 2012; 12:113-7. 17. Palumbo A, Cavo M, Bringhen S et al. Aspirin, warfarin or enoxaparin thromboprophylaxis in patients with multiple myeloma treated with thalidomide: a phase III, open-label, randomized trial. J Clin Oncol. 2011; 29:986-93. 15 Multiple Myeloma: Current Approaches to Managing Relapse and Refractory Disease 18. Palumbo A, Hajek R, Delforge M et al. Continuous lenalidomide treatment for newly diagnosed multiple myeloma. N Engl J Med. 2012; 366:1759-69. 19. Petrucci MT, Giraldo P, Corrandini P et al. A prospective, international phase II study of bortezomib retreatment in patients with relapsed multiple myeloma. Br J Haematol. 2013; 160:649-59. 20. Rajkumar SV, Blood E, Vesole D et al. Phase III clinical trial of thalidomide plus dexamethasone compared with dexamethasone alone in newly diagnosed multiple myeloma: a clinical trial coordinated by the Eastern Cooperative Oncology Group. J Clin Oncol. 2006; 24:431-6. 21. Rajkumar SV, Jacobus S, Callander NS et al. Lenalidomide plus high-dose dexamethasone versus lenalidomide plus low-dose dexamethasone as initial therapy for newly diagnosed multiple myeloma: an open-label randomized controlled trial. Lancet Oncol. 2010; 11:29-37. 22. Richardson PG, Sonneveld P, Schuster MW et al. Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N Engl J Med. 2005; 352:2487-98. 23. Richardson PG, Sonneveld P, Shuster M et al. Extended follow-up of a phase III trial in relapsed multiple myeloma: final time-to-event results of the APEX trial. Blood. 2007; 110:3357-60. 24. Siegel DS, Martin T, Wang M et al. A phase II study of single agent carfilzomib (PX-171-003-A1) in patients with relapsed and refractory multiple myeloma. Blood. 2012; 120:2817-25. 25. Weber DM, Chen C, Niesvizky R et al. Lenalidomide plus dexamethasone for relapsed multiple myeloma in North America. N Engl J Med. 2007; 357:2133-42. 26. Woo SB, Hellstein JW, Kalmar JR. Narrative review: bisphosphonates and osteonecrosis of the jaw. Ann Intern Med. 2006; 144:753-61. 16 Multiple Myeloma: Current Approaches to Managing Relapse and Refractory Disease SELF-ASSESSMENT 1. RB, a 71-year old man, was diagnosed with multiple myeloma (MM) five years ago. Over the course of his three-year disease progression, he received bortezomib and dexamethasone for 4 months (induction therapy), high-dose chemotherapy with autologous stem cell transplant, and lenalidomide (maintenance therapy) until his disease progressed. Which of the following therapy options would be most appropriate for RB in the front-line setting of treating relapsed MM? a. b. c. d. 2. Single-agent dexamethasone. Carfilzomib. Melphalan and prednisone. Vincristine, doxorubicin, and dexamethasone. Since beginning his MM therapy, RB has been taking zoledronic acid 4 mg IV monthly to prevent worsening of documented lytic lesions on bone scan. On a regular dental exam, he learned that he needs a tooth extraction. Which of the following would be the most appropriate recommendation regarding RB’s bisphosphonate therapy? a. b. c. d. 4. Continue lenalidomide despite progression. Discontinue lenalidomide and provide patient with a 6-month treatment reprieve. Start treatment with bortezomib and dexamethasone. Offer patient high-dose chemotherapy with allogeneic stem cell transplant regardless of human leukocyte antigen (HLA) matching. Following implementation of your treatment from the preceding question, RB enjoys a period of disease stabilization that lasts 19 months when there is again evidence of disease progression. At this point, what is the most suitable treatment option? a. b. c. d. 3. QUESTIONS Continue monthly bisphosphonate uninterrupted. Discontinue bisphosphonate permanently. Switch to a different bisphosphonate. Hold bisphosphonate for several months. Which of the following regimens should be avoided in a patient with end-stage liver disease? a. b. c. d. Lenalidomide and dexamethasone. Bortezomib and dexamethasone. Thalidomide. Melphalan and prednisone. Answers 1. 2. 3. 4. c b d b 17 Multiple Myeloma: Current Approaches to Managing Relapse and Refractory Disease LIST ADCC APRIL BAFF BAFF-R BSF-3 CLD CrCl ERK FGFR3 HSCT ICAM-1 IGF-1 IL-6 Imid LFA-1 M MM MoAb MPL MTD MUC-1 NF-κB NSAID SDF-1α Smad VCAM-1 VEGF VEGF-R VLA-4 OF ABREVIATIONS antibody-dependent cell-mediated cytotoxicity a proliferation-inducing ligand B-cell activating factor B-cell activating factor receptor B-cell stimulating factor-3 carfilzomib, lenalidomide, dexamethasone creatinine clearance extracellular signal-regulated kinases fibroblast growth factor receptor-3 hematopoietic stem cell transplant intercellular adhesion molecule-1 insulin-like growth factor -1 interleukin-6 immunomodulatory drugs lymphocyte function-associated antigen-1 monoclonal multiple myeloma monoclonal antibodies melphalan, prednisone, lenalidomide maximum tolerated dose mucin-1 nuclear factor κB nonsteroidal anti-inflammatory drug stromal cell-derived factor-1α intracellular proteins that tranduce extracellular signals for the Sma gene vascular cell adhesion molecule-1 vascular endothelial growth factor vascular endothelial growth factor receptor very late antigen-4 18 Multiple Myeloma: Current Approaches to Managing Relapse and Refractory Disease Instructions for Processing CE Credit with Enrollment Code Pharmacists and Technicians: All ACPE accredited activities which are processed on the eLearning site will be reported directly to CPE Monitor. To claim pharmacy credit, you must have your NABP e-Profile ID, birth month, and birth day. If you do not have an NABP e-Profile ID, go to http://www.MyCPEMonitor.net for information and application. Please follow the instructions below to process your CPE credit for this activity. 1. The ASHP eLearning site allows participants to obtain statements of continuing education credit conveniently and immediately using any computer with an internet connection. Type the following link into your web browser to access the e-Learning site: http://elearning.ashp.org/my-activities 2. If you already have an account registered with ASHP, log in using your username and password. If you have not logged in to any of the ASHP sites before and/or are not a member of ASHP, you will need to set up an account. Click on the Register link and follow the registration instructions. 3. Once logged in to the site, enter the enrollment code for this activity in the field provided and click Redeem. Note: The Enrollment Code was announced at the end of the live activity. Please record the Enrollment Code in the grid below for your records. 4. The title of this activity should now appear in a pop-up box on your screen. Click on the Go button or the activity title. 5. Complete all required elements. A green now claim your credit. should appear as each required element is completed. You can 6. Available credit(s) will appear beneath the completed required activities. Look for your profession in the list of available credits and click the appropriate Claim button. You may have to click to see more credit options if you don’t see your profession listed. CPE Credit for Pharmacists and Technicians: To claim continuing pharmacy education (CPE) credit, you will need to enter your NABP e-Profile ID, birth month, and birth day. Once you have entered this information the first time, it will auto fill in the future. Please note: All CPE credit processed on the eLearning site will be reported directly to CPE Monitor. 7. Review the information for the credit you are claiming. If all information appears to be correct, check the box at the bottom and click Claim. You will see a message if there are any problems claiming your credit. 8. After successfully claiming credit, you may print your statement of credit by clicking on Print. If you require a reprint of a statement of credit, you can return here at any time to print a duplicate. Please note that for CPE credit, printed statements may not be necessary because your credit will be reported directly to CPE Monitor. Date of Activity Activity Title Enrollment Code Credit Hours __ /__ /__ Multiple Myeloma: Current Approaches to Managing Relapse and Refractory Disease _____ 1.0 NEED HELP? Contact [email protected] 19