* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Procedures for Administering Injectable Drugs
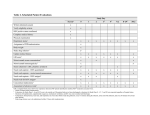
Survey
Document related concepts
Transcript
1 This procedure is adopted for LSW staff from: Livewell Southwest Procedures for Administering Injectable Drugs Version No 4.3 Review: May 2017 Notice to staff using a paper copy of this guidance The policies and procedures page of LSW intranet holds the most recent version of this document and staff must ensure that they are using the most recent guidance. Author: Chief Pharmacist / Clinical Pharmacist Asset Number: 385 1 Procedures for Administering Injectable Drugs Date Version May 2016 Issue 11.4 Purpose The purpose of this document is to inform Trust staff of the correct and safe methods of preparation and administration of injectable drugs. It includes information on the use of infusion devices. Who should read this document? All staff working for or on behalf of Plymouth Hospitals NHS Trust who prepare and administer fluids and drugs by injection or infusion. Key messages Staff working for or on behalf of Plymouth Hospitals NHS Trust who prepare and administer fluids and drugs by injection or infusion must do so in accordance with these procedures. Accountabilities Production Peter Gray, Pharmacist Review and approval Medicines Utilisation and Assurance Committee Ratification Medicines Utilisation and Assurance Committee Dissemination Peter Gray, Pharmacist Compliance Medicines Utilisation and Assurance Committee Links to other policies and procedures Pharmacy documents available on PHNT StaffNet PHNT Medicines Management Policy SOPs for preparing and administering intravenous medicines and fluids. SOPs for the management of phlebitis, infiltraton, air embolism, speedshock and extravasation. SOPs for the safe handling and administration of injectable cytotoxic drugs. SOP for setting up and maintaining variable rate intravenous insulin infusions. PHNT Vascular Access Documents: Administration of Medication through a Central Venous Catheter (CVC) Removal of a Central Line PHNT Central Vascular Access Guidelines PHNT Infection Control Documents: Guidelines for the Management of Peripheral Intravenous Devices Guidelines for the Management of Central Intravenous Catheters Hand Hygeine Guidelines Guidelines for Aseptic Technique Safe Disposal of Sharps Policy Other Documents: Royal College Nursing Standards for Infusion Therapy, 2010 Department of Health High Impact Intervention Care Bundles for- 1 Version History Issue 11.2 (March 2016) The amendment to the phenytoin monograph, to make dilution in saline the preferred method, has been superceded by the amendments in Issue 11.4. Issue 11.3 (April 2016) Monograph for Intravenous Zanamivir added. Issue 11.4 (May 2016) New Monographs for the following medications added: bevacizumab, cetuximab, pertuzumab, ramucirumab and panitumumab, prepared on the ward using a closed-system device. Monographs for ipilimumab, nivolumab, and ofatumumab amended to allow preparation on the ward using a closed-system device. Belatacept – new monograph inserted. Belimumab – new monograph inserted. Tocilizumab – new monograph inserted. Trastuzumab – new monograph inserted In line with the Joint British Diabetes Society guideline for managing diabetic ketoacidosis, and to cover existing practice on Torrington ICU, the following statement has been added to the Potassium Chloride monograph: “In adults, the rate of administration may be increased to 40mmol/hour in the initial management of diabetic ketoacidosis, and if necessary in Cardiothoracic ICU, so long as the patient’s ECG is monitored and resuscitation equipment is available.” Use of oxycodone for Patient Controlled Analgesia (PCA) now included in this monograph. The phenytoin monograph has been amended following a critical incident: the infusion rate for children has been removed, and the instructions “For children, refer to the Paediatric Injection Administration Guide” and “This method, (undiluted infusion) may only be used for adults” have been added. “Where dexamethasone ampoules/vials are labelled for IV, IM, intraarticular, intrabusal or intralesional use, they are suitable (but unlicensed) for subcutaneous administration” has been added to the dexamethasone monograph. Group 8 (Assistant Practitioners) has been added to the groups of staff allowed to administer selected injectable medicines. Added instruction for Savene® (Dexrazoxane) administration: A chemotherapy closed system bag spike should be used with a line adaptor to ensure the safe administration of Savene®. The air inlet port on the bag spike should be opened to allow free flow of Savene®. An air inlet needle should not be used in case of leakage during administration. Rituximab IV infusion monograph amended to reflect additional use to treat lymphoma or leukaemia. Monograph for cisatracurium added as atracurium is intermittently on a manufacturer’s delay. Remifentanil monograph amended to include the Standard Derriford Hospital Protocol for Remifentanil sedation in ICU. Protocol for administering iloprost now included in the monograph. Dexamethasone 1mg is now to be routinely added to each 50ml of ketamine solution for postoperative subcutaneous infusion to reduce tissue irritation. Last Approval Due for Review December 2015 (Updated May 2016) (Extended) May 2017 PHNT is committed to creating a fully inclusive and accessible service. Making equality and diversity an integral part of the business will enable us to enhance the services we deliver and better meet the needs of patients and staff. We will treat people with dignity and respect, actively promote equality and diversity, and eliminate all forms of discrimination regardless of (but not limited to) age, disability, gender reassignment, race, religion or belief, sex, sexual orientation, marriage/civil partnership and pregnancy/ maternity. Larger text, Braille and Audio versions can be made available upon request. An electronic version of this document is available on PHNT StaffNet > Departments > Pharmacy > Injectable Medicines 1 > “Procedures for Administration of Injectable Drug Contents Section 1 2.1 2.2 2.4 2.5 2.6 2.7 Appendix 1 A1.1 A1.2 A1.3 A1.4 A1.5 A1.6 A1.7 A1.8 A1.9 A1.10 A1.11 A1.12 A1.13 A1.14 A1.15 A1.16 Appendix 2 A2.1 A2.2 A2.3 A2.4 Appendix 3 A3.1 A3.2 Appendix 4 A4.1 A4.2 A4.3 Intravenous Drug Calculations Injectable Drug Monographs Chart of Injectable Drug Compatibilities PHNT Protocol for subcutaneous morphine for acute apin in adults PHNT Protocol for administering IV morphine to adults in Acute Care Areas PHNT Protocol for administering IV morphine to adults in the Emergency Dept. PHNT Protocol for subcutaneous ketamine infusion Protocol for administering intramuscular adrenaline 1:1000 (1mg/ml) for treating anaphylaxis, when there is no prescription available Legislation Persons who can be treated under this protocol Anaphylaxis Assessing the patient Explanation of treatment to the patient Patient consent Exclusions from treatment under this protocol Contra-indications to administration of adrenaline to treat anaphylaxis Immediate treatment Source of adrenaline Dosage of adrenaline Adverse Effects Follow up Documentation References Anaphylaxis algorithm Choice of Infusion device Introduction Choice of Infusion device Additional Information References Copy of PHNT Policy for maintenance of patency, flushing and locking of intravascular lines catheters or devices Introduction Policy Document accountability, responsibility and dissemination Accountability Overall Responsibility for These Policies and Guidelines Dissemination and Implementation Page 5 10 195 196 197 198 199 202 202 203 203 204 205 205 205 205 205 205 205 205 205 205 206 207 207 207 207 210 210 212 212 212 1 1 Intravenous Drug Calculations Coverting Between Units Rounding up or down decimals Rounding up or down decimals too early in a calculation can make the final figure inacurate. Only round up or down at the point where you have to measure a volume in a syringe or set a drip rate or an infusion rate on a pump. If a decimal figure is 5 or above, then the preceding decimal figure is rounded up. If a decimal figure is less than 5, then the preceding decimal figure stays as it is (rounded down). Take for example 9.1506ml Your syringe can only measure to one decimal figure so you’ll draw up 9.2ml (the 5 means you round the 1 up to 2) Calculation of the volume of drug to draw up The basic formula for the volume to draw up is: What you want _____________ X Volume in the ampoule What you’ve got Note that the units of “What you want” – i.e. the prescribed dose, and “What you’ve got” – i.e the amount in the ampoule must be the same. You may need to convert the units so that both are mg or both are micrograms for example. 1 Example Your patient has been prescribed gentamicin 350mg IV once daily. Gentamicin ampoules are 80mg in 2ml. What you want (350mg) ____________________ X Volume (2ml amps) What you’ve got (80mg) = 8.75ml which you’ll round up to 8.8ml Concentration, Volume and Amount The Concentration Triangle: Amount Concentration Volume Concentration = Amount Volume Volume = Amount Concentration Amount = Concentration x volume Example Your patient has a low serum magnesium and has been prescribed IV magnesium sulphate 2g. What’s the minimum volume this should be given in? You read the magnesium monograph in the injectable drugs folder and it says “maximum concentration of 200mg/ml” 2g = 2,000mg magnesium Amount (2,000mg) Minimum vol. _______________________ = 10 (ml) Concentration (200mg/ml) Infusion Rate, Volume and Time The Infusion Rate Triangle: Volume Example You have drawn up 8.8ml of gentamicin injection (350mg). As per the injectable drugs folder you dilute this with 100ml saline to make 108.8ml solution, for infusion over 30 minutes. Volume (108.8ml) ________________ =Rate (3.626666ml/minute) Time (30 minutes) Rate Time Rate = Volume Time Volume given = Rate x time Time taken for infusion = Volume Rate You have to set your pump in ml/hour. There are 60 minutes in an hour so multiply 3.6266666ml/minute by 60 to get 217.6ml/hour. You may have to round this figure to 218ml/hour to set your pump. P.S. If the infusion time is in hours then you don’t need to multiply the answer by 60. Also notice that the decimal was only rounded at the final answer. 1 Displacement Values Some, but not all, powdered medications produce a slight expansion of the volume of diluent when they dissolve. The volume by which the diluent expands is called the Displacement Value. When you administer the whole of the dose present in the vial, you draw up the total volume and you don’t need to consider the displacement value. However, if part of the vial is prescribed for a paediatric patient or a patient in renal failure, you should take any displacement value into account. There are a couple of ways of doing this – see the example below. Example A patient is prescribed Co-amoxiclav IV 600mg. The stock vial that you have is 1.2g (1200mg)Bowmed brand. The Injectable Drugs Folder says the displacement value is 0.7ml for this vial (i.e. on dissolution the 20ml expands to 20.7ml). After adding 20ml WFI you would need to withdraw 10.35ml containing 600mg, which cannot be accurately measured. Method 1: Using a 20ml syringe, reconstitute the vial contents with 15ml of WFI, draw the entire contents up into the syringe and then draw up more WFI to the 20ml mark. Mix the syringe contents then give 10ml (containing 600mg) and discard the other 10ml. Method 2: Reconstitute the 1.2g vial contents with 19.3ml WFI (This requires two syringes). The volume in the vial will expand by 0.7ml to 20ml. Then you can draw up 10ml containing 600mg. Calculating a Drip Rate Any fluid containing potassium, magnesium or added drug should be administered using an infusion pump. The only exception to this would be Hartmann’s solution without additional potassium or drugs added. So only plain Normal Saline, 5% Glucose, Hartmann’s or Glucose-Saline can be administered IV using Dosiflows or other gravity-fed administration sets. You can use this drip-rate formula: Example You are asked to set up an infusion of 1 litre Normal Saline to run over the next 8 hours, using a standard drip set. Using the formula: 1000ml x 20 = 20,000 = 41.66 8hours x 60 480 Round 41.66 up to 42 drops/minute Volume (ml) x 20 ______________ = drip rate (drops/minute) Time (hours) x 60 N.B. 20= drops/ml in a standard giving set. (Change to 60drops/ml for a paediatric giving set). 60= number of minutes in an hour. 1 2.1 Injectable Drug Monographs All monographs contained in this section are the current versions as of the time of going to print and are listed in alphabetical order according to generic name. Detailed guidance for the administration of cytotoxic drugs is not given in the monographs, but should be obtained from the appropriate ward or unit protocol. Unlicensed use of medications Where in the monographs the use of a drug is noted to be unlicensed, this either refers to the drug formulation itself not having a UK product licence or where the indication, dosage, dilution or rate of administration fall outside of the UK product licence. When an unlicensed medication is administered to a patient or a licensed medication is administered in an unlicensed manner the prescribing doctor takes full responsibility for any adverse consequences. Important notes Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. This includes infusions such as Patient Controlled Analgesia (PCA) and sliding-scale insulin. Unless described in the drug monograph as “Multidose” all injectable products, including bags of sodium chloride 0.9% and 5% glucose must be treated as single use only and disposed of immediately after use. Any infusion containing drug(s) or potassium or any other additive must be administered using an infusion pump. Dosiflows or other gravity administration sets must only be used for administering crystalloid infusions (eg. Sodium chloride infusion or glucose infusion) containing no potassium or other additives. However, Hartmann’s (which contains 5mmol/L potassium as standard) may be infused using a Dosiflow or other gravity administration set. Hartmann’s with extra potassium added must be pumped. For patients on a variable-rate insulin infusion and glucose infusion, the glucose must be infused using a volumetric pump. Always read the label on the ampoule, syringe or box. Do not rely on familiar colours or shapes of packaging to correctly identify medication. Always label an IV container or syringe containing fluid to which a drug or electrolyte has been added with a completed “Additive Label”. All syringes containing drawn-up medication or flushing solution must be labelled with name of medicine or flushing solution and the dose/strength, unless the risk of doing so (eg contaminating a sterile field) is perceived by the individual practitioner to outweigh the risk of mis-identifying un-labelled syringe(s). The individual practitioner is then responsible for ensuring that any un-labelled syringes are not mis-identified. Labels for this purpose (Code QC31) can be ordered from Pharmacy. Drug solutions that have been drawn up or prepared in clinical areas must be administered immediately after preparation or drawing up. All the intravenous medications listed in the Section 4 monographs may be given via a peripheral cannula or a central venous cannula, unless the monograph specifically says that a particular drug or drug concentration must only be given via a central venous cannula. 1 If you require information on intravenous compatibilities; contact Pharmacy Drug Information on Ext. 39976. Groups of staff allowed to administer injectable medications which are referred to in the monographs: Group 1 o Registered and Provisionally Registered Medical Practitioners. It is recommended that IV drugs are checked by a second person either another medical practitioner or a registered healthcare professional before administration. Group 2 o Registered Nurses, Midwives and Operating Department Practitioners (ODP’s) who have undertaken the Plymouth Hospitals NHS Trust IV drug administration training (or satisfy the criteria for new employees from outside the Trust), and have been assessed as competent. Group 2 can administer to adult patients only. Another Registered healthcare professional should check all aspects of the administration with this Nurse or Midwife. Cytotoxic IV drugs are NOT to be administered by this group. o Exceptions are methotrexate and cyclophosphamide, which can be administered by this group if the practitioner has previous experience of administering parenteral cytotoxics. Group 3 o Nurses who qualify for Group 2, working in identified specialist areas, and have undertaken additional training and assessment to administer cytotoxic IV drugs. Group 4 o o A Registered Sick Children's Nurse (RSCN) or Registered Nurse (Part 15 - Child Branch) working in the paediatric field who qualifies for inclusion in Group 2. The exception is for staff who work regularly in the Emergency Department, Intensive Care Unit, Theatres, Maternity and Neonatal Intensive Care Unit, who can administer Group 2 drugs to paediatric patients, providing they are familiar with the drug and the calculation (if any) required. Group 5 o Nurses who qualify for Group 4 and have undertaken additional training and assessment to administer cytotoxic drugs. Group 6 o Named Individual Radiographers/Sonographers who have completed and passed an accredited training programme in the administration of IV drugs may administer named contrast media, Hyoscine Butylbromide, Sodium Chloride 0.9% and Glucagon via the IV route according to the department’s authorised and signed patient group direction. Group 7 o Named and authorised technical, scientific and delegated medical staff of the department of Nuclear Medicine who have the appropriate training required by IR(ME)R 2000 to administer radiopharmaceuticals and who have completed an accredited course in IV drug administration or equivalent. Such individuals may administer named drugs and radiopharmaceuticals by IV route according to the department’s authorised and signed patient group direction (PGD). o All Registered healthcare professionals must be assessed as competent in the methods required for administration as advised in section 4 monographs. If they have not been assessed as competent with the administration method, e.g. using a central line, or aseptic non-touch technique they must not proceed. 1 o All training and assessment of competency to administer intravenous medication should include training and assessment of aseptic non-touch technique and administration via central vascular access devices. For more information or training please contact the Learning and Development Facilitator. Group 8 o Assistant Practitioners working within PHNT who have received the necessary additional local training on medicines provided by PHNT, and who have been assessed as competent to administer selected oral and parenteral medications in accordance with the Assistant Practitoner Drug Protocols. Abbreviations used in the drug monographs (C) (I) IV IM SC N/S G G/S H Hep/S W Continuous Intermittent Intravenous Intramuscular Subcutaneous Sodium Chloride 0.9% Glucose 5% Glucose 4% and sodium chloride 0.18%. Other combinations of glucose and sodium chloride may not be compatible with the drugs listed in Section 4 – contact Pharmacy for advice on ext.39976. Compound sodium lactate (Hartmann’s) Heparin 10 units in 1ml sodium chloride - heparinised sodium chloride (e.g. Hepsal) Water for Injection (preservative free) DRUG METHOD Abatacept (Orencia®) WHO MAY ADMINISTER OVER GIVE (I) IV infusion via a Groups Infuse all doses over 30 minutes pump. 1 and 2 Infuse via a nonpyrogenic low protein binding filter (0.2-1.2 microns) Abciximab Initial IV bolus Groups 1 minute 1 and 2 (C) IV infusion via Groups pump immediately 1 and 2 following initial IV bolus. Acetazolamide IV bolus Groups 1 and 2 4ml/hour for 12 hours (50ml syringe driver) or 19ml/hour for 12 hours (250ml infusion bag) Suggested maximum 100-500mg/minute INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Reconstitute each 250mg vial with 10ml W using the silicone-free syringe provided. Direct the stream of W down the inside wall of the glass vial. Minimise foam formation by rotating the vial slowly with gentle swirling to dissolve the powder. Do not shake. After dissolution, vent the vial with a needle to dissipate any foam that may be present. Remove a volume of N/S from a 100ml bag N/S equal to the volume of reconstituted vials. Slowly add the reconstituted solution from each vial to the infusion bag using the same silcone-free syringe. Gently mix. Inject 5ml of air into the vial before withdrawing the solution. Use the 20ml syringe to draw up sufficient volume for both the bolus and 12-hour infusion. Connect the 0.2 or 0.22 micron filter and connector provided. Draw the volumes necessary for the bolus dose and infusion into two separate syringes through the connector. See Filter Pack for nomogram. Either dilute the volume drawn up for infusion with N/S or G to make 50ml or add the drawn up volume to 250ml of N/S or G. Reconstitute each 500mg with at least 5ml W. COMMENTS Monitor blood pressure (increase in BP is common), pulse and temperature. Monitor for allergic reactions (rare) and rash (common). Check LFTs (ALT and AST commonly raised). If any serious allergic or anaphylactic reaction occurs discontinue the infusion immediately and initiate appropriate therapy. Do not mix with any other drug solutions. 0.375mmol sodium per 250mg vial Flush with N/S. For stabilisation of unstable angina, bolus dose followed by the infusion is started up to 24 hours prior to PCI and concluded 12 hours after PCI. For other patients bolus is given 1060 minutes prior to PCI followed by the infusion for 12 hours. Do not shake unused vials. Flush: N/S or G. Do not infuse with any other drugs. Flush with N/S or G. Extravasation may cause tissue damage. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 11 DRUG METHOD WHO MAY GIVE Acetylcysteine (C) IV infusion Infusion pump is required. Groups 1 (C) IV infusion via central line Infusion pump is required. Groups 1 ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Treatment of paracetamol overdosage: three consecutive infusions as detailed in the table below (For treating children <40kg follow the instructions on the next 2 pages). and 2 COMMENTS A change in colour of solutions of acetylcysteine to light purple is insignificant. Flush with G or N/S. Sodium content 12.78mmol/10ml . On ICU or HDU acetylcysteine may be infused in smaller volumes of G or undiluted if necessary (unlicensed - see page 7) via a central IV line. However the hourly infusion rate (ml/hour) will be different to the figure in the table below. and 2 Adult Dosage Table for Treating Paracetamol Overdose Regimen Infusion Fluid Duration of Infusion Drug Dose Patient’s weight 1 (kg) 40 - 49 50 - 59 60 - 69 70 – 79 80 – 89 90 – 99 100 – 109 ≥ 110 First Infusion 200ml G (or 200ml N/S if G is unsuitable) 1 hour Grams of acetylcysteine to prescribe 150mg/kg 2 Volume (ml) of acetylcysteine to add to 200ml fluid Infusion rate (ml/hour) 6.8 8.4 9.8 11.4 12.8 14.4 15.8 16.6 34 42 49 57 64 72 79 83 234 242 249 257 264 272 279 283 Second Infusion 500ml G (or 500ml N/S if G is unsuitable) 4 hours Grams of acetylcysteine to prescribe 50mg/kg 2 Volume (ml) of acetylcysteine to add to 500ml fluid Infusion rate (ml/hour) 2.4 2.8 3.4 3.8 4.4 4.8 5.4 5.6 12 14 17 19 22 24 27 28 128 129 129 130 131 131 132 132 Third Infusion 1000ml G (or 1000ml N/S if G is unsuitable) 16 hours Grams of acetylcysteine to prescribe 100mg/kg 2 Volume (ml) of acetylcysteine to add to 1000ml fluid Infusion rate (ml/hour) 4.6 5.6 6.6 7.6 8.6 9.6 10.6 11 23 28 33 38 43 48 53 55 64 64 65 65 65 66 66 66 Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 12 DRUG 1 2 METHOD WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Dose calculations are based on the weight in the middle of each band. If the patient weighs less than 40kg use the paediatric dosage table. Ampoule volume has been rounded up to the nearest whole number. Acetylcysteine for treating paracetamol overdose in Children Children are treated with the same doses and regimen as adults. However, the quantity of intravenous fluid used has been modified to take into account age and weight, as fluid overload is a potential danger. Doses should be administered sequentially using an appropriate infusion pump. Preparation and administration of paediatric infusions Weigh the child to determine the correct weight band. Read off the table (on the next page) the total infusion volume required for each dose according to the weight of the child and make up the solutions according to the directions below. First Infusion Prepare the appropriate volume for the weight of the child. Prepare a 50 mg/mL solution by diluting acetylcysteine (200 mg/mL) with glucose 5% (preferred) or sodium chloride 0.9% as follows: Weight 1-14kg add 10mls of acetylcysteine to 30ml of diluent Weight 15-24kg add 20mls of acetylcysteine to 60ml of diluent Weight 25-39kg add 30mls of acetylcysteine to 90ml of diluent The dose is infused over 1 hour at the infusion rate stated in the table (equiv to 3ml/kg/hour). Second Infusion Prepare the appropriate volume for the weight of the child. Prepare a 6.25 mg/mL solution by diluting acetylcysteine (200 mg/mL) with glucose 5% (preferred) or sodium chloride 0.9% as follows: Weight 1-9kg add 8mls of acetylcysteine 200mg/ml to a 250ml bag Weight 10-19kg add 16mls of acetylcysteine 200mg/ml to a 500ml bag Weight 20-39kg add 32mls of acetylcysteine 200mg/ml to a 1000ml bag The dose is infused over 4 hours at the infusion rate stated in the table (equiv to 2ml/kg/hour). Third Infusion Use the solution prepared under second infusion above. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 13 The dose is infused over 16 hours at the infusion rate stated in the table (equiv to 1ml/kg/hour). For example for a child weighing 12 kg, the first infusion would be 38 mL infused at 38 mL/h over 1 hour,the second infusion would be 100 mL infused at 25 mL/h over 4 hours and the third infusion is 208 mL infused at 13 mL/h over 16 hours. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 14 Weigh the child and prepare the infusion as instructed on the previous page. Paediatric Dosage Table for Treating Paracetamol Overdose Regimen Infusion Infusion rate 1 Patient’s weight (kg) First Infusion 50mg/ml for 1 hour 3ml/kg/hour Dose of Total infusion Infusion rate acetylcysteine volume (ml/hour) to prescribe (ml) 3 6 9 12 15 18 21 24 3 6 9 12 15 18 21 24 Second Infusion 6.25mg/ml for 4 hours 2ml/kg/hour Dose of Total infusion Infusion rate acetylcysteine volume (ml/hour) to prescribe (ml) 1 2 3 4 5 6 7 8 9 150mg 300mg 450mg 600mg 750mg 900mg 1.05g 1.2g 50mg 100mg 150mg 200mg 250mg 300mg 350mg 400mg 1.35g 27 27 450mg 10-14 15-19 20-24 25-29 30-34 35-39 1.9g 2.65g 3.4g 4.15g 4.9g 5.65g 38 53 68 83 98 113 38 53 68 83 98 113 625mg 875mg 1.125g 1.375g 1.625g 1.875g 8 16 24 32 40 48 56 64 Third Infusion 6.25mg/ml for 16 hours 1ml/kg/hour Dose of Total infusion Infusion rate acetylcysteine volume (ml/hour) to prescribe (ml) 2 4 6 8 10 12 14 16 100mg 200mg 300mg 400mg 500mg 600mg 700mg 800mg 16 32 48 64 80 96 112 128 1 2 3 4 5 6 7 8 72 18 900mg 144 9 100 140 180 220 260 300 25 35 45 55 65 75 1.3g 1.8g 2.3g 2.8g 3.3g 3.8g 208 288 368 448 528 608 13 18 23 28 33 38 1 Dose calculations based on the weight in the middle of each band. If the patient weighs more than 40kg use the adult dosage table. Figures have been rounded up to the nearest whole number. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 15 DRUG METHOD Aciclovir (Ready-diluted brands) (I) IV infusion Infusion pump is required. Aciclovir (Powder for reconstitution) (I) IV infusion Infusion pump is required. Actrapid® Adenosine ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Dilute each 250-500mg in a 100ml bag 1 hour Groups N/S, G/S or H. For doses between 1,2,3,4 and 5 500mg and 1000mg use two 100ml bags or one 250ml bag. The concentration should not exceed 5mg/ml. Shake the prepared infusion well before use. COMMENTS 1 hour Flush with N/S, G/S or H. Sodium content approx 1mmol/250mg. Discard infusion if any visible turbidity or crystallisation appears. Extravasation may cause tissue Reconstitute each 250mg with 10ml of W damage. Patient should be adequately hydrated. or N/S to produce a solution containing 25mg/ml. Dilute further with N/S, G/S or H to a concentration not exceeding 5mg/ml. For fluid restricted patients the reconstituted solution may be infused without further dilution via a central IV line. See Insulin Section page IV bolus Group 1 2 seconds Can be diluted with N/S if necessary. Group 1 6 minutes (I) IV infusion for cardiac stress testing Infusion pump is required. WHO MAY GIVE Groups 1,2,3,4 and 5 and Group 7 If given into an IV line, inject as proximally as possible and follow with a rapid N/S flush. Cardiac monitoring and resuscitation equipment should be available for immediate use. Sodium content 0.154mmol/3mg. Administer in accordance with the Nuclear Medicine Department protocol. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 16 DRUG METHOD WHO MAY GIVE ADMINISTER OVER Adrenaline (Epinephrine) (C) IV infusion Infusion pump is required. . Groups 1 Adjust rate according to response. and 2 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Usual local practice on General ICU is to use 1:10,000 adrenaline in a 50ml syringe (5mg in 50ml). Usual dilution on Torrington ICU is 2mg diluted to 50ml with G. Emergency use in CPR: IV bolus Group 1 Emergency use in anaphylaxis IM Injection using 1:1,000 injection All groups Refer to the Marsden Manual for guidance on IM injection. Emergency use in anaphylaxis – IV route is only used in an acute hospital setting by an experienced practitioner for a patient with immediately lifethreatening profound shock. Group 1 Use 1:10,000 injection or dilute 0.5ml of 1:1,000 adrenaline to 5ml with N/S or G to make a 1:10,000 solution. 1 - 2 seconds Specialist use only: Adults: 0.5ml of dilute Only 1:10,000 adrenaline IV anaesthetists over 1 minute with and senior continuous ECG clinicians monitoring, pulse working in oximety and frequent intensive care, theatre or the blood pressure measurements. Emergency Repeat dose as Department. necessary according to response COMMENTS Protect infusion from light. If G used as diluent pH must be below 5.5 (pH of G stocked in this Trust is between 4-4.2). Infuse through a large vein if possible. (I) IV infusion requires continuous blood pressure monitoring. Replace giving set - do not flush. Extravasation may cause tissue damage. Note that 1mg ampoules are only licensed for IM or SC use. However, they are suitable for preparing an IV infusion. Use 1:10,000 (1mg in 10ml) prefilled syringe. Refer to the algorithm for the management of suspected lifethreatening anaphylaxis on page 206. IM is the usual route. If a patient is suffering an anaphylactic reaction, there is no prescription for adrenaline and there is no doctor immediately available to prescribe adrenaline, IM adrenaline can be given by a non-medical member of staff who has the skills to assess a patient and give IM injections. They should do this in accordance with the protocol in Appendix 1 (page 202) Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 17 DRUG METHOD Ajmaline (Unlicensedsee page 7) For diagnosis of Brugada Syndrome Slow IV bolus Alcohol See Ethanol monograph Alemtuzumab 30mg vials ▼ This product is being intensively monitored by the CHM and MHRA. Please report all suspected reactions (including nonserious ones) using a Yellow Card from the BNF Post kidney Groups 1 transplant and 2 SC Injection in to the deltoid or anterior abdominal wall. 1-2 minutes For SC injection draw up 1ml (30mg) from the vial into a syringe. Haemopoietic Groups 1 stem cell and 2 transplant (I) IV infusion via an infusion pump 4 hours Draw up 30mg in 1ml using a closed-system device and further dilute with 100ml N/S. WHO MAY GIVE ADMINISTER INSTRUCTION FOR DILUTION OVER AND SUITABLE DILUENT No greater Undiluted Group 1: than junior doctors trained in the 5mg/minute. technique and Maximum with UK ALS dose is accreditation, 1mg/kg or a consultant cardiologist COMMENTS For detailed instructions it is essential to read the Ajmaline Protocol (Copies on Torcross and Bickleigh wards) Patient to be nil-by-mouth for at least 4 hours before the test. Continuous 12-lead ECG monitoring required during administration. Cardiac rhythm monitoring required for 4 hours following administration. Check the blood pressure at 5 minute intervals during administration and for 10 minutes afterwards. Give the following pre-medication 30-60 minutes prior to giving alemtuzumab: Chlorphenamine 10mg IV and paracetamol 1g PO prior to each dose. Post Kidney transplant also give methylprednisolone 500mg IV prior to first dose, 250mg IV prior to second dose. During and after administration monitor for urticaria, rash, hypotension, nausea, rigors and fever. Serious but rare reactions include: respiratory distress, bronchospasm, syncope, MI and cardiac arrest. Women who are pregnant or trying to become pregnant should not prepare or administer alemtuzumab. Although the packaging states “Concentrate for solution for infusion”, this product can be given by subcutaneous injection. For IV infusion, alemtuzumab can be diluted in 100ml G instead of N/S if there is a need to do this. Note that 30mg/ml alemtuzumab is an unlicensed product (see page 7). Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 18 DRUG METHOD WHO MAY ADMINISTER GIVE OVER (I) IV Groups 4 hours infusion via 1 and 2 an infusion pump INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Withdraw 1.2 ml (12mg) of solution from the vial into a syringe. Inject into 100ml N/S. The bag should be inverted gently to mix the solution. Alemtuzumab 12mg vials For Multiple Sclerosis ▼ This product is being intensively monitored by the CHM and MHRA. Please report all suspected reactions (including nonserious ones) using a Yellow Card from the BNF Premedication prior to alemtuzumab for treating Multiple Sclerosis (Allow 30 minutes for oral paracetamol to take effect). Paracetamol 1gram PO Chlorphenamine 10mg IV Methylprednisolone IV – see below COMMENTS Premedication: see administration schedule below. During the infusion monitor for urticaria, rash, hypotension, nausea, rigors and fever. Serious but rare reactions include: respiratory distress, bronchospasm, syncope, MI and cardiac arrest. Refer to the full Alemtuzumab Prescribing Guidelines held on the Planned Investigation Unit (PIU). The guidelines are also available on Plymouth Healthnet under Clinical Guidelines. Women who are pregnant or trying to become pregnant should not prepare or administer alemtuzumab. Alemtuzumab can be diluted in 100ml G instead of N/S if there is a need to do this. 1st Course of alemtuzumab: Alemtuzumab 12mg IV daily for 5 consecutive days – each dose immediately preceded by 500mg IV methylprednisolone over 30 minutes 2nd Course of alemtuzumab (Given 12 and 24 months after the 1st course) Alemtuzumab 12mg IV daily for 3 consecutive days – each dose immediately preceded by 1g IV methylprednisolone over 1hour Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 19 DRUG METHOD WHO MAY GIVE Alfacalcidol IV bolus Groups 1 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Shake the ampoule for a minimum of 5 seconds before use. Give undiluted. COMMENTS For patients undergoing haemodialysis the injection should be given into the return line from the haemodialysis machine at the end of dialysis. Monitor serum calcium regularly during treatment. Staff prescribing, administering and/or screening prescriptions for opioid medications should be familiar with the PHNT Policy for Reducing Errors with Opioid Medicines in Adults using the following link: http://staffnet.plymouth.nhs.uk/Portals/1/Documents/Trust%20Documents/Medicines%20Management/Policy%20for%20Reducing%20Do sing%20Errors%20with%20Opioid%20Medicines%20in%20Adults.pdf?timestamp=1443106367868 Flush : N/S, G or H IV bolus Can be diluted with N/S, G or H. Groups 1 Approximately Anaesthesia: Adequate plasma levels will 30 seconds in using the and 2 only be achieved rapidly if the infusion (0.5-1 spontaneously 500 microgram/ml micrograms/kg/minute) is preceded by a breathing injection loading dose of 50-100 micrograms/kg given patients. as a bolus or fast infusion over 10 minutes. Ampoules of Alfentanil 5mg/ml are 5000 micrograms/ml and must be diluted as and 2 Alfentanil ADMINISTER OVER Approximately 30 seconds below before administration by infusion. (C) or (I) IV infusion with assisted ventilation. Infusion pump is required. Groups 1 SC injection Groups and 2 1,2,3,4 and 5 (C) SC infusion via Groups syringe driver for 1,2,3,4 and 5 use in palliative care Dilute with N/S, G or H to a usual concentration of 0.5mg/ml. Occasionally concentrations of 1mg/ml or more have been used. Follow the PHNT Care of the Dying Pathway in Advance Kidney Disease and the PHNT Syringe Driver Policy. Dilute with W when 2 or more For combinations of 2 or 3 drugs in the same drugs are being mixed in the same syringe refer to the compatibility charts in the syringe. pump kit or contact Pharmacy on ext. 39976 W or N/S may be used when the for advice. Alfentanil is unlicensed by the SC syringe only contains this drug. route and for use in palliative care (See page 7). Refer to the Marsden Manual for guidance on SC injection. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 20 DRUG METHOD Alglucosidase alfa (Mycozyme®) (I) IV infusion Groups Infusion 1,2 and 3 pump is required. WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Remove the required number of vials Initial rate of from the fridge and allow them to reach 1mg/kg/hour. room temperature (may take about 30 Gradually increased by 2mg/kg/hour every minutes). Reconstitute each 50mg vial 30 minutes if there are with 10.3ml W. Add the W by slow dropwise addition down the side of the vial no reactions to the and not directly in to the powder. Tilt infusion, until a and roll each vial gently. Do not invert, maximum rate of swirl or shake the vials. The 7mg/kg/hour is reconstituted volume is 10.5ml reached. containing 5mg of enzyme/ml, and appears as a clear colourless to pale yellow solution which may contain particles in the form of thin white strands or translucent fibres. If on immediate inspection foreign particles other than those described above are observed, or if the solution is discoloured, do not use. Dilute the drawn up dose of alglucosidase alfa with N/S to a final alglucosidase alfa concentration of 0.5mg/ml to 4mg/ml (Remove the same volume of N/S from the bag first). Remove airspace from within the bag. Mix with gentle massage on inversion of the bag. Do not shake or agitate the bag. Infuse the solution via a 0.2micron low protein-binding in-line filter. COMMENTS Suitable filters include PALL 0.22 micron, Braun Sterifix 0.2 micron, Technopharm codan 0.2 micron filters. These filters should be ordered through ORACLE. Instructions for dosing and administration of alglucosidase alfa will usually be included in the patient’s treatment plan (Recommended dosage for Pompe Disease is 20mg/kg once every 2 weeks) During the infusion monitor for allergic reactions, monitor blood pressure, pulse, temperature, respiratory rate and for difficulty in breathing. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 21 DRUG METHOD WHO MAY ADMINISTER OVER GIVE INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Alprostadil (Prostin VR®) (C) IV infusion Groups Dilute 150micrograms/kg weight of baby to a final volume of 50ml with G, N/S or G10%. (Note that after dilution with G10% the product is unlicensed. See page 7) 1 and 2 Infusion pump is required. Alprostadil (Caverject®) Intracavernosal Group 1 injection (See comments) Initial rate: 5 nanograms/kg/minute = 0.1ml/hour of the prepared dilution. COMMENTS If using a burette avoid direct contact of the undiluted injection with the wall of the plastic burette. If this happens the appearance of the burette chamber may change and a hazy solution may develop requiring the solution to be discarded and the burette to be changed. Monitor arterial blood pressure, heart rate, SaO2 pO2 pH and respiratory rate Fit the 22 gauge needle to the syringe. Using a half inch, 27 to 30 gauge needle is generally recommended. Inject the 1ml of diluent into the vial, The intracavernosal injection must and shake to dissolve the powder be done with aseptic technique. entirely. Withdraw slightly more than the required dose of Caverject solution, The site of injection is usually along the dorsolateral aspect of the remove the 22 gauge needle, and fit the 30 gauge needle. Adjust volume to proximal third of the penis. Visible veins should be avoided. Both the the required dose for injection. side of the penis that is injected and the site of injection must be alternated. Prior to the injection, the injection site must be cleansed with an alcohol swab. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 22 DRUG METHOD WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS If a special pre-programmed alteplase pump is unavailable then refer to the guidance on pages 24 and 25. ECG and haemodynamic Initial IV bolus Accelerated Reconstitute two 50mg vials each with Groups monitoring required. Sodium dose then (I) IV regimen initiated the 50ml of W provided using the transfer 1 and 2 content nil. infusion within 6 hours of needles supplied. Agitate gently until the Acute myocardial Flush with N/S. symptom onset contents of the vials have dissolved. Do using the infarction (AMI) administer over: not shake. special preWhen treating AMI, alteplase is programmed 90 minutes When using the special pre-programmed given together with IV heparin. The alteplase pump Initiated between 6 alteplase pump, draw up the contents of IV heparin regimen is 5,000unit (Available in the and 12 hours after both vials (100ml) into a 100ml syringe. bolus followed by a continuous IV Emergency infusion for at least 48 hours, using symptom onset Dept. and on the standard PHNT IV heparin administer over: Torcross ward). prescription form. 3 hours Alteplase and heparin infusions are not compatible. They should be infused through separate IV catheters. If IV access is a problem, the infusion of heparin can be commenced once the alteplase infusion has finished. ECG and haemodynamic Alteplase (TPA) Initial IV bolus Reconstitute two 50mg vials each with Group 1 1 – 2 minutes to treat: dose the 50ml of W provided using the transfer monitoring required. Sodium needles supplied. Agitate gently until the content nil. Followed by (I) IV Groups 2 hours contents of the vials have dissolved. Do Flush with N/S. infusion 1 and 2 Pulmonary not shake. Alteplase and heparin infusions are using the embolism special preDraw up the 10mg (10ml) bolus in a 10ml not compatible. They should be infused through separate IV programmed syringe for the doctor to inject over 1-2 catheters. alteplase pump minutes. (Available in the When using the special pre-programmed Emergency alteplase pump, draw up the remainder Dept. and on of the total dose into a 100ml syringe. Torcross ward) Alteplase (TPA) to treat: Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 23 Alteplase to treat Acute Myocardial Infarction within 6 hours of symptom onset (Accelerated Regimen) Suggested method when a pre-programmed alteplase pump is not available: Reconstitute two 50mg vials each with 25ml of the W provided using the transfer needles provided to make a 2mg/ml solution. Draw up the 50ml (100mg) of solution into a 50ml syringe. Then using a syringe pump set the infusion rate as follows: Bolus of 15mg over 2 minutes for patients of all weights (Set the pump at 225ml/hour for 2 minutes) then: Patient weight Further doses and infusion rates ≥ 65kg 50mg over 30 minutes. Set the pump at 50ml/hour for 30 minutes then 35mg over 60 minutes. Set the pump at 17.5ml/hour for 60 minutes 64kg 48mg over 30 minutes. Set the pump at 48ml/hour for 30 minutes then 32mg over 60 minutes. Set the pump at 16ml/hour for 60 minutes 62kg 46.5mg over 30 minutes. Set the pump at 46.5ml/hour for 30 minutes then 31mg over 60 minutes. Set the pump at 15.5ml/hour for 60 minutes 60kg 45mg over 30 minutes. Set the pump at 45ml/hour for 30 minutes then 30mg over 60 minutes. Set the pump at 15ml/hour for 60 minutes 58kg 43.5mg over 30 minutes. Set the pump at 43.5ml/hour for 30 minutes then 29mg over 60 minutes. Set the pump at 14.5ml/hour for 60 minutes 56kg 42mg over 30 minutes. Set the pump at 42ml/hour for 30 minutes then 28mg over 60 minutes. Set the pump at 14ml/hour for 60 minutes 54kg 40.5mg over 30 minutes. Set the pump at 40.5ml/hour for 30 minutes then 27mg over 60 minutes. Set the pump at 13.5ml/hour for 60 minutes 52kg 39mg over 30 minutes. Set the pump at 39ml/hour for 30 minutes then 26mg over 60 minutes. Set the pump at 13ml/hour for 60 minutes 50kg 37.5mg over 30 minutes. Set the pump at 37.5ml/hour for 30 minutes then 25mg over 60 minutes. Set the pump at 12.5ml/hour for 60 minutes 48kg 36mg over 30 minutes. Set the pump at 36ml/hour for 30 minutes then 24mg over 60 minutes. Set the pump at 12ml/hour for 60 minutes 46kg 34.5mg over 30 minutes. Set the pump at 34.5ml/hour for 30 minutes then 23mg over 60 minutes. Set the pump at 11.5ml/hour for 60 minutes Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 24 Alteplase to treat Acute Myocardial Infarction between 6 and 12 hours after onset of symptoms Suggested method when a pre-programmed alteplase pump is not available: Reconstitute two 50mg vials each with 25ml of the W provided using the transfer needles provided to make a 2mg/ml solution. Draw up the 50ml (100mg) of solution into a 50ml syringe. Then using a syringe pump set the infusion rate as follows: Bolus of 10mg over 2 minutes for patients of all weights.: set the pump at 150ml/hour for 2 minutes, then: 50mg over 1 hour for patients ≥ 40kg: set the pump at 25ml/hour for 1 hour, then: Patient weight Dose and infusion rate ≥ 65kg 40mg over 2 hours. Set the pump at 10ml/hour for 2 hours 60 - 64kg 30mg over 2 hours. Set the pump at 7.5ml/hour for 2 hours 53.4 -63.9kg 20mg over 2 hours. Set the pump at 5ml/hour for 2 hours 46.7 – 53.3kg 10mg over 2 hours. Set the pump at 2.5ml/hour for 2 hours 40 – 46.6kg No additional alteplase Alteplase to treat Pulmonary Embolism Suggested method when a pre-programmed alteplase pump is not available: Reconstitute two 50mg vials each with 25ml of the W provided using the transfer needles provided to make a 2mg/ml solution. Draw up the Bolus of 10mg (5ml) in a 5 ml or 10ml syringe for the doctor to inject over 1 -2 minutes Then draw up the remainder of the total dose in a 50ml syringe. Then using a syringe pump set the infusion rate as follows: Patient weight Dose and infusion rate ≥ 65kg 90mg over 2 hours. Set the pump at 22.5ml/hour for 2 hours < 65kg For patients less than 65kg the total prescribed dose (including bolus dose) should not exceed 1.5mg/kg. Following the bolus dose of 10mg, the infusion rate = Total prescribed dose (mg) – Bolus dose (10mg) ml/hour for 2 hours 4 Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 25 DRUG METHOD WHO MAY ADMINISTER GIVE OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Total dose is 900 micrograms/kg (Maximum dose 90mg). 10% of this dose (90micrograms/kg) given as a bolus over 2 minutes IV bolus It is essential to follow the detailed Group 1 1 – 2 minutes Reconstitute one or two 50mg vials each with 50ml of the W provided to instructions in the PHNT Acute Ischaemic make 1mg/ml solution. For the bolus Stroke Protocol (Copy in the Emergency Acute Ischaemic dose, draw up 10% of the total dose Department). Stroke (see table below) and inject using a Unless the patient or companion knows their 10ml syringe. recent weight, estimate to the nearest 5kg. Take (I) IV infusion Groups 1 hour From the solution above, draw up the 2 initial blood pressure readings at 15 minute remainder of total dose (see table intervals. Record in both arms initially to exclude 1 and 2 below) into one or two 50ml syringes. aortic dissection. Alteplase to treat Use 1 x 50mg vial Use 2 x 50mg vials Weight(Kg) Weight (Imperial) Total dose 900micrograms/kg (Maximum 90mg) Bolus dose (ml) Inject over 1 -2 minutes Infusion dose infused over 1 hour 45 7st 1lb 40 4 36 50 7st 12lb 45 4.5 40.5 55 8st 9lb 49 4.9 44.1 60 9st 6lb 54 5.4 48.6 65 10st 3lb 58 5.8 52.2 70 11st 0lb 63 6.3 56.7 75 11st 11lb 67 6.7 60.3 80 12st 8lb 72 7.2 64.8 85 13st 5lb 76 7.6 68.4 90 14st 2lb 81 8.1 72.9 95 14st 13lb 85 8.5 76.5 ≥100 15st 10lb 90 9 81 Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 26 DRUG METHOD WHO MAY ADMINISTER GIVE OVER Alteplase (Low-Dose) to treat acute venous thrombosis (subclavian or ilio-femoral deep vein thrombosis) (C) IV Infusion Groups INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Reconstitute 1 x 10mg alteplase with the 10ml of W provided. 1,2,3,4 and Further dilute the 10mg of 5 This will deliver reconstituted alteplase to 50ml 0.5mg alteplase with N/S. per hour 2.5ml/hour This indication for alteplase is unlicensed – see page 7 Amikacin IM injection Slow IV bolus (For large once daily doses see (I) IV infusion below) Groups Groups 2 – 3 minutes 1,2,3,4 and 5 (I) IV infusion Groups 30 minutes For once daily doses 1,2,3,4 and of 15mg/kg or greater. 5 Infusion pump is required Irrigation Groups 1,2,3,4 and 5 The minimum stable concentration is 0.2mg/ml. Each prepared infusion is stable upto 8 hours at room temperature. Prepare a fresh syringe and change the infusion promptly, every 8 hours. After 8 hours, 30ml of solution will remain in the used syringe which must be discarded. Follow the Low-Dose Alteplase Protocol. A copy is kept on Torcross ward. Alternatively, a copy has been uploaded onto: StaffNet> Document Library> Clinical Guidelines> Prescribing Regimens 1,2,3,4 and 5 COMMENTS Do not dilute. Refer to the For most infections the intramuscular Marsden Manual for guidance on route is preferred, but the IV route may be IM injection. used for life threatening infection or when IM injection is not feasible. Undiluted Once diluted for infusion use immediately. Patient should be well hydrated during amikacin therapy. A common dilution for adults is with 100ml of N/S or G. Dilute the required dose with N/S Sterile irrigation of amikacin may be used to a concentration of 2.5mg/ml. in abscess cavities, the pleural space, peritoneum or in the cerebral ventricles. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 27 DRUG METHOD WHO MAY GIVE Aminophylline (I) IV infusion Groups 1, (initial loading 2 3 and 7 dose) Infusion pump is required. (I) or (C) IV infusion (after loading dose). Infusion pump is required. Groups ADMINISTER OVER Minimum 20 minutes. INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Dilute further with 100ml N/S, G, G/S or H. However, the loading dose can be diluted to a smaller volume e.g. 50ml or given undiluted (25mg/ml) if necessary. COMMENTS Flush with N/S, G or G/S. Do not give loading dose if patient previously taking theophylline. Usual starting rates: Remove 20ml from a 500ml bag of N/S, Do not infuse aminophylline down G, G/S or H then add 500mg (20ml) the same central line lumen or 1,2,3,4 and 5 peripheral line as salbutamol. aminophylline to make a concentration of 0.5-0.7mg/kg/hour for 1mg/ml. adults and children aged 12 years and older. Take blood to check theophylline Can be diluted to higher concentrations levels 4-6 hours after commencing 0.3mg/kg/hour for the than 1mg/ml or given undiluted the aminophylline infusion. elderly. (25mg/ml) through a central line, but take care with the calculation and prescription 1mg/kg/hour for children of the infusion rate. aged under 12 years. To avoid excessive dosage in obese patients, the dose should be calculated on ideal body weight. Adjust the rate according to plasma theophylline levels. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 28 DRUG METHOD Amiodarone (C) or (I) IV infusion. Infusion pump is required. WHO MAY GIVE ADMINISTER OVER Groups 1,2 5mg/kg loading dose (usually and 3 300mg) over 20 minutes - 2 hours. This may be followed by repeat infusion up to 1.2g per 24 hours. Adjust rate according to response IV bolus Group 1 Emergency use INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Recommended dilution: 5mg/kg loading dose (Usually 300mg) diluted in 100ml or 250ml G. Repeat infusion (usually 900mg over next 23 hours) diluted in 250ml or 500ml G. Where a lower volume is needed the dose (e.g. 300mg, 900mg or 600mg) may be diluted in 50, 100 or 250ml G. Stability is concentration dependent - do not over dilute. Do NOT add 300mg to more than 500ml G or 600mg to more than 1 litre G. During Advanced Dilute each 150-300mg with 10-20ml G. Life Support for Pre-filled syringe contains 300mg ready VF/VT give as a diluted in 10ml G. fast bolus. Otherwise give over a minimum of 3 minutes. Do not repeat dose for at least 15 minutes. COMMENTS Cardiac monitoring required. Flush with G. Avoid peripheral administration unless absolutely necessary as infusion via peripheral veins has lead to local discomfort and inflammation. Infusion concentrations greater than 2mg amiodarone per ml must be infused via a central venous catheter. When repeated or continuous infusion of any concentration is anticipated, administration via a central venous catheter is recommended. Sodium content nil. As soon as an adequate response has been obtained, oral therapy should be initiated concomitantly at the usual loading dose (i.e. 200mg three times a day). Intravenous amiodarone should then be phased out gradually. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 29 DRUG WHO MAY ADMINISTER INSTRUCTION FOR DILUTION AND COMMENTS GIVE OVER SUITABLE DILUENT Amoxicillin is a penicillin – Check patient’s allergy status before administration Flush with N/S. Amoxicillin IV bolus Inject doses up to Reconstitute each 500mg with 10ml W. Groups 1g over 3 4 Displacement 0.4ml/500mg. Add 9.6ml W MRHA Safety Alert 2015: Do not use 1,2,3,4 and 5 (Usual method) minutes. to 500mg to produce 50mg/ml. Wockhardt brand amoxicillin for infants and neonates below one year Inject 2g doses old due to reports of extravasation & slowly over 6 - 8 injection site reactions. Other brands minutes or give by eg. Bowmed and GSK are safe to use infusion (see in this age group. below). (I) IV infusion 30 - 60 minutes Reconstitute as above then dilute with N/S Use infusion within 90 minutes of preparation. via infusion or G to 100ml. Alternatively each 500mg pump amoxicillin may first be reconstituted with Sodium content: 1.65mmol/500mg 10ml of the diluent (N/S or G). (Avoid Intrathecal administration) IM Injection Reconstitute a 500mg vial with 2.5ml W and For Amoxil® brand only: If pain is shake vigorously (Final volume is 2.9ml). experienced on IM injection, lidocaine Reconstitute a 250mg vial with 1.5ml W and 1% or procaine 0.5% injection may be shake vigorously (Final volume is 1.7ml). used instead of W to reconstitute the Refer to the Marsden Manual for guidance vial. on IM injection. Amphotericin (I) IV infusion 2-4 hours. Displacement is negligible. Add 10ml A test dose must be given at start of Groups via infusion diluent for 50mg in 10ml. each new course of treatment; Infuse 1,2,3,4 and 5 Up to 6 hours if (Fungizone® ) pump Reconstitute vial with 10ml W, then dilute the first 1mg of the first infusion over poorly tolerated. dose required with 50 times as much G to 20-30 minutes and observe for signs produce a maximum concentration of of anaphylactic reaction for at least a 100micrograms/1ml. further 30 minutes. If no reaction then give the remainder of the first infusion. Flush with G before and after Concentrations up to a maximum of administration. 500micrograms/1ml can be given using a Protect infusion from light. central line (unlicensed use see page 7). For AMBISOME May cause thrombophlebitis; change see next page infusion site frequently. METHOD Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 30 DRUG METHOD Liposomal Amphotericin (AmBisome ) (I) IV infusion Groups Infusion pump 1,2,3,4 and is required. 5 For Fungizone® See previous page (I) IV infusion Anti-thymocyte into a large globulin rabbit vein. Infusion (ATG rabbit) pump is required. Anidulafungin Aprotinin This drug is unlicensed – see page 7 WHO MAY ADMINISTER GIVE OVER Groups 1,2,3,4 and 5 (I) IV infusion Groups Infusion pump 1,2,3,4 and is required. 5 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS 30-60 minutes Add 12ml W (2-8oC), shake vigorously for at least 15 seconds. Resulting amphotericin concentration 4mg/1ml. Dilute dose required with between 1 and 19 parts by volume G, using 5 micron filter provided, to give a final concentration of 200micrograms-2mg/1ml. At least 6 hours Doctor to prescribe dose in a volume of N/S such that the concentration of the infusion is 0.5mg/ml. Infusion to be prepared by Pharmacy.Telephone Ext.31083. Administration of a test dose is advisable before a new course: Give 1mg of prepared infusion over 10 minutes, stop infusion and observe patient for 30 minutes. Protect infusion from direct sunlight. Flush before and after administration with G. Do not infuse with any other drugs or infusion fluids. Sodium content less than 0.5mmol/vial. A test dose is usually given. Give hydrocortisone 100mg IV, chlorphenamine 10mg IV and paracetamol 1g PO 30-60 minutes before the ATG infusion. Flush with N/S. Do not infuse with any other drugs. Do not infuse with any other drugs or infusion fluids. If the un-reconstituted vials are accidentally left out of the fridge, as long as the period at room temperature does not exceed 96 hours, they can be returned to the fridge and are ok to use. Flush with N/S. Infuse the 200mg dose over at least 3 hours. Reconstitute each 100mg vial with 30ml WFI. Reconstitution can take up to 5 minutes. For the 200mg dose, remove 50ml from a 250ml bag of N/S or G, then add 60ml (2 x 100mg in 30ml) of reconstituted solution (Final Infuse the volume 260ml). 100mg dose For the 100mg dose, add the 30ml of over at least 1½ reconstituted solution to a 100ml bag of N/S or G (final volume 130ml). hours. IV bolus (initial Group 1 Maximum rate Provided ready diluted. loading dose) 10ml/minute (I) IV infusion Groups 1 20-50ml/hour Infusion pump and 2 is required. Flush with N/S. Initial 1ml (10,000 KIU) should always be given at least 10 minutes prior to treatment to test for possible allergic and anaphylactic reactions. Sodium content 7.7mmol/50ml. Do not infuse with any other drugs including heparin. Patient must be in the supine position during the administration of aprotinin. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 31 DRUG METHOD Argatroban WHO MAY ADMINISTER OVER GIVE (I) IV infusion Groups Initial infusion rate in patients via infusion without hepatic impairment is 1 and 2 pump. 2micrograms/kg/minute. INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Add the 250mg in 2.5ml from the vial to a 250ml bag of N/S or G. Mix the solution for 1 minute by repeated inversion of the For critically ill or hepatically prepared infusion. There may be impaired patients the initial infusion some brief haziness of the rate is 0.5micrograms/kg/minute. solution that clears upon mixing. See tables at foot of monograph for setting the initial infusion rate COMMENTS Obtain a baseline APTT. The target APTT is 1.5-3.0 times the baseline value, but not more than 100 seconds. Check the APTT 2 hours after starting the infusion or after a change of rate, and at least once a day thereafter (For critically ill or hepatically impaired patients, check the APTT 4 hours after starting infusion or changing the rate). The maximum rate is 10micrograms/kg/minute APTT (s) Standard dosing schedule Initial Infusion Rate 2 micrograms/kg/minute Infusion Rate change Next APTT Critically Ill/Hepatically impaired patients Initial infusion rate 0.5 micrograms/kg/minute Infusion Rate change Next APTT < 1.5 times baseline Increase by 0.5 mcg/kg/min. 2 hours Increase by 0.1 mcg/kg/min. 1.5-3.0 times baseline (not exceeding 100 s) No change 2 hours; after 2 consecutive No change APTT's within target range, Check at least once per day > 3.0 times baseline or > 100 s Stop infusion until the APTT is 1.5-3.0 times baseline; Resume at half of the previous infusion rate. 2 hours Body weight (kg) 50 60 70 80 90 2micrograms/kg/min Infusion rate (ml/hour) 6 7 8 10 11 0.5micrograms/kg/min Infusion rate (ml/hour) 1.5 1.8 2.1 2.4 2.7 4 hours 4 hours; after 2 consecutive APTT's within target range, Check at least once per day Stop infusion until the APTT is 4 hours 1.5-3.0 times baseline; Resume at half of the previous infusion rate. Body weight (kg) 100 110 120 130 140 2micrograms/kg/min Infusion rate (ml/hour) 12 13 14 16 17 0.5micrograms/kg/min Infusion rate (ml/hour) 3 3.3 3.6 3.9 4.2 Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 32 Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 33 DRUG METHOD WHO MAY ADMINISTER INSTRUCTION FOR DILUTION AND GIVE OVER SUITABLE DILUENT Argipressin Artesunate See vasopressin IV bolus Groups 1 1-2 minutes and 2 This drug is unlicensed – see page 7 IM Injection Groups 1 and 2 Reconstitute each 60mg vial with 1ml of the supplied sodium bicarbonate solvent from the ampoule. Shake the vial for several minutes to mix well until the powder is completely dissolved and the solution is clear. Dilute further with 5ml of N/S or G to make 60mg in 6ml (10mg/ml) solution. Shake to mix well, ensuring that the resulting solution is still clear. If the solution appears cloudy or a precipitate is present, it should be discarded. Reconstitute each 60mg vial with 1ml of the supplied sodium bicarbonate solvent from the ampoule. Shake the vial for several minutes to mix well until the powder is completely dissolved and the solution is clear. Dilute further with 2ml of N/S or G to make 60mg in 3ml (20mg/ml) solution. Shake to mix well, ensuring that the resulting solution is still clear. If the solution appears cloudy or a precipitate is present, it should be discarded. COMMENTS The reconstituted artesunate solution should always be used immediately, and discarded if not used within one hour. Do not use water for injection for reconstitution of the artesunate powder or for dilution of the resulting solution prior to injection. Dosage: 2.4mg of artesunate / kg body weight, by IV or IM injection, at 0, 12 and 24 hours, then once daily until oral treatment can be substituted. Dosage adjustment is not considered necessary in patients with hepatic or renal impairment. The anterior thigh is usually the preferred site for intramuscular injection. If the total volume of solution to be injected intramuscularly is large, it may be preferable to divide the volume and inject it at several sites, e.g. both thighs. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 34 DRUG METHOD WHO MAY GIVE Atenolol IV bolus Groups 1 and 2 (I) Infusion Infusion pump is required. Groups 1 and 2 ADMINISTER OVER Maximum rate 1mg/minute 20 minutes INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Can be diluted with N/S or G to any convenient volume e.g.10ml. Dilute with N/S or G to a suggested volume of 50ml or 100ml. ATG Atosiban See Anti-Thymocyte Globulin Rabbit (ATG rabbit) Step 1: IV bolus loading Groups 1 and 2 0.9ml (6.75mg) dose using 7.5mg/ml over 1 minute Solution For Injection immediately followed by Step 2 24ml (18mg)/hour Step 2: for 3 hours (I) IV loading infusion. followed by Step 3 Infusion pump is required. 8ml (6mg)/hour for Step 2: up to 45 hours (I) IV infusion Infusion pump is required. Atracurium IV bolus Group 1 – must only be given by doctors proficient in advanced airway management. Also see comments. (C) IV infusion. Infusion Groups 300-600 pump is required. micrograms/kg/ 1 and 2 hour COMMENTS Severe bradycardia and hypotension may occur; monitor heart rate and blood pressure. Can cause conduction defects; monitor ECG. Infusing quickly increases incidence of side effects. Flush with N/S or G. Sodium content : approximately 1.31.8mmol/5mg Total duration of treatment should not exceed 48 hours. The total dose given should preferably not exceed 330mg. Withdraw 10ml from a 100ml bag of N/S or G. Replace it with 10ml of Atosiban 7.5mg/ml Concentrate Solution for Infusion from two 5ml vials to obtain a concentration of 75mg in 100ml Can be diluted with H, G, G/S or N/S. The vials and infusions should be inspected visually for particulate matter and discolouration prior to administration. Do not mix with any other drug solutions. A 0.5mg/ml dilution is stable for 4 hours in H, 8 hours in G or G/S and 24 hours in N/S. Flush with N/S. If the patient is ventilated IV bolus can be administered by Group 2 staff. Incompatibilities include: propofol. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 35 DRUG METHOD WHO MAY GIVE Atropine IV bolus Groups 1, 2 SC injection IM Injection Augmentin Azathioprine and 8 Groups 1 and 2 Groups 1 and 2 ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT See comments If necessary atropine injection can be diluted with N/S. Refer to the Marsden Manual for guidance on SC injection. Refer to the Marsden Manual for guidance on IM injection. See Co-amoxiclav (I) IV infusion 30-60 minutes Group 1 or (preferred Group 2 who method have previous wherever experience of possible). administering Infusion pump intravenous is required. cytotoxics. Or a Group 3 nurse. IV bolus Usually 3-5 minutes. Group 1 or through tubing Group 2 who Minimum 1 minute. of a fast flowing have previous N/S or G drip. experience of administering intravenous cytotoxics. Or a Group 3 nurse. Azathioprine injection is reconstituted and diluted only by Pharmacy (Tel. 31083). Handle the prepared injection or infusion as for cytotoxic drugs (See Appendix 3). COMMENTS Give rapidly since slow IV administration may cause paradoxical slowing of the heart. ECG monitoring required. Flush with N/S. IV incompatibilities include bromides, iodides, noradrenaline, metaraminol and sodium bicarbonate. Premedication: IV immediately before induction. IM or SC 30-60 minutes before induction. Control of muscarinic side effects of neostimine: IV bolus. Flush the IV bolus with at least 50ml N/S, G or G/S since very irritant. Extravasation may cause tissue damage. Sodium content 0.2mmol/vial. Do not infuse with any other drugs. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 36 DRUG METHOD WHO MAY GIVE Aztreonam IV bolus Groups ADMINISTER OVER 3-5 minutes INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Reconstitute vial contents with 6 - 10ml W and shake well. Displacement 0.8ml/1g. Add 9.2ml to 1g vial for 100mg/ml 20-60 minutes Reconstitute each 1 gram with at least 3ml W and shake well .Then dilute each 1 gram with at least 50ml N/S, G or H. 1,2,3,4 and 5 (I) IV infusion Infusion pump is required. Groups IM injection Groups 1,2,3,4 and 5 1,2,3,4 and 5 Baclofen Basiliximab (C) Intrathecal infusion or Intrathecal bolus Group 1 or Group 2* Preferred method: Groups 20-30 minutes 1,2,3,4 and 5 (I) IV infusion. Infusion pump is required. IV bolus Groups 1,2,3,4 and 5 Reconstitute a 1gram vial with at least 3ml W or N/S and shake well. Refer to the Marsden Manual for guidance on IM injection. Prepare and administer in accordance with the Pain Management Centre procedures. Reconstitute 10mg vial with 2.5ml of the W supplied in the accompanying ampoule. Reconstitute 20mg vial with 5ml of the W supplied in the accompanying ampoule. Then dilute each 10mg to a volume of 25ml or greater with N/S or G. To avoid foaming mix by gently inverting – do not shake. Reconstitute 10mg vial with 2.5ml of the W supplied in the accompanying ampoule. Reconstitute 20mg vial with 5ml of the W supplied in the accompanying ampoule. COMMENTS Development of slight pink colour on standing does not affect potency. Flush with N/S or G. Sodium content nil. Give by deep injection into a large muscle mass such as the upper quadrant of the gluteus maximus or the lateral part of the thigh. For doses higher than 1g, or for septicaemia, meninigitis, localised parenchymal abcess, peritonitis or other severe systemic or life-threatening infections, use the IV route as above. * Restricted to those persons who are trained and competent to administer medication via the intrathecal route. Use immediately and complete administration within 4 hours of reconstitution. Do not mix or infuse with other drugs in the same lumen or IV line. Anaphylactic reactions can occur rarely Flush with N/S or G. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 37 DRUG METHOD Belatacept (I) IV infusion via infusion pump Belimumab (I) IV infusion ▼ This product is via infusion being intensively pump monitored by the CHM and MHRA. Please report all suspected reactions (including nonserious ones) using a Yellow Card from the BNF WHO MAY GIVE ADMINISTER OVER 30 minutes via Groups 1,2,3,4 and 5 a 0.2-1.2 micron in-line filter Groups 1,2,3,4 and 5 1 hour INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Reconstitute each vial with 10.5ml W or N/S using the silicone-free syringe provided with the vials. Direct the stream of fluid to the glass wall of the vial and not into the powder. To minimize foam formation, gently swirl and invert the vial for at least 30 seconds or until the powder is completely dissolved. Do not shake. Draw up the prescribed dose, using the same disposable syringe used for reconstitution of the powder, and dilute further with N/S or G so that the final concentration of Belatacept is between 2mg/ml and 10mg/ml. Gently mix the infusion. Allow 10-15 minutes for the vial to warm to room temperature. Reconstitute the 120mg vial of belimumab with 1.5ml of W. Reconstitute the 400mg vial of belimumab with 4.8ml of W. This will make a concentration of 80mg/ml belimumab for both vial sizes. During reconstitution, direct the stream of W toward the side of the vial to minimize foaming. Gently swirl the vial for 60 seconds. Allow the vial to sit at room temperature during reconstitution, gently swirling the vial for 60 seconds every 5 minutes until the powder is dissolved. Do not shake. Reconstitution is typically complete within 10 to 15 minutes after the water has been added, but it may take up to 30 minutes. Dilute the prescribed dose to 250ml with N/S (First remove a volume of N/S from the bag equal to the volume of belimumab being diluted). Gently invert the bag to mix the solution. COMMENTS Flush the line after the infusion with N/S. To allow for slight loss in the form of foam, the vial contains a small excess of powder such that you will be able to extract 250mg in 10ml (The reconstituted solution is 25mg/ml). Protect the reconstituted solution from sunlight. Belimumab is incompatible with 5% glucose solution. Patients should remain under clinical supervision for a prolonged period of time (for several hours), following at least the first 2 infusions, taking into account the possibility of a late onset hypersensitivity reaction (eg. anaphylaxis, bradycardia, hypotension, angioedema, dyspnoea). Other delayed-onset reactions can include: rash, nausea, fatigue, myalgia, headache, and facial oedema. Flush with N/S. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 38 DRUG WHO MAY ADMINISTER INSTRUCTION FOR DILUTION AND COMMENTS GIVE OVER SUITABLE DILUENT ▼ This is a penicillin – Check patient’s allergy status before administration ▼ Administration faster than the Benzylpenicillin IV bolus 3-5 minutes. Reconstitute each 600mg with 3.6-10ml W or Groups recommended rate may cause Maximum rate N/S. 1,2,3,4 and 5 (Usual for doses Displacement 0.4ml/600mg. Add 3.6ml of W or seizures and CNS toxicity. (Regular method) Incompatibilities include: gentamicin. exceeding 1.2g: N/S for 600mg in 4ml. benzylpenicillin Flush with N/S or G. 300mg/minute. 600mg and Sodium content 1.68mmol/600mg. (I) IV infusion. Groups 30-60 minutes Reconstitute each 600mg with 10ml N/S or W 1200mg vials) Infusion pump 1,2,3,4 and 5 .Can be further diluted if necessary with N/S or 1 mega unit = 600mg. Doses greater than 1.2g should be is required. G (Suggested volume 100ml). IM Injection Reconstitute each 600mg vial with 1.6ml to 2ml given by the IV route. Groups W. Refer to the Marsden Manual for guidance on 1,2,3,4 and 5 IM injection. For regular intravenous benzylpenicillin see above Do not inject this formulation Benzathine Deep IM Shake the vial to loosen the powder inside. Groups intravenously. benzylpenicillin injection Reconstitute the vial contents with the 8ml of W 1,2,3,4 and 5 provided in the unlabelled ampoule. (Extencillin®) Refer to the Marsden Manual for guidance on IM 2.4 megaunit vial injection. (Unlicensed product –see p4) DRUG METHOD METHOD WHO MAY ADMINISTER GIVE OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 39 DRUG METHOD Beriplex P/N® (I) IV Infusion Only prescribe using an after consultation infusion with a Consultant pump Haematologist Available on request from the Blood Bank WHO MAY ADMINISTER GIVE OVER Groups Each 500 IU in 20ml 1,2,3,4 and W over 10-15 minutes 5 So set the infusion pump rate at 80-120ml/hour INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Follow the nine steps illustrated below and continued on the next page for reconstituting the vials. Using the transfer device provided, reconstitute each 250 IU vial with the 10ml of W provided. Using the transfer device provided, reconstitute each 500 IU vial with the 20ml W provided. The concentration is 25 IU/ml. Do not further dilute the reconstituted solution. COMMENTS The Consultant Haematologist will advise on the dosage to be given, and the monitoring to be performed. Do not administer down the same lumen or catheter as other drugs and fluids. May be flushed with N/S. Take care that no blood enters the syringe filled with product, as there is a risk that the blood could coagulate in the syringe and fibrin clots would therefore be administered to the patient. Store Beriplex P/N® in the fridge. Use reconstituted Beriplex® within 8 hours Instructions for reconstituting Beriplex P/N® 1. Open the Mix2Vial package by 3. Carefully remove the package from the Mix2Vial set. Make peeling away the lid. sure that you only pull up the package and not the Mix2Vial set. 1 3 2. Place the diluent vial on an even, clean surface and hold the vial tight. Take the Mix2Vial together with the package and push the blue end straight down through the diluent stopper. 2 4. Place the product vial on an even and firm surface. Invert the diluent vial with the Mix2Vial set attached and push the transparent adapter straight down through the product vial stopper. The diluent will automatically flow into the product vial. 4 Instructions continued on the next page Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 40 Instructions for reconstituting Beriplex P/N® continued 5. With one hand hold the 6. Gently swirl the product vial 6 product-side of the Mix2Vial set, until the substance is fully hold the diluent-side with the other dissolved. Do not shake. hand and unscrew the set into two pieces. Discard the diluent vial with the blue part attached 5 7. Draw air into an empty, sterile syringe. While the product vial is upright, connect the syringe to the Mix2Vial's Luer Lock fitting. Inject air into the product vial. 7 8. While keeping the syringe 9 plunger pressed, invert the system upside down and draw the concentrate into the syringe by pulling the plunger back slowly. 8 9. Now that the concentrate has been transferred into the syringe, firmly hold on to the barrel of the syringe (keeping the syringe plunger facing down) and disconnect the Mix2Vial set from the syringe. 8 DRUG METHOD WHO MAY GIVE Bevacizumab (I) IV Infusion using an infusion pump. Groups ADMINISTER OVER Initial dose should be infused 1,2,3,4 and 5 over 90 minutes. If the first infusion is well tolerated, the second infusion may be administered over 60 minutes. If the 60-minute infusion is well tolerated, all subsequent infusions may be administered over 30 minutes. INSTRUCTION FOR DILUTION AND SUITABLE DILUENT A closed-system device must be used to prepare bevacizumab. Draw up the prescribed dose and dilute with N/S so that the final concentration is within the range of 1.4 mg/ml to 16.5 mg/ml. Usually the prescribed dose diluted with N/S to a total volume of 100 ml is within these limits – but check. COMMENTS Do not infuse bevacizumab through th same line or lumen as any other drugs or glucose. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 41 DRUG METHOD Bivalirudin Rapid Initial IV bolus Patients undergoing PCI, including primary PCI : 0.75 mg/kg WHO MAY ADMINISTER OVER GIVE Groups Suggestion: 1,2,3,4 and 2 seconds 5 Patients with unstable angina/non-ST segment elevated myocardial infarction: 0.1 mg/kg (C) IV infusion immediately following the IV bolus INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Add 5 ml W to one vial of 250mg bivalirudin and swirl gently until completely dissolved and the solution is clear. Withdraw 5 ml from the vial, and further dilute to 50 ml with G or N/S to give a final bivalirudin concentration of 5 mg/ml. Mix thoroughly. The reconstituted/diluted solution will be a clear to slightly opalescent, colourless to slightly yellow solution. Groups Patients undergoing PCI, 1,2,3,4 and including primary PCI : 1.75mg/kg/hour = 0.35ml/kg/hour 5 of the 5mg/ml infusion during the procedure and for up to 4 hours post PCI if necessary. Then 0.25mg/kg/hour = 0.05ml/kg/hour for 4- 12 hours if necessary. COMMENTS Incompatible with alteplase, amiodarone, amphotericin B, chlorpromazine, diazepam, prochlorperazine, reteplase, streptokinase and vancomycin. Activated Clotting Time (ACT) values 5 minutes after bivalirudin bolus average 365 +/- 100 seconds. If the 5-minute ACT is less than 225 seconds, a second bolus dose of 0.3 mg/kg should be administered. Once the ACT value is greater than 225 seconds, no further monitoring is required provided the 1.75 mg/kg infusion dose is properly administered. Patients with unstable angina/non-ST segment elevated myocardial infarction: 0.25 mg/kg/hour = 0.05ml/kg/hour of the 5mg/ml infusion for up to 72 hours. Blinatumomab (C) IV infusion via pump Groups 1 and 2 Duration of infusion may vary Infusion to be prepared by Pharmacy. Telephone ext. 31083 Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 42 DRUG METHOD WHO MAY ADMINISTER INSTRUCTION FOR DILUTION AND GIVE OVER SUITABLE DILUENT Botulinum toxin IM injection into specific Group 1 Reconstitute the 500unit vial with 1ml of (Dysport®) W to make a 500unit/ml solution. muscles to treat spasticity Reconstitute the 300unit vial with 0.6ml of W to make a 500unit/ml solution. SC injection into specific Group 1 facial sites to treat blepharospam and hemifacial spasm. Reconstitute the 500unit vial with 2.5ml of W to make a 200unit/ml solution. Reconstitute the 300unit vial with 1.5ml of W to make a 200unit/ml solution. Note that Dysport and Botox brands are NOT interchangable due to different unit potencies. Botox brand has only been approved locally for the indications stated below. Reconstitute a 200 unit vial of Botox® Botulinum toxin 31-39 x 0.1ml (5unit) Group 1 with 4ml of N/S and mix gently. injections into specific (Botox® 200 unit head and neck muscles vials) to treat chronic migraine Reconstitute a 200 unit vial of Botox® Botulinum toxin 30 x 1ml (6.7unit) Group 1 with 6ml of N/S and mix gently. (Botox® 200 unit injections into the Draw 2ml from the vial into each of three detrusor muscle to treat vials) 10ml syringes. Then complete the neurogenic detrusor reconstitution by adding 8ml N/S into overactivity each of the 10ml syringes, and mix gently. This will result in three 10ml syringes, each containing about 67 units of reconstituted Botox® Botulinum toxin 20 x 0.5ml (5unit) Reconstitute a 100 unit vial of Botox® Group 1 with 10ml of N/S and mix gently injections into the (Botox® 100 unit detrusor muscle to treat vials) overactive bladder COMMENTS Sharing a vials of botulinum between patients in a day-case/clinic setting (i.e. not in-patient on ward or in theatre) has been risk assessed and sanctioned by the PHNT Medicines Governance Committee so long as the following practice is strictly adhered to: Between patients the reconstituted vial is kept in the fridge. A separate drawing-up needle is used for each patient. Any reconstituted botulinum remaining in the vial(s) at the end of the session must be discarded. The maximum time Dysport® may be stored at 2-80C following reconstitution is 8 hours. The maximum time Botox® may be stored at 2-80C following reconstitution is 24 hours. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 43 DRUG METHOD WHO MAY GIVE Bumetanide IV bolus Groups 1 and 2 (I) IV infusion. Infusion Groups 1 pump is required. and 2 Bupivacaine (epidural) Adults: 0.167% (with or without Fentanyl) Paediatric: 0.125% Bupivacaine Infusion for local infiltration 0.167% 0.125% 0.0625% ADMINISTER OVER Suggestion: 1 minute INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Give undiluted. COMMENTS Flush with N/S. Leave a gap of 20 minutes between repeat bolus doses. Protect infusion from light and discard if cloudiness develops. Sodium content 0.007mmol/1ml. Dilute 2 – 5mg with 500ml of G, N/S or G/S. Alternatively dilute to 1mg/10ml with G, N/S or G/S (unlicensed dilution- see page 7) IM Injection Refer to the Marsden Manual for Groups 1 guidance on IM injection. and 2 All epidural administration sets and epidural catheters must be labelled “Epidural” when in use (NPSA/2007/21) Epidural infusion via a Groups Adult patients: Pre-made bags are supplied from *Staff administering and monitoring McKinley epidural Epidurals: Pharmacy. epidural infusions must have received 1and 2* pump, using a yellow Protocol “A” PCEA training from the Acute Care Team coloured line which or “B” CEA. Modified and demonstrated their competency at must be labelled epidural protocols administering and monitoring epidural “Epidural” are very rarely infusions. Follow the PHNT Epidural prescribed by Protocols. Anaesthetists Additional clinician boluses may be administered by Pain Nurses if required as per epidural protocol. For specialist use: Refer to Acute Care Pre-made bags are supplied from Refer to the PHNT protocol for Groups local infiltration at Team Guidelines Pharmacy. Continuous Local Anaesthetic 1and 2 other sites i.e. near Infusions. nerves, wound, joint, body cavity (e.g. interpleural, paravertebral) Via a dedicated, grey McKinley 595 pump, using a grey coloured line which must be labelled with the route 30-60 minutes Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 44 DRUG METHOD WHO MAY GIVE Buprenorphine IV bolus Groups 1 ADMINISTER OVER 3-5 minutes INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Can be diluted with N/S or G. and 2 IM Injection Groups 1 Caffeine and sodium benzoate For treating low CSF pressure headache (I) IV infusion Calcitonin SC injection Groups IM injection 1,2,3,4 and 5 Groups 1,2,3,4 and 5 For hypercalcaemia of malignancy IV injection* Groups 1,2,3,4 and 5 (I) IV infusion for Groups severe or emergency 1,2,3,4 and 5 cases of hypercalcaemia of malignancy only. 1-2 hours and 2 Refer to the Marsden Manual for guidance on IM injection. Dilute 500mg caffeine sodium benzoate in 1 litre of N/S. Refer to the Marsden Manual for guidance on SC injection. Refer to the Marsden Manual for guidance on IM injection. Suggestion: 12 minutes At least 6 hours Dilute 10units/kg in 500ml N/S. COMMENTS Flush with N/S. Sodium content nil. Record a resting ECG before administration. Monitor for possible side effects: tachycardia, cardiac arrythythmias, extrasystoles, restlessness, agitation, nausea, diuresis, hypoglycaemia, and hyperglycaemia. Note that caffeine and sodium benzoate injection is unlicensed – see page 7. Allow the ampoule or vial to reach room temperature before SC or IM injection. When in use the 400unit in 2ml multidose vial can be stored at room temperature. Record date of first use. Discard the remaining contents of the 400unit in 2ml multidose vial 1 month after first use. Ampoules of calcitonin are for single use only. May be given by IV injection for hypercalcaemia of malignancy after previous rehydration.* Do not use the calcitonin from the multiple dose 400unit in 2ml vial for bolus injection (As it contains phenol). Some adsorption of calcitonin to the plastic of the infusion set will occur so monitor the patient’s response to treatment. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 45 DRUG METHOD Calcium chloride Rapid IV bolus during CPR for Cardiac Arrest WHO MAY ADMINISTER OVER GIVE Groups 1-2 seconds 1 and 2 IV bolus Groups Emergency use 1 and 2 or for severe acute hypocalcaemia (I) or (C) IV infusion. Infusion pump is required. Groups 1 and 2 Calcium IV bolus Groups gluconate Emergency use or 1 and 2 for severe acute hypocalcaemia (I) or (C) infusion Groups using plastic 1 and 2 ampoules of calcium gluconate Maximum adult rates: 1ml of 14.7%/minute 1-1.5ml of 10%/minute 1ml of 13.4%/minute INSTRUCTION FOR DILUTION AND SUITABLE DILUENT If 10% Calcium Chloride Minijets are not available then in cardiac arrest give 6.8ml of 14.7% calcium chloride undiluted which is 6.8mmol Ca2+ (equivalent to a 10% Calcium Chloride Minijet) COMMENTS In the presence of spontaneous circulation, calcium must be given slowly. Very irritant; always administer slowly. Extravasation may cause tissue irritation and necrosis. Flush with N/S. Calcium chloride 10% contains Adults: Maximum rate May be diluted with N/S, G or G/S to any suitable 6.8mmol calcium/10ml. 1mmol/minute. volume. However, concentrations greater than 10ml of Calcium chloride 13.4% 14.7% calcium chloride in each 100ml diluent will be contains 9.12mmol irritant to peripheral veins and should ideally be given calcium/10ml. via a central IV line. Calcium chloride 14.7% contains 10mmol calcium/10ml. If 10% Calcium Chloride Minijets are not available Adults: Each 10ml Flush with N/S. ampoule preferably then in cardiac arrest give 30ml of 10% calcium Calcium gluconate 10% over 5 minutes, gluconate undiluted which is 6.6mmol Ca2+ contains 2.2mmol calcium in minimum 3 minutes. (approximately equivalent to a 10% Calcium Chloride 10ml. Minijet) Irritant; extravasation may cause tissue irritation and Adults: Maximum rate May be diluted with N/S, G or G/S to any suitable by infusion 200mg volume e.g. 100ml, 250ml, 500ml or 1 litre. However, necrosis. (0.44mmol concentrations greater than 10ml of 10% calcium Calcium)/minute gluconate in each 100ml diluent will be irritant to peripheral veins and should ideally be given via a central IV line. In severe acute hypocalcaemia or hypocalcaemic tetany, an initial slow intravenous injection of 10–20 ml of calcium gluconate injection 10% (use the plastic ampoules) should be given, with plasma-calcium and ECG monitoring (risk of arrhythmias if given too rapidly), and either repeated as required or, if only temporary improvement, followed by a continuous intravenous infusion to prevent recurrence. For infusion, dilute 100 ml of calcium gluconate 10%(Use the plastic ampoules) in 1 litre of glucose 5% or sodium chloride 0.9% (remove 100ml from the bag first) and give at an initial rate of 50 ml/hour adjusted according to response. Calcium gluconate injection in glass ampoules or vials is now contra-indicated for use as repeated or prolonged treatment, including as an IV infusion, in children younger than 18 years and in patients with renal impairment. This is to limit exposure of patients to aluminium which is leached from the glass by the calcium gluconate solution. (MHRA Drug Safety Update, August 2010). Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 46 DRUG METHOD ‘Campath’ See Alemtuzumab Caspofungin (I) IV infusion. Infusion pump is required. Cefotaxime Only to be prescribed when ceftriaxone is contra-indicated due to the risk of precipitation with calcium containing fluids and TPN. Cefoxitine (Unlicensed product – see page 7) WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Groups 1 hour Allow the vial to warm to room temperature. Reconstitute each 50mg and 70mg vial with 10.5ml W. For the 50mg dose withdraw 10ml from the reconstituted 50mg vial. For the 70mg dose withdraw 10ml from the reconstituted 70mg vial. For reduced dose in moderate hepatic impairment (35mg) withdraw 7ml from the reconstituted 50mg vial. Further dilute with 250ml N/S or H. If the patient is fluid restricted the 50mg and 35mg doses may be diluted in 100ml N/S or H. Flush with N/S. Do not infuse caspofungin with any other drug solutions or infusions containing glucose. Phebitis is commonly reported. Flush with N/S, G or G/S. Sodium content 2.09mmol/1g. 1,2,3,4 and 5 IV bolus preferred Groups 3-5 minutes method. 1,2,3,4 and 5 (I) IV infusion via infusion pump IM Injection Groups IM Injection Groups 20-60 minutes 1,2,3,4 and 5 Groups 1,2,3,4 and 5 IV bolus preferred Groups 3-5 minutes method 1,2,3,4 and 5 1,2,3,4 and 5 (C) IV infusion via Groups infusion pump 1,2,3,4 and 5 Reconstitute 500mg with 2ml, 1g with 4ml and 2g with 10ml W. Displacement 0.2ml for 500mg vial. Add 1.8ml of W for 500mg in 2ml. Displacement 0.5ml for 1g vial. Add 3.5ml W for 1g in 4ml. Displacement 1.2ml for 2g vial. Add 8.8ml W for 2g in 10ml. Reconstitute as above then dilute 1-2g with 40100ml N/S, G, G/S or H. Reconstitute as for IV bolus. For paediatric doses apply the same displacement values. Reconstitute the 2g vial with 10ml or 20ml W, N/S, G or G10%. Displacement is 1ml for the 2g vial. Shake to dissolve and let stand until clear. Reconstitute the 2g vial with 4ml W. Displacement is 1ml for the 2g vial. Shake to dissolve and let stand until clear. Reconstitute each 2g vial with 10ml W. Shake to dissolve and let stand until clear. Further dilute with a suitable volume (eg. 500ml or 250ml) of N/S, G, G10% or H. Refer to the Marsden Manual for guidance on IM injection. Incompatible with aminoglycosides eg.gentamicin, tobramycin and amikacin. Inject into a large muscle mass, eg. gluteus maximus. Diluted solutions for IV infusion must be discarded 12 hours after preparation. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 47 DRUG METHOD Cefradine Ceftazidime Ceftriaxone WHO MAY ADMINISTER OVER INSTRUCTION FOR DILUTION AND GIVE SUITABLE DILUENT Cefradine injection is no longer commercially available. IV bolus 3-5 minutes Reconstitute 500mg vial with 5ml, 1g Groups vials with 10ml and 2g vial with 10ml 1,2,3,4 and 5 A 3g dose (1x1g N/S or G. Carbon dioxide is released; +1x2g vials) may be see package insert. given by slow IV bolus. (I) IV infusion. Maximum 30 minutes Reconstitute 2g vial with 50ml of N/S Groups Infusion pump 1,2,3,4 and 5 or G. is required. For 3g dose, also reconstitute a 1g vial with10ml N/S. Dilute the reconstituted 1g and 2g vials further to 75ml with N/S. IM Injection Reconstitute 250mg with 1ml, 500mg Groups with 1.5ml and 1g with 3ml N/S or W. 1,2,3,4 and 5 carbon dioxide is released, see package insert. IV bolus 2-4 minutes Reconstitute 250mg vial with 5ml W Groups and 1g vial with 10ml. Displacement 1,2,3,4 and 5 values vary between brands and are not consistent – refer to the package insert or SPC for the particular brand and vial size being used. (I) IV infusion At least 30 minutes Reconstitute 2g vial with 40ml G, G Groups (doses of 2g 10%, or N/S. 1,2,3,4 and 5 and above) via infusion pump IM Injection Reconstitute 250mg with 1ml, 1g with Groups 3.5ml and 2g with 7ml of 1% 1,2,3,4 and 5 lidocaine injection. Refer to the Marsden Manual for guidance on IM injection. COMMENTS Flush with N/S, G or G/S. Sodium content 2.3mmol/1g. Displacement values vary between brands, and are not consistent. Refer to the SPC or package insert for the brand and vial size being used. Doses exceeding 1g should be given IV – see above. When IM injection causes pain Lidocaine 1% injection may be used to reconstitute the vial instead of N/S or W. Do not give with TPN or fluids containing calcium, even by different infusion lines (Cefotaxime is a suitable alternative for these patients). Sodium content: 3.6mmol/1g Flush with N/S or G For infants and children up to 12 years, doses of 50mg/kg or over should be given by slow IV infusion over at least 30 minutes. (For neonates the dose is given over 60 minutes). Give by deep IM injection. Doses greater than 1g should be divided and injected at more than one site. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 48 DRUG METHOD Cefuroxime Cernevit (Water and fat-soluble vitamins) WHO MAY ADMINISTER OVER GIVE Groups 3-5 minutes 1,2,3,4 and 5 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT IV bolus Reconstitute 250mg with at least 2ml, 750mg (Usual with at least 6ml and 1.5g with at least 15ml W. method) Shake gently to produce an opaque suspension. (I) IV infusion Groups Maximum 30 minutes Reconstitute as above then dilute to via pump. 50 - 100ml with N/S or G. 1,2,3,4 and 5 IM Injection Groups Reconstitute 250mg with 1ml W and 750mg with 3ml W. Shake gently to produce an opaque 1,2,3,4 and suspension. Refer to the Marsden Manual for 5 guidance on IM injection. Slow IV Reconstitute the vial with 5ml of W, N/S or G. Groups At least 10 minutes bolus Mix gently to dissolve the powder forming a 1,2,3,4 and yellow-orange coloured solution. 5 Either give undiluted or dilute further with a small volume of N/S or G. (I) IV infusion Groups At least 10 minutes Infusion 1,2,3,4 and pump is 5 required. COMMENTS Flush with N/S, G or G/S. Sodium content: 1.8mmol/750mg Cefuroxime can be added to an infusion bag of metronidazole. Displacement values vary between brands and are not consistent – refer to the package insert or SPC for the particular brand and vial size being used. Dosage for adults and children aged over 11 years: 1 vial of 5ml per day. Cernevit does not contain Vitamin K. Cernevit may be administered via any type of intravenous cannula (including peripheral). Do not mix with any other drug solutions. Reconstitute the vial with 5ml of W, N/S or G. Mix gently to dissolve the powder forming a yellow-orange coloured solution, then dilute further with N/S or G (e.g. up to 50ml). Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 49 DRUG METHOD WHO MAY ADMINISTER GIVE OVER Cetuximab (I) IV infusion Groups Infusion 1,2,3,4 and pump is required. Infuse doses of 400mg/m2 or 500mg/ m2 over 2 hours. Infuse doses of 250mg/m2 over 1 hour. Chloramphenicol IV bolus sodium succinate (Usual method) (I) IV infusion. Infusion pump is required. INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT A closed-system device must Prior to the first infusion, patients must receive be used to prepare premedication with an antihistamine and a corticosteroid cetuximab. at least 1 hour prior to administration of cetuximab. This premedication is recommended prior to all subsequent Give undiluted in an EVA bag infusions. (EVA bag supplied by Close monitoring is required during the infusion and for Pharmacy). at least 1 hour after the end of the infusion. Availability of resuscitation equipment must be ensured. Severe infusion-related reactions, including anaphylactic reactions, may commonly occur, despite premedication. Fever, chills, dizziness, dyspnoea, bronchospasm, urticaria or skin reactions are also very common, particularly with the first infusion. Do not infuse cetuximab through th same line or lumen as any other drugs or glucose. Reconstitute with W, N/S or G. Groups See package insert. Suggested 1,2,3,4 and maximum concentration 5 100mg/1ml. Displacement 0.8ml/1g vial. Add 9.2ml diluent to 1g vial for 1g in 10ml (100mg in 1ml). Groups Give slowly over 15 Reconstitute as above then dilute with N/S or G (suggested 1,2,3,4 and to 30 minutes volume 100ml). 5 At least 1 minute Flush with N/S. Flush with N/S. Sodium content 2.98/1g In order to ensure rapid attainment of high blood levels, chloramphenicol succinate is best administered by IV injection. Where this is not possible, however, IM injection may be used, although it should be borne in mind that absorption may be slow and unpredictable. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 50 DRUG METHOD WHO MAY GIVE Chloroquine (C) IV infusion. Groups 2 Infusion pump is and 2 required. Chlorphenamine IV bolus Groups 1,2,3,4, 5 & 8 ADMINISTER OVER Initially 10mg/kg of Dilute with N/S to a suitable volume Chloroquine base e.g. 50ml. over 8 hours then 5mg of base/kg for 3 more 8-hour infusions Minimum 1 minute May be diluted with N/S to a convenient volume e.g. 10ml. IM injection Groups (Use the IV route 1,2,3,4 and 5 if a rapid effect is required) Chlorpromazine SC injection (Use the IV route if a rapid effect is required) Deep IM injection (I) IV infusion via an infusion pump to treat hiccups when IM injection fails. IV bolus (This method is unlicensed – see page 7). Refer to the Marsden Manual for guidance on IM injection. Groups Refer to the Marsden Manual for guidance on SC injection. 1,2,3,4 and 5 Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Slowly (Suggestion: 12 hours) Adults: Maximum 1mg/minute. Refer to the Marsden Manual for guidance on IM injection. Dilute 25-50mg with 500ml-1 litre N/S. COMMENTS Oral therapy is started as soon as possible to complete the course. Flush with N/S. Flush with N/S (IV) Extra care should be taken when preparing the injection for children under 1 year due to the small volumes that are required. Dilution of chlorphenamine injection with N/S should facilitate preparation. For example, diluting 0.2ml chlorphenamine injection to 2ml with N/S produces a solution containing chlorphenamine 1mg/ml. The diluted product should be used immediately. IM injection can be repeated at 6 to 8 hour intervals if required. Substitute with oral chlorpromazine as soon as possible. Very irritant; avoid IV administration if possible. Do not administer via the SC route. Dilute to a maximum concentration of Flush with N/S (IV). Sodium content 0.2mmol/2ml. 1mg/1ml with N/S. Hypotension can occur, especially with rapid administration: Keep the patient supine and monitor the blood pressure during and for 30 minutes after IM or IV administration. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 51 DRUG METHOD Ciclosporin (I) IV infusion. Infusion Groups 2-6 hours pump is required. 1,2,3,4 and 5 Dilute to a concentration of 0.5 2.5mg/ml of N/S or G. Do not use a standard PVC infusion bag. Either prepare the infusion in a 50ml syringe, or in a PVC-free polyolefil bag of N/S (available from pharmacy in 50ml, 250ml and 500ml sizes). Cidofovir (I) IV infusion. Infusion Groups 1 hour pump is required. 1,2,3,4 and 5 Infusion to be prepared by Pharmacy. Telephone Ext. 31083. Doctor to prescribe dose (see comments) in 100ml N/S. Ciprofloxacin Not for general use. Refer to Trust Policy for Control of Infection. WHO MAY ADMINISTER OVER GIVE INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Use a PE/PVC (Polyethylene-lined) extension set when prepared in a 50ml syringe. Observe patient continuously for the first 30 minutes and at frequent intervals thereafter (Risk of anaphylactic reactions, acute respiratory distress, blood pressure changes). Flush with N/S. Do not infuse down the same line as any other drug solutions. To facilitate accurate measurement of the dose, the prescribed dose in milligrams (rounded up or down if necessary) divided by 75 should have no more than one decimal figure. Wear gloves, gown and safety glasses when handling. Avoid handling drug if pregnant or trying to become pregnant. Do not infuse with any other drugs. Flush with N/S. Give 2g probenecid PO 3 hours pre-cidofovir infusion, 1g PO 2 hours after cidofovir infusion and 1g PO 8 hours after cidofovir infusion. Probenecid can cause nausea so if possible the patient should eat some food before each dose. Alternatively, administer antiemetics as required. Infuse 1 Litre N/S IV over 1 hour immediately before the cidofovir infusion. An additional 1 Litre of N/S may be infused IV over 2 hours after this (I) IV infusion. Infusion Groups pump is required. 1,2,3,4 and Infusion into a large 5 vein will reduce venous irritation (low pH) Adults: 200mg over 30 Provided suitably diluted. minutes, 400mg over 60 minutes. For children, infuse the dose over 60 minutes. Flush with N/S. Sodium content 15.4mmol/100ml. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 52 DRUG METHOD Cisatracurium IV bolus Clarithromycin (C) IV infusion. Infusion pump is required. (I) IV infusion via a large peripheral vein (or central vein). Infusion pump is required. WHO MAY GIVE ADMINISTER OVER Group 1 – must only be given by doctors proficient in advanced airway management. Also see comments. Groups 1 and 2 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Can be given undiluted, or diluted further with N/S or G. Groups 1,2,3,4 60 minutes Reconstitute 500mg vial with 10ml W and shake to dissolve the contents. Further dilute to a concentration of 2mg/ml with N/S, G or H (Adult dose of 500mg = 10ml of reconstituted solution in 250ml N/S, G or H). and 5 (The lowest recommended concentration is 0.1mg/ml) COMMENTS Flush with N/S. If the patient is ventilated IV bolus can be administered by Group 2 staff. Cisatracurium is incompatible with propofol and Hartmann’s. Do not give by IV bolus (can cause cardiac arrythmias). Do not give by IM injection. The reconstituted vial contains 500mg in 10ml (although the final volume in the vial will be 10.4ml). Use infusion within 6 hours of preparation. Flush with N/S or G. Sodium content: Less than 0.5mmol/500mg For fluid restricted patients 500mg Incompatible with aminophylline, clarithromycin, reconstituted as above, cefuroxime, furosemide, heparin, may be diluted in 100ml of N/S and phenytoin, flucloxacillin and ceftazidime. infused over 60 minutes via a central IV Monitor infusion site for signs of line (This dilution is unlicensed – see page inflammation, tenderness, phlebitis and 7). pain. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 53 DRUG METHOD Clindamycin I) IV infusion Maximum 1.2g. Infusion pump is required (C) IV infusion via pump for doses above 1.2g IM injection WHO MAY ADMINISTER OVER GIVE INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS groups Dilute to a maximum concentration of 18mg/ml with N/S or G. Typically: For doses of 300mg, 600mg or 900mg, dilute in 50ml or 100ml N/S or G. Dilute 1200mg in 100ml N/S or G. Dilute to a maximum concentration of 18mg/ml with N/S or G. Flush with N/S. Sodium content: Nil. 300mg over at least 10 1,2,3,4 and minutes, 600mg over at least 20 minutes, 5 900mg over at least 30 minutes, 1.2g over at least 40 minutes. groups Rate not to exceed 1,2,3,4 and 30mg/minute. 5 groups 1,2,3,4 & 5 Clonazepam IV bolus Groups In to a large vein 1,2,3,4 and in the antecubital 5 fossa. Emergency use (I) IV infusion. Infusion pump is required. Adults: Maximum rate 0.25 - 0.5mg/minute Infants & children: 50microgram/kg (maximum 1mg) over at least 2 minutes Groups Adjust rate according 1,2,3,4 and to response. 5 Neonates and children 1 month to 18 years: 10 – 60 micrograms/Kg/hour = 0.83 – 5ml/kg/hour of the 12microgram/ml dilution. Refer to the Marsden Manual for guidance on IM injection. Continuous intravenous infusion may begin with a single rapid infusion of the first dose (generally over 30minutes), followed by a continuous infusion of 0.75 to 1.25mg/minute. Single IM injections of greater than 600mg are not recommended. Immediately before use dilute each 1mg in 1ml with 1ml W (diluent supplied), to produce a 1mg in 2ml solution. Resuscitation equipment must be readily available. EEG, respiratory function and blood pressure should be monitored. Flush with N/S, G or G10%. Sodium content: Nil Dilute up to 3mg in 250ml of N/S, If using a PVC bag and/or a PVC line begin the infusion immediately and infuse over a period no G, G10% or G/S(2.5%/0.45%). longer than 2 hours. On Neonatal ICU dilute to a Alternatively dilute to 12 micrograms/ml with N/S maximum concentration of in a 50ml Terumo or BD syringe using a PVC300micrograms in 25ml or free extension set. The following are available to 600micrograms in 50ml (12 micrograms/ml) with G10%. In fluid be ordered from NHS Supplies: restricted infants concentrations up Codan PVC-free extension set 71.4001, order code FKA064 to 100micrograms/ml have been Alaris G30302M line, order code FKA058 used. Using this method the solution will be stable for 12 hours. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 54 DRUG METHOD WHO MAY ADMINISTER OVER GIVE INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Clonidine IV bolus Groups Can be diluted with N/S or G to any suitable volume. Flush with N/S. Sodium content 0.15mmol/1ml. (C) IV infusion is unlicensed (See page 7). Monitor for bradycardia and hypotension. Withdraw gradually to avoid rebound tachycardia, hypertension, agitation and sweating. Very little compatibility data – infuse through a dedicated lumen or line. May be infused via a peripheral or central IV line. 1 and 2 (C) IV infusion Groups for sedation/ 1 and 2 withdrawal from sedation in critical care areas only. Infusion pump is required. (C) Intrathecal Group 1 infusion or or Group 2* Intrathecal bolus Give slowly preferably over 10-15 minutes to avoid transient pressor effect. Usual rate: 0.5 - 1 Dilute 750 micrograms to 50ml micrograms/kg/hour. with N/S or G. Rates up to 2 microgram/kg/hour have been used. Prepare and administer in accordance with the Pain Management Centre procedures * Restricted to those persons who are trained and competent to administer medication via the intrathecal route. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 55 DRUG METHOD Co-amoxiclav Colistimethate (Colistin) (Colomycin ®) WHO MAY GIVE INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Co-amoxiclav contains a penicillin – Check patient’s allergy status before administration IV bolus 3-4 minutes Reconstitute 1.2g vial with 20ml Flush with N/S. Groups W and 600mg vial with 10ml W. Complete infusion within 4 hours of 1,2,3,4 and 5 Usual method. For doses requiring part of a vial reconstitution. Displacement values: Sodium content 2.7mmol/1.2g. Potassium content 1mmol/1.2g. Bowmed/Actavis brand: For bolus injection use within 20 minutes of 0.4ml for the 600mg vial and reconstitution. 0.7ml for the 1.2g vial. Do not dilute Co-amoxiclav with G. Augmentin® and Wockhardt Not suitable for IM injection. brands: Example: How to give 900mg 0.5ml for the 600mg vial and 0.9ml for the 1.2g vial. Using a 20ml syringe, reconstitute a 1.2g vial (I) IV infusion. 30-40 minutes Reconstitute as above then dilute with 15ml WFI. Draw up the entire vial Groups contents into the syringe then draw up more Infusion pump is 1.2g with 100ml N/S or 600mg 1,2,3,4 and 5 W to the 20ml mark. Mix the syringe contents. required. with 50ml N/S. Then administer 15ml (contains 900mg) and discard 5ml. (I) IV infusion. Infusion pump is required. Groups 1,2,3,4 and 5 Patients with a Groups Totally Implantable 1,2,3,4 and 5 Venous Access Device (TIVAD) may tolerate a slow IV bolus of up to 2 million units ADMINISTER OVER 30 minutes Reconstitute all vial strengths with 10ml W or N/S. Roll vial in hand to dissolve. Do not shake to avoid foam formation, then dilute further with N/S to 50ml. Via TIVAD only: Reconstitute all vial strengths Minimum 5 with 10ml W or N/S. Roll vial in minutes hand to dissolve. Do not shake to avoid foam formation. Flush with N/S. Do not infuse with any other drugs. Sodium content: less than 0.5mmol per 500,000 unit and 1,000,000 unit vials The powder for injection is also licensed for use via a nebuliser. To nebulise dissolve dose in 2-4ml of W or N/S. The output from the nebuliser may be vented to the open air or a filter may be fitted. Nebulisation should take place in a well ventilated room. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 56 DRUG METHOD WHO MAY GIVE Collagenase Clostridium histolyticum ▼ This product is being intensively monitored by the CHM and MHRA. Please report all suspected reactions (including non-serious ones) using a Yellow Card from the BNF 0.58mg per Group 1 injection into a palpable Dupuytren's cord ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Remove the vial from the fridge and allow to stand at room temperature for at least 15 minutes and no longer than 60 minutes. Reconstitute the vial with the solvent supplied according to the table below. Use only the supplied solvent as it contains calcium required to activate the medication. Inject the appropriate volume (see below) of the solvent slowly into the sides of the vial. Do not invert or shake the solution. Slowly swirl to ensure dissolution. The final solution must be clear and colourless. Each vial is for single use only. When injecting a cord affecting a proximal interphalangeal joint of the fifth finger, the needle insertion must not be more than 2 to 3 mm in depth and not more than 4 mm distal to the palmar digital crease. Volumes needed for reconstitution and administration of Collagenase Clostridium histolyticum Joint to be treated Solvent required for reconstitution Sodium injected per joint: Metacarpophalangeal joints: 0.9mg Proximal interphalangeal joints: 0.7mg Injection volume to deliver 0.58 mg dose* Metacarpophalangeal joints 0.39ml 0.25ml Proximal interphalangeal joints 0.31ml 0.20ml * Note that injection volume for delivery of a 0.58 mg dose is less than the total volume of solvent used for reconstitution. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 57 DRUG METHOD WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Co-trimoxazole (I) IV infusion. Infusion pump is required. Groups The dilution for PJP (Formerly known as PCP) – each 5ml with 75ml G – should be given over no longer than 1 hour. For patients with Pneumocystis jirovecii (formerly known as Pneumocystis carinii) pneumonitis 1,2,3,4 and 5 COMMENTS Do not infuse with any other drugs. Flush with N/S. Monitor all infusions carefully for turbidity and crystallization. Dilute each 5ml with at least 75ml Commence the infusion within half an hour of preparation. G. For fluid-restricted patients: Other dilutions should High doses have been given undiluted via a Other infections dilute each be given over no central line and syringe pump over 1.5 - 2 480mg (5ml) with 125ml, longer than 90 hours (Unlicensed). 960mg (10ml) with 250ml, minutes, but this 1440mg (15ml) with 500ml or an Sodium content 1.64mmol/480mg. should be balanced equivalent dilution with N/S, G or Extravasation: may cause tissue damage. against the patient’s G/S. fluid requirements These infusions must be administered within 6 hours Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 58 DRUG METHOD WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND COMMENTS SUITABLE DILUENT Cyclizine IV bolus Groups 3-5 minutes Flush with 5 ml of N/S or G. Can be diluted with N/S or G if necessary to a convenient volume e.g. Sodium content nil. 5ml. If diluted with N/S, visually check the dilution. Discard if there is any crystallization, precipitation or haziness. Otherwise use immediately. 1,2,3,4 and 5 IM Injection Groups Refer to the Marsden Manual for guidance on IM injection. 1,2,3,4 & 5 (C) SC Groups infusion via 1,2,3,4 and syringe driver 5 in palliative care Follow the PHNT Care of The Dying Pathways and the PHNT Syringe Driver Policy. Cyclizine may precipitate if the concentration in W exceeds 10mg/ml. Precipitation occurs if mixed with N/S. For combinations of 2 or 3 drugs in the same Refer to the Marsden Manual for (C) SC Groups syringe, refer to the Syringe Driver Drug guidance on SC injection. injection for 1,2,3,4 and Compatibility chart provided in the pump kit. use in 5 Contact Pharmacy on ext. 39976 for further palliative care compatibility advice if necessary. Cyclizine is not licensed via the SC route (See page 124). Cyclophosphamide When cyclophosphamide is prescribed to treat conditions including multiple sclerosis, glomerular kidney disease or rheumatoid arthritis, it may be administered by Group 2 practitioners who have previous experience of administering parenteral cytotoxics. On the Planned Investigation Unit, refer to the Unit protocol. 3-5 minutes Pharmacy will supply pre-filled Wear gloves, gown and safety glasses when Slow IV Groups syringes of 150mg, 200mg, 400mg or handling. Avoid handling drug if pregnant or bolus 1,2,3, 4 and 500mg to make up the prescribed trying to become pregnant. 5 dose. Flush with N/S. Typically, doses of 1500mg or less are given 30-60 minutes Infusion to be prepared by Pharmacy. (I) IV Groups by slow IV bolus. Telephone Ext. 31083. Typically the infusion. 1,2,3,4 and dose is diluted in 250ml or 500ml N/S. Infuse via 5 pump Continuous over 24 hours Dilute with W. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 59 METHOD Danaparoid IV loading dose See comments Groups injected over 30 1,2,3,4 and 5 seconds followed by (C) IV infusion to treat thrombo-embolism in patients with Heparin- Induced Thrombocytopenia (HIT). Infusion pump is required. SC Injection WHO MAY GIVE ADMINISTER OVER DRUG Groups IV bolus Group 1 COMMENTS Dilute with N/S, G or G/S. The volume of diluent is not critical and can be adjusted to the fluid needs of the patient. One suggested dilution: Draw up the contents of six 750 unit ampoules (6x750 units = 4500 units) into a 50ml syringe and dilute to 45ml with N/S or G to make a 100unit/ml dilution. However, if the maintenance infusion rate is less than 187 units/hour the above dilution will waste danaparoid (expensive). In this case draw up the contents of three 750 unit ampoules (3x750units = 2250 units) into a 50ml syringe and dilute to 45ml with N/S or G to make a 50unit/ml dilution. Seek advice of Consultant Haematologist as the Consultant Haematologists have different regimens for different indications. Although the Orgaran® packing states “For subcutaneous administration”, this product is also licensed for intravenous infusion. Refer to the Marsden Manual for guidance on SC injection. 1,2,3,4 and 5 Dantrolene INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Give rapidly Reconstitute 20mg with 60ml W. Shake the vial until the solution is clear. Due to high pH (9.5) avoid extravasation. Sodium content 2mmol/20mg vial. Each 20mg vial also contains 3g mannitol. Protect from light. Incompatible: do not give with any other drugs or infusion fluids including G and N/S. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 60 DRUG METHOD WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Daptomycin May only be initiated on the advice of a consultant microbiologist IV bolus Groups 2 minutes Reconstitute the 500mg vial with 10ml N/S or the 350mg vial with 7ml N/S Do not use W to reconstitute. Gently rotate the vial to ensure complete wetting of the product and then allow to stand for 10 minutes. The vial should then be gently rotated/swirled for a few minutes as needed to obtain a clear reconstituted solution. Vigorous shaking/agitation should be avoided to prevent foaming of the product. The concentration of the reconstituted solution is 50mg/ml (No displacement) Contains negligible sodium (<0.05mmol/vial). Treatment should be discontinued if the CPK level reaches greater than 5 times upper limit of normal in the presence of unexplained muscle symptoms. Store vial in a refrigerator at 2-8oC. If clotting profiles are required during treatment, samples should be taken pre-dose. Compatible with: Aztreonam, ceftazidime, ceftriaxone, dopamine, fluconazole, gentamicin, heparin, levofloxacin, lidocaine. Incompatible with Glucose solutions. Flush with N/S. 30 minutes Reconstitute and dissolve as above. Further dilute to 50ml or 100ml N/S. Suggestion: 1 hour Via a peripheral IV cannula, 40ml Decan must be diluted to at least 250ml with N/S, or to at least 500ml with G. Via a CVC or PICC line, 40ml Decan may be diluted in a smaller volume of N/S or G or given undiluted if necessary. Decan (Trace elements) 1,2,3,4 and 5 (I) IV infusion Groups 1,2,3,4 and 5 (I) IV infusion Groups Infusion 1,2,3,4 and 5 pump is required. Dosage for adults: 1 vial of 40ml per day. Contra-indicated in children, patients weighing less than 40kg and in patients with pronounced cholestasis (serum bilirubin > 140micromol/l). Do not mix with any other drug solutions. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 61 DRUG METHOD WHO MAY ADMINISTER OVER INSTRUCTION FOR DILUTION AND GIVE SUITABLE DILUENT Defibrotide (I) IV Groups ▼ This product is being infusion via 1,2,3,4 a pump and 5 intensively monitored by the CHM and MHRA. Please report all suspected reactions (including non-serious ones) using a Yellow Card from the BNF Desferrioxamine (I) or (C) IV Groups infusion. 1,2,3,4 Infusion and 5 pump is required. SC infusion Groups using a 1,2,3,4 portable and 5 ambulatory pump 2 hours Treatment of acute iron poisoning: 15mg/kg/hour, reduced as soon as the situation permits (usually after 4-6 hours). Total IV dose not to exceed 80mg/kg in any 24 hour period Chronic iron overload: 20 – 60mg/kg/day Chronic iron overload: 20 – 60mg/kg/day. Infuse the dose over 8 to 24 hours Dilute the dose (6.25mg/kg) with N/S or G to a final concentration in the range of 4mg/ml to 20mg/ml. The total final volume of infusion should be suitable for the patient’s weight. Remove a volume of the N/S or G from the infusion bag equal to the total volume of defibrotide solution to be added. Then add the defibrotide in to the bag and mix gently. Reconstitute each 500mg with 5ml W and each 2g vial with 20ml W then dilute with N/S, G or G/S. to any suitable volume (e.g. 500ml, 1000ml or 250ml). Example for treating acute iron poisoning: Reconstitute 5 x 2g vials each with 20ml W, remove 100ml from a 500ml bag of N/S and add the contents from the 5 x 2g vials to the bag then to produce 10g desferrioxamine in 500ml(=20mg/ml). The initial rate for will be 0.75ml/kg/hour (= 15mg/kg/hour). Displacements: 0.4ml/500mg Desferal® vial, 0.3ml/500mg Hospira vial and 1.5ml/2g vial (both brands). COMMENTS Monitor for side effects: bleeding, vomiting and hypotension are all common. Flush with N/S. The prepared infusion will be stable if stored in a fridge for upto 24 hours before use. Discard infusion if opalescent. Flush with N/S. May be infused into the blood line through a “Y” adaptor located near to the venous site of injection. For use in children with chronic iron overload follow the protocol on CYPOD (Childrens’ and Young Persons Outpatient Department). Desferrioxamine is incompatible with heparin solutions. Suggestion: Reconstitute as above then either dilute with N/S or give without If giving by SC infusion, monitor for further dilution. irritation or discomfort at the site of administration. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 62 DRUG METHOD Desmopressin SC injection 4micrograms in 1ml IM injection WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Groups Refer to the Marsden Manual for guidance on SC injection. 1,2,3,4 and 5 Groups Refer to the Marsden Manual for guidance on IM injection. 1,2,3,4 and 5 IV bolus Groups COMMENTS Flush after IV bolus with N/S. After repeated doses monitor for fluid overload; restrict fluid intake and check body weight regularly Suggestion: 1 minute Undiluted 1,2,3,4 and 5 (I) IV infusion Groups (Haemophilia 1,2,3,4 and 5 and Von Willibrands). Infusion pump is required. Desmopressin 15micrograms in 1ml (OCTIM Brand) For specialist use in Haematology patients SC injection 20 minutes Groups Tachycardia, hypotension and facial flushing may occur during infusion; monitor blood pressure continuously during infusion. For (I) IV infusion 100ml N/S can be used (unlicensed) if necessary but the 20 minute infusion time should be adhered to. Do not mix with other fluids or drugs Refer to the Marsden Manual for guidance on SC injection. 1and 2 (I) IV infusion Groups 1 and 2 Infusion pump is required. Dilute the dose to 50ml with N/S but see comments. 20 minutes Dilute the dose to 50ml with N/S but see comments. Tachycardia, hypotension and facial flushing may occur during infusion; monitor blood pressure continuously during infusion. Do not mix with other fluids or drugs. Restrict fluid intake and check body weight regularly. Continued monitoring of Factor VIII levels is recommended. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 63 DRUG METHOD Dexamethasone IV bolus or sodium (I) IV infusion phosphate via infusion pump IM injection WHO MAY GIVE ADMINISTER OVER Groups Give doses of May be diluted with N/S, G or H 4mg or less over to any convenient volume. 1 minute. Give large doses over several minutes. 1,2,3,4,5 & 8 Groups 1,2,3,4, 5 Intra-articular Group 1 Soft tissue infiltration (Intralesional) Nerve Root Blocks or Intrathecal use (Use Hospira 3.3mg in 1ml vials) SC injection for use in palliative care (C) SC infusion via syringe driver in palliative care Group 1 Group 1 INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Refer to the Marsden Manual for guidance on IM injection. Hospira and Hameln brands contain 4mg in 1ml of dexamethasone phosphate equivalent to 3.3mg dexamethasone in 1ml. For a 4mg dose of dexamethasone give 1.2ml over 1 minute. Flush IV doses with N/S. Anaphylactic reactions can occur. Aspen Pharma brand contains a quantity of dexamethasone phosphate equivalent to 3.8mg/ml dexamethasone. Prior to intra-articular injection, the joint fluid should be examined to exclude a septic process. Administer under strictly aseptic conditions. Licensed sites include: bursae, tendon sheaths and ganglia. *Restricted to those persons who are trained and competent to administer medication via the or Group 2* intrathecal route. Use Hospira 3.3mgin 1ml dexamethasone as it does not contain sulphites or disodium edetate which are potentially neurotoxic. Follow the PHNT Care of The Dying Pathways and the Refer to the Marsden Manual Groups PHNT Syringe Driver Policy. for guidance on SC injection. 1,2,3,4 & 5 For combinations of 2 or 3 drugs in the same syringe, refer to the Syringe Driver Drug Compatibility chart Dilute with W when 2 or more Continuous over Groups provided in the pump kit. Contact Pharmacy on ext. drugs are being mixed in the 1,2,3,4 & 5 24 hours 39976 for further compatibility advice if necessary. same syringe. W or N/S may be used when the N.B.Where dexamethasone ampoules/vials are syringe only contains this drug. labelled for IV, IM, intraarticular, intrabusal or intralesional use, they are suitable (but unlicensed) for subcutaneous administration. Administer in accordance with the Pain Management Centre procedures or current neurosurgical practice. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 64 DRUG METHOD WHO MAY GIVE ADMINISTER INSTRUCTION FOR DILUTION COMMENTS OVER AND SUITABLE DILUENT Dexrazoxane (Cardioxane®) (I) IV infusion Groups 15 minutes Infusion to be prepared by Pharmacy. Telephone Ext. 31083. Dexrazoxane (Savene®) (I) IV infusion Groups into a large vein in 1,3 and 5 extremity/area other than the one affected by the extravasation 1 – 2 hours Infusion to be prepared by Pharmacy. Telephone Ext. 31083. 1,3 and 5 A chemotherapy closed system bag spike should be used with a line adaptor to ensure the safe administration of Savene®. The air inlet port on the bag spike should be opened to allow free flow of Savene®. An air inlet needle should not be used in case of leakage during administration. Administer about 30 minutes before anthracycline (e.g. doxorubicin or epirubicin) administration. Handle as for cytotoxics. Wear gloves, gown and safety glasses when handling. Avoid handling drug if pregnant. Store the prepared infusion in the fridge and use within 6 hours of pharmacy preparation. The first infusion should be initiated as soon as possible and within the first six hours after the accident. Cooling procedures such as ice packs should have been removed from the area at least 15 min before the Savene administration in order to allow sufficient blood flow. Treatment Day 2 and Day 3 should start at the same hour (+/- 3 hours) as on the first day. Refer to the Guidelines for the administration of Savene(dexrazoxzane) for the treatment of extravasations caused by anthracyclines. Handle as for cytotoxics. Wear gloves, gown and safety glasses when handling. Avoid handling drug if pregnant. Store the prepared infusion in the fridge and use within 4 hours of pharmacy preparation. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 65 DRUG METHOD Diamorphine Staff prescribing, administering and/or screening prescriptions for opioid medications should be familiar with the PHNT Policy for Reducing Errors with Opioid Medicines in Adults using the following link: http://staffnet.plymouth.nhs.uk/Portals/1/Documents/Trust%20Documents/Medicines%20Management/Policy%20for%20Reducing%20D osing%20Errors%20with%20Opioid%20Medicines%20in%20Adults.pdf?timestamp=1443106367868 Observe respiratory rate (especially with IV IV bolus Maximum rate Usually reconstitute 5mg, 10mg , Groups bolus doses). Naloxone and resuscitation 30mg and 100mg ampoules with 1,2,3,4 and 5 1mg/minute 1ml W. Use a minimum of 2ml W to equipment should be available. For acute pain the IV dose will be a quarter to reconstitute 500mg ampoule. half of the corresponding IM dose. For elderly Can be diluted with N/S or G. and frail patients reduce the usual dose by half. Flush with N/S or G. Sodium content nil. IM injection Reconstitute as above. Refer to the Groups Marsden Manual for guidance on IM 1,2,3,4 and 5 injection. SC injection Reconstitute as above. Refer to the For use in palliative care follow the PHNT Care Groups of The Dying Pathways Marsden Manual for guidance on 1,2,3,4 and 5 SC injection. Continuous over 24 Reconstitute as above. Dilute further Follow the PHNT Care of The Dying Pathways (C) SC Groups with W when 2 or more drugs are and the PHNT Syringe Driver Policy. infusion via 1,2,3,4 and 5 hours being mixed in the same syringe. For combinations of 2 or 3 drugs in the same syringe driver W or N/S may be used where the syringe, refer to the Syringe Driver Drug in palliative syringe only contains diamorphine. Compatibility chart provided in the pump kit. care Contact Pharmacy on ext. 39976 for further compatibility advice if necessary. In chronic pain, the total daily dosage of IM or SC diamorphine is about one third of the equivalent total daily dosage of oral morphine. Administer in accordance with All syringes containing solution for epidural Epidural or Group 1 standard anaesthetic practice. administration should be labelled “For Epidural spinal injection Use Only” (NPSA/2007/21) WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 66 DRUG METHOD Diamorphine 50 micrograms/ml with bupivacaine 0.167% epidural infusion for adults All epidural administration sets and epidural catheters must be labelled “Epidural” when in use (NPSA/2007/21) Epidural Background rate of Pre-made bags supplied by *Staff administering and monitoring epidural Groups infusion via 0 -10 ml/hour with Pharmacy. infusions must have received training from 1and 2* McKinley additional Patientthe Acute Care Team and demonstrated their pump Controlled Epidural When these are not available the competency at administering and monitoring Analgesia (PCEA) of anaesthetist may prepare the epidural infusions. Follow the Acute Care 5ml boluses with a infusion in theatre, with the bag Team Protocols. Additional clinician boluses lock-out time of 30 labelled “For Epidural Use Only”. may be administered by Pain Nurses if minutes, if prescribed. required as per epidural protocol. IV bolus Maximum rate: 5mg Do not dilute. Flush with G (do not use N/S). Groups (1ml) per minute. 1,2,3,4 and 5 Use infusion within 6 hours. Diazepam is (I) IV infusion. groups Titrate dose to Dilute 2-8ml with 100ml G or adsorbed by plastic infusion equipment. Infusion G10%, to produce a 1,2,3,4 and 5 response. pump is concentration between 100It can be injected into the infusion tubing required. . 400micrograms/1ml. during an ongoing infusion of N/S, G or G10%. Diazepam emulsion (Diazemuls) (This is the preferred diazepam formulation for IV injection) Diazepam IV bolus WHO MAY GIVE Groups 1,2,3,4 and 5 (C) or (I) IV infusion. Infusion pump is required. Groups IM injection Groups 1,2,3,4 and 5 1,2,3,4 and 5 ADMINISTER OVER Suggestion for adults: Maximum rate 5mg (1ml) per minute Titrate dose to response. INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Undiluted Dilute with N/S or G to a concentration not exceeding 40mg in 500ml. Refer to the Marsden Manual for guidance on IM injection. COMMENTS Elderly or debilitated patients should be given not more than half of the usual dose. Flush with N/S or G. Give IV injections into a large vein to reduce local reactions (thrombophlebitis and thrombosis). It is recommended that patients should remain under medical supervision and in a supine position for at least one hour after administration. Resuscitation equipment should be available. Use infusion within 6 hours. Diazepam is adsorbed by plastic infusion equipment. The IM route should only be used when IV or oral administration is not possible. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 67 DRUG METHOD WHO MAY GIVE Diclofenac (C) or (I) Infusion. Do NOT give as IV bolus. Infusion pump is required. Groups 1 IM injection Groups 1 and 2 and 2 Dicobalt edetate IV bolus. Group 1 ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Treatment of post-op First add 0.5ml of 8.4%, or 1ml of pain: 4.2% sodium bicarbonate solution 75mg over to 100-500ml N/S or G with then 30 minutes - 2hours. add the contents of one ampoule Prevention of post-op (75mg diclofenac in 3ml). pain: 25-50mg over 15 minutes - 1 hour then (C) IV infusion at 5mg/hour. Give undiluted. Refer to the Marsden Manual for guidance on IM injection. Adults: Each 300mg dose over 1 minute, or in less severe poisoning over 5 minutes. Give undiluted. COMMENTS Only use if solution is clear. Once prepared, use infusion immediately. Maximum daily dosage is 150mg. Parenteral administration should not exceed 2 days. Flush with N/S or G. Sodium content: negligible. Do not infuse with any other drugs. By deep intragluteal injection into the outer quadrant. If a second IM injection of diclofenac is needed, it is advised that the other buttock is used. Each dose may be followed immediately with 50ml G 50%. 100% oxygen should be administered concurrently with Dicobalt Edetate. When the patient is fully conscious, it is unlikely that the extent of poisoning warrants the use of Dicobalt Edetate Injection. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 68 DRUG METHOD DigiFab ® (Digoxin Immune Fab) WHO MAY ADMINISTER OVER GIVE (I) IV infusion. Groups 30 minutes Infusion pump 1,2,3,4 and is required. 5 Bolus only if cardiac arrest seems imminent Digoxin Dihydroergotamine Group 1 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Reconstitute each vial with 4 ml W. Mix gently. The reconstituted solution may be further diluted to any convenient volume with N/S. Reconstitute as above. COMMENTS Can rarely cause anaphylaxis, allergic or febrile reactions. Resuscitation equipment should be available. Monitor blood pressure & body temperature. Monitor ECG continuously during and for at least 24 hours after Digibind. Hypokalaemia can develop- sometimes rapidly. Monitor serum potassium level carefully during and after DigiFab. ECG monitoring required. Flush with N/S. Emergency Loading Dose depends on age, lean body weight and renal function. Either avoid giving an IV loading dose, or give a reduced loading dose if digoxin has been taken within the last 2 weeks. Note that 500micrograms of IV digoxin is equivalent to 750micrograms of digoxin in tablet form. For plasma monitoring, take blood at least 6 hours after a dose. (I) IV infusion. Groups Emergency Loading Adults: Dilute loading and Dose of 500micrograms to Infusion pump 1,2,3,4 and maintenance doses to 50-100ml is required. 1mg infused over at least 2 with N/S. 5 hours (see comments), or alternatively give in divided doses at intervals of 4-8 hours, assessing clinical response before giving each additional dose, with each part-dose being given over 20 minutes. Maintenance dose (when patient unable to take by mouth or enteral feeding tube) infused over 1 hour. For the use of IV dihydroergotamine to treat migraine or cluster headache, follow a copy of the protocol from the Planned Investigation Unit (PIU). The protocol may also be found on Plymouth Healthnet > Depts > Pharmacy. Note that dihydroergotamine injection is an unlicensed product (see page 7). Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 69 DRUG METHOD Disopyramide Regimen 1 Slow IV bolus WHO MAY ADMINISTER GIVE OVER Groups Adults: 2mg/kg (maximum 150mg) 1 and 2 over at least 5 minutes INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Either give undiluted or dilute further with any suitable volume of N/S or G. COMMENTS ECG monitoring is necessary. Monitor for ventricular arrythmias, widening of QRS complex and lengthening of QT interval, hypotension, hypoglycaemia, myocardial depression, AV block and antimuscarinic side effects. Stop administration of disopyramide if width of QRScomplex or QT-interval increase by more than 25%, or hypogylaemia occurs. If cardioversion occurs during the injection, stop injecting the remainder of the dose. Disopyramide Regimen 2 This regimen should be used for patients who are unable to take disopyramide by mouth or who have serious arrhythmias being treated in critical or coronary care areas. Slow IV loading dose Groups 1 and 2 (C) IV Groups maintenance 1 and 2 infusion Adults: 2mg/kg Either give undiluted or dilute (maximum 150mg) further with any suitable volume of over at least 5 N/S or G. minutes Adults: 0.4mg/kg/hour Maximum 30mg/hour. Maximum total 800mg in 24 hours. Suggested dilution: Remove 50ml from a 500ml bag of N/S or G. Then add 500mg = 50ml of disopyramide injection into the bag to make a 1mg/ml dilution. If cardioversion is achieved (usually within 10-15 minutes after the first injection) but the arrhythmia recurs, a second dose of 2mg/kg (maximum 150mg) may be given by slow IV injection over at least 5 minutes (maximum of 300mg in the first hour, maximum of 800mg disopyramide by any route in 24 hours). Flush slowly with N/S. ECG monitoring is necessary. Monitor for ventricular arrythmias, widening of QRS complex and lengthening of QT interval, hypotension, hypoglycaemia, myocardial depression, AV block and antimuscarinic side effects. Stop administration of disopyramide if width of QRScomplex or QT-interval increase by more than 25%, or hypogylaemia occurs. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 70 DRUG METHOD WHO MAY GIVE Dobutamine (C) IV infusion Infusion pump is required. Groups 1 and 2 ADMINISTER OVER Adjust rate according to response. Administration via a central IV line is recommended* as solutions of dobutamine have a low pH. INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Dilute 250mg to at least 50ml with N/S or G (If no central IV access available see below*) COMMENTS Do not flush - replace giving set. Infusion may turn a harmless pink colour. Haemodynamic monitoring required. Sodium content: 0.046mmol/vial. Concentrations of up to 10mg/1ml have been used via a central IV line but this is An alternative dilution: For administration via a central IV line draw up milligrams of outside the manufacturer's recommendations. dobutamine equal to six times the patient’s body weight in kilograms, and dilute to *In circumstances where a central 100ml with N/S or G (or milligrams of venous catheter is not available and the dobutamine equal to three times the infusion is going to be run for more than patient’s body weight in kg in 50ml). The a couple of hours, use a solution of 1mg infusion rate set in ml/hour will equal in 1mL (250mg in 250ml N/S) and micrograms/kg/minute. administer via a large peripheral vein. Pump rate (ml/hour) = Prescribed rate (mcg/kg/min) x weight(kg) x 60(minutes in an hour) 1000 x concentration(mg/ml) Rate (mcg/kg/min) (I) IV infusion using infusion pump for cardiac stress testing. Infusion pump is required. = Pump rate(ml/hour) x concentration(mg/ml) x 1000 60 x weight(kg) Group 1 or See comments Group 7 Calculate the required amount of dobutamine and dilute to 50ml with N/S. Infuse at 10mcg/kg/min for 4 minutes, then 20mcg/kg/min for 4 minutes, then 30mcg/kg/min for 4 minutes, then 40mcg/kg/min. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 71 DRUG METHOD Dopamine (C) IV infusion. Infusion pump is and 2 required. WHO MAY GIVE Groups 1 ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT For administration via a central IV ECG monitoring usually required. Do not line draw up milligrams of flush - replace giving set. dopamine equal to six times the For peripheral administration use a dilute patient’s body weight in kilograms, solution and a large vein. Use a central Administration and dilute to 100ml with N/S, G, venous line for concentrations over via a central IV G10%, G/S or H (or milligrams of 1.6mg/ml. line is preferred dopamine equal to three times the Extravasation causes local vasoconstriction; as solutions of patient’s body weight in kg in 50ml). irrigate affected area with 5-10mg dobutamine The infusion rate set in ml/hour will phentolamine in 10-15ml N/S. have a low pH. equal micrograms/kg/minute. Sodium content 0.52mmol/200mg. Alternatively for administration via a central IV line dilute 200mg If no central IV access is dopamine to 50ml with N/S, G, available the G10%, G/S or H and infuse at the maximum calculated rate. For administration via a peripheral concentration for IV line add 400mg dopamine to infusion through a peripheral vein 250ml N/S and infuse at calculated is 1.6mg/ml. rate. Pump rate (ml/hour) = Prescribed rate (mcg/kg/min) x weight(kg) x 60(minutes in an hour) 1000 x concentration(mg/ml) Rate dependent on indication and response. Rate (mcg/kg/min) Dopexamine COMMENTS (C) IV infusion. Groups 1 Infusion pump is and 2 required. = Pump rate(ml/hour) x concentration(mg/ml) x 1000 60 x weight(kg) Adjust rate according Dilute with N/S, G, G/S or H to a to response. maximum concentration of 4mg/ml via a central IV line or a maximum concentration of 1mg/ml via a large peripheral vein. Infuse via a central vein or a large peripheral vein. Monitor BP, heart rate, ECG, urine flow and where possible cardiac output. Infusion may turn a harmless pink colour. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 72 DRUG METHOD WHO MAY GIVE ADMINISTER OVER Doxapram IV bolus Group 1 Minimum 30 seconds Eculizumab Edrophonium (C) IV Groups infusion. 1,2,3,4 and 5 Infusion pump is required. Adults: 1.5 – 4mg/minute = 45 – 120ml/hour using the 1g in 500ml infusion, increasing the rate gradually. (I) IV infusion. Groups 1 Infusion pump and 2 is required. 25 – 45 minutes IV bolus Group 1 For example, to give 900mg in 180ml N/S over 30 minutes, set the infusion pump at 360ml/hour. To give 1200mg in 240ml over 30 minutes, set the pump at 480ml/hour. INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Ampoule can be diluted with N/S, G or G10%. Adults: Dilute 1g doxapram in 500ml G. COMMENTS Flush with N/S or G. IV bolus dose may be repeated at one hour intervals if necessary. Monitoring of blood pressure, heart rate and deep tendon reflexes is recommended to prevent overdosage. Check arterial blood gases (ABGs) frequently (every 30 minutes suggested) after starting infusion. If no improvement increase infusion rate in suggested increments of up to 1 mg/min (to a maximum of 4 mg/min) Infusion to be prepared by Patients should be monitored for one hour Pharmacy. Telephone Ext. following infusion. If an adverse event occurs 31083. during the administration of eculizumab, the infusion may be slowed or stopped at the Doctor to prescribe each dose medical team’s discretion. If the infusion is as an infusion in N/S at a slowed, the total infusion time must not concentration of 5mg/ml, eg. exceed two hours in adults and adolescents prescribe 900mg eculizumab (aged 12 years to under18 years) and four in 180ml N/S hours in children aged less than 12 years. Prescribe 1200mg eculizumab Flush with N/S. in 240ml N/S. Sodium content: 5mmol/300mg eculizumab. Can be diluted with W, but Have atropine available to counteract maintenance of stability possible severe cholinergic reactions. In cannot be guaranteed. case of cholinergic crisis resuscitation equipment should be available. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 73 DRUG METHOD WHO MAY GIVE Enoxaparin Pre-filled syringes SC injection For dose banding and guidance on choice of syringe strength(s) and volumes to inject see the table below ADMINISTER INSTRUCTION FOR DILUTION AND OVER SUITABLE DILUENT Refer to the Marsden Manual for Groups guidance on SC injection. 1,2,3,4,5 and 8 COMMENTS Do not press the plunger before injecting to expel the air bubble. Hold the syringe so that the needle is pointing downwards (vertically at a 900 angle). Insert the full length of the needle into the skin fold. To avoid bruising, do not rub the injection site after giving the injection. Enoxaparin VTE Dosing Guidance Treatment Dose Weight (kg) 40 – 49 50 – 59 60 – 74 75 – 89 90 – 99 100 – 109 110 – 120 121 – 150 Continue for at least 5 days AND until two consecuive INRs >2.0 Separate protocol applies to pregnant women GFR > 30ml/minute (≈1.5mg/kg) 60mg Daily 80mg Daily 100mg Daily 120mg Daily Prophylactic Dose GFR < 30ml/minute (≈1mg/kg) 40mg Daily GFR > 30ml/minute 20mg Daily GFR < 30ml/minute 60mg Daily 80mg Daily 40mg Daily 20mg Daily 40mg TWICE Daily 40mg Daily 150mg Daily 100mg Daily 180mg Daily 120mg Daily Contact Consultant Haematologist For patients over 150kg or complex cases, advice may be obtained from a Consultant Haematologist. For patients requiring treatment doses who are morbidly obese (BMI> 35mg/m2), pregnant, or have significant renal impairment (eGFR <30ml/minute) monitor anti-Xa levels. Take the first anti-Xa level 3 hours after the 3rd dose and state time dose was administered and time of level take on blood form. Thereafter, repeat level if patient’s condition changes or advised by Haematology. For ACS patients, use fondaparinux unless patient’s eGFR < 30ml/minute, then use enoxaparin ≈1mg/kg daily as above. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 74 DRUG Enoximone Ephedrine METHOD WHO MAY GIVE (C) or (I) Groups IV 1 and 2 infusion via a pump. IV bolus Epoprostenol (C) IV infusion via a pump. ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Initial rate: 90 micrograms/ Dilute with an equal volume of W or kg/minute for 10-30 minutes until the N/S (i.e. dilute to a concentration of required haemodynamic response is 2.5mg/ml). achieved (This is 2.16ml/kg/hour using an infusion of 2.5mg/ml) then Maintenance rate: 5-20 micrograms/kg/minute. (This is 0.12ml/kg/hour to 0.48ml/kg/hour using an infusion of 2.5mg/ml) Must be diluted prior to Group 1 3-5 minutes administration with N/S (suggested dilution: 3mg in 1ml). Withdraw about 10ml of the diluent Groups See package insert. For use during CVVH on ICU, refer to provided, inject into the vial of 1,2,3,4 and the critical care protocol for epoprostenol and shake gently to 5 epoprostenol. dissolve the powder. Then draw up the reconstituted epoprostenol and re-inject via the filter into the remainder of the diluent Mix well. This is the “Concentrated solution” (10micrograms/ml). For use during CVVH on ICU, patient is initially acclimatized with systemic IV infusion of 2microgram/ml epoprostenol for 2 hours (10ml of “Concentrated solution” diluted further to 50ml with N/S). COMMENTS Flush with N/S. Extravasation will cause tissue damage. Do not administer unless diluted product is a clear yellow solution. Monitor blood pressure, heart rate, ECG and CVP. Incompatible: do not infuse with any other drugs including G and furosemide. Flush with N/S. Cardiac and blood pressure monitoring required until dose is titrated. Do not stop infusion for more than a few minutes. Replace giving set; do not flush. On the Derriford Hospital Critical Care Unit the prepared solution is used for up to 24 hours. This is unlicensed but cost-saving. A drop in blood pressure is possible when renewing an infusion that’s been made up longer than 12 hours. Sodium content 2.5mmol/reconstituted vial. Incompatible: do not infuse with any other drugs including G and G/S. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 75 DRUG METHOD Ergocalciferol 300,000unit injection IM Injection Ertapenem (I) IV infusion Groups 30 minutes via pump 1,2,3,4 and 5 May only be initiated on the advice of a consultant microbiologist Erythromycin (I) IV infusion Groups 20-60 minutes via pump 1,2,3,4 and 5 (C) IV infusion via pump (I) IV infusion via a central line using a pump WHO MAY ADMINISTER GIVE OVER Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 Groups Minimum 60 1,2,3,4and minutes 5 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Reconstitute the contents of the 1g vial with 10ml W or N/S to give a solution of approximately 100mg/ml. Shake well to dissolve. Dilute further with N/S to a final concentration of 20mg/ml or less (e.g.1g in 100ml N/S). Reconstitute each 1g with 20ml W to produce 50mg/1ml then further dilute to a maximum concentration of 5mg/ml with N/S, G or G/S. If G or G/S are used add 5ml sodium bicarbonate 8.4%/litre as a buffer. Displacement is allowed for. Addition of 20ml W to 1g vial gives 1g in 20ml (50mg in 1ml). Reconstitute as above then dilute as above to a concentration of 1mg/ml to 5mg/ml (1mg/ml is recommended). Reconstitute as above then dilute 1g to 100ml with N/S. COMMENTS The product packaging states “Only glass syringes should be used”, as the solution is very difficult to expel from ordinary plastic syringes. However, glass syringes are not available. The injection is easier to expel from green B.Braun 3ml syringes which are available from Pharmacy. One of these syringes should be supplied with each dispensed ampoule. Within Pharmacy, further supplies are available in T/Services. Use the infusion within 6 hours of preparation. The product information suggests using a 50ml bottle or bag of N/S but these are not stocked in this Trust. Sodium content: 6mmol/1g Extravasation is hazardous. IV infusion may cause thrombophlebitis, particularly concentrations exceeding 5mg/1ml. Flush with N/S. Sodium content nil. 125mg erythromycin used as prokinetic for GI tract (Unlicensed use - see page 7) should be diluted in 25ml N/S and given over 5 minutes. Prepare a fresh infusion every 8 hours. In addition to the above points, this is an unlicensed use for use in fluid restricted patients. Cardiac monitoring necessary. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 76 DRUG METHOD WHO MAY GIVE ADMINISTER OVER Follow the dosage titration flow chart in the package insert. INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Vials containing 100mg esmolol in 10ml (10mg/ml) are used without further dilution. COMMENTS (I) IV infusion via an Treatment of supraventricular tachycardia: After Groups infusion pump. Preferably 1 and 2 achieving adequate control of heart rate introduce administer via a central alternative oral agent and gradually reduce esmolol line to avoid potential infusion rate - see package insert for instructions. venous irritation as the Monitor the blood pressure frequently. Caution: Flushing preparation has a low pH. the line will administer a bolus dose. However 5ml N/S If this is not possible, use has been used as a flush following loading doses, given a large peripheral vein at the same slow rate as the loading dose. 10mg/ml IV infusion of esmolol for supraventricular tachycardia or post-operative tachycardia and/or hypertension Loading dose given before each titration step to produce rapid Maintenance Infusion Elapsed Time (Minutes) onset of action, infused over 1 minute (pump setting) (pump setting) Esmolol 0–1 1–5 5–6 6 – 10 10 – 11 11 – 15 15 – 16 16 – 20 20 - 21 21 – 25 25 – 26 26 - 30 500micrograms/kg (=3ml/kg/hour) 500micrograms/kg (=3ml/kg/hour) *500micrograms/kg (=3ml/kg/hour) *500micrograms/kg *500micrograms/kg *500micrograms/kg 50micrograms/kg/minute (=0.3ml/kg/hour) 100micrograms/kg/minute (=0.6ml/kg/hour) *150micrograms/kg/minute (=0.9ml/kg/hour *200micrograms/kg/minute (=1.2ml/kg/hour) *250micrograms/kg/minute (=1.5ml/kg/hour) *300micrograms/kg/minute (=1.8ml/kg/hour) (=3ml/kg/hour) (=3ml/kg/hour) (=3ml/kg/hour) *As the desired heart rate or endpoint (eg. Lowered blood pressure) is approached, omit the loading dose and reduce the incremental increases in infusion rate to 25micrograms/kg/minute (0.075ml/kg/hour to 0.15ml/kg/hour). The interval between titration steps may be increased from 5 to 10 minutes. Once the desired clinical endpoint is reached continue the maintenance infusion at that rate. 10mg/ml IV infusion of esmolol for intra-operative immediate control of tachycardia and/or hypertension 80 mg (approximately 1 mg/kg) bolus dose over 15 to 30 seconds followed by a 150 mcg/kg/min infusion (0.9ml/kg/hour), if necessary. Adjust the infusion rate as required up to 300 mcg/kg/min (1.8ml/kg/hour) to maintain desired heart rate and/or blood pressure. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 77 DRUG METHOD WHO MAY ADMINISTER OVER GIVE INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Esomeprazole IV bolus Groups Reconstitute 40mg vial with 5ml N/S. 1,2,3,4 and 5 (I) IV infusion Groups via infusion 1,2,3,4 and pump 5 Esomeprazole IV Loading For the specialist dose of treatment of 80mg endoscopically controlled bleeding peptic ulceration. (C) IV infusion via infusion pump Ethanol (Alcohol) (C) IV infusion via (Unlicensed infusion product- see page pump 7) . Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 At least 3 minutes COMMENTS The reconstituted solution is clear and colourless to very slightly yellow. Revert to omeprazole capsules orally as soon 10 – 30 minutes Reconstitute as above then further as possible. Alternatively revert to dispersible lansoprazole Fastabs via PEG/NG/NJ as soon dilute up to 100ml with N/S. as possible. Use infusion in N/S within 12 hours. Do not infuse with any other drugs. 80mg in 100ml N/S over For each 40mg vial, withdraw 5ml of Use infusion in N/S within 12 hours. 30 minutes N/S from a 100ml bag and use to Do not infuse with any other drugs. reconstitute the vial. Then inject the reconstituted esomeprazole into the * The Gastroenterologists have agreed to a 70bag. Do not add more than 80mg hour treatment (rather than 72 hours). A preesomeprazole to 100ml of diluent. printed prescription is available. After loading dose, infuse Reconstitute and dilute each 40mg at 8mg/hour for 70 hours* vial as above. (This is 10ml//hour with each 80mg in 100ml N/S) For ethylene glycol or Dilute to 5 or 10% with G. Flush with N/S or G. methanol overdose: 10% solutions of ethanol are hyperosmolar and For a 5% solution: irritant to veins and are best given by central Refer to the Toxbase Remove 56ml from a litre bag of 5% venous catheter. Website for details of the glucose. Then add 56ml of 90% Some references recommend discontinuing infusion rates. ethanol injection into the bag. gradually over 24-48 hours to avoid a possible major secondary withdrawal reaction. For a 10% solution: For ethylene glycol overdose adjust infusion Remove 111ml from a litre bag of rate to achieve blood ethanol conc. of 1- 1.5g/L. 5% glucose. Then add 111ml of Monitor blood glucose level. 90% ethanol injection into the bag. Always refer to the Toxbase website for more detailed instructions in the case of ethylene glycol or methanol overdose. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 78 DRUG METHOD WHO MAY GIVE ADMINISTER OVER Etomidate IV bolus Group 1 30 – 60 seconds Fentanyl Staff prescribing, administering and/or screening prescriptions for opioid medications should be familiar with the PHNT Policy for Reducing Errors with Opioid Medicines in Adults using the following link: http://staffnet.plymouth.nhs.uk/Portals/1/Documents/Trust%20Documents/Medicines%20Management/Policy%20for%20Reducing%20 Dosing%20Errors%20with%20Opioid%20Medicines%20in%20Adults.pdf?timestamp=1443106367868 IV bolus Monitor the patient in accordance with the Groups 1 Follow the algorithm Dilute 200 micrograms fentanyl to (Theatre from Recovery 2 10ml with N/S algorithm from Recovery 2. and 2 Recovery) IV bolus Can be diluted with N/S, G, G/S or For sedation in conscious adult patients follow Groups 1 H. the Sedation Guidelines on Plymouth Healthnet and 2 (under Clinical Guidelines). All healthcare practitioners involved directly or participating in sedation techniques must have the necessary knowledge, skills and competences required. Flush with N/S. Patient 1000 micrograms fentanyl (20ml of PCA: 20 microgram (1ml) bolus, 5 minute lock Groups Controlled 1,2,3,4 and 5 injection) diluted to 50ml with N/S. out period. Follow the Acute Pain/Care Service Analgesia Protocols. (PCA) (I) or (C) IV Groups 1 Sodium content 0.3mmol/1ml. infusion. and 2 Infusion pump is required. INSTRUCTION FOR DILUTION AND SUITABLE DILUENT May be diluted with N/S or G. COMMENTS Pain can occur after injection into veins of the dorsum of the hand. Use of larger veins reduces pain on injection. Incompatible with Hartmann’s. Flush with N/S or G. Can reduce serum cortisol levels during induction so no longer kept in Main Theatres Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 79 DRUG WHO MAY ADMINISTER OVER INSTRUCTION FOR DILUTION COMMENTS GIVE AND SUITABLE DILUENT All epidural administration sets must be labelled “Epidural” when in use (not just the epidural catheter) NPSA/2007/21 Fentanyl 2micrograms/ml Epidural Pre-made bags supplied by *Staff administering and monitoring epidural Groups Background rate of with bupivacaine infusion via 7 – 15ml/hour with Pharmacy. infusions must have received training from the 1and 2* 0.1% epidural McKinley pump additional PatientAcute Care Team and demonstrated their infusion Controlled Epidural competency at administering and monitoring Analgesia (PCEA) of epidural infusions. Follow the Acute Care Team 5ml boluses with a Protocols. Additional clinician boluses may be lock-out time of 30 administered by Pain Nurses if required as per minutes. epidural protocol. Ferric For doses of Groups Suggestion: 2 Either give undiluted or dilute with a Inspect vials visually for sediment and damage carboxymaltose 100-200mg: before use. Use only those that are sedimentsmall volume N/S eg.10ml N/S 1,2 and 8 minutes (Ferinject®) free. IV bolus (No more than 50ml of N/S). The patient should be monitored closely for signs of hypersensitivity during administration ▼ This product is For doses of Groups 6 minutes For slow IV bolus, either give and for 30 minutes after every dose of being intensively 201-500mg: undiluted or dilute with a small 1,2 amd 8 Ferinject® given. monitored by the Either slow IV volume N/S eg.10ml. CHM and MHRA. A single dose of Ferinject® should not exceed bolus or (I) IV Please report all 1000mg. Do not administer 1000mg more than infusion via For IV infusion, dilute with no more once a week. If the total dose is greater than suspected pump than 100ml N/S. 1000mg then it should be divided and given reactions For doses of Groups 15 minutes Either give undiluted or dilute with over 2 weeks. (including non501-1000mg: 1,2 and 8 N/S (No more than 250ml of N/S). Dilutions less than 2mg/ml are unstable. serious ones) (I) IV infusion Do not mix with any other infusion or drug using a Yellow solutions, including glucose. Card from the BNF via pump Flush with N/S. Each 50mg in 1ml of Ferinject® contains 0.24mmol sodium. METHOD Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 80 DRUG METHOD Ferumoxytol IV Bolus WHO MAY ADMINISTER INSTRUCTION FOR DILUTION AND GIVE OVER SUITABLE DILUENT Groups Maximum rate Do not dilute further. 1,2,3,4 and 1ml/second (i.e. the 5 contents of each 17ml vial over at least 17 seconds). ▼ This product is being intensively monitored by the CHM and MHRA. Please report all suspected reactions (including nonserious ones) using a Yellow Card from the BNF Filgrastim SC injection Groups (Zarzio®) Post chemotherapy, 1,2,3,4,5 Chronic neutopenia, and 8 or HIV Short IV infusion Groups Post chemotherapy 1,2,3,4,5 or for mobilisation of and 8 PBPCs after bone marrow transplant Continuous SC or Groups IV infusion for 1,2,3,4, 5 mobilisation of and 8 PBPCs after bone marrow transplant Do not dilute further. Refer to the Marsden Manual for guidance on SC injection. 30 minutes Over 24 hours Dilute the required dose in 20ml G to produce a final concentration of at least 1.5MU/mL (15micrograms/mL; 300micrograms in 20ml). COMMENTS Follow the administration with a slow flush of N/S to clear the line. Monitor the patient for signs of hypotension and hypersensitivity reactions for at least 30 minutes after giving the injection. The maximum dose for a course of treatment is 2 vials, but these must not be given at the same time (The second injection should be given 2 to 8 days after the first injection). Within its shelf-life and for the purpose of ambulatory use, the patient may remove the product from the refrigerator and store it at room temperature (not above 25°C) for one single period of up to 72 hours. At the end of this period, the product should not be put back in the refrigerator and should be disposed of. Do not dilute to a concentration of less than 0.2MU/ml (2micrograms/ml). Flush with G. If a concentration of less than 1.5MU/ml (15micrograms/ml; equivalent to less than Zarzio® is not compatible with saline 300micrograms in 20ml) is prepared in glucose solutions. 5%, add human serum albumin to a final concentration of 2mg/ml (e.g. in a final volume of 20mL add 0.2ml 20% human serum albumin). This is to reduce the amount of filgrastim adsorbed on to the surface of the administration set. Do not shake the syringe before removing the required dose. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 81 DRUG METHOD Flebogamma® Flecainide See Immunoglobulin Human Normal IV bolus Groups In an emergency or for Adults: rapid effect, give over at 1 and 2 2mg/kg least 10 minutes. Minimum Maximum 30 minutes for patients with 150mg cardiac failure or ventricular tachycardia. (I) IV Groups Adults: Loading dose over 30 minutes as above infusion. 1 and 2 Infusion followed by IV infusion at pump is 1.5 mg/kg/hour for the first required. hour then 0.1-0.25 mg/kg/hour thereafter. Using a 300mg in 50ml dilution, this is 0.25ml/kg/hour for the first hour then 0.017 – 0.042ml/kg/hour thereafter. WHO MAY ADMINISTER OVER GIVE INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Can be diluted with G and given Flush with G. as a mini-infusion (e.g. 50ml or Continuous ECG monitoring required for bolus 100ml of G). doses. It is recommended that the maximum duration by infusion is 24 hours. The maximum cumulative dose in the first 24 hours should not exceed 600mg. Suggested dilution for Switch to oral treatment as soon as possible. maintenance infusion: Dilute If infusion in N/S or H is necessary 150mg 300mg to 50ml with G. flecainide must be diluted in at least 500ml. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 82 DRUG METHOD Flucloxacillin IV bolus Usual method (I) IV infusion. via pump IM Injection Intrapleural Intra-articular Fluconazole (I) IV infusion. Infusion pump is required. Flucytosine (I) IV infusion. Infusion pump is required. WHO MAY ADMINISTER OVER INSTRUCTION FOR DILUTION AND COMMENTS GIVE SUITABLE DILUENT Flucloxacillin is a penicillin – Check patient’s allergy status before administration Inject doses up to 1g Reconstitute 250-500mg with 5-10ml and Flush with N/S. Groups 1g with 15-20ml W. Can be diluted with Sodium content 0.57mmol/250mg. 1,2,3,4 and 5 over 3-4 minutes N/S or G. Displacement volumes: Inject 2g doses For IV administration: The following slowly over 6-8 Bowmed/Actavis brand: 0.15mL for drugs are incompatible with minutes or give by 250mg, 0.3mL for 500mg, 0.6mL for 1g. flucloxacillin: amiodarone, atropine infusion (see below). Wockhardt brand: 0.2mL for 250mg, sulphate, buprenorphine, calcium 0.4mL for 500mg, 0.7mL for 1g. gluconate, chlorpromazine hydrochloride, 30-60 minutes Reconstitute as above then dilute with ciprofloxacin, diazepam, dobutamine Groups N/S or G to 100ml. hydrochloride, erythromycin lactobionate, 1,2,3,4 and 5 Add 1.5ml of water for injections to 250mg gentamicin sulphate, metoclopramide Groups vial contents or 2ml of water for injections hydrochloride, morphine sulphate, 1,2,3,4 and 5 netilmicin sulphate, ofloxacin, to 500mg vial contents. Refer to the papaveretum, pethidine hydrochloride, Marsden Manual for guidance on IM prochlorperazine edisylate, promethazine injection. Dissolve 250mg in 5 to 10ml of water for hydrochloride, tobramycin and verapamil Group 1 hydrochloride. injections. Dissolve 250 to 500mg in up to 5ml of Group 1 water for injections or 0.5% lidocaine hydrochloride solution for injection. 10-20mg/minute. Set Provided ready diluted (2mg/ml). Flush with N/S. Groups the pump at 300 – Fluconazole is well absorbed from the 1,2,3,4 and 5 600ml/hour gut so consider an early switch to oral/NG/PEG treatment. Sodium content 15mmol/200mg (100ml bottle). 20-40 minutes Provided ready diluted. Flush with N/S. Must be stored at 18oC Groups Can be administered concurrently with to 25oC. Sodium content 1,2,3,4 and 5 N/S, G or G/S. 34.5mmol/250ml. Infusion must not be used as a multidose container. Incompatible: do not infuse with any other drugs except N/S, G, or G/S. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 83 DRUG METHOD Flumazenil IV bolus WHO MAY GIVE ADMINISTER OVER Minimum 15 Groups 1,2,3,4,5 and 8 seconds (I) IV infusion. Infusion pump is required. Groups IV bolus Group 1 or F Folic acid IV bolus Folinic acid (calcium folinate) IV bolus grade Group 2 with ENB346 or relevant ophthalmic qualification Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 Fluorescein Fomepizole (I) IV infusion via infusion pump (I) IV infusion via infusion pump 1,2,3,4 and 5 Groups 1,2,3,4 and 5 INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Can be diluted with N/S or G to any Flush with N/S. suitable volume. Give (I) IV infusion if drowsiness recurs after initial IV bolus. 100-400 Flumazenil infusion should be used within 3 micrograms/ hour hours of preparation. Incompatible: do not infuse with any other drugs. Test dose in 5ml N/S then 3-5ml of Follow the REI Fluorescein Angiograhy 10%-20% fluorescein injection Guidelines followed by N/S flush. Suggestion: 1 minute Minimum 3-5 minutes Maximum rate of 160 mg/minute All doses should be infused over 30 minutes Can be diluted with N/S Flush with N/S. Flush with N/S. Can be diluted with N/S. Folinic acid (calcium folinate) 350mg contains 0.7mmol of calcium therefore administer slowly. Intravenous incompatibilities include: Dilute with N/S or G. droperidol, methotrexate, 5-fluorouracil and foscarnet. Dilute each calculated dose of If the fomepizole injection has become solid in fomepizole injection with N/S or G the vial, the solution should be liquefied by to a final volume of 250ml or 500ml running the vial under warm water or by holding and mix well. in the hand (solidification does not affect efficacy or stability of the product) (Can be diluted with 100ml N/S or Continue treatment with fomepizole until the G if patient is fluid restricted) plasma ethylene glycol or methanol concentration is either undetectable or has been reduced below 50mg/L and acidosis and signs of systemic toxicity have resolved. Refer to the Toxbase website for full details. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 84 DRUG METHOD Fondaparinux Deep SC injection. Alternate sites For the treatment between the left & of Acute right anterolateral Coronary and left & right Syndrome posterolateral abdominal wall. Insert the whole length of the needle at right angles into the skin. Foscarnet (I) IV infusion. sodium Initial loading dose. Infusion pump is required. (C) IV infusion Maintenance therapy. Infusion pump is required. Fosfomycin (I) IV infusion. (Fomicyt®) Infusion pump is required WHO MAY ADMINISTER GIVE OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Groups To avoid the loss of fondaparinux solution, do not expel the air bubble from the pre-filled syringe before injection. 2.5mg once daily initiated as soon as possible following diagnosis and continued for up to 8 days. The medical team can stop the treatment once the patient has had no chest pain for 48 hours. For patients with ACS and an eGFR less than 30ml/minute, prescribe 1mg/kg enoxaparin once daily instead. 1,2,3,4 and 5 Refer to the Marsden Manual for guidance on SC injection. Groups Minimum Infusion to be prepared by 1,2,3,4 and infusion time of Pharmacy. Telephone Ext 31083. 1 hour. 5 Groups 1,2,3,4 and 5 Groups 2g over at least 1,2,3,4 and 15 minutes. 4g over at least 5 30 minutes. 8g over at least 60 minutes. Dissolve 2g fosfomycin (Fomicyt®) in 50ml W, G or G10%. Dissolve 4g fosfomycin (Fomicty®) in 100ml W, G or G10%. Dissolve 8g fosfomycin (Fomicyt®) in 200ml W, G or G10%. On dissolution the solution becomes slightly warm. Displacement values: 1ml for the 2g vial 2ml for the 4g vial 4ml for the 8g vial Can be infused undiluted via a central line. Flush with N/S or G. Sodium content 15.6mmol/1g. Incompatible: do not infuse with any other drugs. Peripheral administration may lead to local irritation and thrombophlebitis. DO NOT administer by rapid intravenous injection. Wear gloves, gown and safety glasses when handling. Avoid handling drug if pregnant. Do not infuse with any other drugs. Avoid inadvertent intra-arterial administration. 2g vial contains 27.8mmol sodium 4g vial contains 55.6mmol sodium 8g vial contains 111.3mmol sodium Flush with N/S. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 85 DRUG METHOD Fosfomycin (Fosfocina®) (I) IV infusion. Groups Infuse all doses over 1 Reconstitute the 4g vial with 20ml of W. Infusion pump 1,2,3,4 and 5 hour Reconstitute each 1g vial with 10ml W is required. (ampoule provided). Upon dissolving, the vial will become slightly warm. To give a 4g dose, remove 50ml G from a 250ml bag of G. Then add 4g of reconstituted fosfomycin into the bag containing 200ml G. To give a 2g dose, add 2g reconstituted fosfomycin to 100ml G. (I) IV infusion. Groups Infuse all doses over Reconstitute the 2g bottle with 40ml to Infusion pump 1,2,3,4 and 5 30 minutes 60ml W and begin infusion immediately. is required. Reconstitute the 3g and 5g bottles with 100ml W. Reconstitute the 8g vial with 200ml W. Begin the infusion immediately after reconstitution. During reconstitution the solution may get warm. If necessary G or G10% may be used instead of W to reconstitute the bottles (volumes as for W). Do not further dilute. N.B. This brand is unlicensed Fosfomycin (Infectofos®) WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Sodium content 14.35mmol/1g fosfomycin Incompatible with the following drug solutions: erythromycin, gentamicin and rifampicin. Flush with N/S. Sodium content 14.5mmol/1g fosfomycin Monitor serum electrolytes, in particular serum sodium, potassium and creatinine. Monitor patient for phlebitis at the infusion site. Flush with N/S. Safe to be given to patients with allergies to any other commonly used antibiotics including penicillins, cephalosporins, levofloxacin, tetracyclines, trimethoprim and erythromycin. On storage the bottles should be protected from light (Keep in original box) Furosemide IV bolus Adults: The rate Either dilute with N/S (a common dilution is Flush with N/S. Groups 1mg/ml) or give undiluted. Sodium content 0.14mmol/1ml for 20mg/2ml 1,2,3,4,5 and should not usually exceed 4mg/minute, and 50mg/5ml; 0.04mmol/1ml for (C) or (I) IV 7 however single doses 250mg/25ml. Rapid administration may infusion. of up to 80mg may be damage the hearing. Furosemide Infusion pump given more quickly. precipitates in glucose solutions. is required. See Sodium Fusidate Fusidic Acid Gallamine IV bolus Flush with N/S. Group 1 Gammanorm® See Immunoglobulin Human Normal Gammapex® See Immunoglobulin Human Normal Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 86 DRUG METHOD Ganciclovir (I) IV infusion. Infusion pump is required. Gentamicin IV bolus WHO MAY GIVE ADMINISTER OVER Minimum 60 Group 1 or minutes Group 2 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Infusion to be prepared by Pharmacy. Telephone Ext. 31083. Doctor to prescribe dose (see comments) in 100ml N/S or G. Groups Either give undiluted or dilute with N/S or G (usually 10-20ml). 1,2,3,4 and 5 Refer to the Plymouth Healthnet Clinical Guidelines/ Infection Control for the use and current dosage of gentamicin, teicoplanin and vancomycin. (I) IV infusion for once-daily dosing (>200mg). Infusion pump is required. Groups Intraperitoneal Groups 1 and 1,2,3,4 and 5 2 IM injection Groups Discuss further with a 1,2,3,4 and 5 Consultant Microbiologist if unable to give gentamicin via the IV route Glargine insulin See Insulin Section page 3-5 minutes (minimum 3 minutes) 30 minutes Dilute with 50ml or 100ml N/S or G. COMMENTS To facilitate accurate measurement of the dose, the prescribed dose in milligrams (rounded up or down if necessary) divided by 50 should have no more than one decimal figure. Wear gloves, gown and safety glasses when handling. Avoid handling drug if pregnant or trying to become pregnant. Do not infuse with any other drugs. Preferably infuse through a large vein. Flush with N/S or G. Administration by (I) IV infusion once a day is current Trust policy, although this use is outside of the manufacturer’s recommendations. Flush with N/S. Sodium content negligible Incompatibilies include benzylpenicillin and teicoplanin. Follow the Renal Services Directorate Peritoneal Dialysis Peritonitis Protocol Refer to the Marsden Manual for guidance on IM injection. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 87 DRUG METHOD WHO MAY GIVE Glucagon SC Injection Groups 1,2,3,4,5 and 6 IM Injection Groups 1,2,3,4,5 and 6 IV bolus Groups (For diagnostic 1,2,3,4,5 and 6 testing) IV bolus (Loading dose) followed by (I) IV infusion. Infusion pump is required. Groups 1,2,3,4 and 5 ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Reconstitute with diluent provided (1ml W) and shake gently until the glucagon has dissolved and the solution is clear. The resulting solution is 1mg/ml. Do not further dilute. Refer to the Marsden Manual for guidance on SC injection. Reconstitute as above. Refer to the Marsden Manual for guidance on IM injection. COMMENTS Intravenous glucose must be given if the patient fails to respond to Glucagon within 10 minutes. Intravenous glucose must be given if the patient fails to respond to Glucagon within 10 minutes. Flush with N/S. Reconstitute as above. However, for doses > 2mg reconstitute each vial with 1ml G instead of the diluent provided, to avoid administration of large amounts of preservative. Treatment of cardiogenic shock caused by beta-blocker poisoning Loading dose of 2 -10mg For loading doses > 2mg reconstitute each vial with (I) IV infusion is an unlicensed use (See page 7) to treat cardiogenic (Child: 50 – 150 1ml G instead of the diluent provided, to avoid shock from beta blocker poisoning. administration of large amounts of preservative. microgram/kg, max. 10mg) by slow IV bolus Suggestion for the infusion for an adult: over 3 – 5 minutes Reconstitute 10 x 1mg vials, each with 1ml G (Do followed by IV infusion not use the diluent provided as the patient will get a of 50 micrograms/kg/hour: large dose of preservative). Using syringe pump Using 1mg/ml glucagon Draw up the reconstituted glucagon into a 50ml for infusion: syringe and either infuse undiluted (1mg/ml) or 50micrograms/kg/hour dilute further with G. = 0.05ml/kg/hour Using a volumetric pump Using a dilution of 10mg Draw up the reconstituted glucagon and dilute further with G. (suggestion for an adult: 10mg in 100ml for infusion: glucagon diluted to a volume of 100ml with G. 10ml 50micrograms/kg/hour G from the bag can be used to reconstitute the 10 = 0.5ml/kg/hour vials of glucagon). Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 88 DRUG METHOD WHO MAY GIVE Glucose 5-10% N.B All bags of glucose are for single use only. IV bolus Groups 1,2,3,4 and 5 (C) or (I) IV infusion Groups (C) or (I) IV infusion Groups or Glucose 10% to treat severe hypoglycaemia IV infusion via infusion pump Groups Glucose 50% to treat severe hypoglycaemia IV bolus via a central vein. Groups Glucose 20-50% ADMINISTER OVER 1,2,3,4,5 and 8 INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Glucose infusions can be diluted G5% is iso-osmotic with blood and can be infused with W if the concentration required through a peripheral line. is unavailable. If G10% is administered peripherally use a large vein and preferably alter the injection site daily. Concentrations greater than 20% should be infused through a central line to prevent venous irritation and thrombophlebitis. 1,2,3,4 and 5 1,2,3,4 and 5 1,2,3,4 and 5 150-200ml 10% glucose over 15 minutes Refer to the PHNT Hypoglycaemia Guideline 2014 for detailed guidance). 20ml of 50% glucose over 1-2 minutes 20ml of 50% glucose over 1-2 minutes is very irritant and potentially damaging to peripheral veins. Glucose 10% to (I) IV infusion Groups treat hyperkalaemia via a large 1,2,3,4 and vein 5 500ml of 10% glucose over 30 minutes Add 10 units of Actrapid insulin into the 500ml of 10% glucose using a 29 gauge Magellan 12.7mm (1.3cm) Insulin Safety Syringe available from Thrushel, Tavy or ED (NHS order code: FTR1276) For patients at risk (I) IV infusion Groups from heart failure or via a large 1,2,3,4 and fluid overload : vein 5 Glucose 50% to treat hyperkalaemia 50ml of 50% glucose over 15 minutes Add 10 units of Actrapid insulin into Monitor U&E’s every 2 hours until the serum the 50ml of 50% glucose. potassium is stable and less than 6mmol/L. Monitor blood glucose every 30 minutes during the infusion of glucose with Actrapid, and for 2 hours after the infusion Monitor U&E’s every 2 hours until the serum potassium is stable and less than 6mmol/L. Monitor blood glucose every 30 minutes during the infusion of glucose with Actrapid, and for 2 hours after the infusion Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 89 DRUG METHOD WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Glucose 5% (C) SC infusion Only use gravity-feed administration sets. Never use an infusion pump for SC infusions. (C) or (I) IV infusion via pump Groups Usual rate is 500ml over 8 hours (21 drops per minute). Maximum rate is 500ml over 4 hours (40 drops per minute) Maximum concentration of glucose for SC infusion is 5% Maximum of 2 litres of glucose 5% in 24 hours. The needle and giving set should preferably be changed every 72 hours. However, infusion sets can be left in place for up to 5-7 days if there are no complications. Refer to potassium chloride monograph for SC potassium. Due to the acidic pH of glucose 5%, monitor the infusion site regularly for early signs of inflammation and irritation. Glyceryl trinitrate 1,2,3,4 and 5 Groups 1 0.6 - 12 mg/hour and 2 Intra-coronary Groups in Cardiac 1,2 and 8 Catheter Labs. Use the 50mg in 50ml ready-made vials. If these are not available Up to a maximum dilute with G to 1mg/ml. of 24 mg/hour Can be diluted with N/S instead. depending on indication. Give via a PVC-free or PE/PVC (PE –lined) extension set. Do not flush - replacing giving set. Monitor blood pressure and pulse during infusion. Follow Cardiac Catheter Laboratory procedures. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 90 DRUG METHOD Glycopyrronium IV bolus (Glycopyrrolate) IM injection WHO MAY GIVE ADMINISTER OVER Groups 1 Rapid IV bolus and 2 Groups 1 Groups May be diluted with N/S or G if needed. Flush with N/S or G. Refer to the Marsden Manual for guidance on SC injection. 1,2,3,4 and 5 (C) SC infusion Groups via syringe 1,2,3,4 and driver to reduce 5 secretions in palliative care COMMENTS Refer to the Marsden Manual for guidance on IM injection. and 2 SC injection to reduce secretions in palliative care INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Continuous over 24 hours Dilute with W when 2 or more drugs are being mixed in the same syringe. W or N/S may be used where the syringe only contains glycopyrromium. Follow the PHNT Care of The Dying Pathways and the PHNT Syringe Driver Policy. For combinations of 2 or 3 drugs in the same syringe, refer to the Syringe Driver Drug Compatibility chart provided in the pump kit. Contact Pharmacy on ext. 39976 for further compatibility advice if necessary. Glycopyrronium is not licensed via the SC route (See page 124). Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 91 DRUG METHOD Glypressin Gonadorelin See Terlipressin. IV bolus or SC Group 1 Injection (for pituitary function test) IV bolus Minimum 30 seconds Groups 1,2,3,4,5 and (I) IV infusion 5 minutes 8 (Adults). Infusion pump is required. IM injection Groups 1,2,3,4 and 5 Granisetron Haloperidol IV bolus SC injection for use in palliative care (C) SC infusion via syringe driver in palliative care WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Reconstitute 100microgram vial with 1ml W. COMMENTS Refer to the Marsden Manual for guidance on SC injection. Dilute each 1mg with 5ml with N/S. Flush with N/S. Dilute each 3mg with 20-50ml N/S, Sodium content 1.17mmol/3mg vial, H, G or G/S. 0.15mmol/1mg vial. Oral treatment should succeed IM administration as soon as practicable. Oral bioavailability is about 60% of that from the IM route so adjustment of the dosage may be necessary. 1-2 minutes, longer if Do not dilute to give by IV route. Flush with N/S. Groups Note that haloperidol injection is no longer 1,2,3,4 and 5 possible. Maximum licensed by the IV route in the UK. This is not due 5mg/minute. to any new safety concerns about IV haloperidol. The manufacturer has only taken this action to standardise the license across all global markets. Refer to the Marsden Manual for Follow the PHNT Care of The Dying Pathways and Groups guidance on SC injection. the PHNT Syringe Driver Policy. 1,2,3,4 and 5 For combinations of 2 or 3 drugs in the same Continuous over 24 Dilute with W when 2 or more drugs syringe, refer to the Syringe Driver Drug Groups Compatibility chart provided in the pump kit. are being mixed in the same 1,2,3,4 and 5 hours Contact Pharmacy on ext. 39976 for further syringe. compatibility advice if necessary. W or N/S may be used where the Haloperidol is not licensed by the SC route (See syringe only contains haloperidol. page 4). Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 92 DRUG METHOD WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Heparin IV bolus loading dose followed by (C) below. Groups 3 – 5 minutes (C) IV infusion Immediately following the loading dose. Infusion pump is required. Groups 5,000 units = 5ml of 1,000 unit/ml solution with no further dilution. (Or 10,000 units = 10ml of 1,000 unit/ml solution with no further dilution for severe pulmonary embolism – see prescription). Take a 20ml ampoule containing 20,000 units of heparin. Draw up the 20ml into a 50ml syringe. SC injection Groups Intraperitoneal Hizentra® Humalog® Humalog Mix® Humulin® 1,2,3,4 and 5 Initial infusion rate 15 1,2,3,4 and 5 units/kg/hour = 0.015ml/kg/hour of 1,000 unit/ml infusion. COMMENTS Use of a PVC-free or PE/PVC (PE-lined) extension set will avoid adsorption of heparin to the line. Prepare a fresh infusion every 24 hours. Do not dilute this any further Alter rate according to APTTR (Check before commencing heparin therapy, then 4-6 hours after commencing the infusion, 4-6 hours after every infusion rate change, and at least once daily thereafter. Refer to the Marsden Manual for guidance on SC injection. 1,2,3,4 and 5 1,000 units per litre of dialysis fluid Follow the PHNT Renal Services Directorate Groups 1 Procedures and 2 Groups1, Heparin may only be used for locking or flushing IV lines, cannulae or devices in accordance with PHNT policy – see Appendix 3, page 208 2, 4 and 8 Flushing or locking IV access device See Immunoglobulin Human Normal See Insulin Section Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 93 DRUG METHOD WHO MAY ADMINISTER GIVE OVER Groups 1,2,3,4 and 5 Hyaluronidase With S/C infusion of fluid (Hypodermoclysis) Either give 1,500iu by S/C injection into the site before the infusion is set up, or iniect 1,500iu into the tubing of the infusion set about 2cm back from the needle at the start of the infusion. With S/C and I/M Groups injections 1,2,3,4 and 5 INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Reconstitute 1,500iu of 1,500iu hyaluronidase is sufficient for the hyaluronidase with 1ml of N/S administration of 500-1000ml of most fluids. or W. Compatible fluids include: N/S, G, G/S(4%/0.18%), G/S(2.5%/0.45%). 1,500iu to be dissolved directly in the solution to be injected. Compatible when mixed with: morphine, diamorphine, hydrmorphone, chlorpromazine, metoclopramide, dexamethasone and very low concentrations of adrenaline. Incompatible with: heparin, moderate to high concentrations of adrenaline, furosemide, phenytoin and benzodiazepines. With local anaesthetics Group 1 (Other Groups only in accordance with specific PGDs) Groups 1,2,3,4 and 5 Extravastion where dispersal rather than localisation is indicated. Administer by S/C infiltration Haematoma Groups By S/C infiltration 1,2,3,4 and 5 1,500iu mixed with the quantity of local anaesthetic solution to be used. In ophthalmology 15iu hyaluronidase per ml is the recommended concentration. Reconstitute 1,500 iu of hyaluronidase with 1ml of N/S or W. Follow the PHNT protocol for managing extravasation – See Section 2.8.6 Reconstitute 1,500 iu of hyaluronidase with 1ml of N/S or W. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 94 DRUG METHOD Hydralazine Slow IV bolus (C) IV infusion via an infusion pump WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Over at least 5 minutes to avoid over-rapid Reconstitute with 1ml W then dilute Groups with 10ml with N/S. 1,2,3,4 and 5 reduction in blood pressure. Groups Adults: 1,2,3,4 and 5 Initial rate of 200-300micrograms/minute Usual maintenance rate of 50-150micrograms/minute Adjust rate according to patient's blood pressure response and tolerance. Reconstitute as above then dilute 20mg with 500ml of N/S to give 40 micrograms/ml. COMMENTS Flush with N/S. If necessary, a repeat injection can be given after an interval of 20-30 minutes. Sodium content nil. Monitor heart rate and blood pressure. Incompatible with glucose solutions. However, for fluid restricted patients 60mg hydralazine may be diluted to 60ml with N/S to make a 1000microgram/ml solution, and infused via a central IV line. (This dilution is unlicensed). Pump rate (ml/hour) =Prescribed rate(micrograms/minute) x 60(minutes in an hour) Concentration of the infusion(micrograms/ml) Hydrocortisone sodium succinate IV bolus (Usual method) (C) or (I) IV infusion via an infusion pump IM injection Groups Inject doses of 100mg – 500mg over 1,2,3,4,5 and 1 - 10 minutes. Inject 50mg in 1ml dose over at least 30 seconds. Inject 25mg in 8 0.5ml over at least 15 seconds Groups 1,2,3,4 and 5 Reconstitute each 100mg with not more than 2ml W and shake before drawing up. Groups Reconstitute as for IV bolus. Refer to the Marsden Manual for guidance on IM injection. 1,2,3,4 and 5 Flush with N/S or G. Sodium content 0.5mmol/100mg. Reconstitute as above then dilute to 100-1000ml with N/S or G (maximum concentration of 1mg/1ml). The preferred method for initial emergency use is IV injection. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 95 DRUG METHOD WHO MAY GIVE Hyoscine butylbromide (Buscopan®) Slow IV bolus Groups 1,2,3,4,5 and 6 IM injection ADMINISTER INSTRUCTION FOR DILUTION AND COMMENTS OVER SUITABLE DILUENT 3-5 minutes Can be diluted with G or N/S. Flush with N/S or G. Give “slowly” as in rare cases it has caused a marked drop in blood pressure or even shock. Groups Refer to the Marsden Manual for guidance on IM injection. 1,2,3,4,5 and 6 (C) SC infusion Groups via syringe driver 1,2,3,4 and 5 in palliative care Hyoscine hydrobromide IM injection as premedication SC injection as premedication IV bolus as premedication (For acute use) SC injection for use in palliative care (C) SC infusion via syringe driver in palliative care Continuous Dilute with W when 2 or more drugs over 24 hours are being mixed in the same syringe. W or N/S may be used when the syringe only contains this drug. Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 Follow the PHNT Care of The Dying Pathways and the PHNT Syringe Driver Policy. For combinations of 2 or 3 drugs in the same syringe, refer to the Syringe Driver Drug Compatibility chart provided in the pump kit. Contact Pharmacy on ext. 39976 for further compatibility advice if necessary. Hyoscine butylbromide is not licensed via the SC route (See page 124). Refer to the Marsden Manual for guidance on IM injection. Refer to the Marsden Manual for guidance on SC injection. 3-5 minutes Refer to the Marsden Manual for guidance on SC injection. Continuous Dilute with W when 2 or more drugs over 24 hours are being mixed in the same syringe. W or N/S may be used when the syringe only contains this drug. Follow the PHNT Care of The Dying Pathways and the PHNT Syringe Driver Policy. For combinations of 2 or 3 drugs in the same syringe, refer to the Syringe Driver Drug Compatibility chart provided in the pump kit. Contact Pharmacy on ext. 39976 for further compatibility advice if necessary. Hyoscine hydrobromide is not licensed for use in palliative care (See page 124). Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 96 DRUG METHOD WHO MAY ADMINISTER OVER INSTRUCTION FOR DILUTION AND GIVE SUITABLE DILUENT Ibandronic acid For prevention of skeletal events in patients with breast cancer and bone metastases: (Ibandronate) (I) IV infusion At least 15 minutes. Add the dose to 100ml N/S or G. Groups Infusion pump 1,2 and 8 If GFR<50ml/minute is required. then infuse dose over If GFR<50ml/minute then add the 1 hour. reduced dose to 500ml N/S or G. COMMENTS Do not mix with calcium containing solutions. Extravasation can lead to tissue damage. Treatment of tumour-induced hypercalcaemia: (I) IV infusion Infusion pump is required. Groups 2 hours Add the dose to 500ml N/S (or G). Patient should be adequately rehydrated with N/S prior to treatment for tumourinduced hypercalcaemia. 1,2 and 8 Treatment of post-menopausal osteoporosis: Ibuprofen (Pedea®) IV bolus using the prefilled syringes Groups (I) IV infusion Infusion pump is required. Groups 1 15-30 seconds The contents of the prefilled syringes may be injected into an existing IV line through which N/S or G is running. 1,2, and 8 and 2 15 minutes Preferably do not dilute further. If necessary, the injection volume may be adjusted with either N/S or G. A course of therapy is defined as three intravenous injections of Pedea given at 24hour intervals. The first injection should be given after the first 6 hours of life. 1st injection:10 mg/kg, 2nd and 3rd injections: 5 mg/kg. If anuria or manifest oliguria occurs after the first or second dose, the next dose should be withheld until urine output returns to normal levels. If the ductus arteriosus does not close 48 hours after the last injection or if it re-opens, a second course of 3 doses may be given. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 97 DRUG METHOD Iloprost (Unlicensed product – see page 7) (I) IV infusion via a syringe pump. Preferred method. WHO MAY ADMINISTER INSTRUCTION FOR DILUTION GIVE OVER AND SUITABLE DILUENT Groups 6 hour infusion Dilute 50 micrograms(0.5ml) to 25ml with N/S or G. For patients 1,2,3,4 and (once each day) who require more than 50 5 micrograms during the 6 hour infusion dilute 100 micrograms(1ml) to 50ml with N/S or G. (I) IV infusion. Groups 6 hour infusion Dilute 50 micrograms(0.5ml) to Infusion via 250ml with N/S or G. For 1,2,3,4 and (once each pump day) patients who require more than 5 50 micrograms during the 6 hour infusion dilute 100 micrograms(1ml) to 500ml with N/S or G. COMMENTS Monitor for side effects: nausea, vomiting, facial flushing, headache, abdominal cramps. Also closely monitor the blood pressure and pulse rate. Days 1, 2 and 3: Start the daily infusion at 1ml/hour for 30 minutes. Continue to increase the rate by 1ml/hour every 30 minutes until the patient experiences unacceptable side effects. Then reduce the rate by 1ml/hour – this is the optimal rate. For the majority of patients the optimal rate will not exceed 5ml/hour. For patients who weigh less than 75kg, the optimal rate seldom exceeds 4ml/hour. Stop the infusion each day after 6 hours. If significant hypotension, tachycardia, bradycardia or vomiting occurs, stop the infusion until the situation returns to normal. Wait one hour and then recommence the infusion at half the previous flow-rate. Day 4 until the end of the treatment course: Start the daily infusion at the optimal hourly rate established over days 1-3. Monitor for side effects: nausea, vomiting, facial flushing, headache, abdominal cramps. Also closely monitor the blood pressure and pulse rate. Days 1, 2 and 3: Start the daily infusion at 10ml/hour for 30 minutes. Continue to increase the rate by 10ml/hour every 30 minutes until the patient experiences unacceptable side effects. Then reduce the rate by 10ml/hour – this is the optimal rate. For the majority of patients the optimal rate will not exceed 50ml/hour. For patients who weigh less than 75kg, the optimal rate seldom exceeds 40ml/hour. Stop the infusion each day after 6 hours. If significant hypotension, tachycardia, bradycardia or vomiting occurs, stop the infusion until the situation returns to normal. Wait one hour and then recommence the infusion at half the previous flow-rate. Day 4 until the end of the treatment course: Start the daily infusion at the optimal hourly rate established over days 1-3. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 98 DRUG METHOD Immunoglobulin human normal (FlebogammaDIF) 50mg/ml = 5% WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT (I) IV infusion. Groups Initially 0.6 – 1.2ml/kg/hour Provided ready diluted. Infusion 1,2,3,4 and 5 for 30 minutes. If well pump is tolerated, the rate may be required. gradually increased to a maximum of 6ml/kg/hour Supplied by Pharmacy Immunoglobulin human normal (FlebogammaDIF) 100mg/ml = 10% Supplied by Pharmacy (I) IV infusion. Groups Infusion 1,2,3,4 and 5 pump is required. Initially 0.6ml/kg/hour for Provided ready diluted. 30 minutes. If tolerated, advance to 1.2ml/kg/hour for the second 30 minutes. Again, if tolerated, advance to 2.4ml/kg/hour for the third 30 minutes. It the patient tolerates the infusion well, additional increments of 1.2ml/kg/hour may be made at 30 minute intervals up to a maximum of 4.8ml/kg/hour. COMMENTS If side effects occur reduce rate or interrupt infusion until symptoms subside then restart at lower tolerated infusion rate. Have adrenaline available in case of anaphylactoid reactions. Monitor vital signs and observe patient during infusion and for 20 minutes afterwards (for 1 hour after the first infusion, or after the first infusion after a long interval in treatment eg. Several weeks). Do not infuse with other drugs or fluids. If side effects occur reduce rate or interrupt infusion until symptoms subside then restart at lower tolerated infusion rate. Have adrenaline available in case of anaphylactoid reactions. Monitor vital signs and observe patient during infusion and for 20 minutes afterwards (for 1 hour after the first infusion, or after the first infusion after a long interval in treatment eg. Several weeks). Do not infuse with other drugs or fluids. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 99 DRUG METHOD WHO MAY GIVE ADMINISTER OVER Immunoglobulin Human Normal (Gammanorm) 16.5%=165mg/ml Subcutaneous infusion via syringe driver for home treatment. Groups Supplied by Pharmacy If Gammanorm is Initial infusion rate: 10ml/hour per syringe driver. The infusion rate may be gradually increased by 1ml/hour per syringe driver every three to four weeks. The maximum dose administered has been 40 ml/hour using two syringe drivers simultaneously. accidentally administered into a blood vessel, the patient could develop shock. IM Injection-Only in exceptional cases where subcutaneous administration is not possible 1,2,3,4 and 5 Also administered by patient or patient’s guardian. Groups INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Provided ready diluted Instruct the patient in the use of a syringe driver, infusion techniques, the keeping of a treatment diary and measures to be taken in case of severe adverse events. When large doses are given, it is advisable to administer them in divided doses at different sites. Monitor vital signs and observe patient during infusion and for 20 minutes afterwards. Sodium content: 100mg/40ml Provided ready diluted 1,2,3,4 and 5 Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 100 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Immunoglobulin human normal (Gammaplex) 50mg/ml = 5% (I) IV infusion. Infusion pump is required. Supplied by Pharmacy ▼ This product is being intensively monitored by the CHM and MHRA. Please report all suspected reactions (including non-serious ones) using a Yellow Card from the BNF WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Infuse at an initial rate Provided ready diluted. If side effects occur reduce rate or interrupt Groups infusion until symptoms subside then 1,2,3,4 and 5 of 0.6 - 1.2 ml/kg/hour for 15 minutes. If well restart at lower tolerated infusion rate. tolerated, the rate of Have adrenaline available in case of administration may be anaphylactoid reactions. increased to Monitor vital signs and observe patient 2.4ml/kg/hour for 15 during infusion and for 20 minutes minutes, then to afterwards (for 1 hour after the first 3.6ml/kg/hour for 15 infusion, or after the first infusion after a minutes, followed by a long interval in treatment eg. Several maximum of weeks). 4.8ml/kg/hour for the Do not infuse with other drugs or fluids. remainder of the infusion. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 101 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Immunoglobulin Subcutaneous The recommended Provided ready diluted Instruct the patient or carer in the use of a Groups human normal infusion via syringe 1,2,3,4 and 5 initial infusion rate syringe driver, infusion techniques, the driver for home depends on individual keeping of a treatment diary and (Hizentra) Also treatment. Suitable administered needs of the patient measures to be taken in case of severe 200mg/ml = 20% sites of and should not exceed adverse events. by patient or administration 15 ml/hour/site. If wellSupplied by Pharmacy patient’s include the tolerated, the infusion If side effects occur reduce rate or interrupt carer. abdomen, thigh, rate can then infusion until symptoms subside then ▼ This product is upper arm and gradually be increased restart at lower tolerated infusion rate. being intensively Have adrenaline available in case of to 25 ml/hour/site. monitored by the CHM lateral hip. anaphylactoid reactions. and MHRA. Please Monitor vital signs and observe patient report all suspected If Hizentra is Up to 4 infusion sites during infusion and for 20 minutes reactions (including accidentally can be used afterwards (for 1 hour after the first non-serious ones) administered into a simultaneously, infusion, or after the first infusion after a using a Yellow Card blood vessel, provided that the long interval in treatment eg. several from the BNF patients could maximum infusion rate weeks). develop shock. for all sites combined Do not infuse with other drugs or fluids. does not exceed 50 ml/hour. Injection sites Hizentra® is essentially sodium-free. should be at least 5cm apart. METHOD WHO MAY GIVE ADMINISTER OVER Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 102 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Immunoglobulin human normal (Kiovig) 10%=100mg/ml (I) IV infusion via pump. Supplied by Pharmacy WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Initially 0.5ml/kg/hour Provided ready diluted. If side effects occur reduce rate or interrupt Groups infusion until symptoms subside then 1,2,3,4 and 5 for 30 minutes. If well tolerated, the rate may restart at lower tolerated infusion rate. be gradually increased Have adrenaline available in case of to a maximum of anaphylactoid reactions. 6ml/kg/hour Monitor vital signs and observe patient during infusion and for 20 minutes afterwards (for 1 hour after the first infusion, or after the first infusion after a long interval in treatment eg. several weeks). Do not infuse with other drugs or fluids. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 103 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Immunoglobulin human normal (Octagam) 5%=50mg/ml Supplied by Pharmacy Immunoglobulin human normal (Octagam) 10%=100mg/ml Supplied by Pharmacy WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT (I) IV Initially 1ml/kg/hour for Provided ready diluted. If side effects occur reduce rate or interrupt Groups infusion via 1,2,3,4 and 5 30 minutes, If well infusion until symptoms subside then restart at pump. tolerated, the rate of lower tolerated infusion rate. administration may Have adrenaline available in case of gradually be increased anaphylactoid reactions. to a maximum of 5 Monitor vital signs and observe patient during ml/kg/hour. infusion and for 20 minutes afterwards (for 1 hour after the first infusion, or after the first infusion after a long interval in treatment eg. several weeks). Do not infuse with other drugs or fluids. (I) IV Initially 0.6ml/kg/hour Provided ready diluted. If side effects occur reduce rate or interrupt Groups infusion via 1,2,3,4 and 5 for 30 minutes. If well infusion until symptoms subside then restart at pump. tolerated, the rate of lower tolerated infusion rate. administration may Have adrenaline available in case of gradually be increased anaphylactoid reactions. to a maximum of Monitor vital signs and observe patient during 7.2ml/kg/hour. infusion and for 20 minutes afterwards (for 1 hour after the first infusion, or after the first infusion after a long interval in treatment eg. several weeks). Do not infuse with other drugs or fluids. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 104 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Immunoglobulin human normal (Privigen) 10%=100mg/ml (I) IV infusion. Infusion pump is required. Supplied by Pharmacy WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Initially 0.3ml/kg/hour. Provided ready diluted. Have adrenaline available in case of Groups anaphylactoid reactions. 1,2,3,4 and 5 If well tolerated, the rate may be gradually However, if dilution prior to Monitor vital signs and observe patient during increased to infusion is required Privagen® infusion and for 20 minutes afterwards (for 1 hour 4.8ml/kg/hour. 100mg/ml may be diluted with after the first infusion, or after the first infusion In patients with an equal volume of G to make a after a long interval in treatment eg. Several Primary 50mg/ml solution. weeks). Immunodeficiency who In all patients, IV immunoglobulin administration have tolerated requires: 4.8ml/kg/hour well, the adequate hydration prior to the initiation of the rate may be further infusion of IV immunoglobulin. increased gradually to monitoring of urine output 7.2ml/kg/hour monitoring of serum creatinine levels avoidance of concomitant use of loop diuretics. In case of adverse reaction, either the rate of administration must be reduced or the infusion stopped. Privigen® is essentially sodium-free. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 105 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Immunoglobulin Human Normal (Subcuvia) 16%=160mg/ml Subcutaneous infusion via syringe driver for home treatment, preferentially administered into the abdominal wall, thigh and/or buttocks. Groups Supplied by Pharmacy DRUG ADMINISTER OVER INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT The recommended Provided ready diluted initial rate is 10 1,2,3,4 and 5 ml/hour per syringe Also administered driver. by patient or The infusion speed can be increased by 1 patient’s ml/hour per syringe guardian. driver every subsequent infusion. The recommended maximum speed is 20 If Subcuvia is ml/hour. accidentally More than one pump administered into a can be used blood vessel, simultaneously. patients could develop anaphylactic shock or thromboembolic events. Instruct the patient in the use of a syringe driver, infusion techniques, the keeping of a treatment diary and measures to be taken in case of severe adverse events. The infusion site should be changed every 5-15ml. Monitor vital signs and observe patient during infusion and for 20 minutes afterwards (for 1 hour after the first infusion, or after the first infusion after a long interval in treatment eg. several weeks). IM Injection Groups Only in exceptional 1,2,3,4 and 5 cases where subcutaneous administration is not possible. In exceptional cases where IM administration is necessary, cumulative monthly dose should be divided up into weekly or bi-weekly applications, in order to keep the injected volume low. To further minimize the discomfort for the patient, each single dosage may need to be injected at different anatomic sites. METHOD WHO MAY GIVE ADMINISTER OVER Provided ready diluted INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 106 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 Immunoglobulin Human Normal (Subgam) 16%=160mg/ml Subcutaneous infusion via syringe driver for home treatment. Supplied by Pharmacy If Subgam is accidentally administered into a blood vessel, patients could develop shock. IM InjectionOnly in exceptional cases where subcutaneous administration is not possible. Immunoglobulin (I) IV infusion via Human Normal pump. (Vigam) Infuse via an IV 5%=50mg/ml infusion set fitted with a 15 micron Supplied by filter Pharmacy Groups 1,2,3,4 and 5 Also administered by patient or patient’s guardian. Groups Initially the infusion Provided ready diluted rate should be no more than 10ml/hour for each syringe driver. If well tolerated it can be increased at weekly intervals by 2ml/hour per syringe driver to a maximum of 20ml/hour. The administration can be performed at two or more different sites simultaneously to reduce infusion time. Provided ready diluted 1,2,3,4 and 5 Initially: Groups 1,2,3,4 and 5 0.6 – 1.2ml/kg/hour for 30 minutes. Increase gradually up to 2.4ml/kg/hour (Maximum of 180ml/hour). Provided ready diluted. Instruct the patient in the use of a syringe driver, infusion techniques, the keeping of a treatment diary and measures to be taken in case of severe adverse events. Monitor vital signs and observe patient during infusion and for 20 minutes afterwards (for 1 hour after the first infusion). In exceptional cases where IM administration is necessary, cumulative monthly dose should be divided up into weekly or bi-weekly applications, in order to keep the injected volume low. To further minimize the discomfort for the patient, each single dosage may need to be injected at different anatomic sites. If side effects occur, reduce rate or interrupt infusion. Have adrenaline available in case of anaphylactoid reactions. Monitor vital signs and observe patient during infusion and for 20 minutes afterwards (for 1 hour after the first infusion, or after the first infusion after a long interval in treatment eg. several weeks). Careful consideration needed before giving to diabetic patients (contains sucrose). Flush with G or N/S. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 107 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY ADMINISTER OVER GIVE 20 – 30 minutes 1 and 2 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Indometacin (I) IV infusion Either reconstitute the 1mg of (Indocid PDA®) powder with 1ml of N/S or W to produce a concentration of Single use vials 100micrograms in 0.1ml, or reconstitute the 1mg of powder with 2ml N/S or W to produce a concentration of 50micrograms in 0.1ml. Do not further dilute. Infliximab (I) IV infusion. Groups Infuse over 2 hours. Reconstitute each 100mg vial Infusion pump is 1,2,3,4 and with 10ml W to make a 10mg/ml (Both Remicade® required. solution. Direct the stream of W 5 and Inflectra® ) In carefully selected to the glass wall of the vial and patients who have gently swirl the solution. Avoid tolerated three 2vigorous agitation and do not hour infusions, shake as foaming is common. subsequent infusions Allow the reconstituted solution to may be given over stand for 5 minutes. First remove not less than 1 hour. from a 250ml bag of N/S a volume equal to the volume of infliximab being added then add in the required dose of infliximab. Mix gently. COMMENTS Do not reconstitute with glucose solutions. If anuria or marked oliguria (urinary output <0.6ml/kg/hour) is evident at the time of the scheduled second or third dose, further doses must not be given until laboratory studies indicate that renal function has returned to normal. If the ductus reopens, a second course of treatment may be given. Observe patients for at least 1-2 hours after the infusion for anaphylactic reactions. Equipment and medication to treat anaphylaxis must be immediately available. Use an infusion set with an in-line sterile nonpyrogenic, low protein-binding filter (pore size 1.2 micrometre or less). PIU (Planned Investigation Unit) use these filters routinely to administer infliximab and will know where to obtain them. The displacement value is insignificant. Pre-made bags from Bath ASU Doses greater than 470mg supplied pre-made by Bath ASU will be in more than 250ml total volume, and doses greater than 500mg will be diluted to 500ml. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 108 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 Insulin Section Important notes for all insulins When prescribing and administering insulin refer to the patient’s Insulin Passport to confirm the brand of insulin and type of injection device. Only use Insulin syringes to draw up insulin. Do not use intravenous syringes to draw up or measure insulin (Even for IV sliding scale infusion). Subcutaneous administration should be in the upper arms, thighs, buttocks, or abdomen. When administered subcutaneously, care should be taken when injecting to ensure that a blood vessel has not been entered (inject into a lifted skin-fold). Keep the needle under the skin for at least 6 seconds to ensure that the entire dose is injected. After injection, the site of injection should not be massaged. Patients must be educated to use the proper injection techniques. Before first use store all insulin products in the refrigerator (2 – 80C). Do not freeze. If the package insert is missing, refer to the SPC on www.medicines.org.uk for instructions on how to use the various devices. Patients’ own insulin pens containing insulin do not need to be kept in a fridge when they are in current use. DRUG METHOD WHO MAY ADMINISTER OVER INSTRUCTION FOR DILUTION COMMENTS GIVE AND SUITABLE DILUENT Insulin neutral (C) IV infusion Groups In accordance with Inspect product before use: Actrapid Follow the appropriate PHNT protocols/pre-printed (e.g. Human Infusion pump 1,2,3,4,5 and the sliding-scale and Humulin S injection should be prescriptions for the control of blood glucose: is required. instructions. clear and colourless. Actrapid, Peri-operative/Fasting/Unstable Adults 8 Adult patients with an acute MI Humulin S) Dilute with N/S to 1unit/1ml. Multidose Vial Hyperglycaemic Emergencies in diabetic adults See the guidelines for setting up Critical Care Unit insulin protocol and maintaining I.V Sliding Scale Loss of drug into bag, plastic syringe or giving set Insulin Infusion in Section 8. may occur. If an infusion bag is used ensure insulin is not injected into dead space of injection port. Compatible with IV glucose infusion/injection and N/S or G containing potassium chloride for infusion. SC Injection Inspect product before use: Actrapid Refer to the Marsden Manual for guidance on SC Groups and Humulin S injection should be injection. 1,2,3,4,5 and clear and colourless. Actrapid: Discard vial 6 weeks after first use 8 Humulin S: Discard vial 4 weeks after first use Record the date of first use on the vial. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 109 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD ADMINISTRATION Humalog® (Insulin Lispro) Humalog Mix 25 Humalog Mix 50 SC Injection Refer to the Marsden Manual for guidance on SC injection. by Groups 1,2,3,4,5 and 8 Give Humalog very close to mealtimes. Give Humalog Mix (25 or 50) shortly before meals. When necessary, Humalog Mix® (25 or 50) can be given soon after meals. Humalog should not be mixed with insulin produced by other manufacturers or with animal insulin preparations. Expiry after cartridge insertion, or after first use (vial and prefilled pen): 28 days. After cartridge insertion or first use (pre-filled pen) store below 30°C. Do not refrigerate. The pen with the inserted cartridge and the pre-filled pen should not be stored with the needle attached. Humulin I® (Isophane) Humulin M3® SC Injection Refer to the Marsden Manual for guidance on SC injection. by Groups 1,2,3,4,5 and 8 Vials containing Humulin I or the Humulin M3 formulations should be rotated several times in the palms of the hands before use to completely resuspend the insulin, until it appears uniformly cloudy or milky. Cartridges and pre-filled pens containing Humulin I and Humulin M3 formulations should be rolled in the palms of the hands ten times and inverted 180° ten times immediately before use to resuspend the insulin until it appears uniformly cloudy or milky. If not, repeat the above procedure until contents are mixed. Cartridges contain a small glass bead to assist mixing. Do not shake vigorously Expiry after insertion of the cartridge in the pen or first use of a vial: 28 days. Do not use beyond this period. When in use, the cartridges and vials should be stored below 30°C. The cartridge or pen in-use or carried as a spare may be stored for a maximum of 4 weeks not above 25°C and away from direct heat or direct light. The pen containing a cartridge in-use or the solostar pen in-use must not be stored in the refrigerator. The pen cap must be put back on the pen after each injection in order to protect from light. Before use, keep a new cartridge (in the pen) or the new solostar pen at room temperature for 1 to 2 hours. Insuman Basal® SC Injection Refer to the Marsden Manual for Insuman Comb 25® by Groups guidance on SC injection. Insuman Rapid® 1,2,3,4,5 and 8 Apidra® (Insuline glulisine) SC Injection by Groups 1,2,3,4,5 & 8 Refer to the Marsden Manual for guidance on SC injection. COMMENTS As for Insuman preparations above. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 110 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD ADMINISTRATION COMMENTS Lantus® SC Injection (Insulin Glargine) by Groups 1,2,3,4,5 and 8 If the Lantus has been in the refrigerator, it should ideally be taken out 1 to 2 hours before injection to allow it to warm up as cold insulin is more painful to inject. Levemir® (Insulin Detemir) Shelf life after first opening: A maximum of 6 weeks when stored below 30°C. NovoMix 30® Novorapid® (Insulin Aspart) Inspect the cartridge, pen or vial before use. It must only be used if the solution is clear, colourless, with no solid particles visible, and if it is of water-like consistency SC Injection Inspect the Levemir injection: it must by Groups not be used if it does not appear clear 1,2,3,4, 5 and and colourless. Refer to the Marsden Manual for 8 guidance on SC injection. After first use, Lantus may be kept for a maximum of 4 weeks at a temperature below 25°C. Record the date of first use on the vial. Each Penfill cartridge, Flexpen or Innolet must only be used for a single patient. SC Injection Refer to the Marsden Manual for by Groups guidance on SC injection. 1,2,3,4,5 and 8 Allow the NovoMix30 to warm up to room temperature (Makes mixing easier). Alternate rolling the pen 10 times horizontally in your palm with tilting to get the glass ball to roll from one end to the other several times until the suspension of insulin appears uniformly white and cloudy. When stored at room temperature (less than 300C) the expiry date of a vial, Penfill or Flexpen is 4 weeks from the date of first use. Each Penfill cartridge or Flexpen must only be used for a single patient Inspect product before use: Novorapid NovoRapid should generally be given immediately before a meal. When necessary injection should be clear and NovoRapid can be given soon after a meal. colourless. When stored at room temperature (less than 300C) the expiry date of a vial, Penfill or Refer to the Marsden Manual for Flexpen is 4 weeks form the date of first use. guidance on SC injection. Each Penfill cartridge or Flexpen must only be used for a single patient. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 111 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Intralipid® 20% WHO MAY GIVE IV bolus and Group 1 IV infusion For the treatment of cardiac arrest due to toxic intravenous concentrations of local anaesthetic ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Follow the Association of Anaesthetists of GB and Ireland guidelines. The Intralipid is located on the crash trolleys in Theatre, along with a laminated copy of the guideline. COMMENTS 1. Give IV bolus of 1.5ml/kg over 1 minute and start IV infusion at 15ml/kg/hour. 2. After 5 minutes give a maximum of two repeat IV boluses of 1.5ml/kg if: adequate circulation has not been restored or an adequate circulation deteriorates. Leave 5 minutes between boluses. A maximum of three boluses can be given (including the initial bolus). Continue CPR throughout treatment with Intralipid®. Recovery from local anaesthetic induced cardiac arrest may take more than 1 hour. Propofol is not a suitable substitute for Intralipid®. Lidocaine should not be used as an anti-arrythmic therapy. 3. Continue the infusion at the same rate, but double the rate to 30ml/kg/hour at any time after 5 minutes if: cardiovascular stability has not been restored or an adequate circulation deteriorates. 4. Continue the infusion until stable and adequate circulation restored or the maximum cumulative dose of Intralipid has been given. Ipilimumab ▼ This product is being intensively monitored by the CHM and MHRA. Please report all suspected reactions (including nonserious ones) using a Yellow Card from the BNF (I) IV infusion. Infusion pump is required. Do not exceed a maximum cumulative dose of Intralipid of 12ml/kg A closed-system device must be used to Groups 1 Infuse over 90 minutes via a 0.2-1.2 prepare ipilimumab. and 2 micron in-line filter The concentrate in the vials is a clear to slightly opalescent, colourless to pale yellow liquid that may contain light (few) particulates. Do not use if unusual amount of particles and signs of discoloration are present. Dilute the prescribed dose with N/S to a final concentration between 1mg/ml and 4mg/ml (First remove a volume of N/S from the bag equal to the volume of drug solution being added). Flush with N/S Do not co-administer other medicinal products through the same infusion line. Very common side effects include rash, pruritis, injection site reactions, pyrexia, nausea and vomiting. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 112 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Iron dextran (Cosmofer®) Preferred method: Groups 1,2,3,4 and (I) IV infusion. Infusion pump is 5 required. Each ml contains 50mg Iron(III) ▼ This product is being intensively monitored by the CHM and MHRA. Please report all suspected reactions (including nonserious ones) using a Yellow Card from the BNF Hospital Use Only:Total Dose IV Infusion. Infusion pump is required. WHO MAY GIVE Groups 1,2,3,4 and 5 IV bolus Groups (or injection into 1,2,3,4 and the venous limb 5 of the dialyser during haemodialysis) ADMINISTER OVER INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Infuse the first 25mg over 15 Dilute 100-200mg iron (2 – 4ml) Monitor patient closely in case of minutes before each subsequent in 100ml of N/S or G. anaphylaxis. infusion. If no adverse effects Resuscitation equipment should be during this time infuse the available. remaining solution at maximum Stop the infusion or injection immediately if rate of 100ml/30 minutes. any signs of hypersensitivity or intolerance Infuse the first 25mg of the For Total Dose Infusion add the occur. Observe the patient closely for signs of infusion over 15 minutes. If no required dose (determined by adverse effects during this time the dosage table or calculation hypersensitivity during Cosmofer administration and for at least 30 minutes infuse the remaining solution over in the product leaflet) to 500ml after IV administration (Especially after Total 4 – 6 hours. The rate of infusion N/S or G. Dose Infusion to monitor for delayed may be increased progressively hypersensitivity-like reactions). to 135-180ml/hour. Administer the first 25mg over 1-2 Dose of 100-200mg iron (2-4ml) Do not infuse with any other drugs or fluids. Flush with N/S. minutes before each subsequent preferably diluted in 10-20ml slow bolus. Wait 15 minutes and N/S or G. Cosmofer® may alternatively be given by monitor for adverse effects. If no deep IM injection – refer to the SPC for adverse effects give remainder of further instructions (www.medicines.org.uk) each dose at 10mg/minute Do not give Cosmofer® to patients with a (0.2ml/minute) history of asthma, allergic eczema or other atopic allergy by the IV route (For these patients IM is the preferred route for Cosmofer®). For use on the Planned Investigation Unit, follow the PIU Cosmofer® Pathway. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 113 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Iron sucrose (Venofer®) IV bolus Groups (or injection into 1,2,3,4,5 the venous limb and 8 of the dialyser during haemodialysis ) Each ml contains 20mg Iron (I) IV infusion. Infusion pump is required. WHO MAY GIVE Groups 1,2,3,4,5 and 8 ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS 1ml/minute (5ml ampoule over 5 minutes). Undiluted Do not give Venofer by IM injection. The patient should be monitored closely for signs of hypersensitivity during administration and for 30 minutes after every dose of Venofer given. If hypersensitivity reactions or signs of intolerance occur during administration, the treatment must be stopped immediately Resuscitation equipment should be available. Do not infuse with any other drugs or fluids. Extravasation may cause tissue damage. Maximum 10ml (200mg) per injection. 100mg over at least 15 minutes Dilute each 5ml ampoule to a maximum of 100ml with N/S. Two 5ml ampoules should not be diluted to more than 200ml with N/S Give slowly. Suggestion: Recommended to administer 3-5 minutes undiluted but can be further diluted with W if needed. 200mg over at least 30 minutes Isoniazid IV bolus Groups 1,2,3,4 and 5 Isophane insulin Isophane insulin should be prescribed by brand. See Insulin Section page Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 114 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Isoprenaline (C) or (I) IV Groups infusion. 1,2,3,4 and 5 Infusion pump is required. Preferably administer via a central venous catheter to avoid potential venous irritation as the preparation has a low pH ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS For severe bradycardia: Dose range 0.5 – 10 micrograms/minute Adjust rate according to response ECG monitoring required. Via a central IV line (or large peripheral vein if central access is not available) dilute 2mg or 2.25mg isoprenaline sulphate (depending on the brand of ampoule available) in 500ml G. In fluid restricted patients 2mg or 2.25mg isoprenaline sulphate (depending on the brand of ampoule available) may be diluted to 50ml with G and given via a central line. Pump rate (ml/hour) =Prescribed rate(micrograms/minute) x 60(minutes in an hour) Concentration of the infusion(micrograms/ml) Infusion using 2mg isoprenaline sulphate in 500ml G: 0.5 – 10micrograms/minute = 7.5 – 150ml/hour Infusion using 2.25mg isoprenaline sulphate in 500ml G: 0.5 – 10micrograms/minute = 6.7 – 133ml/hour If patient is fluid restricted then via a central line: Infusion using 2mg isoprenaline sulphate in 50ml G: 0.5 – 10micrograms/minute = 0.75 – 15ml/hour Infusion using 2.25mg isoprenaline sulphate in 50ml G: 0.5 – 10micrograms/minute = 0.67 – 13.3ml/hour IV bolus Group 1 Using the 100microgram in 2ml ampoule, dilute 2ml (100micrograms) to 5ml with N/S or G. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 115 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 WHO MAY ADMINISTER OVER GIVE DRUG METHOD Isosorbide dinitrate (Isoket®) (C) or (I) IV Groups 1 Usually 2-12mg/hour. Up Provided ready-diluted 25mg of to 20mg/hour if needed. isosorbide dinitrate in 50ml. infusion via and 2 pump This equates to 4 -24 ml/hour (Max 40ml/hour) of 0.05% (25mg in 50ml) solution. Intracoronary Group 1 1mg bolus given prior to balloon inflation INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Use a plastic syringe with a PVC-free or PE-lined extension set. The following extension sets are suitable and are available to order from NHS Supplies: Codan PVC-free extension set 71.4001, order code FKA064. Alaris G30302M line, order code FKA058 Vygon PE-lined extension set 6222.151, order code FSB147. BMS PE-lined extension set 30-7200, order code FSB646. Other suitable sets include the Vygon 71100.15 PE extension set and the Vygon 0832.211R PE-lined extension set. Flush with N/S or G. Monitor blood pressure and pulse during infusion. Manufacturer recommends Further doses may be given, not exceeding 5mg within a dilution to 0.5mg/ml with N/S or G. 30 minute period. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 116 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY ADMINISTER OVER GIVE INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Itraconazole (I) IV infusion. Infusion pump is required. Groups Following the package insert instructions remove the outer wrap from the 50ml bag of N/S provided. Inject 250mg itraconazole (25ml) into the bag in a slow single action (up to 60 seconds) and agitate gently.(The bag now contains 250mg in 75ml). Close the infusion set clamp then push the pin of an infusion set into the flexible port of the infusion bag. Then prime the infusion set in the usual manner. Connect the infusion set to the two-way stop cock of the extension line and open the clamp to allow all the air to be expelled from the infusion set and extension line. To avoid incompatibility problems, after infusing the itraconazole flush the extension line with 15-20ml N/S at the two-way stop cock, just before the 0.2 micron in-line filter as directed in the package insert instructions. Do not infuse any other drug solutions together with itraconazole down the same line/lumen. Protect prepared infusion from direct sunlight. Do not administer if the solution is a milky white colour that does not disappear after gentle mixing. Administer 60 ml (200mg) 1,2,3,4 and over 1 hour 5 Stop the infusion when 60ml (200mg) has been administered (About 15ml will remain in the bag and infusion set to be discarded) Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 117 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE ADMINISTER OVER Ketamine Induction & maintenance of anaesthesia IV bolus Group 1 Minimum 60 seconds Low dose as premedication prior to invasive or painful procedures IV bolus (C) IV infusion. Infusion pump is required. Groups 1 and 2 3-5 minutes Induction & maintenance of anaesthesia IM Injection Post-operative (C) SC Infusion. Use a locked infusion pump designated for ketamine. Group 1 Refer to the Marsden Manual for guidance on IM injection. 1 – 2ml/hour via antiOnly to be siphon/reflux line. prescribed by an anaesthetist or the Titrate to response. Acute Care Team. Group 2 staff can administer. Draw up 0.1ml/kg of ketamine 50mg/ml injection. Dilute this to 50ml with N/S. Add 1mg dexamethasone (0.3ml of 3.3mg/ml injection) before making the infusion upto 50ml with N/S. Refer to the subcutaneous ketamine protocol (Copy on page 199). Dexamethasone is now added to reduce tissue irritation. At this dosage (1mg in 50ml), blood glucose levels should not be adversely affected. IV bolus Groups 1,2,3,4 Not usually diluted further. Compatible with N/S, G and H. Do NOT mix in the same syringe as morphine or pethidine. Flush with N/S. Ketorolac Group 1 IM Injection Groups 1,2,3,4 and 5 Over no less than 15 seconds COMMENTS Flush IV bolus with N/S or G. 50mg/ml is the recommended maximum concentration. Can be diluted to 1mg/1ml with G or N/S or infused as 10mg/ml or 50mg/ml (undiluted product). Can be given by Group 2 staff to a ventilated patient in level 3 critical care. and 5 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT 50mg/ml is the recommended maximum concentration. Resuscitation equipment should be available. Monitor cardiac and respiratory functions. Ketamine is chemically incompatible with barbiturates and diazepam because of precipitate formation. Therefore, these should not be mixed in the same syringe or infusion fluid. Refer to the Marsden Manual for guidance on IM injection. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 118 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Kidney perfusion solution (Soltran) Kidney perfusion via kidney transplant catheter Kiovig® Labetalol Lacosamide Lantus ® WHO MAY ADMINISTER OVER GIVE INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Chill to 4oC then Do not further dilute. or Group 2 rapidly perfuse kidney with 8 litres, trained in the use of followed by slower the LifePort perfusion of 75100ml/minute system See Immunoglobulin Human Normal IV bolus Groups 1 50mg bolus over at least 1 minute. and 2 Lower doses are used during anaesthesia. (C) or (I) IV Dilute to 1mg/1ml with G or G/S. Suggested volume Groups Usual maximum infusion. 200ml. 1,2,3,4 and rate 120mg/hour Infusion pump 5 is required. For patients in critical care areas who are fluid restricted undiluted labetolol injection (5mg/ml) may be given by IV infusion via a central IV line -this method is unlicensed (See page 4) (I) IV infusion. Groups All doses over 15 Can be given undiluted. Alternatively, dilute the dose Infusion pump 1,2,3,4 and to 60 minutes with a suitable volume of N/S, G or H (eg. Dilute to is required. 50ml or 100ml). 5 Group 1 COMMENTS Not for Intravenous Infusion Follow the operating instructions for the LifePort system. IV bolus can be repeated every 5 minutes to a maximum dose of 200mg. ECG and blood pressure monitoring required. The patient should remain supine for at least 3 hours after administration. Flush with G. Neat labetalol injection has a pH of 34.5 (5% glucose has a pH of 4.2). IV and oral dosage (dose and frequency) are the same. No adjustment is needed when switching between these routes. Flush with N/S or G. Do not infuse down the same IV line as other medicinal products. See Insulin Section page Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 119 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY ADMINISTER INSTRUCTION FOR DILUTION AND SUITABLE OVER GIVE DILUENT Lenograstim (I) IV infusion. Infusion pump is required. Groups SC Injection Groups 1,2,3,4 and 5 1,2,3,4 and 5 Leucovorin calcium Levemir® Levetiracetam Flush with N/S. Using the 19G needle provided, reconstitute with the 1.05ml W provided and agitate gently to ensure complete dissolution (do not shake vigorously). Dilute with N/S or G up to 50ml/vial for Granocyte13 or up to 100ml/vial for Granocyte-34. Reconstitute as above using the 19G needle. Keep Refer to the Marsden Manual for the19G needle and the syringe attached to the vial guidance on SC injection. and withdraw the required volume of reconstituted solution from the vial. Replace the needle used for reconstitution and fit the syringe with the 26G needle provided for subcutaneous injection. See Folinic Acid See Insulin Section page (I) IV infusion. Groups Give all doses Dilute all doses with 100ml N/S or G. Infusion pump 1,2,3,4 and over 15 is required. minutes 5 Levobupivacaine Epidural Group 1 injection Local Infiltration Intrathecal injection Peripheral nerve block Peribulbar block 30 minutes COMMENTS IV and oral dosage (dose and frequency) are the same. No adjustment is needed when switching between these routes. Flush with N/S or G. Sodium content: 1.5g dose contains 25mmol sodium. The SPC states that there is no experience with administration of IV levetiracetam for longer than 4 days. Administer in accordance with standard anaesthetic All syringes containing solution for practice epidural administration should be labelled “For Epidural Use Only” (NPSA/2007/21) Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 120 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 WHO MAY ADMINISTER OVER GIVE DRUG METHOD Levofloxacin (I) IV infusion. Groups 250mg over at least 30 Infusion pump is 1,2,3,4 and minutes. 500mg over at required. least 60 minutes 5 Levomepromazine IV bolus Groups 1 3-5 minutes and 2 SC injection for use in palliative care (C) SC infusion via syringe driver in palliative care Groups 1,2,3,4 and 5 Groups Continuous over 24 hours 1,2,3,4 and 5 INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Provided ready diluted. Dilute with at least an equal volume of N/S before administration. Refer to the Marsden Manual for guidance on SC injection. Dilute with W when 2 or more drugs are being mixed in the same syringe. W or N/S may be used when the syringe only contains this drug. Flush with N/S or G. Sodium content : 15.4mmol/100ml bottle. Rarely, profound hypotension may occur during infusion. If this happens halt the infusion immediately. Levofloxacin is well absorbed from the GI tract so consider an early switch to the oral route. The bag should only be removed from the outer covering at the time of infusion as the shelf life reduces to 7 days once this outer covering is removed. Protect infusion from light. Discard injection if pink or yellow colouration occurs. Flush with N/S. Postural hypotension can occur, particularly in patients over 50; monitor blood pressure. Sodium content: 0.037mmol/1ml Follow the PHNT Care of The Dying Pathways. Follow the PHNT Care of The Dying Pathways and the PHNT Syringe Driver Policy. For combinations of 2 or 3 drugs in the same syringe, refer to the Syringe Driver Drug Compatibility chart provided in the pump kit. Contact Pharmacy on ext. 39976 for further compatibility advice if necessary. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 121 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Levosimendan IV infusion using infusion (Unlicensed pump via product – see peripheral or page 7) central IV line N.B. The duty consultant on ITU may decide not to give the loading dose INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Add the contents of one vial (12.5mg in 5ml) to 500ml G to make a 25 microgram/ml dilution. Or add the contents of one vial (12.5mg in 5ml) to 250ml G to make a 50 microgram/ml Concentration. COMMENTS *The lower loading dose of 6 microgram/kg is recommended for patients already on IV vasodilators and/or inotropes. Run a single infusion over 24 hours to produce haemodynamic effects that last 7-10 days. Avoid using levosimendan if the eGFR<30ml/min, or in patients with severe hepatic impairment. 25 microgram/ml dilution (One 12.5mg vial diluted to 500ml with 5% glucose) Patient’s weight (kg) 40 45 50 55 60 65 70 75 80 85 90 95 100 105 110 115 120 WHO MAY ADMINISTER OVER GIVE Groups 1 Loading dose of 6* to12 microgram/kg over 10 and 2 minutes followed by infusion of 0.1microgram/kg/minute over 24 hours, adjusted if necessary. Loading dose is given as an infusion over 10 minutes with the infusion rate (ml/hour) below Loading dose of Loading dose of 6 microgram/kg 12 microgram/kg 58 65 72 79 86 94 101 108 115 122 130 137 144 151 158 166 173 Continuous infusion rate (ml/hour) 0.05 microgram/kg/min 0.1 microgram/kg/min 115 4.8 130 5.4 144 6 158 6.6 173 7.2 187 7.8 202 8.4 216 9 230 9.6 245 10.2 259 10.8 274 11.4 288 12 302 12.6 317 13.2 331 13.8 346 14.4 For 50 microgram/ml dilution see table on next page 9.6 10.8 12 13.2 14.4 15.6 16.8 18 19.2 20.4 21.6 22.8 24 25.2 26.4 27.6 28.8 0.2 microgram/kg/min 19.2 21.6 24 26.4 28.8 31.2 33.6 36 38.4 40.8 43.2 45.6 48 50.4 52.8 55.2 57.6 Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 122 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Levosimendan IV infusion using infusion (Unlicensed pump via product – see peripheral or page 7) central IV line N.B. The duty consultant on ITU may decide not to give the loading dose INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Add the contents of one vial (12.5mg in 5ml) to 500ml G to make a 25 microgram/ml dilution. Or add the contents of one vial (12.5mg in 5ml) to 250ml G to make a 50 microgram/ml Concentration. COMMENTS *The lower loading dose of 6 microgram/kg is recommended for patients already on IV vasodilators and/or inotropes. Run a single infusion over 24 hours to produce haemodynamic effects that last 7-10 days. Avoid using levosimendan if the eGFR<30ml/min, or in patients with severe hepatic impairment. 50 microgram/ml dilution (One 12.5mg vial diluted to 250ml with 5% glucose) Patient’s weight (kg) 40 45 50 55 60 65 70 75 80 85 90 95 100 105 110 115 120 WHO MAY ADMINISTER OVER GIVE Groups 1 Loading dose of 6* to12 microgram/kg over 10 and 2 minutes followed by infusion of 0.1microgram/kg/minute over 24 hours, adjusted if necessary. Loading dose is given as an infusion over 10 minutes with the infusion rate (ml/hour) below Loading dose of Loading dose of 6 microgram/kg 12 microgram/kg 28.8 32.4 36 39.6 43.2 46.8 50.4 54 57.6 61.2 64.8 68.4 72 75.6 79.2 82.8 86.4 Continuous infusion rate (ml/hour) 0.05 microgram/kg/min 0.1 microgram/kg/min 57.6 2.4 64.8 2.7 72 3 79.2 3.3 86.4 3.6 93.6 3.9 100.8 4.2 108 4.5 115.2 4.8 122.4 5.1 129.6 5.4 136.8 5.7 144 6 151.2 6.3 158.4 6.6 165.6 6.9 172.8 7.2 For 25 microgram/ml dilution see table on previous page 4.8 5.4 6 6.6 7.2 7.8 8.4 9 9.6 10.2 10.8 11.4 12 12.6 13.2 13.8 14.4 0.2 microgram/kg/min 9.6 10.8 12 13.2 14.4 15.6 16.8 18 19.2 20.4 21.6 22.8 24 25.2 26.4 27.6 28.8 Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 123 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Lidocaine Slow IV bolus Groups 1 and 2 Loading Dose Groups 1 and 2 (Slow IV bolus as above) followed by (C) or (I) IV infusion. Infusion pump is required. ADMINISTER OVER 2 – 3 minutes Infusion for adults: 4mg/minute for 30 minutes then 2mg/minute for 2 hours than 1mg/minute. Anaesthesia: ♠ Infiltration ♠ Regional IV Nerve blocks ♠ Linezolid (I) IV infusion. Infusion pump is required. Group1 Group 2 in accordance with specific PGDs. Selected Group 8 Assistant Practitioners in accordance with AP protocols Groups 1 and 2 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Dilute with N/S or G. Usual concentration of 1mg/ml or 2mg/ml but concentrations up to 8mg/ml have been used in fluid restricted patients. COMMENTS ECG monitoring required. Flush with N/S. 50mg bolus dose for patients who have gross circulatory impairment or low body weight. Use reduced dosage for patients with CCF, hepatic failure and cardiac surgery. If an IV infusion is not immediately commenced, the slow bolus may be repeated once or twice at intervals of at least 10 minutes. Administer in accordance with standard anaesthetic practice 30 to 120 minutes Provided ready diluted With the new FreeFlex bag containing linezolid, the spike of the giving set should be pushed into the blue port, after twisting off the cap marked with a downward pointing arrow. The white port is not intended to be used. Flush with N/S or G. Linezolid is a reversible non-selective inhibitor of Monoamine Oxidase (MAOI) and may theoretically enhance increases in blood pressure produced by sympathomimetics (e.g. dopamine, noradrenaline, adrenaline). Theoretically it may cause serotonin syndrome with serotonin re-uptake inhibitors e.g. SSRI’s (fluoxetine etc). Sodium content 5mmol/600mg. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 124 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Liothyronine 20micrograms Slow IV bolus Groups Lorazepam IV bolus (DL)-Lysine acetyl salicylate (Aspegic®) (Unlicensed product – see page 4) MabCampath® 1,2,3,4 and 5 Groups ADMINISTER OVER 3-5 minutes INSTRUCTION FOR DILUTION AND COMMENTS SUITABLE DILUENT Reconstitute the 20microgram vial with 1 to Flush with N/S. 2ml W and shake gently until the powder has Sodium content 1.49mmol/1g. dissolved. Displacement 0.2ml/20micrograms. (For example, to give 10micrograms, reconstitute with 1ml W which expands to 1.2ml. Then withdraw 0.6ml = 10micrograms) Can be diluted 1:1 with N/S or W. Usual 1,2,3,4 and 5 maximum rate 2mg/minute except in control of status epilepticus where rapid injection is required. For IM administration the injection must be IM injection Groups (Give IV to treat 1,2,3,4 and 5 diluted 1:1 with N/S or W. Refer to the status Marsden Manual for guidance on IM injection. epilepticus) IV bolus Suggestion: 2 – Immediately before use, reconstitute the Groups contents of each 500mg vial with the 5ml of 1,2,3,4 and 5 3 minutes W provided to make a 100mg/5ml solution. (I) infusion Suggestion: 30 Reconstitute as above then dilute the dose Groups minutes (500mg or 1g) with N/S or G – suggested 1,2,3,4 and 5 volume 100ml. Deep IM Reconstitute as above. Refer to the Marsden Groups injection Manual for guidance on IM injection. 1,2,3,4 and 5 See Alemtuzumab Absorption from an IM injection is too slow for a rapid effect, and no more rapid than oral administration. Do not mix with other injectable products in the same line. Minimum interval between doses is 4 hours. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 125 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY ADMINISTER OVER GIVE Magnesium sulphate (I) IV infusion. Infusion pump is required. Groups 2g (8mmol Mg2+) magnesium sulphate= 20ml of 10%(1g in 10ml) injection or 4ml of 50%(5g in 10ml) injection. 4g (16mmol Mg2+) magnesium sulphate= 40ml of 10%(1g in 10ml) injection or 8ml of 50%(5g in 10ml) injection. 5g (20mmol Mg2+) magnesium sulphate= 50ml of 10%(1g in 10ml) injection or 10ml of 50%(5g in 10ml) injection. INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Arrythmias: 2g (8mmol 10% (1g in 10ml) magnesium 2+ sulphate injection may be given 1,2,3,4 and Mg ) over 10-15 minutes repeated once if necessary. undiluted. 5 Dilute 50% (5g in 10ml) Treatment of magnesium sulphate injection to hypomagnesaemia: a maximum concentration of 2g (8mmol Mg2+) over a 200mg/1ml with N/S or G (e.g. 2g minimum of 30 minutes or (4ml of 50% injection) diluted to 5g (20mmol Mg2+) over a at least 10ml). minimum of 1 hour For patients requiring rehydration Prevention of Re-Feeding or larger volumes of fluid, the Syndrome: magnesium replacement dose 0.2mmol/kg (0.05g/kg) over may be diluted with 500ml or 1L a minimum of 1 hour of N/S or G. Treatment of seizures and Loading dose: Draw up 4g (8ml and prevention of of 50% magnesium sulphate recurrence in Eclampsia: injection). Dilute to 20ml in a 4g loading dose over 5-15 50ml syringe with N/S. Mix well. minutes. Maintenance infusion: 1g/hour. Using 5g in 50ml dilution set pump at 10ml/hour. Maintenance infusion: Draw up 5g (10ml of 50% magnesium sulphate injection). Dilute to 50ml in a 50ml syringe with N/S. Mix well. COMMENTS Flush with N/S. Monitor blood pressure and pulse. Also monitor for signs of Mg overdose which include weakness, nausea, drowsiness & slurred speech. Continue the infusion for at least 24 hours after the seizure or delivery, whichever is later. If seizure recurs, increase the infusion rate to 1.52g/hour or give an additional IV bolus of 2g over 5 minutes (Dilute 4ml of 50% magnesium sulphate injection to 10ml with N/S). Monitor the patellar reflex and oxygen saturation levels hourly during administration of magnesium sulphate (including overnight) to exclude signs of toxicity. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 126 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY ADMINISTER OVER GIVE Magnesium sulphate (Continued from previous page) IM Injection, only if IV access is not possible or impractical Groups 1,2,3,4 and 5 SC infusion, Groups only if no other 1,2,3,4 and route is 5 possible or practical Mannitol (I) IV infusion. Infusion pump is required. Groups Reduction of intracranial 1,2,3,4 and pressure: 0.25g -0.5g/kg over 30-60 5 minutes. Can be repeated as necessary. Urgent reduction of intra-ocular pressure before eye surgery: Up to 500ml of 20% mannitol given by slow IV infusion until the intra-ocular pressure has been satisfactorily reduced. INSTRUCTION FOR DILUTION AND SUITABLE DILUENT For adults, administer the dose using 50% (1g in 2ml) injection undiluted, or dilute to 25% (1g in 4ml) with N/S. For children a maximum recommended concentration for IM injection is 20% (200mg/ml) eg. For a 500mg dose, dilute 1ml of 50% magnesium sulphate injection to 2.5ml with N/S. Keep the concentration as low as possible, preferably not greatly exceeding the isotonic concentration of 6.3% w/v in Water For Injections (6.3g =25.2mmol in 100ml Water For Injections). Discuss and check dose/concentration/route with a Pharmacist. 500ml of ready-to-use 10% (50g in 500ml) mannitol is routinely stocked. (If using 20% mannitol, infuse through an administration set incorporating a filter*). COMMENTS IM injection of magnesium sulphate is painful. Refer to the Marsden Manual for guidance on IM injection. There is little published data to support administration of magnesium sulphate by the S/C route. There are isolated case reports of between 2 and 4mmol magnesium sulphate added to 500ml - 1 litre of N/S being tolerated by S/C infusion. Administration via the S/C route is not licensed in the UK (See page 124). Flush with N/S Infusion may crystallise at low temperatures; redissolve by warming. Extravasation causes inflammation and thrombophlebitis. 20% mannitol should preferably be administered via a central IV line or at least through a large peripheral vein due to its high osmolarity. *Suitable filters to administer mannitol are PALL 0.22 micron, Braun Sterifix 0.2 micron, Technopharm codan 0.2 micron filters. These filters should be ordered via ORACLE. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 127 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Meropenem IV bolus for doses of 1g or less Mesna WHO MAY ADMINISTER OVER GIVE Groups 5 minutes 1,2,3,4 and 5 (I) IV infusion. Infusion via pump (I) IV infusion when ifosfamide or cyclophosphamide are given as an (I) infusion over 1-2 hours or as IV bolus, or cyclophosphamide has been given orally Groups (C) IV infusion Groups 15-30 minutes 1,2,3,4, 5 Groups 15-30 minutes 1,2,3,4 and 5 Typically, for the duration of 1,2,3,4 and a (C) infusion of ifosfamide, and then for a further 12 5 hours afterwards. INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Reconstitute each 250mg meropenem with 5ml W. This provides an approximate concentration of 50mg/ml. Reconstitute and dilute to 50200ml using N/S or G. Dilute the required dose of mesna (Usually 20% of the dose of cyclophosphamide or ifosfamide) to 50ml or 100ml with N/S. Dilute with N/S or G to any convenient volume COMMENTS Flush with N/S or G. Sodium content: 4mmol/gram. The preferred method for administering doses greater than 1g is intermittent IV infusion. When protection against urothelial toxicity is required, three doses of mesna are typically given with each dose of cyclophospamide or ifosfamide. The first dose of mesna is usually IV and given just prior to the injection/infusion of cyclophosphamide or ifosfamide. Intravenous second and third doses are given at 4 hours and 8 hours (after the injection or after the end of an infusion). Alternatively, the second and third doses of mesna can be given orally, in which case each oral dose is 40% of the dose of cyclophosphamide or ifosfamide given, given at 2 hours and 6 hours (after the injection or after the end of an infusion), using mesna injection by the oral route. On occasions Pharmacy Technical Services add the required dose of Mesna into the bag containing ifosfamide. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 128 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Metaraminol IV bolus Groups 1 Emergency use and 2 only. IV bolus Groups 1,2 and (Group 8 Assistant Practitioners working in Cardiac Catheter Labs) (C) IV infusion. Infusion pump is required. WHO MAY GIVE Groups 1 ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Undiluted. 0.5 – 1ml over a few Dilute 10mg in 1ml with 19ml of seconds via a large N/S to make 10mg in 20ml. peripheral vein or a central vein. COMMENTS Bolus dose: 0.5 – 5mg (0.05 – 0.5ml) Flush with N/S or G. Sodium content : 0.087mmol/ml. Follow each bolus dose with a 20ml flush of N/S. The bolus dose of 0.5 – 1ml of the prepared dilution may be repeated every 1 – 5 minutes as indicated by the mean arterial pressure (MAP) and patient response. Dilute 15-100mg in 500ml N/S or Metaraminol injection from Torbay G. Manufacturing Unit is unlicensed (See page and 2 The volume may be varied 7). depending on the rate of administration and the patient's fluid needs. Methotrexate When methotrexate is prescribed to treat conditions including multiple sclerosis, glomerular kidney disease, severe psoriasis or rheumatoid arthritis, it may be administered by Group 1 or 2 practitioners who have previous experience of administering parenteral cytotoxics. Read For use in Appendix 3 for guidance on the handling of cytotoxic drugs. Explicitly inform the patient of the once a week dosing schedule for ongoing therapy haematology and and determine a fixed weekday as the day of injection. This should be stated on the prescription. oncology refer to IV bolus injection Group 1 or 2 Consider folic acid supplementation. chemotherapy (Not for children or Refer to the SPC for Metoject® on protocols adolescents) www.medicines.org.uk for details of the SC bolus injection Group 1 or 2 Refer to the Marsden Manual for recommended monitoring to detect signs of toxicity (Mouth and throat examinations, full guidance on SC injection. IM injection Group 1 or 2 Refer to the Marsden Manual for blood counts, liver function tests, renal function etc). Refer to specific protocols as guidance on IM injection. appropriate: IM methotrexate for ectopic pregnancy (EPU and Monkswell). Adjust rate according to response. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 129 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Methylthioninium chloride Proveblue (Methylene Blue) Important: (I) IV infusion. Infusion pump is required. . (C) IV infusion. To treat hypotension Infusion pump is refractory to fluids required. and vasopressors in septic shock Methyl-prednisolone IV bolus (doses sodium succinate up to 250mg) (Solu-Medrone) ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Only Proveblue brand ampoules are suitable for intravenous use 15 – 60 minutes Dilute to a suggested Groups concentration of 1mg/ml with G. 1 and 2 Groups 1 and 2 Groups 1,2,3,4 and 5 (I) IV infusion Groups (doses over 1,2,3,4 and 5 250mg) via pump IM injection Groups 1,2,3,4 and 5 Methyl-prednisolone IM injection acetate Intra-articular (Depo-Medrone) Peri-articular Intrabursal Intralesional Into tendon sheaths WHO MAY GIVE Groups 1,2,3,4 and 5 Group 1 Dose to treat hypotension in septic shock refractory to fluids and vasopressors is 1-2mg/kg over 15-60 minutes. May be repeated as required, alternatively after 2 hours set up a continuous infusion. 0.25-2 mg/kg/hour Dilute to a suggested Do not infuse down the same lumen/line as any concentration of 1mg/ml with G. other drugs. Do not dilute with N/S. Extravasation can cause tissue damage. The use of methylene blue to treat hypotension in septic shock is unlicensed (See page 7) Give slowly minimum Reconstitute with diluent provided. Flush with N/S, G or G/S. 5 minutes. Sodium content: 2mmol/g. Minimum 30 minutes Reconstitute as above then dilute For Acute Spinal Cord Injury refer to protocol with G, N/S or G/S to any suitable on Pencarrow. volume (e.g. 50-250ml). Reconstitute with diluent provided. Refer to the Marsden Manual for guidance on IM injection. Inject deeply into the gluteal Refer to the Marsden Manual for guidance on muscle. IM injection. Prior to intra-articular injection the joint fluid should be examined to exclude a septic process. Administer under strictly aseptic conditions. Do not give via the intrathecal route (potentially neurotoxic) or the IV route. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 130 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Metoclopramide 10mg in 2ml Slow IV bolus Groups At least 3 minutes Give undiluted. Flush with N/S or G. Sodium content 10mg/2ml = 0.26mmol. IM injection SC injection for use in palliative care (C) SC infusion for us in palliative care Metoprolol IV bolus 1,2,3,4,5 and 8 Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 Metronidazole (I)IV infusion via Groups an infusion pump 1,2,3,4 and 5 Refer to the Marsden Manual for guidance on IM injection. Refer to the Marsden Manual for guidance on SC injection. Continuous over 24 hours Dilute with W when 2 or more drugs are being mixed in the same syringe. W or N/S may be used when the syringe only contains this drug. Cardiac arrhythmias: Give undiluted 1-2 mg/minute During anaesthesia: 2-4mg injected “slowly” Further injections of 2mg up to a maximum overall dose of 10mg may be given Adults: Provided ready diluted. 100ml over 20 minutes = 100 drops/minute via a standard blue gravity set Follow the PHNT Care of The Dying Pathways. Follow the PHNT Care of The Dying Pathways and the PHNT Syringe Driver Policy. For combinations of 2 or 3 drugs in the same syringe refer to the compatibility charts in the pump kit or contact Pharmacy on ext. 39976 for advice. If an infusion containing metoclopramide becomes discoloured it should be discarded. Early intervention post MI: 5mg every 2 minutes up to a maximum of 15mg total as determined by blood pressure and heart rate. Monitor blood pressure, heart rate and ECG. Flush with N/S or G. Flush with N/S, G or G/S. Cefuroxime can be mixed into an infusion of metronidazole. Sodium content: 13.5mmol/500mg infusion. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 131 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG WHO MAY ADMINISTER OVER GIVE Midazolam IV bolus for sedation Groups Administer over at least 30 seconds an in conscious adult 1,2,3,4 and initial dose of midazolam guided by: (Monograph patients Age 5 continues on Weight the next Other medications page) Medical history and co-existing disease Planned procedure Assess the level of sedation after 2-5 minutes and repeat as necessary (minimum of 2 minutes between subsequent doses). During the procedure, additional doses may be given. IV bolus for induction Groups Induction of anaesthesia and loading of anaesthesia 1,2,3,4 and dose for ICU sedation for adults: Each increment over 20-30 seconds allowing 5 2 minutes between successive increments. (I) or (C) IV infusion Groups 1 following initial and 2 loading dose via infusion pump METHOD INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Use 1mg/ml midazolam Use 1mg/ml midazolam COMMENTS For sedation in conscious adult patients follow the Sedation Policy on Plymouth Healthnet (under Clinical Guidelines). All healthcare practitioners involved directly or participating in sedation techniques must have the necessary knowledge, skills and competences required Flush with N/S. Respiratory depression and arrest have occurred when doses were given too rapidly. Flumazenil and resuscitation equipment must be immediately available. Dilute with N/S, G or G/S. For adults the usual dilution is 50mg in 50ml. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 132 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Midazolam (Continued) Slow IV bolus for Carotid Artery Rupture SC injection for terminal restlessness and agitation (C) SC infusion via syringe driver for terminal restlessness and agitation WHO MAY ADMINISTER OVER GIVE Groups 1 2.5 – 5mg over 1-2 minutes repeated at 2 minute intervals if sedation is not and 2 adequate. Groups 1,2,3,4 and 5 Groups Continuous over 24 hours 1,2,3,4 and 5 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Use the 5mg in 5ml pre-filled syringe prepared by Pharmacy and kept in the patient’s bedside locker. If a pre-filled syringe is not available use a 5mg in 5ml ampoule. Use the 10mg in 2ml ampoules. Refer to the Marsden Manual for guidance on SC injection. Use the 10mg in 2ml ampoules. Dilute with W when 2 or more drugs are being mixed in the same syringe. W or N/S may be used when the syringe only contains this drug. COMMENTS For the Management of Carotid Artery Rupture (Carotid Blow Out) follow the specific additional guideline on Lynher ward. Follow the PHNT Care of The Dying Pathways and the PHNT Syringe Driver Policy. For combinations of 2 or 3 drugs in the same syringe, refer to the Syringe Driver Drug Compatibility chart provided in the pump kit. Contact Pharmacy on ext. 39976 for further compatibility advice if necessary. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 133 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Milrinone (I) or (C) IV infusion. Infusion pump is required. Groups 1 and 2 Milrinone 10mg in 50ml G dilution eGFR >50ml/minute Maintenance infusion rate: Infusion pump rate Titrate from 0.375 to 0.750 ml/kg/hour micrograms/kg/minute 0.375 0.11 0.400 0.12 0.500 0.15 0.600 0.18 0.700 0.21 0.750 0.22 ADMINISTER OVER INSTRUCTION FOR COMMENTS DILUTION AND SUITABLE DILUENT Loading dose (50microgram/Kg) Dilute to 200 microgram/ml Monitor blood pressure, heart rate, ECG, over 10 minutes followed by with N/S or G (e.g. 10mg fluid balance and renal function. infusion at 0.375-0.75 ampoule diluted to 50ml). Do not mix with other drugs. microgram/kg/minute according Flush with N/S or G. to haemodynamic response (For However solutions of different Using a 200microgram/ml dilution the help setting the infusion pump concentrations may be used recommended maintenance infusion rate rate see table below). according to the patient’s fluid is 0.11-0.22ml/kg/hour. requirements. For patients with renal impairment (eGFR < 50ml/minute) using Milrinone 10mg in 50ml G dilution eGFR ml/minute/1.73m2 5 10 20 30 40 50 Initial maintenance infusion rate micrograms/kg/minute (titrate according to haemodynamic response). 0.20 0.23 0.28 0.33 0.38 0.43 Initial Infusion pump rate ml/kg/hour (titrate according to haemodynamic response). 0.06 0.07 0.08 0.10 0.11 0.13 Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 134 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Morphine WHO MAY ADMINISTER OVER INSTRUCTION FOR DILUTION COMMENTS GIVE AND SUITABLE DILUENT Staff prescribing, administering and/or screening prescriptions for opioid medications should be familiar with the PHNT Policy for Reducing Errors with Opioid Medicines in Adults using the following link: http://staffnet.plymouth.nhs.uk/Portals/1/Documents/Trust%20Documents/Medicines%20Management/Policy%20for%20Reducing%20Dosing%20 Errors%20with%20Opioid%20Medicines%20in%20Adults.pdf?timestamp=1443106367868 SC injection Follow the SC Morphine Do not dilute Flush each SC dose with 0.5ml N/S Groups Preferred route Flush with N/S, G or G/S. 1,2,3,4 and 5 Protocol for Adults (Copy on for treating acute page 196) Sodium content negligible. pain on general wards IV bolus Follow the algorithm from Dilute 10mg morphine to 10ml Groups 1 (Theatre Recovery) and 2 Recovery 2 with N/S IV bolus Groups 1 (Acute Care Areas) and 2 IV bolus (Emergency Department) Groups 1 (C) or (I) IV infusion in Critical Care areas via infusion pump. Patient Controlled Analgesia (PCA) Groups 1 IM injection Groups and 2 and 2 Groups 1,2,3,4 and 5 1,2,3,4 and 5 Follow the IV Morphine Dilute 10mg morphine to 10ml Protocol for Adults in Acute with N/S Areas (Copy on page 197) Follow the IV Morphine Protocol for Adults in the Emergency Department (Copy on page 198) Vials of ready-diluted morphine 50mg in 50ml N/S are available from Pharmacy). See comments Vials of ready-diluted morphine 50mg in 50ml N/S are available from Pharmacy. Refer to the Marsden Manual for guidance on IM injection. For monitoring required when IV morphine is given in the Emergency Department, see the protocol on page 198. Monitor blood pressure, heart rate, respiratory rate. Have naloxone and resuscitation equipment available. Adult PCA: Usual bolus dose 1mg. Usual lock-out period is 5 minutes. Refer to Acute Pain/Care Service Protocols. Background morphine infusion may only be prescribed by a member of the Acute Pain/Care Team. Nurse-led Controlled Analgesia via the PCA pump is available – seek advice from the Acute Pain/care Team. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 135 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Morphine 40mg in 1ml preservative-free (Unlicensed) Mycophenolate (C) Intrathecal Group 1 or infusion or Group 2* Intrathecal bolus (I) IV infusion WHO MAY GIVE Groups 1,2,3,4 and 5 Mycozyme® ADMINISTER OVER INSTRUCTION FOR DILUTION AND COMMENTS SUITABLE DILUENT Prepare and administer in accordance with * Restricted to those persons who are trained and competent to administer the Pain Management Centre protocols. medication via the intrathecal route. 2 hours. Infusion to be prepared by Pharmacy. Wear gloves, gown and safety glasses Telephone Ext. 31083. Doctor to prescribe when handling. Avoid handling drug if dose in 100ml G. pregnant or trying to become pregnant. See Alglucosidase alfa Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 136 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Naloxone IV bolus for: Reversal of opiate induced respiratory depression in adults prescribed opiates as part of their palliative, chronic pain or peri-operative or peri-procedure care IV bolus followed by (C) infusion to treat PCA or epidural opiate-induced pruritis IV boluses to treat Acute opiate overdose/poisoning IV infusion to treat Acute opiate overdose/poisoning IM Injection only if IV administration is not possible WHO MAY ADMINISTER OVER GIVE Groups Adults: Bolus dose of 100 micrograms may be repeated at intervals of not less than 2 minutes 1,2,3,4,5 to achieve desired response. and 8 Groups 40microgram IV bolus (=0.1ml of 400mcg/ml 1,2,3,4 and injection) followed by 200micrograms infused over 6 – 8 hours. 5 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Dilute to a concentration of 100micrograms/ml with N/S. If repeated bolus doses are insufficient a continuous infusion may be required using an infusion pump – Dilute 2mg naloxone with 500ml N/S or G (Resulting concentration 4micrograms/ml). Starting rate is 60% of the initial IV bolus infused over 1 hour then titrate to response. For the infusion, dilute 200micrograms in 1 litre N/S infused over 6 – 8 hours. Groups 1 Initially 400 micrograms, then 800 micrograms for up to 2 doses at 1 minute intervals. If no response to preceding dose, then increase to 2 mg for 1 dose if still no response, then review diagnosis; further doses may be required if respiratory function deteriorates, 4 mg dose may be required in seriously poisoned patients Groups 1 Adjust rate according to response (initially, rate may be set at 60% of the initial and 2 resuscitative intravenous injection dose per hour). The initial resuscitative intravenous injection dose is that which maintained satisfactory ventilation for at least 15 minutes Groups Refer to the Marsden Manual for guidance on 1,2,3,4 and IM injection. 5 and 2 Dilute 10mg in 50ml N/S or G. COMMENTS Use infusions within 12 hours. Monitor for possible hypotension, hypertension, ventricular tachycardia and fibrillation and withdrawal syndrome. Flush with N/S or G. Note that 4mg in 20ml is an unlicensed dilution (see page 7). When using a continuous infusion to treat opiate induced respiratory depression in adults prescribed opiates as part of their palliative, chronic pain or peri-operative care do not suddenly stop the infusion. Once the patient is stabilised and it is deemed appropriate, the naloxone infusion should be titrated down rather than just turned off. Close monitoring is essential at this stage for the possibility of opioid toxicity recurring again especially when it is due to long acting opioids. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 137 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Natalizumab (Tysabri®) ▼ This product is being intensively monitored by the CHM and MHRA. Please report all suspected reactions (including non-serious ones) using a Yellow Card from the BNF Neostigmine WHO MAY GIVE (I) IV infusion. Groups Infusion pump is required. IV bolus Approximately 1 1,2,3,4 and 5 hour Groups 1 and 2 ADMINISTER OVER (I) or (C) IV infusion to treat severe constipation in Critical Care Groups SC Injection Groups IM injection 1 and 2 Groups 1 and 2 1 and 2 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Check that the solution is clear and free of particles. Draw up 15 ml from the vial and add to 100ml N/S. Gently invert the bag to mix completely. Do not shake. Visually inspect the diluted product for particles or discolouration prior to administration. Flush the line with N/S when the infusion has finished. Do not mix with any other drugs or diluents. Give undiluted. Observe the patient during the infusion and for 1 hour after the completion of the infusion for signs and symptoms of hypersensitivity reactions. Do not administer as a bolus injection. Equipment and medication to treat anaphylaxis must be immediately available. Discontinue administration of natalizumab and initiate appropriate therapy at the first symptoms or signs of hypersensitivity. Minimum 3-5 Flush with N/S. Protect from light. minutes. Have atropine or glycopyrollate available to However, for counteract possible cholinergic reactions. reversal of For use in Critical Care for acute colonic neuromuscular pseudo-obstruction, follow the Critical Care block, administer Bowel Management Protocol (Use for this over 1 minute. indication is unlicensed -see page 7). Start at 0.4mg/hour Dilute 5mg neostigmine to 50ml with N/S to Use atropine or glycopyrronium if necessary (4ml/hour). If no make a concentration of 0.1mg/ml. to treat bradycardia, and for patients with response after 8 spinal cord lesions. hours increase to Follow the Critical Care Bowel Management 0.8mg/hour Protocol (Use for this indication is unlicensed (8ml/hour) - see page 7). The only confirmed Y-Site compatibilities are with heparin, hydrocortisone and potassium chloride. When treating Myaesthenia Gravis, Refer to the 500micrograms of neostigmine metilsulfate Marsden Manual by intravenous injection is equivalent in for guidance on IM effect to about 1 to 1.5mg of neostigmine or SC injection. metilsulfate by intramuscular or subcutaneous injection, and to about 60mg of oral pyridostigmine Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 138 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Nimodipine (I) IV infusion via a central IV line. Infusion pump is required. Niopam® In accordance with Radiology Dept. protocols WHO MAY ADMINISTER INSTRUCTION FOR DILUTION GIVE OVER AND SUITABLE DILUENT Groups 500microgram Provided ready diluted (10mg in s-2mg/ hour 50ml). 1 and 2 =2.5 – 10ml/hour Groups 1 and 6 Injection via the Group 8 balloon catheter for (Cardiac angioplasty or Catheter valvuloplasty Labs.) Nitroprusside See Sodium Nitroprusside Nivolumab (C) IV infusion. Groups ▼ This product is Infusion pump is 1 and 2 being intensively required. monitored by the CHM and MHRA. Please report all suspected reactions (including nonserious ones) using a Yellow Card from the BNF In accordance Not for further dilution with Radiology Dept. protocols COMMENTS Draw up solution into 50ml syringe and use the polyethylene line provided in the box. Administer via a central catheter through a Y-piece connector into an infusion of N/S, G, H, Dextran 40, human albumin 5% or mannitol 10% running at 40ml/hour. Protect infusion from direct sunlight. Flush with N/S or G. Incompatible with PVC Although the product is labelled for “Single use”, each bottle of Niopam can be used with the Bracco CT Expres pump injector system in a multi-dose technique for one or more patients, in accordance with local Radiology Dept. protocols. Niopam can be followed with a flush of N/S in accordance with Radiology Dept. protocols. In accordance with Cardiac Catheter Labs. and Assistant Practitioner protocols. Infuse over 60 A closed-system device must be used minutes via a to prepare nivolumab. 0.2-1.2 micron in-line filter Either give the prescribed dose undiluted (10mg/ml), or dilute the dose in N/S so that the final concentration is at least 1mg/ml. The final concentration should therefore be within the range 1-10mg/ml. (First remove a volume of N/S from the bag equal to the volume of drug solution being added). Flush with N/S. Do not co-administer other medicinal products through the same infusion line. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 139 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Noradrenaline (Norepinephrine) base 1mg/1ml (=Noradrenaline tartrate 2mg/ml) Novomix 30® Insulin Novorapid® Insulin Octagam® Octreotide WHO MAY ADMINISTER GIVE OVER (C) or (I) IV Groups Adjust rate infusion via a 1 and 2 according to central IV line. response. Infusion pump is required. Pump rate (ml/hour) =Prescribed rate(micrograms/kg/minute) x 60(minutes in an hour) x Patient’s weight (kg) Concentration of the infusion(micrograms/ml) See Insulin Section, page 107 See Immunoglobulin Human Normal SC injection Groups 1 and 2 IV bolus Groups 3-5 minutes 1 and 2 (C) SC infusion via syringe driver in palliative care. (Unlicensed – see page 7) INSTRUCTION FOR DILUTION AND SUITABLE DILUENT “Single Strength” Infuse via a central venous catheter. Loss 4ml (4mg noradrenaline base) diluted to of potency occurs if diluent is N/S. Discard 50ml with G (or G/S) = 80micrograms/ml. infusion if brown colour develops. “Double strength” Flush with G or N/S. 8ml (8mg noradrenaline base) diluted to Protect infusion from direct sunlight. 50ml with G (or G/S) = 160micrograms/ml. Haemodynamic monitoring required. “Quadruple Strength” 16ml (16mg noradrenaline base) diluted to 50ml with G (or G/S)= 320micrograms/ml. Rate (micrograms/kg/minute) = Pump rate (ml/hour) x concentration (micrograms/ml) Patient’s weight (kg) x 60 Refer to the Marsden Manual for guidance on SC injection. Dilute each 1ml octreotide injection with a minimum of 1ml and a maximum of 9ml of N/S. Subcutaneous injection is preferred method of administration. ECG monitoring necessary with IV injection (Not with SC injection). Flush after IV injection with N/S. It is not recommended to use G to dilute octreotide (except for treatment of variceal bleeding below). The rubber caps of the Multidose vials should not be punctured more than 10 times. Groups Continuous over Dilute with W when 2 or more drugs Follow the PHNT Care of The Dying Pathways and 24 hours are being mixed in the same syringe. the PHNT Syringe Driver Policy. 1 and 2 W or N/S may be used when the For combinations of 2 or 3 drugs in the same syringe only contains this drug. syringe refer to the compatibility charts in the pump kit or contact Pharmacy on ext. 39976 for advice. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 140 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG WHO MAY ADMINISTER INSTRUCTION FOR DILUTION COMMENTS GIVE OVER AND SUITABLE DILUENT Octreotide Instructions for IM injection of Sandostatin LAR for deep intragluteal injection only Depot 1. Remove the cap from vial containing Sandostatin LAR. Ensure that the powder is settled at the bottom of the vial by lightly tapping the vial. IM injection Remove the cap from the vehicle syringe. Attach one of the supplied needles to the vehicle syringe. 2. Insert needle through centre of rubber stopper of the Sandostatin LAR vial. by Groups 3. Without disturbing the Sandostatin LAR powder, gently inject the vehicle into the vial by running the vehicle down the inside wall of the vial. 1 and 2 Do not inject the vehicle directly into the powder. Withdraw any excess air present in the vial. 4. Do not disturb the vial until the vehicle has wetted the Sandostatin LAR powder for suspension. Once complete wetting (approximately 2-5 minutes) has occurred, the vial should be moderately swirled until a uniform suspension is achieved. Do not vigorously shake the vial. 5. Immediately draw 2ml of air into the syringe and re-insert the needle through the rubber stopper. Inject the 2ml of air into the vial and then, with the bevel down and the vial tipped at approximately 45 degree angle, slowly draw the entire contents of the vial containing the suspension into the syringe. Immediately change the needle (supplied). 6. Gently invert the syringe as needed to maintain a uniform suspension. Eliminate air from syringe and disinfect the injection site. Insert needle into right or left gluteus and draw back to ensure that no blood vessel has been penetrated. Immediately inject IM by deep intragluteal injection. 7. Sandostatin LAR must be given only by intragluteal injection, never IV If a blood vessel has been penetrated, select another injection site. Olanzapine IM injection Reconstitute the vial contents Use the solution immediately within 1 hour of reconstitution. Groups 1 10mg with 2.1ml W. Rotate the vial until Administration of olanzapine 10mg injection via the SC and and 2 injection the contents have completely IV routes is unlicensed. The safety via these routes has not dissolved making a 5mg/ml been fully established. However, in one published study, IV solution (The vial actually boluses of 5mg olanzapine were tolerated by patients. Due contains 11mg drug with 0.1ml to possible bradycardia and hypotension, use with caution in displacement). patients with serious cardiovascular disease. 10mg dose – draw up 2ml 5mg dose – draw up 1ml 2.5mg dose – draw up 0.5ml METHOD Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 141 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY ADMINISTER GIVE OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Ofatumumab (I) IV infusion Groups 1 See tables below and 2 via infusion pump. Dilute all doses to 1000ml with N/S (remove a volume of N/S from the bag first equal to the volume of drug solution being added). Do not shake. Mix by gentle inversion. Rates of infusion for Ofatumumab First Infusion Previously untreated CLL Start at 12ml/hour. Increase rate every 30 minutes to a maximum of 400ml/hour Second Infusion Subsequent Infusions If no adverse reactions to the first infusion, start the second and subsequent infusions at 25ml/hour. Increase rate every 30 minutes to a maximum of 400ml/hour. COMMENTS A closed-system device must be used to prepare Ofatumumab. Patients should always be pre-medicated 30 minutes to 2 hours prior to Ofatumumab infusions with paracetamol, antihistamine & intravenous corticosteroid. Patients should be closely monitored during administration of ofatumumab for the onset of infusion reactions (ADRs), including cytokine release syndrome, particularly during the first infusion. •In case of a mild or moderate ADR, the infusion should be interrupted and restarted at half of the infusion rate at the time of interruption, when the patient's condition is stable. If the infusion rate had Start first and second infusions at If no adverse reactions to the first and second not been increased from the starting rate of 12 Refractory 12ml/hour. Increase rate every 30 infusions, start subsequent infusions at ml/hour prior to interrupting due to an ADR, the CLL minutes to a maximum of 200ml/hour. 25ml/hour. Increase the rate every 30 minutes infusion should be restarted at 12 ml/hour, the to a maximum of 400ml/hour. standard starting infusion rate. The infusion rate can Titration of infusion rates continue to be increased according to standard Previously untreated CLL Refractory CLL procedures, according to physician discretion and Infusion 1 over 4.5 Infusions 2 to 13 Infusions 1 and 2 Infusions 3 to 12 over patient tolerance (not to exceed increasing the rate every 30 minutes). hours Over 4 hours over 6.5 hours 4 hours Time (minutes) Rate (ml/hour) Time (minutes) Rate (ml/hour) Time (minutes) Rate (ml/hour) Time (minutes) Rate (ml/hour) 0-30 12 0-30 25 0-30 12 0-30 25 31-60 25 31-60 50 31-60 25 31-60 50 61-90 50 61-90 100 61-90 50 61-90 100 91-120 100 91-120 200 91-120 100 91-120 200 121-150 200 121+ 400 121+ 200 121+ 400 151-180 300 180+ 400 •In case of a severe ADR, the infusion should be interrupted and restarted at 12 ml/hour, when the patient's condition is stable. The infusion rate can continue to be increased according to standard procedures, according to physician discretion and patient tolerance (not to exceed increasing the rate every 30 minutes). Flush line with N/S before and after ofatumumab infusion. Do not co-administer other medicinal products through the same infusion line. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 142 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Omalizumab SC injection in Groups 1 the deltoid region and 2 of the arm. Omeprazole (I) IV infusion. Infusion pump is required. Omeprazole IV Loading dose For the specialist of 80mg treatment of endoscopically controlled bleeding peptic ulceration (C) IV infusion. Infusion pump is required. Omnipaque® In accordance with Radiology Dept. protocols Injection via the balloon catheter for angioplasty or valvuloplasty WHO MAY ADMINISTER GIVE OVER Group 20-30 minutes 1,2 and 3 Groups 80mg in 100ml N/S 1,2,3,4 and over 30 minutes 5 Groups After loading dose, 1,2,3,4 and infuse at 8mg/hour for 70 hours* 5 (This is 10ml//hour with each 80mg in 100ml N/S) Group 1 In accordance with or Group 6 Radiology Dept. protocols Group 8 (Cardiac Catheter Labs.) INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Available in pre-filled syringes. Alternatively, the injections can be administered in the thigh if there is any reason precluding administration in the deltoid region. Reconstitute each 40mg with approximately 5ml N/S or G. Dilute each 40mg to 100ml with N/S or G. For each 40mg vial, withdraw 5ml of N/S from a 100ml bag and use to reconstitute the vial. Then inject the reconstituted omeprazole into the bag. Do not add more than 80mg omeprazole to 100ml of diluent. Reconstitute and dilute each 40mg vial as above. Flush with N/S. Sodium content 0.1mmol/40mg vial. Use infusion in N/S within 12 hours, 3 hours if in G. Incompatible: do not infuse with any other drugs. Use infusion in N/S within 12 hours. Omeprazole infusion must not be infused through the same venflon or line lumen as any other drug solution. Each bag is for single use only and must be used immediately after preparation. Not for further dilution Although the product is labelled for “Single use”, each bottle of Optiray can be used with the Bracco CT Expres pump injector system in a multi-dose technique for one or more patients, in accordance with local Radiology Dept. protocols. Optiray can be followed with a flush of N/S in accordance with Radiology Dept. protocols. * The Gastroenterologists have agreed to a 70-hour treatment (rather than 72 hours). A pre-printed prescription is available. In accordance with Cardiac Catheter Labs. and Assistant Practitioner protocols. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 143 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 144 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Ondansetron IV bolus only for: 4mg dose in any adult patient. 8mg dose in patients younger than 65 years. (I) IV infusion via infusion pump is required for: 8mg doses in patients aged 65 and older. 16mg doses (only allowed for patients younger than 75 years). (C) IV infusion. Infusion pump is required. IM injection WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND COMMENTS SUITABLE DILUENT 3-5 minutes Either give undiluted or dilute to any Flush with N/S. Groups convenient volume of N/S or G. Sodium content 0.16mmol/1ml. 1,2,3,4,5 and As recommended in MHRA Drug Safety 8 Update July 2013 to prevent lengthening of the QT-interval and possible Torsade De Pointes. 8mg doses for patients aged 65 or older should be given by IV infusion over 15 minutes. 15 minutes Dilute with 50ml to 100ml N/S or G Groups 8mg is the maximum dose for patients 1,2,3,4,5 and aged 75 or older. 8 All 16mg doses should be given by IV infusion over 15 minures. Repeat doses should be given at least 4 hours apart. Ondansetron should be avoided in patients with congenital long QT syndrome. Caution must be used if administering ondansetron to patients with risk factors 1mg/hour Groups for QT interval prolongation or cardiac 1,2,3,4 and 5 arrhythmias. These include: electrolyte abnormalities; use of other medicines that Refer to the Marsden Manual for Groups prolong QT interval (including cytotoxic guidance on IM injection. 1,2,3,4 and 5 drugs) or that may lead to electrolyte abnormalities; congestive heart failure; bradyarrhythmias; or use of medicines that lower heart rate . Hypokalaemia and hypomagnesaemia should be corrected before ondansetron administration. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 145 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Optiray® In accordance with Radiology Dept. protocols Oxytocin (C) infusion. Groups 1 Infusion pump is and 2 required. Orencia® WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Not for further dilution Group 1 or In accordance with Radiology Dept. Group 6 protocols Increase the rate Dilute 3 units of oxytocin (3 units = every 30 minutes 0.6ml of the 5 units/ml injection) to until contractions are 50ml with N/S. satisfactory (4 – 5/10) Using the 3 unit in 50ml dilution: Time from start of infusion Infusion rate Infusion rate (Minutes) (milliunits/minute) (ml/hour 0 1 1 30 2 2 60 4 4 90 8 8 120 12 12 150 16 16 180 20 20 Only increase the rate beyond this point following review and at the discretion of the specialist registrar or consultant. 210 24 24 240 28 28 270 32 32 See Abatacept COMMENTS Although the product is labelled for “Single use”, each bottle of Optiray can be used with the Bracco CT Expres pump injector system in a multi-dose technique for one or more patients, in accordance with local Radiology Dept. protocols. Optiray can be followed with a flush of N/S in accordance with Radiology Dept. protocols. For detailed instructions it is essential to read the PHNT Guidelines for Augmentation of Labour Continuous electronic fetal monitoring during administration is required. Stop the infusion during a prolonged deceleration or definite fetal distress (if CTG is abnormal perform FBS first). Do not infuse through the same line as blood or plasma. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 146 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Oxycodone WHO MAY ADMINISTER OVER INSTRUCTION FOR DILUTION AND COMMENTS GIVE SUITABLE DILUENT Staff prescribing, administering and/or screening prescriptions for opioid medications should be familiar with the PHNT Policy for Reducing Errors with Opioid Medicines in Adults using the following link: http://staffnet.plymouth.nhs.uk/Portals/1/Documents/Trust%20Documents/Medicines%20Management/Policy%20for%20Reducing%20D osing%20Errors%20with%20Opioid%20Medicines%20in%20Adults.pdf?timestamp=1443106367868 SC bolus Follow the PHNT Care of the Dying Refer to the Marsden Manual for Groups Pathway in Advance Kidney Disease and guidance on SC injection. 1,2,3,4 and 5 the PHNT Syringe Driver Policy. (C) SC infusion Groups 24 hours Dilute with W when 2 or more drugs via syringe driver 1,2,3,4 and 5 are being mixed in the same syringe. For combinations of 2 or 3 drugs in the same syringe refer to the compatibility for use in W or N/S may be used when the charts in the pump kit or contact palliative care. syringe only contains this drug. Pharmacy on ext. 39976 for advice. Patient See comments Dilute 50mg to 50ml with N/S. Adult PCA: Usual bolus dose 1mg. Usual Groups Controlled lock-out period is 5 minutes. Refer to 1,2,3,4 and 5 Analgesia (PCA) Acute Pain/Care Service Protocols. Background oxycodone infusion may only be prescribed by a member of the Acute Pain/Care Team. Nurse-led Controlled Analgesia via the PCA pump is available – seek advice from the Acute Pain/care Team. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 147 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE ADMINISTER OVER Pabrinex ® IV high potency injection (I) IV infusion (Preferred method) via infusion pump IV bolus Groups 1 30 minutes and 2 Groups 1 and 2 Groups 1 10 minutes INSTRUCTION FOR DILUTION AND SUITABLE DILUENT The contents of the pair(s) of ampoules should be diluted with 50 to 100ml N/S or G. (Up to 3 pairs of 5ml ampoules can be diluted with 50-100ml N/S or G). Mix contents of one 5ml Ampoule No.1 and one 5ml Ampoule No.2 (Maximum volume 10ml) in a single syringe immediately before use. The contents of one ampoule number 1 and one ampoule number 2 of Pabrinex Intramuscular High Potency (total 7ml) are drawn up into a syringe to mix them just before use, then injected slowly high into the gluteal muscle, 5cm below the iliac crest. For some brands the vials contain solution that requires further dilution. Pabrinex ® IM high potency injection IM injection Pamidronate (I) IV infusion. Maximum 1mg/minute. Groups Infusion pump is 1,2,3,4 and 5 required. A dose of 90 mg should normally be For vials that contain powder needing administered as a 2reconstitution before further dilution: hour infusion. reconstitute each 15mg vial with 5ml W. Reconstitute each 30mg and 90mg vial In renally impaired with 10ml W. patients the maximum recommended rate is Further dilution is necessary: 20mg/hour. Dilute 30mg to at least 125ml with N/S Dilute 60mg to at least 250ml with N/S Dilute 90mg to at least 375ml with N/S and 2 COMMENTS Flush with N/S or G. Mild allergic reactions are warning signs that further doses may cause anaphylactic shock Facilities for treating anaphylaxis must be available. Do not give the IM formulation via the IV route. Refer to the Marsden Manual for guidance on IM injection. Mild allergic reactions are warning signs that further doses may cause anaphylactic shock. Facilities for treating anaphylaxis must be available. Flush with N/S. Sodium content 0.11mmol/15mg. Monitor serum electrolytes, calcium and phosphate. Aredia® and Wockhardt® brands state that they should not be given if eGFR<30 unless the hypercalcaemia is lifethreatening and the benefit outweighs the risk. In order to minimise local reactions at the infusion site, the cannula should be inserted carefully into a relatively large vein. (If needed, pamidronate can be diluted with G instead of N/S). Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 148 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Pancuronium IV bolus preferably via a central IV line or through tubing of flowing N/S or G drip. (I) IV infusion via a 0.2-0.22 micron inline filter. Infusion pump is required. Groups 1 Panitumumab Paracetamol Parecoxib ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Flush with N/S or G. and 2 Groups A closed-system device must be Approximately 60 Do not mix with other drugs in the same used to prepare panitumumab. minutes. If the first line or lumen. infusion is tolerated, Flush with N/S. then subsequent Draw up the required dose and dilute infusions may be with N/S to a final concentration not administered over 30 exceeding 10 mg/ml. (First remove a to 60 minutes. Doses volume of N/S from the bag equal to higher than 1000 mg the volume of drug solution being should be infused added).The diluted solution should be over approximately mixed by gentle inversion, do not 90 minutes shake. Intravenous paracetamol must only be used when a patient cannot take any medicines by mouth and paracetamol cannot be given via an enteral feeding tube. Peri-operative patients able to take sips of water can take paracetamol orally with a little water. (I) IV infusion. Provided ready-diluted Can be flushed with N/S. Groups 100ml over 15 Infusion pump is minutes Each bottle is for single use only. 1,2,3,4,5 required. and 8 IV bolus Groups Rapid bolus directly Reconstitute 40mg vial with 2ml N/S (can Do not administer parecoxib together be reconstituted with 2ml G instead of with opioids in the same syringe. 1,2,3,4 and into a vein or into an existing line N/S if necessary). Dissolve the powder Do not reconstitute with Hartmann’s as 5 through which N/S, with a gentle swirling motion. this will cause precipitation. G or H is running. Deep IM injection Groups Reconstitute as above. Refer to the Marsden Manual for guidance on IM 1,2,3,4 and injection. 5 1,2,3,4 and 5 Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 149 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG INSTRUCTION FOR DILUTION AND COMMENTS SUITABLE DILUENT Parenteral nutrition (C) IV infusion. Adults: Each bag Do not infuse with any other drugs. Groups (TPN) Infusion pump is See back of Pharmacy TPN order 1,2,3,4 and 5 should run over no required. longer than 24 hours form for required monitoring of electrolytes, and LFT’s etc. 1. TPN must be ordered by 12 noon on the day it is required. Ensure that biochemistry results are available before the TPN is prescribed. It is advised to “Red Spot” the samples to speed the results. 2. All patients (except those on Penrose or Pencarrow) should be referred to the Nutrition Support Team (NST). If you wish to contact or refer a patient to the NST contact Dr Stephen Lewis Consultant Gastroenterologist on bleep 89756, Nutrition Nurse Specialist bleep 89755 or 89760, Dietitian on Ext 32243 or Pharmacy Technical Services on Ext 31084. 3. For patients on ICU please follow the ICU TPN protocol. 4. The protocol for connecting TPN bags and monitoring should be followed with meticulous attention. 5. TPN should not be commenced out-of-hours on weekdays (Between 5pm and 9am). On a Saturday, Sunday or Bank Holiday TPN is only available after discussion with the on-call Gastroenterologist. Once the on-call Gastroenterologist has agreed on the commencement of TPN, then he will contact the on-call pharmacist for a supply. This applies to all wards other than Penrose and Pencarrow (TPN bags are no longer available from the Pharmacy Night Cupboard). Pembrolizumab (C) IV infusion. Infusion to be prepared by Pharmacy. Flush with N/S. Groups 1 Infuse over 30 Infusion pump is minutes via a 0.2-5 Telephone ext. 31083. Doctor to Do not co-administer other ▼ This product is and 2 required. micron in-line filter prescribe dose diluted in N/S with a medicinal products through the being intensively final concentration between 1mg/ml same infusion line. monitored by the and 10mg/ml. CHM and MHRA. Please report all suspected reactions (including nonserious ones) using a Yellow Card from the BNF METHOD WHO MAY GIVE ADMINISTER OVER Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 150 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Pentamidine (Pentamidine isethionate) (I) IV infusion with patient Groups supine, via an infusion 1,2,3,4 and 5 pump, for the treatment of Pneumocystis jirovecii (formerly known as Pneumocystis carinii) pneumonia, or Trypanosomiasis Pertuzumab ▼ This product is being intensively monitored by the CHM and MHRA. Please report all suspected reactions (including nonserious ones) using a Yellow Card from the BNF IM injection for the treatment of Leishmaniasis or Trypanosomiasis (I) IV infusion. Infusion pump is required. WHO MAY GIVE ADMINISTER OVER Minimum 1 hour INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Pharmacy must prepare this. Contact Ext. 31083 Groups 1 1,2,3,4 and 5 Flush with N/S or G. Sodium content nil. Blood pressure must be closely monitored. To reduce the risk of severe, sudden hypotension, patient should be supine. Do not infuse with any other drugs. Refer to the Marsden Manual for guidance on IM injection. and 2 Groups COMMENTS Loading dose over A closed-system device must be used to prepare 60 minutes. pertuzumab. Maintenance doses over 30-60 Draw up the prescribed dose and minutes add to a 250ml bag of N/S. Gently invert the bag to mix the solution in order to avoid foaming. An observation period of 30 to 60 minutes is recommended after each Perjeta infusion and before commencement of any subsequent infusion of trastuzumab or docetaxel. Do not mix in the same line or lumen as any other drug solution or glucose. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 151 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Pethidine IM injection Groups Slow IV bolus SC injection 1,2,3,4 and 5 Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 Groups 1,2,3,4 and 5 ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Refer to the Marsden Manual for guidance on IM injection. 2 - 5 minutes Can be diluted with N/S or G. Refer to the Marsden Manual for guidance on SC injection. For status epilepticus Dilute to 10 times its own volume in adults: 10mg/kg at with W. a rate of no more than 100mg/minute. Maximum dose 1g. Phenobarbitone IV bolus Phentolamine mesylate IV bolus To treat hypertensive episodes due to phaeochromocytoma Group 1 May be diluted with N/S if required. Rapid IV bolus or IM injection for Group 1 Refer to the Marsden Manual for guidance on IM injection. Diagnosis of phaeochromocytoma Rogitine blocking test (C) IV infusion Group 1 0.2-2mg per minute titrating the dose to the desired blood pressure response Dilute with a suitable volume of N/S or G. COMMENTS Flush after IV bolus with N/S or G Monitor blood pressure, heart rate and respiratory rate. Have naloxone and resuscitation equipment available. Sodium content nil. Flush with N/S. Sodium content 0.79mmol/200mg. The injection is highly alkaline and may produce local tissue damage. Extravasation may cause tissue damage. Monitor sedation score, respiratory rate, heart rate and blood pressure. Flush with N/S or G. Monitor blood pressure and ECG. Protect from light. Use with care in asthmatics: monitor for hypersensitivity reactions. Refer to the translation of the package insert for details of how to perform the test and the monitoring required. Note that IV infusion of phentolamine is unlicensed. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 152 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Phenylephrine IV bolus Group 1 (I) IV infusion. Infusion pump is required. Groups 1 IM injection Groups 1 SC injection Phenytoin sodium For children, refer to the Paediatric Injection Administration Guide. (I) IV infusion through a large vein via an in-line 0.22-0.5 micron filter, using an infusion pump. and 2 and 2 Groups 1 and 2 Groups 1,2,3,4 and 5 Slow IV bolus or (I) Groups IV infusion into a 1,2,3,4 and large vein. A pump 5 is required for infusion. This method, (undiluted infusion) may only be used for adults. ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT 100-500micrograms slowly Dilute to 1mg in 1ml with N/S. over 3-5 minutes, repeated if necessary after at least 15 minutes. Adults: Maximum initial Add 10mg to 500ml of N/S or G. rate 180micrograms/ minute reduced according to response to 30 – 60 micrograms/minute Refer to the Marsden Manual for guidance on IM injection. Refer to the Marsden Manual for guidance on SC injection. Adults: Maximum If a suitable in-line filter is not 50mg/minute. available then give as undiluted injection via a syringe pump as below. If a suitable filter is available After dilution: Use dilute with N/S to a final immediately, complete concentration not exceeding infusion within 1 hour. 10mg/1ml. Do not use if solution is hazy or contains precipitate. Adults: Maximum 50mg/minute. Give undiluted. COMMENTS Flush IV bolus with N/S or G. Extravasation may cause tissue damage. Monitor blood pressure and heart rate. When an IV infusion is discontinued, slow the infusion rate gradually; do not stop it abruptly ECG and blood pressure monitoring essential. Monitor for possible respiratory depression. Flush with N/S before and after administration of each injection or infusion to avoid venous irritation. Sodium content 0.91mmol/250mg. Incompatible: Do not infuse with any other drugs. Resuscitation equipment should be available. Suitable filters to administer phenytoin diluted in N/S include PALL 0.22 micron, Braun Sterifix 0.2 micron, Technopharm codan 0.2 micron filters. These filters should be ordered through ORACLE. Note that dilution of Kent/Hikma brand phenytoin injection is not licensed. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 153 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Phosphate Polyfusor ADMINISTER OVER INSTRUCTION FOR DILUTION AND COMMENTS SUITABLE DILUENT Dosage: Serum phosphate 0.5-0.7mmol/L (I) IV infusion via Groups Infuse over 6 – 12 Provided ready-diluted. Do not infuse 1 - 2ml/kg. Serum phosphate <0.5mmol/L further dilute. peripheral or 1,2,3,4 and 5 hours. infuse 2 – 5ml/kg. Maximum dose 500ml per central IV line. Maximum rate: infusion. Infusion can be repeated if necessary. Infusion pump is 150ml/hour required. To treat Re-feeding Syndrome, 500ml (50mmol phosphate) is typically infused over 12 hours. Incompatible with This dose may be repeated depending on serum other solutions phosphate levels. containing calcium Consider reduced dosage in the elderly or or magnesium, patients with impaired renal function. Monitor Hartmann’s serum electrolytes including phosphate and solution, Ringer’s calcium (frequently in renal impairment). Monitor solution, renal function, ECG and fluid balance. ciprofloxacin, Pain and phlebitis may occur at the infusion site. dobutamine and TPN Sodium content 162mmol/L Potassium content 19mmol/L Phosphate content 100mmol/L Flush with N/S. Phytomenadione IV bolus (Konakion MM® vitamin K) 10mg in 1ml WHO MAY GIVE Groups Over at least 30 May be given undiluted. seconds, usually 3-5 1,2,3,4 and 5 Alternatively, draw up the required minutes per 10mg. dose from the ampoule then dilute further with a small volume (eg. 10-20ml) of G. Do not dilute the 10mg in 1ml with G and take the fraction of the diluted injection corresponding to the required dose, as the MM formulation does not distribute evenly in the diluent. Product has been reformulated without polyethoxylated castor oil, however there is still a risk of anaphylaxis with rapid IV administration. Protect infusion and giving set from light. Flush with G. The contents of the 10mg in 1ml ampoules can be given by mouth, but this use is unlicensed (See page 7) Do not administer via the IM route. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 154 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Phytomenadione (Konakion MM® Paediatric vitamin K) 2mg in 0.2ml IV bolus. Groups The dose may be 1,2 and 4 injected into the lower part of an infusion set containing 5% dextrose or 0.9% sodium chloride running at 0.7ml/minute IM injection WHO MAY GIVE Groups 1,2 and 4 ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Do not further dilute. COMMENTS Product has been reformulated without polyethoxylated castor oil, however there is still a risk of anaphylaxis with rapid IV administration. Flush with G. The contents of the 2mg in 0.2ml ampoules are also licensed to be given by mouth. For neonatal use following the protocols Further neonatal information can be found on NICU in the Neonatal Formulary 6th Edition. Konakion MM Paediatric must be administered by IV injection when used as an antidote to anticoagulant drugs such as warfarin & phenindione, as IM injections may result in significant bleeding in these patients. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 155 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Piperacillin/ Tazobactam WHO MAY ADMINISTER INSTRUCTION FOR DILUTION AND COMMENTS GIVE OVER SUITABLE DILUENT Piperacillin/Tazobactam (= Tazocin®) contains a penicillin – check patient’s allergy status before administration (I)IV infusion Give over 30 Reconstitute each 2.25g with 10ml and Flush with N/S. Groups using an infusion 1,2,3,4 and 5 minutes each 4.5g with 20ml of W, or N/S. Sodium content: 4.7 - 5.58mmol/2.25g vial pump. Swirl until dissolved. When swirled and 9.4 – 11.2mmol/4.5g vial. constantly reconstitution should occur Incompatible with all aminoglycosides. within 3 minutes. Do not mix with or give through the same Slow IV bolus of this medication Displacement ranges 1.5 – 1.7ml per line at the same time as gentamicin, amikacin, tobramycin etc. If only one line is no longer 2.25g. available separate the doses and flush well recommended The reconstituted solution may be with N/S before and after each dose. or licensed. further diluted with N/S or G to the desired volume (eg. dilute to 50ml or Do not give through the same line as add to a 100ml mini-bag). Hartmann’s In paediatrics, the maximum concentration for infusion is 90mg/ml. Pitressin ® See vasopressin Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 156 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Potassium chloride (C) IV infusion. ready prepared Infusion pump infusion bags is required. containing 20mmol/L or 40mmol/L potassium in N/S, G or G/S. Can be kept as stock by all wards and departments. Ready-made bags containing 80mmol/litre are also available WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Groups Adults: Usual maximum rate 20mmol potassium/hour. If a concentration of potassium other than 20, 40 or 80mmol/litre is prescribed contact the ICU pharmacist or the on-call pharmacist. Adults: Usual maximum rate 20mmol potassium/hour* Critical care areas only may give undiluted 2mmol/ml potassium injection via a central line with ECG monitoring, or dilute to the required concentration with N/S, G, G/S or H with thorough mixing. Pain or phlebitis may occur during peripheral administration of solutions containing 30mmol or more potassium/litre. Solutions containing more than 40mmol/litre potassium should ideally be given via a central line. However, in cases of serious hypokalaemia with no central access up to 80mmol/litre potassium may be tolerated peripherally if given via a large vein (e.g. femoral vein). Extravasation will cause tissue damage. *In adults, the rate of administration may be increased to 40mmol/hour in the initial management of diabetic ketoacidosis, and if necessary in Cardiothoracic ICU, so long as the patient’s ECG is monitored and resuscitation equipment is available. Administration of IV potassium at a rate exceeding 40mmol/hour poses a serious risk of asystole. Flush with N/S. For instructions on the use of potassium chloride injection during cardiopulmonary bypass refer to the Blood Cardioplegia Management section of the Clinical Perfusion policy. 1,2,3,4 and 5. Selected Group 8 Assistant Practitioners can administer potassium chloride 20mmol in 1L N/S in accordance with the AP protocols. Potassium chloride (I) IV infusion Groups 1 15% injection via central IV and 2 line via infusion Potassium chloride pump. 50mmol in 50ml pre-filled syringes May only be stocked by Critical Care areas From October 2015 Penrose and Pencarrow will be using pre-filled syringes containing 50mmol potassium chloride in 50ml. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 157 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Potassium chloride ready prepared infusion bags containing 20mmol/L potassium in N/S, G or G/S. (C) SC infusion Adults: maximum Groups Only use gravity- 1,2,3,4 and 5 rate 20mmol potassium/hour. feed administration sets. Never use an infusion pump for SC infusions. Potassium chloride Intra-cardiac for 15% injection feticide WHO MAY GIVE Group 1 ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Use the ready-made infusion bags containing 20mmol/L potassium chloride available from Pharmacy. There is anecdotal evidence that up to 40mmol/L potassium can be given by SC infusion. However, SC potassium infusion can cause ulceration and the risk is greater at 40mmol/L than at 20mmol/L. Monitor the infusion site regularly for early signs of irritation and inflammation. To be administered in accordance with procedures for feticide on the Early Pregnancy Unit or the Emergency Gynaecology Unit. A single ampoule may be ordered as a Controlled Drug by these Units. Records of receipt and administration are as for Controlled Drugs. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 158 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Potassium phosphate (Dipotassium hydrogen phosphate) injection (I) infusion. Infusion pump is and 2 required. *May only be stocked by Critical Care areas. Privigen® Prochlorperazine Procyclidine WHO MAY GIVE Groups 1 ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Adult patients on a critical care unit: Usual maximum rate 20mmol potassium/hour (30mmol phosphate over 3 hours) Critical care areas only may give undiluted potassium phosphate injection via a central line with ECG monitoring. For administration via a peripheral line dilute with N/S, G or G/S to a usual maximum concentration of 40mmol potassium/litre. Flush with N/S Up to 0.3 – 0.6mmol/kg/day of phosphate may be required during the treatment of Refeeding Syndrome. Dipotassium phosphate 17.42 % injection contains 1mmol phosphate/ml and 2 mmol potassium/ml. Refer to the Marsden Manual for guidance on IM injection. Dilute 1 part with 5 parts N/S before administration. Flush IV bolus with N/S. Prochlorperazine is unlicensed (See page 7) by the IV route. IV administration can cause hypotension and venous irritation. Dilution is not recommended. Flush with N/S It is suggested that general wards ask the doctor to prescribe a dose of Phosphate Polyfusor instead (See page 182) See Immunglobulin Human Normal Deep IM injection Groups 1,2,3,4 and 5 IV bolus Maximum rate Groups 1,2,3,4 and 5 6.25mg/minute IV bolus Groups Suggestion: over 1 1,2,3,4 and 5 minute Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 159 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Propofol IV bolus Groups 1 ADMINISTER OVER and 2* (C) IV infusion. Groups 1 and 2 Propranolol IV bolus Emergency use. Group 1 Dependent on indication. Adults: 1mg over 1 minute. May be repeated at 2-minute intervals until desired response observed or until maximum dose* INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Do not dilute. Can be administered through tubing (close to the injection site) of infusions of N/S, G or G/S. COMMENTS Monitor ECG and blood pressure. Also monitor for airway obstruction and oxygen saturation. Resuscitation equipment should be available. *Boluses of propofol may only be given by Group 2 nurses to ventilated patients in level 3 critical care. Infuse undiluted or dilute with G to a Administer immediately after preparation of concentration of not less than 2mg/1ml. the syringe or infusion. Anaesthetics Directorate policy: Administer B.Braun Propfol-Lipuro can be diluted propofol within 30 minutes of drawing up with G, N/S or G/S to a concentration into syringe. of not less than 2mg/1ml. Use propofol diluted with G, N/S or G/S within 6 hours of preparation. When using B.Braun (Propofol –Lipuro), Generics UK and Fresenius kabi brands of propofol in bottles for infusion, the bottle and line should be changed at least every If diluted in a PVC bag withdraw a 12 hours. volume of infusion fluid and replace it To reduce pain on injection 20ml 1% with an equal volume of propofol 1%. propofol may be mixed with up to 1ml of 1% lignocaine immediately before use. Flush with N/S. Can be diluted with N/S or G. ECG monitoring required. Flush with N/S. Sodium content nil. If IV used as temporary substitute for oral propranolol 1mg IV = 10mg orally. *Maximum dose of 10mg in conscious patients or 5mg in patients under anaesthesia. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 160 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Protamine sulphate Protirelin ADMINISTER OVER Reversal of IV heparin Groups Slow injection over infusion 1,2,3,4 and 10 minutes. Maximum rate 5 IV bolus 5mg/minute Reversal of SC heparin: Groups Slow IV injection 1,2,3,4 and (maximum rate Dose: 1mg protamine per 5mg/minute) 100 units heparin. Give 25- 5 followed by 50mg of this dose by slow infusion of the IV bolus followed by (C) IV remainder of the infusion of the remainder of calculated the calculated protamine protamine dose dose via an Infusion pump. over 8-16 hours INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Can be diluted with N/S. Flush with N/S. Monitor APTT coagulation tests. Dilute to a suitable volume with N/S or G. Too rapid administration of protamine sulphate may cause severe hypotension and anaphylactoid reactions. Facilities for resuscitation and treatment of shock should be available. Partial (60% maximum) Groups Maximum rate reversal of enoxaparin 1,2,3,4 and 5mg/minute Within the first 8 hours after 5 enoxaparin administration: 1mg protamine per 1mg enoxaparin (maximum dose 50mg protamine) by slow IV bolus Can be diluted with N/S. Decisions regarding the necessity and dose of subsequent protamine injections should be based on clinical response rather than measurement of anti Xa or anti XIIa results. The physician should also consider that the amount of enoxaparin in the body drops to 50% after 8 hours and 33% or less after 12 hours. The dose of protamine should be adjusted depending on the length of time since enoxaparin was administered. IV bolus WHO MAY GIVE Group 1 30-60 seconds Suggestion: Over 30-60 seconds Diagnostic test. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 161 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Quinine dihydrochloride (I) IV infusion. Infusion pump is required. Groups Ramucirumab (I) IV infusion. Infusion pump ▼ This product is is required. being intensively monitored by the CHM and MHRA. Please report all suspected reactions (including non-serious ones) using a Yellow Card from the BNF ADMINISTER OVER 4 hours INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Dilute required dose in 250ml or 500ml N/S or G. However, in fluid restricted patients a maximum dilution of 30mg/ml may be infused via a central IV line, COMMENTS Flush with N/S Therapy should be changed to oral as soon as 1 and 2 possible. Sodium content: negligible. See comments Usual loading dose is 20mg/kg (upto a maximum for alternative of 1.4g) quinine dihydrochloride over 4 hours. On possible ICU the loading dose can alternatively be given administration of as 7mg/kg quinine dihydrochloride infused over loading dose on 30 minutes followed immediately by 10mg/kg ICU. over 4 hours. A closed-system device must Infuse over *The infusion rate of ramucirumab should be Groups be used to prepare reduced by 50% for the duration of the infusion 1,2,3,4 and 5 approximately 60 ramucirumab. minutes* via a and all subsequent infusions if the patient 0.22 micron inexperiences a grade 1 or 2 infusion-relatedline filter. reaction. Dilute the prescribed dose to Monitor for: rigors/tremors, back-pain/spasms, 250ml N/S (first remove a chest pain and/or tightness, chills, flushing, (Maximum rate of volume of N/S from the bag, dyspnoea, wheezing, hypoxia, paraesthesia, equal to the volume of 25mg/minute – bronchospasm, supraventricular tachycardia, ramucirumab solution being for very large added). Gently invert the bag to and hypotension. patients the Temporarily discontinue the infusion in the event infusion time may ensure adequate mixing. DO of severe hypertension, until controlled with NOT SHAKE the infusion need extending) antihypertensives. solution. Resuscitation equipment should be immediately available. Flush with N/S’ DO NOT dilute with other solutions or co-infuse with other electrolytes or medicinal products. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 162 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Ranitidine IV bolus Groups (I) IV infusion via pump. Groups (C) IV infusion via pump, after initial IV bolus. Groups 125-250 1,2,3,4 and 5 micrograms/ kg/hour Dilute 150mg ranitidine to 250ml with N/S or G. IM injection Groups Refer to the Marsden Manual for guidance on IM injection. INSTRUCTION FOR DILUTION COMMENTS AND SUITABLE DILUENT Adults: at least 2 May be diluted further with G or N/S (20ml for example) 1,2,3,4,5 and minutes* 8 Children: at least 3 minutes* 1,2,3,4 & 5 1,2,3,4 and 5 ADMINISTER OVER 2 hours at 25mg/hour Add 50mg ranitidine to 100ml N/S or G. Flush with N/S, G or G/S. Sodium content 0.12mmol/2ml. *A slower bolus over 5 minutes is recommended by some references because of the risk of causing bradycardia on administration. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 163 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Groups 1 RadioPharmaceuticals Rasburicase WHO MAY ADMINISTER OVER GIVE Refer to Group Protocols/PGD’s within the Department of Nuclear Medicine. and 7 (I) IV infusion. Infusion pump is required. Groups 1,2,3,4 and 5 COMMENTS 30 minutes Reconstitute each 1.5mg vial with the 1ml of solvent provided. Reconstitute each 7.5mg vial with the 5ml solvent provided. Swirl the vials gently to dissolve the powder. Do not shake. The reconstituted solution will be 1.5mg/ml. Draw up the prescribed dose from the reconstituted vials and add to a 50ml EasyFlex bag of N/S. Infuse through a different line to that used for chemotherapy agents. If this is not possible, flush between the chemotherapy agents and rasburicase with N/S. Rasburicase is not cytotoxic or mutagenic Rasburicase is not compatible with glucose solutions. Pharmacy will dispense a 50ml EasyFlex bag of N/S for each dose of rasburicase when it dispenses the rasburicase vials. Usual dosages: Prophylactic: 3mg once daily for 1-3 days Treatment: 0.2mg/kg rounded to the nearest 1.5mg, once daily, depending on seum uric acid levels. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 164 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY ADMINISTER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT GIVE OVER Remifentanil IV bolus infusion at Groups 1 induction of and 2 anaesthesia. (C) IV infusion during maintenance of anaesthesia or for sedation of ventilated patients in intensive care. Infusion pump is required. Anaesthesia in adults including cardiac anaesthesia Bolus infusion 0.5 –1 microgram/kg over at least 30 seconds. Continuous infusion 0.025 –2 microgram/kg/minute (rate dependent on choice of general anaesthetic(s)) If not using preprogrammed syringe pump see table below Reconstitute to a concentration of 1mg/ml with N/S or W. Further dilute to a concentration of 20-250 micrograms/ml with N/S or G. (20 -25 micrograms/ml is recommended for paediatric patients aged 1 year and over). For TCI (Target Controlled Infusion) the recommended dilution is 20-50 micrograms/ml. However, 100 microgram/ml (eg 5mg in 50ml) is often used for TCI and for sedation of ventilated ICU patients. COMMENTS IV bolus infusion not necessary if intubation is to occur more than 8-10 minutes after commencing remifentanil infusion. IV bolus infusion is not recommended for induction in cardiac anaesthesia .Instead intubate at least 5 minutes after start of infusion. Monitor cardiovascular and respiratory functions. Resuscitation equipment must be available. Do not flush line. Sodium content: Nil. REMIFENTANIL INFUSION RATES Anaesthesia in children Sedation in Intensive Care 1 – 12 years of age (Standard Remifentanil Protocol for Penrose & Pencarrow wards, Derriford Hospital) Bolus infusion Continuous infusion Dilute the reconstituted remifentanil to 100mcg/ml with N/S (equivalent to 5mg in 50ml). 1 microgram/kg 0.05 –1.3 over at least 30 microgram/kg/minute Start the infusion at 5ml/hour, and titrate rate in 1ml/hour increments every 5 minutes to achieve the desired analgesia/sedation. seconds. (rate dependent on Usual range 1 – 10ml/hour. choice of general anaesthetic(s)) At rates above 10ml/hour, monitor for bradycardia and hypotension. Do not bolus remifentanil. However, when infusing remifentanil and propofol through the same lumen, propofol may be bolused, as the volume of remifentanil between the 3-way tap and the tip of the catheter is not considered significant. N.B. the use of remifentanil, and the bolusing of propofol often require mandatory ventilation. For patients <50kg, start infusion at 2.5ml/hour and titrate in 0.5ml increments. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 165 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Rifampicin (I) IV infusion. Groups 1,2,3,4 Infusion and 5 pump is required. Rocuronium Rapid IV bolus (C) IV infusion. Infusion pump is required. Rituximab For treating lymphoma SC injection WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Reconstitute with diluent provided (10ml) and 2-3 hours shake vigorously for 30 seconds. Then dilute to a concentration of 600mg in 500ml N/S, G or G10%. If patient is fluid restricted 600mg may be diluted in 100ml G and given over 30 minutes. Group 1- must only be given by doctors proficient in advanced airway management. Also see comments Groups 1 and 2 Groups 1 and 2 No specific recommendations. Dilute to appropriate volume with N/S, H or G. COMMENTS Flush with N/S. Discard remaining infusion after 6 hours. Sodium content less than 0.5mmol/600mg. Displacement volume for a 600mg vial is 0.48ml. Do not infuse with any other drugs. Flush with N/S or G. Compatible with G/S and H. Sodium content 0.72mmol/50mg. If the patient is ventilated IV bolus can be administered by Group 2 staff. 300-600 micrograms/kg/hour Draw up the 1400mg in 11.7ml from the vial using a closed-system device. Common side effecs: injection site erythema, pain or oedema Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 166 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Rituximab For treating severe active Rheumatoid Arthritis in adults, or for treating lymphoma or leukaemia WHO MAY ADMINISTER OVER INSTRUCTION FOR DILUTION GIVE AND SUITABLE DILUENT Read and print off the full guideline from the Royal College of Nursing: http://www.rcn.org.uk/__data/assets/pdf_file/0008/262385/Rituximab_protocol.pdf (I) IV Groups 1 (Premedication is required – see comments) Although rituximab may be diluted with N/S to a concentration infusion via and 2 First infusion on Day 1: between 1mg/ml and 4mg/ml, the an infusion 50mg/hour (25ml/hour of 1g in 500ml dilution) usual concentration is 2mg/ml. pump for the first 30 minutes then 100mg/hour (50ml/hour of 1g in 500ml Rituximab infusion should be dilution) for the second 30 minutes, prepared by Pharmacy. then the rate can be increased by 50mg/hour Telephone Ext. 31083. (25ml/hour of 1g in 500ml dilution) every 30 minutes to a maximum rate of 400mg/hour (200ml/hour of 1g in 500ml dilution) providing no adverse reactions occur. (Premedication is required – see comments) Second infusion on Day 15: 100mg/hour (50ml/hour of 1g in 500ml dilution) for the first 30 minutes then 200mg/hour (100ml/hour of 1g in 500ml dilution) for the second 30 minutes, then the rate can be increased by 100mg/hour (50ml/hour of 1g in 500ml dilution) every 30 minutes to a maximum rate of 400mg/hour (200ml/hour of 1g in 500ml dilution) providing no adverse reactions occur. COMMENTS Premdication: Dose of oral paracetamol 60 minutes before each rituximab infusion (not if paracetamol already given in the last 4 hours). Chlorphenamine 10mg IV 60 minutes before each rituximab infusion. Methylprednisolone 100mg in 100nl N/S infused over 30 minutes to be commenced 60 minutes before each rituximab infusion (not always in Haematology). Full resuscitation facilities must be immediately available. Monitoring: 1st hour – blood pressure, pulse, temperature and O2 sats every 15 minutes. Thereafter, every 30 minutes after increasing the infusion rate, and throughout the course of the infusion once maximum rate is reached. Possible reactions: Low grade fever, BP drop of <30mmHg from baseline: halve the infusion rate. Fever >38.50C, chills, mucosal swelling, dyspnoea, BP drop of > 30mmHg from baseline: stop the infusion and contact the doctor. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 167 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Romiplostim (Nplate®) SC Injection by 1. Remove the plastic cap from Romiplostim powder vial and clean rubber stopper using the provided alcohol swab. 5. Holding the pre-filled syringe of 2. Attach vial adapter to Romiplostim vial by peeling off paper backing from vial adapter, keeping the vial adapter in its packaging. Keeping the vial on the bench, push the vial adapter down onto the centre of the vial until it is firmly in place. 6. Keeping the vial on the bench, attach the pre-filled syringe of water for injections to vial adapter: hold the outer edge of the vial adapter with one hand and twist the syringe tip clockwise onto the adapter with the other hand until you feel a slight resistance. 3. Remove and discard vial adapter packaging. 7. Very slowly and gently expel all water (0.72ml) into the 250 microgram powder vial. Water should flow slowly onto powder. GENTLY swirl the vial until all of the powder has dissolved and the fluid in the vial is clear and colourless. Do not shake or agitate vial 4. Attach plunger rod to the prefilled syringe of water for injections by twisting the plunger rod clockwise onto the syringe plunger, until you feel a slight resistance. 8. Visually inspect the reconstituted solution for particulate matter and/or discoloration. The reconstituted solution should be clear and colourless and should not be administered if particulate matter and/or discolouration are observed. Make sure solution is fully dissolved before removing syringe. Instructions continued on next page… Groups 1 and 2 Each vial is for single use only. Do not mix with N/S or any drug solutions Refer to the Marsden Manual for guidance on SC injection. water for injections with one hand, bend the tip of the white plastic cover downward with your other hand. This will break the seal of the white plastic cover. Once the seal is broken, pull cover off to separate the grey rubber cap from the clear plastic syringe tip. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 168 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD (Continued from previous page) Romiplostim (Nplate®) SC Injection by 9. Remove the empty pre-filled syringe from the vial adapter. 10. Remove 1 ml administration syringe from package. Attach the 1 ml syringe to vial adapter of reconstituted solution by twisting the syringe tip onto the vial adapter until you feel a slight resistance. 13. Twist off administration syringe from vial adapter. 11. Turn assembled syringe-vial unit upside down, so the vial of reconstituted product is above the syringe. Withdraw all of the medicinal product solution into the administration syringe. 14. Prepare injection site with a new alcohol swab. Pull back on the pink safety cover toward the syringe and away from the needle. Remove clear needle shield from prepared needle by holding syringe in one hand and carefully pulling shield straight off with the other hand. 12. Ensure the correct amount of solution for the patient dose is in the administration syringe by expelling any excess solution back into the vial. 15. Administer subcutaneous injection following local protocols and good aseptic technique. Groups 1 and 2 (Continued) 0.5ml of reconstituted solution contains 250micrograms Attach safety needle to the filled administration syringe by twisting needle clockwise into syringe Luer lock tip. 16. After injecting, activate the pink safety cover by pushing the cover forward using the same hand until you hear and/or feel it click/lock. 17. Immediately discard syringe and needle into an approved Sharps Container Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 169 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Salbutamol IV bolus SC injection WHO MAY ADMINISTER OVER GIVE Groups 3-5 minutes 1and 2 Groups 1 and 2 (C) IV infusion. Groups Infusion pump 1,2,3,4 and is required. 5 (I) IV infusion using syringe pump. Groups 1 (I) IV infusion. Using volumetric pump. Groups 1 and 2 and 2 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Dilute 500micrograms in 1ml salbutamol injection with 9ml W, N/S or G to give a concentration of 50micrograms in 1ml. Refer to the Marsden Manual for guidance on SC injection. Asthma: Asthma: Dilute 5ml (5mg) of Ventolin Solution for Infusion to 3-20 micrograms/minute = 18 -120ml/hour of the 5mg in 500ml with G or N/S to make a concentration of 10micrograms/ml 500ml dilution Premature Labour: Premature labour: Dilute 10ml 10 micrograms/minute (10mg) of Ventolin Solution for increasing the rate at 10 minute Infusion to 50ml with G or N/S to intervals to maximum rate of 45 make a concentration of 200 micrograms/minute. Once micrograms/ml uterine contractions have Premature Labour: Dilute 10ml ceased the infusion rate should (10mg) of Ventolin Solution for be maintained at the same level Infusion to 500ml with G or N/S to for one hour and then reduced make a concentration of by 50% decrements at six 20 micrograms/ml hourly intervals COMMENTS Flush with N/S or G. ECG monitoring recommended. Sodium content 0.15 mmol/ml. If necessary in adult or paediatric intensive care salbutamol 5mg/5ml IV solution for infusion may be given undiluted via a central IV line (this method is unlicensed -see page 7) 3 – 20 micrograms/minute = 0.18 – 1.2ml/hour using this dilution. 10 – 45micrograms/minute = 3 -13.5ml/hour of the 10mg in 50ml dilution. 10 – 45micrograms/minute = 30 – 135ml/hour of the 10mg in 500ml dilution. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 170 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Secretin pentahydrochloride (Secrelux®) IV bolus Groups 1 (Secrelux® is an unlicensed productsee page 7) Sodium benzoate 2g in 10ml and 2 (I) IV infusion. Groups 1 Infusion pump is and 2 required. Loading dose (I) IV infusion (Unlicensed product- Maintenance see page 7) (C) IV infusion Groups 1 and 2 Groups 1 and 2 ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT For exocrine Reconstitute each vial with the pancreatic function test 10ml N/S provided making a inject over 1 – 2 concentration of 10 Clinical minutes Units/ml. Draw up the prescribed dose. 1 hour Reconstitute each vial with the 10ml N/S provided making a concentration of 10 Clinical Units/ml. Draw up the prescribed dose and infuse over 1 hour. 90 minutes Draw up 250mg/kg = 1.25ml/kg of injection and dilute in 5ml/kg of 10%G. 24 hours Draw up 250mg/kg = 1.25ml/kg of injection and dilute in 5ml/kg of 10%G. COMMENTS Can be given as infusion using a syringe pump depending on how the test is run. 1 Clinical Unit/kg dose = 0.1ml/kg of reconstituted secretin 2 Clinical Unit/kg dose = 0.2ml/kg of reconstituted secretin. Administer immediately after preparation. Follow the BRHC guidelines for the management of hyperammonaemia – http://nww.swretrieval.nhs.uk/DI_ALL.htm Click on “Clinical Guidelines” then “Hyperammonaemia” Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 171 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Sodium bicarbonate (C) IV infusion. Groups Infusion pump is 1,2,3,4 and 5 required. Sodium chloride N.B. All bags of sodium chloride are for single use only. WHO MAY GIVE IV bolus Group 1 (C) or (I) IV infusion. Groups IV bolus All groups 1,2,3,4,5 and 8 (C) SC infusion Groups Only use gravity- 1,2,3,4 and 5 feed administration sets. Never use an infusion pump for SC infusions. ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Ready prepared infusions are available from pharmacy. Can be diluted with N/S or G. COMMENTS Ready prepared infusions are available from pharmacy. Concentrations over 1.8% should be given via a central line. Sodium content of 0.9% injection is 150mmol/1 litre. Flush with N/S or G. Concentrations for IV infusion greater than 1.4% should be given via a central IV line Can be diluted with G, G/S or H. Usual rate is 500ml over 8 hours (21 drops per minute). Maximum rate is 500ml over 1 hour (167 drops per minute) Maximum concentration of sodium chloride by subcutaneous infusion is 0.9%. Usual maximum of 2 litres in 24 hours. However, 3 litres may be given if necessary over 24 hours using two SC sites. The needle and giving set should preferably be changed every 72 hours. However, infusion sets can be left in place for up to 5-7 days if there are no complications. Refer to potassium chloride monograph for SC potassium. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 172 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Sodium fusidate/ Fusidic acid (I) IV infusion into Groups a central venous 1,2,3,4 and 5 line (preferred method). Infusion pump is required ADMINISTER OVER 2 hours 6 - 8 hours (I) IV infusion into Groups wide bore 1,2,3,4 and 5 peripheral vein. Infusion pump is required. 6 -8 hours INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Displacement is negligible. Add 10ml buffered diluent for 500mg in 10ml (50mg in 1ml). Reconstitute with 10ml buffered diluent provided then dilute with 500ml N/S or G. For fluid restricted patients reconstitute as above then dilute with 100ml N/S (unlicensed dilution - see page 7) Reconstitute and dilute with 500ml as above. Alternatively for fluid restricted patients dilute with 250ml N/S or G (unlicensed dilution - see page 7). COMMENTS G can be used as diluent but opalescence may occur with more acidic samples (infusion must be discarded). Flush with N/S. When reconstituted with 10ml buffer, preparation contains 3.1mmol sodium and 1.1mmol phosphate. Sodium fusidate is well absorbed from the GI tract so consider an early switch to tablets or mixture. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 173 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Sodium nitroprusside (C) IV infusion. Infusion pump is 1 and 2 required. (N.B Nitroprussiat fides brand is unlicensed – see page 7) INSTRUCTION FOR DILUTION WHO MAY ADMINISTER OVER AND SUITABLE DILUENT GIVE Increase rate slowly until Reconstitute 50mg with the 5ml G Groups COMMENTS Intra-arterial blood pressure monitoring necessary. Protect infusion and administration set from light: Use the tin foil provided to wrap Intensive care areas or Theatres the bag and administration set, or the line. only may use a dilution of 1mg/ml Use an amber syringe if giving by syringe 50mg in 50ml) in G via a central IV pump. line. Discontinue infusion gradually over 15-30 minutes to avoid rebound hypertension. Discard infusion solution if it is highly coloured. When using the Nitroprussiat fides brand the prepared infusion should be discarded after 4 hours. Do not flush - replace giving set. Sodium content 0.34mmol/50mg. Using the 50mg in 50ml dilution for Intensive Care areas or Theatres: Hypertensive crisis 0.5 – 8micrograms/kg/minute = 0.03 – 0.48ml/kg/hour Maintenance of blood pressure at 30-40% lower than pre- 20 – 400micrograms/minute =1.2 – 24ml/hour treatment diastolic (Lower doses if treated with other antihypertensives) Controlled hypotension in surgery Up to a maximum of =Up to a maximum of 0.09ml/kg/hour 1.5micrograms/kg/minute Heart failure 10 – 200micrograms/minute =0.6 – 12ml/hour desired effect occurs. The maximum rate is 8micrograms/kg/minute in order to avoid excessive levels of cyanide and thiocyanate and to lessen the possibility of a sudden drop in blood pressure. provided then further dilute with 500ml or 1000ml of G. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 174 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Sodium phenylbutyrate 2g in 10ml Loading dose (I) IV infusion (Unlicensed product- see page 7) Maintenance (C) IV infusion WHO MAY GIVE Groups 1 ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS About 90 minutes Draw up 250mg/kg = 1.25ml/kg of injection and dilute in 5ml/kg of 10%G. Draw up 250mg/kg = 1.25ml/kg of injection and dilute in 5ml/kg of 10%G. Follow the BRHC guidelines for the management of hyperammonaemia – and 2 Groups 1 and 2 24 hours http://nww.swretrieval.nhs.uk/DI_ALL.htm Click on “Clinical Guidelines”, then “ALL” then “Hyperammonaemia” For a ready-made phosphate infusion that can be given via a peripheral or central vein, see the monograph for Phosphate Polyfusor Sodium Via a peripheral vein dilute dose (I) or (C) IV Adult patients on a Flush with N/S. Groups Phosphate infusion. Infusion 1,2,3,4 and 5 critical care unit: with a suggested volume of 500ml (Disodium pump is required Suggested maximum N/S or G. Up to 0.3 – 0.6mmol/kg/day of phosphate Hydrogen infusion rate of may be required during the treatment of Phosphate) 10mmol phosphate per Undiluted sodium phosphate Refeeding Syndrome. hour (30mmol injection may be infused via a central IV line using a syringe phosphate in 50ml Disodium hydrogen phosphate 21.49% over 3 hours). pump. injection contains 6mmol phosphate in It is suggested that 10ml general wards infuse (30mmol phosphate in 50ml). the dose of phosphate over 12 hours or ask the doctor to prescribe a dose of Phosphate Polyfusor instead (See page 146) Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 175 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE ADMINISTER OVER Sodium valproate IV bolus Usual method Groups 3 - 5 minutes. (C) IV infusion. Infusion pump is required. (I) IV infusion. Infusion pump is required. (C) or (I) IV infusion. Infusion pump is required. Groups Streptokinase 1,2,3,4 and 5 1,2,3,4 and 5 Groups Divide total infusion volume by 24 to set the hourly rate on the pump 1 hour 1,2,3,4 and 5 Groups 1,2 and 3 Myocardial Infarction: 1.5 MU over 60 minutes. Embolism/thrombosis 250,000 units over 30 minutes followed by 100,000units/hour. INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Wockhardt brand is supplied as a 400mg in 4ml solution. No further dilution needed for slow IV bolus. COMMENTS Flush with N/S, G or G/S. Sodium content 2.41mmol/400mg vial. Usually continue the patient’s current oral dosage as repeated slow bolus injections. Alternatively continue total usual oral daily Epilim® brand: Reconstitute with dosage as a continuous IV infusion over 4ml diluent provided. 24 hours. Due to the product displacement For patient’s not previously treated with this produces a solution of sodium valproate a slow bolus of 400 – 95mg/ml. 800mg depending on patient’s weight (up to 10mg/kg) is given followed by Reconstitute as above then continuous infusion (Max. 2500mg per dilute with N/S or G to any suitable volume of at least 50ml day). Do not infuse with any other drugs. Reconstitute as above then dilute with N/S or G to any suitable volume of at least 50ml Streptase brand reconstitute all ECG and blood pressure monitoring sizes with 5ml N/S. Further required. dilute 1.5 MU dose in 501 MU= 1,500,000 units 200mlN/S, G or H. Flush with N/S. Dilute other doses in any Duration of infusion: 72 hours for DVT or suitable volume of N/S or G e.g. 24 hours for PE or 24-72 hours for arterial 50-250ml. thrombosis or 12 hours for central retinal thrombosis. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 176 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Streptomycin Deep IM injection Groups 1 (Unlicensed product – see page 7) and 2 Change the injection site each time. ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Refer to the Marsden Reconstitute the 1g vial with Manual for guidance on 2 -3ml W. IM injection. The concentration for IM injection should not exceed 500mg/ml The displacement volume is approximately 0.8ml (I) IV infusion Groups 1 into a and 2 peripheral or central venous line via a pump 30-60 minutes Subcuvia® See Immunoglobulin Human Normal Subgam® See Immunoglobulin Human Normal So if you dissolve the powder with 3.2ml W the solution produced will be 250mg/ml Reconstitute the 1g vial as above then draw up the required dose and add it to 100ml N/S. COMMENTS In the treatment of tuberculosis the usual dose for adults and children 1month to 18 years is 15mg/kg up to a maximum of 1000mg, given daily or three times a week. For the elderly and adults over 40 years of age or less than 50kg body weight give 500mg-750mg once daily or 750mg three times a week. Monitor serum levels, particularly in patients with renal impairment, and adjust dosage accordingly. The vial labelled for IM-only use may be reconstituted with W, diluted in 100ml N/S and infused over 30-60 minutes as described. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 177 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE ADMINISTER OVER Sugammadex Rapid IV bolus Group 1 Rapid injection within 10 seconds Approved use in this Trust: Immediate reversal of neuromuscular block by rocurronium when intubation and ventilation have failed. It will also be effective in a similar emergency situation to reverse vecuronium. INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Adult dose for immediate reversal of rocuronium block is 16mg/kg of undiluted 500mg in 5ml injection. 16mg/kg = 0.16ml/kg of the 500mg in 5ml injection COMMENTS If sugammadex is administered via the same infusion line that is also used for other medicinal products, flush before and after sugammadex administration with N/S. However, sugammadex can be injected into the intravenous line of a running infusion with the following intravenous solutions: N/S, G, H, and sodium chloride 0.45% and glucose 2.5%. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 178 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE ADMINISTER OVER Sulphadiazine (I) IV infusion. Infusion pump is required. Groups 1,2,3,4 and Minimum 30-60 minutes IV bolus Group - must only Suxamethonium 5 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Dilute dose with N/S to a maximum concentration of 50mg/1ml. Preferably dilute required dose to 500ml to 1 litre to reduce risk of crystallisation in the urine. Ready diluted COMMENTS Flush with N/S. Sodium content approximately 4mmol/1g. To reduce the risk of crystallisation in the urine a high fluid intake (2.5-3.5 litres in 24 hours) should be maintained with urinary output of not less than half that amount. In addition the urine should be rendered alkaline. Flush with N/S or G. be given by doctors proficient in advanced airway management. (C) IV infusion. Groups 1 and 2 Infusion pump is required. Synacthen® 2.5 - 4mg/minute Infuse as a 1mg/ml to 2mg/ml solution diluted in N/S or G. Infusion not usually recommended due to development of phase II neuromuscular block and likelihood of exceeding maximum dose. See Tetracosactide. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 179 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Tacrolimus (C) IV infusion. Give by mouth Infusion or enteral pump is feeding tube required. routes if at all possible. WHO MAY ADMINISTER GIVE OVER Groups Infuse daily 1,2,3,4 and dose in 48ml over 24 hours 5 (Pump set at 2ml/hour) INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Draw up the correct dose in a 1ml syringe (See table below). Transfer and dilute to 48ml with N/S or G in a 50ml Terumo or BD syringe. The final concentration should be between 4 and 100 micrograms/ml. Infuse through a PVC-free or PE-lined extension set. Oral to IV tacrolimus conversion chart Total oral dose of Approximately Volume of tacrolimus equivalent IV dose tacrolimus in 24 hours injection (5mg in 1ml) to over 24 hours draw up for further dilution 0.5mg 100micrograms 0.02ml 1mg 200micrograms 0.04ml 1.5mg 300micrograms 0.06ml 2mg 400micrograms 0.08ml 2.5mg 500micrograms 0.1ml 3mg 600micrograms 0.12ml 3.5mg 700micrograms 0.14ml 4mg 800micrograms 0.16ml 4.5mg 900micrograms 0.18ml 5mg 1mg 0.2ml Tazocin® COMMENTS Tacrolimus is adsorbed to PVC and must be infused though a PVC-free or PE-lined extension set (Torcross, Penrose and NICU stock these). Wear gloves when preparing the infusion Not Y-site compatible with ganciclovir or aciclovir. Flush with N/S or G. Oral to IV tacrolimus conversion chart (continued) Total oral dose of Approximately Volume of tacrolimus tacrolimus in 24 hours equivalent IV dose injection (5mg in 1ml) to draw over 24 hours up for further dilution 5.5mg 1.1mg 0.22ml 6mg 1.2mg 0.24ml 6.5mg 1.3mg 0.26ml 7mg 1.4mg 0.28ml 7.5mg 1.5mg 0.3ml 8mg 1.6mg 0.32ml 8.5mg 1.7mg 0.34ml 9mg 1.8mg 0.36ml 9.5mg 1.9mg 0.38ml 10mg 2mg 0.4ml See Pipercillin/Tazobactam Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 180 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY ADMINISTER INSTRUCTION FOR DILUTION AND GIVE OVER SUITABLE DILUENT (I) IV infusion. via Groups 1 hour Reconstitute the 200mg vial with 4ml W. Swirl pump gently to dissolve the powder (Avoid shaking). 1,2,3,4 & 5 This will produce a 50mg/ml solution. Tedizolid ▼ This product is being intensively monitored by the CHM and MHRA. Please report all suspected reactions (including nonserious ones) using a Yellow Card from the BNF Teicoplanin IV bolus Usual method. Refer to the Plymouth Healthnet For doses greater Clinical than 600mg, give Guidelines/Infection as an infusion Control for the use over 30 minutes – and current dosage see below. of gentamicin, teicoplanin and (I) IV infusion. via vancomycin. pump Groups 3 – 5 minutes 1,2,3,4 and for all doses. 5 Groups 1,2,3,4 & 5 IM injection of Groups doses up to 1,2,3,4 and 400mg possible 5 only when IV access cannot be established and after discussion with Microbiologist 30 minutes COMMENTS Flush with N/S. Tedizolid is a reversible non-selective inhibitor of Monoamine Oxidase (MAOI) and may theoretically enhance increases in Further dilute in 250ml N/S. Do not shake the blood pressure produced by bag. sympathomimetics (e.g. dopamine, noradrenaline, adrenaline). Theoretically it may cause serotonin syndrome with serotonin re-uptake inhibitors (SSRIs). Incompatible with Hartmann’s and solutions containing calcium or magnesium. Slowly reconstitute each 200mg or 400mg vial Flush with N/S. with the 3.2ml of W provided. Roll the vial Sodium content less than 0.5mmol/vial gently until the powder has completely (200mg and 400mg). dissolved. Take care to avoid formation of foam. Incompatibile with aminoglycosides (eg. If it does foam, leave the vial to settle for 15 gentamicin). minutes until the foam subsides. Reconstituted Teicoplanin solutions will precipitate when in this manner you will be able to extract 200mg they come into contact with gentamicin – in 3ml from the 200mg vial and 400mg in 3ml flush the catheter well with N/S between from the 400mg vial. giving these two antibiotics. Reconstitute as above then dilute the required dose further with N/S, G, G/S or H (e.g. 50ml or 100ml). Reconstitute as above. Refer to the Marsden Manual for guidance on IM injection. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 181 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Temocillin Slow IV bolus WHO MAY ADMINISTER INSTRUCTION FOR DILUTION AND COMMENTS GIVE OVER SUITABLE DILUENT Temocillin is a penicillin – check patient’s allergy status before administration Groups 3 – 4minutes 1,2,3,4 and 5 (I) IV infusion Infusion pump is required. Groups IM injection Groups 1,2,3,4 and 5 1,2,3,4 and 5 30-40minutes Reconstitute each 1g with 10ml W and Incompatible with aminoglycosides e.g. shake vigorously. The final volume is gentamicin, tobramycin & amikacin – if 10.7ml (i.e. displacement volume is 0.7ml) administering down the same IV line, flush Reconstitute as above then add the dose with N/S between the temocillin and the aminoglycoside. to 100ml N/S. Reconstitute each 1g with 2ml W and Refer to the Marsden Manual for guidance on IM injection. shake vigorously. The final volume is 2.7ml (i.e. displacement volume is 0.7ml). If pain is experienced at the site of IM injection each 1g can be reconstituted with 2ml of lidocaine 0.5% or 1% injection instead of W. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 182 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Tenecteplase IV bolus Groups ADMINISTER OVER About 10 seconds 1and 2 Follow the protocol for the treatment of Acute Myocardial Infarction (See Plymouth Healthnet Clinical Guidelines) INSTRUCTION FOR DILUTION AND SUITABLE DILUENT 1) Remove the flip-off cap from the vial. 2) Remove the tip-cap from the syringe. Then immediately screw the pre-filled syringe onto the vial adapter and penetrate the vial stopper in the middle with the spike of the vial adapter. 3) Add the water for injections into the vial by pushing the syringe plunger down slowly to avoid foaming. 4) Reconstitute by swirling gently. 5) The reconstituted preparation results in a colourless to pale yellow, clear solution. Only clear solution without particles should be used. 6) Directly before the solution will be administered, invert the vial with the syringe still attached, so that the syringe is below the vial. 7) Transfer the appropriate volume of reconstituted solution of Metalyse into the syringe, based on the patient's weight. 8) Disconnect the syringe from the vial adapter. 9) Alternatively the reconstitution can be performed with the included needle. Do not inject into a line containing glucose. Compatible with N/S Patient Weight Vial size to pick Reconstitute with Dose the W provided Volume to give <60kg 40mg 8ml 30mg 6ml >60kg to <70kg 40mg 8ml 35mg 7ml >70kg to <80kg 40mg 8ml 40mg 8ml >80kg to <90kg 50mg 10ml 45mg 9ml >90kg 10ml 50mg 10ml 50mg Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 183 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Terbutaline SC injection IM injection WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Refer to the Marsden Manual for Groups guidance on SC injection. 1,2,3,4 and 5 Groups Refer to the Marsden Manual for guidance on IM injection. 1,2,3,4 and 5 Slow IV bolus Groups Suggestion: 3 – 5 1,2,3,4 and 5 minutes (C) IV infusion for Adult dosage: Groups bronchodilation via 1,2,3,4 and 5 30 – 60ml/hour for 8 a volumetric pump – 10 hours (C) IV infusion for Groups premature labour 1,2,3,4 and 5 via syringe pump. (Recommended method to avoid fluid overload) SC and IM injection are usually preferable to slow IV bolus, but if slow IV bolus is necessary monitor the patient’s pulse. Dilute 3 – 5ml (1.5 – 2.5mg) of terbutaline injection in 500ml G, N/S or G/S. Initially 3ml/hour Dilute 10ml (5mg) of terbutaline (5microgram/minute) injection to 50ml with G. for 20 minutes. Titrate dosage in increments of 1.5ml/hour (2.5microgram/minut e) (C) IV infusion for Initially 30ml/hour Dilute 10ml (5mg) of terbutaline Groups premature labour (5microgram/minute) injection to 500ml with G (remove 1,2,3,4 and 5 via volumetric pump. 10ml G from the bag first). for 20 minutes. Titrate dosage in increments of 15ml/hour (2.5microgram/minut e) SC infusion treating brittle asthma Groups COMMENTS Typical dose range: 1,2,3,4 and 5 5 – 15mg/24 hours Can be infused undiluted or diluted with N/S to the required volume. Titrate the hourly rate with reference to suppression of contractions, increase in pulse rate and changes in blood pressure, which are limiting factors. These parameters should be carefully monitored during treatment. A maternal heart rate of more than 135 beats/min should be avoided. In order to minimise the risk of hypotension associated with tocolytic therapy, special care should be taken to avoid caval compression by keeping the patient in the left or right lateral positions throughout the infusion. Infusion via a syringe pump is preferable to keep the volume of fluid administered to a minimum and to avoid maternal pulmonary oedema. The recommended diluent in premature labour is G. If it is necessary to use N/S monitor for maternal pulmonary oedema. SC infusion of terbutaline is unlicensed – see page 7 Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 184 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Terlipressin Acetate IV bolus WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Suggestion: Each 1mg Variquel® solution: Groups Ready diluted (1mg in 5ml) 1,2,3,4 and 5 over 1 minute Variquel® powder: Slowly add the entire contents of the solvent ampoule (5ml) to the powder vial and roll the vial gently until the powder is completely dissolved. This may be further diluted to 10 ml with N/S if required. Glypressin®: Ready diluted (1mg in 8.5ml) 1.3micrograms/kg/hour For Variquel®: =0.065ml/kg/hour of a Either reconstitute one 1mg powder 1mg in 50ml G dilution. vial as above, or take one ready diluted 1mg in 5ml vial, and dilute the contents (Infusion rate may be further to 50ml with G. titrated to effect at the discretion of the For Glypressin® brand: consultant intensivist) Dilute the contents of a 1mg ampoule further to 50ml with G. (C) infusion in Groups 1 Critical Care and 2 areas only via central IV line. (Preceded by an IV bolus of 0.5mg or 1mg at the discretion of the consultant intensivist) Tetracosactide IV bolus Suggestion: Give over Ready diluted. Groups (Synacthen®) 1,2,3,4 and 5 30 to 60 seconds Terlipressin to treat septic shock in critical care areas only, when vasopressin is unavailable IM injection Groups Inject deep into the 1,2,3,4 and 5 deltoid muscle COMMENTS Monitor blood pressure, serum sodium and potassium and fluid balance. Flush with N/S. This is an unlicensed regimen (see page 7) to reduce noradrenaline requirements in patients with septic shock based on the following reference: http://www.biomedcentral.com/content/pdf/cc 7990.pdf N/S is not a suitable diluent for terlipressin infusion. The suggested expiry for terlipressin in G infusion is 12 hours after preparation. Flush with N/S. Keep patient under observation for 30 minutes after the injection – hypersensitivity reactions are possible. The Planned Investigation Unit (PIU) have copies of the “Short Synacthen test” protocol. Refer to the Marsden Manual for guidance on IM injection. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 185 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Thiopental (Thiopentone) IV bolus Group 1 ADMINISTER OVER INSTRUCTION FOR DILUTION AND COMMENTS SUITABLE DILUENT Anaesthesia – Reconstitute 500mg vial with 20ml W Flush with N/S. induction: to produce a 2.5% (25mg/ml) solution. Check for haze or precipitation before administering. 100 –150mg over 10Extravasation causes local tissue necrosis 15 seconds Longer in and severe pain. This can be relieved by the elderly or application of an ice pack and local injection debilitated) repeated of hydrocortisone. after 1 minute if necessary. The reconstituted solution should be Control of discarded after 7 hours. convulsions: 75 –125mg over 3-5 minutes Lowering raised intracranial pressure: 1.5 –3mg/kg over 35 minutes. Repeat as necessary. (C) infusion Groups 1 via a central and 2* IV line Pump is required. For the management of refractory intracranial hypertension or Status Epilepticus, refer to the appropriate critical care protocol. Reconstitute three 500mg vials, each with 20ml W, making an infusion of 1500mg in 60ml (2.5% solution). (C) IV infusion is not a licensed method of administration of thiopentone (See page 126) Sodium content: 2.31mmol/500mg In intensive care areas or Theatres Use the prepared solution within 7 hours. only, the 2.5% (25mg/ml) solution may For the management of refractory be infused without further dilution intracranial hypertension or Status through a central line (local practice). Epilepticus, refer to the appropriate critical care protocol. *Group 2 nurses may only administer prescribed additional boluses of thiopental to ventilated patients in level 3 critical care. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 186 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Ticarcillin with clavulanic acid Tigecycline See Timentin® WHO MAY GIVE ADMINISTER OVER (I) IV infusion 30 – 60 minutes Groups Infusion pump is 1,2,3,4 and 5 May only be initiated required. on the advice of a consultant microbiologist ▼ This product is being intensively monitored by the CHM and MHRA. Please report all suspected reactions (including nonserious ones) using a Yellow Card from the BNF. INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Reconstitute the powder in the vial with 5.3ml N/S or G to make a 10mg/ml solution. Gently swirl to dissolve the powder. Then withdraw 5ml (50mg) from the vial and add to a 100ml bag of N/S or G. For the 100mg dose reconstitute two vials as above and add 10ml to a 100ml bag of N/S or G. Flush with N/S or G. Tigecycline in N/S is compatible at a YSite with dobutamine, dopamine, gentamicin, lidocaine,morphine, potassium chloride, propofol, ranitidine and Hartmann’s The solution should be inspected for the presence of particulate matter or green or black discolouration before use. Tigecycline should be yellow/orange in colour once reconstituted, if it is not, it should be discarded. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 187 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Timentin® Tinzaparin 2,500units 3,500units 4,500units Pre-filled syringes Tinzaparin 40,000units in 2ml Multidose vial (Non-Formulary) WHO MAY ADMINISTER INSTRUCTION FOR DILUTION AND COMMENTS GIVE OVER SUITABLE DILUENT Timentin contains a penicillin – Check patient’s allergy status before administration (I) IV infusion 30-40 minutes Reconstitute the 3.2g vial with 10ml W Incompatible with gentamicin and other Groups Infusion pump is 1,2,3,4 and 5 to form a pale straw-coloured solution. aminoglycosides. Each 3.2g of Timentin® contains required. Heat is released when the powder dissolves. Further dilute 3.2g with 100 - approximately 15.9mmol of sodium. Do not administer Timentin® by IV bolus 150ml G. or IM injection. Displacement value: 2.2ml for 3.2g of Flush with N/S. Timentin® so reconstitute 3.2g vial with 7.8ml W to get 3.2g in 10ml. Follow the PHNT guidelines for the use Injection into the Groups No further dilution required. of tinzaparin (sodium) for preventing arterial limb of 1,2 and 8 clotting in the haemodialysis circuit. the dialyser at the start of (Firstly, prime the circuit with 1 litre N/S). haemodialysis SC injection Groups 1,2,3,4 and 5 Refer to the Marsden Manual for guidance on SC injection. Tinzaparin must not be administered by intramuscular injection due to the risk of haematoma. Do not administer intravenously. Discard the vial 14 days after first use. Record the date of first use on the vial. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 188 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY ADMINISTER INSTRUCTION FOR DILUTION COMMENTS GIVE OVER AND SUITABLE DILUENT Tirofiban Loading dose Groups See below for Withdraw 50ml from a 250ml bag of Intravenous infusion of unfractionated heparin (5,000unit IV followed by indicationN/S or G and replace with 50ml of bolus followed by IV infusion at initial rate of 1,000units per 1,2,3,4 and specific infusion Tirofiban solution to make a hour: target APTTR approximately 2) should be (C) IV infusion 5 rates. concentration of 50 micrograms/ml. administered concurrently with Tirofiban and may be via Infusion Mix well before use. infused through the same catheter/Venflon as the Tirofiban. pump For patients diagnosed with NSTE-ACS and managed with an invasive For NSTE-ACS patients managed with an early invasive strategy and not strategy undergoing angiography within 4 hours after the diagnosis, planned to undergo angiography for at least 4 hours and up to 48 hours after tirofiban is given IV initially by 25 microgram/kg bolus dose given over 3 diagnosis, tirofiban is given IV at an initial infusion rate of 0.4 microgram/kg/min minutes initiated at the start of PCI followed by a continuous infusion of 0.15 for 30 minutes. At the end of the initial infusion, tirofiban is continued at a microgram/kg/min for 18-24 hours and up to 48 hours. maintenance infusion rate of 0.1 microgram/kg/min. When administering the bolus dose, always pre-set the infusion pump with the When administering the loading infusion, always pre-set the infusion pump with the total bolus volume to be administered total loading infusion volume to be administered. Patient weight(kg) Bolus (ml) 3 minute bolus infusion rate (ml/hour) Maintenance infusion rate (ml/hour) Patient weight(kg) 30 minute loading infusion (ml) 30 minute loading infusion rate (ml/hour) Maintenance infusion rate (ml/hour) 30 – 37 38 – 45 46 – 54 55 – 62 63 – 70 71 – 79 80 – 87 88 – 95 96 – 104 105 – 112 113 – 120 121 – 128 129 – 137 138 – 145 146 – 153 17 21 25 29 33 38 42 46 50 54 58 62 67 71 75 340 420 500 580 660 760 840 920 1000 1080 1160 1240 1340 1420 1500 6 7 9 11 12 14 15 16 18 20 21 22 24 25 27 30 – 37 38 – 45 46 – 54 55 – 62 63 – 70 71 – 79 80 – 87 88 – 95 96 – 104 105 – 112 113 – 120 121 – 128 129 – 137 138 – 145 146 – 153 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 16 20 24 28 32 36 40 44 48 52 56 60 64 68 72 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 In patients with an eGFR<30ml/min reduce the dosage by 50% In patients with an eGFR<30ml/min reduce the dosage by 50% Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 189 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Tobramycin IV bolus Groups ADMINISTER OVER 3 – 5 minutes 1,2,3,4 and 5 (I) IV infusion for Groups 30 minutes once daily dosing 1,2,3,4 and 5 in cystic fibrosis via pump IM injection Groups 1,2,3,4 and 5 TPN Tramadol See Parenteral Nutrition Staff prescribing, administering and/or screening prescriptions for opioid medications should be familiar with the PHNT Policy for Reducing Errors with Opioid Medicines in Adults using the following link: http://staffnet.plymouth.nhs.uk/Portals/1/Documents/Trust%20Documents/Medicines%20Management/Policy%20for%20Reducing%20Dosing %20Errors%20with%20Opioid%20Medicines%20in%20Adults.pdf?timestamp=1443106367868 IV bolus Slowly over 2 – 3 Undiluted Maximum total IV/IM dose in 24 hours is 600mg Groups IV infusion is incompatible with diazepam, 1,2,3,4 and 5 minutes (I) IV infusion via Groups 12 – 24mg/hour Dilute 200mg tramadol in 500ml N/S, diclofenac, indometacin, midazolam and piroxicam. pump 1,2,3,4 and 5 (=30 – 60ml/hour) G or H IM injection Groups Refer to the Marsden Manual for guidance on IM injection. 1,2,3,4 and 5 Tocilizumab (I) IV infusion Infusion pump is required. INSTRUCTION FOR DILUTION AND COMMENTS SUITABLE DILUENT Flush with N/S. N.B. Current recommended dose of 10mg/kg once daily in Cystic Fibrosis patients exceeds the dose 10mg/kg dose in Cystic Fibrosis diluted to 50ml or 100ml with N/S or G. stated in the package insert. Maximum once daily dose in Cystic Fibrosis is 660mg with trough levels measured before the 2nd and 8th doses (Target trough level <1mg/L. Modify Refer to the Marsden Manual for dose interval if trough level >2mg/L. guidance on IM injection. Groups 1,2,3,4 and 5 1 hour Dilute the prescribed dose of tocilizumab to 100ml with N/S. First remove a volume of N/S from the bag equal to the volume of tocilizumab being diluted. Mix by gently inverting the bag to avoid foaming. Bristol Royal Chidrens’ Hospital Infusion Regime: 10 ml/ hour for 15 minutes followed by 130 ml/hour to complete dosing over 1 hour Check TPR & BP prior to commencing the infusion every 30 minutes during the infusion. On completion of the infusion flush through the giving set with 20 ml of 0.9% saline ensuring all the drug has been given. Monitor vital signs every 30 minutes for 2 hours. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 190 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY ADMINISTER OVER GIVE INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Tranexamic acid IV bolus Groups Can be diluted with any convenient volume Flush with N/S or G. of N/S or G (e.g. 20-50ml for a bolus or more for an infusion) or given undiluted. Trastuzumab (Herceptin®) (C) IV infusion via pump (I) IV infusion Infusion pump is required. SC Injection 1,2,3,4 & 5 Groups 25-50mg/kg/24 hours 1,2,3,4 & 5 Groups 1 Loading dose over 90 Infusion to be prepared by Pharmacy. minutes. If the initial Telephone ext. 31083. Doctor to prescribe and 2 loading dose was well dose diluted with 250ml N/S. tolerated, the subsequent doses can be administered over 30 minutes Groups 1 Slow SC injection and 2 Tri-iodothyronine 100mg/minute over 2-5 minutes Draw up the 600mg in 5ml solution from the vial. COMMENTS Patients should be observed for at least six hours after the start of the first infusion and for two hours after the start of the subsequent infusions for symptoms like fever and chills or other infusion-related symptoms. Do not dilute with glucose solutions since these cause aggregation of the protein. The injection site should be alternated between the left and right thigh. New injections should be given at least 2.5 cm from the old site and never into areas where the skin is red, bruised, tender, or hard. Patients should be observed for six hours after the first injection and for two hours after subsequent injections for signs or symptoms of administrationrelated reactions. See Liothyronine Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 191 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE Triptorelin (Decapeptyl®) IM injection Groups 1,2,3,4 and 5 ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Draw up the mannitol diluent provided This is a single-use vial into the syringe provided using one of the injection needles and inject in to Refer to the Marsden Manual for the vial containing the powder. Gently guidance on IM injection. swirl the vial until a uniform suspension is formed, then draw the mixture back into the syringe without inverting the vial. The injection needle should then be changed and the second needle used to administer the injection. As the product is a suspension, the injection should be administered immediately after reconstitution to prevent sedimentation. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 192 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Tysabri® Urokinase See natalizumab Lock for unblocking Groups midlines and PICC 1,2 and 8 lines (Adults) WHO MAY ADMINISTER GIVE OVER Catheter lock for unblocking haemodialysis CVC (Adults) Groups Inter-dialysis infusion via the haemodialysis CVC (Adults) Groups Intraperitoneal catheter lock for unblocking the catheter. Groups 1and 2 1and 2 1and 2 Retain in the line for 1-2 hours (or longer) INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Reconstitute one 10,000unit vial of urokinase with 3ml of N/S. Instil 1.5ml (5,000units) of the reconstituted solution into each lumen of the catheter. If the lumen is completely blocked do not force urokinase into the lumen.Refer to the full PHNT guidelines: http://www.plymouthhospitals.nhs.uk/ourservices/clinic aldepartments/Pages/VascularAccessTeam.aspx Reconstitute urokinase 25,000unit vial with N/S in a volume equal to the priming volume of both catheter lumen plus an additional 0.2mls (e.g. ‘A’ lumen = 1.7, ‘V’ lumen = 1.9, therefore 1.7 + 1.9 + 0.2 = 3.8 ml of N/S). Draw up solution into two syringes: one equal to arterial lumen volume + 0.1ml and one equal to venous lumen + 0.1ml (e.g. ‘A’ lumen syringe = 1.7 + 0.1 = 0.8 ml; ‘V’ lumen syringe = 1.9 + 0.1 = 2ml) All staff must be aware that any connection/disconnection to a haemodialysis CVC must be performed using aseptic technique o Flush each lumen with 10ml of N/S o Inject 12,500unit urokinase into each lumen to the priming volume o Positively lock the lumen and place the red obdurate, then wait for 30 minutes o Aspirate 5mls from each lumen and flush with 10-20ml of N/S if flows have restored Commence dialysis treatment The decision to use an inter-dialysis infusion of urokinase must be agreed beforehand with one of the Trust consultant nephrologists each time it is used, and after assessment of any increased bleeding risk. Reconstitute two 100,000unit vials of urokinase each with 2ml N/S and add both vials to 100ml N/S (200,000unit urokinase in 100ml N/S). Draw up the urokinase solution into two 50ml luer-lock syringes. Attach the 50ml syringes to the lumens of the dialysis CVC. Using a syringe driver, infuse a 50ml syringe containing the urokinase solution (100,000iu in 50ml N/S) down each lumen over 90 minutes (34ml/hour). When the infusion is complete, flush each lumen with 10–20ml N/S to establish blood-flow. Commence haemodialysis. Retain in Dilute 12,500 international units with 5ml Follow the Renal Services Directorate Peritoneal Dialysis Protocols catheter for 2 N/S. hours Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 193 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Vancomycin (I) IV infusion preferred method. Infusion pump is required. Refer to the Plymouth Healthnet Clinical Guidelines/Infection Control for the use and current dosage of gentamicin, teicoplanin and vancomycin. WHO MAY ADMINISTER OVER GIVE Groups Adults: 500mg over 1 1,2,3,4 and hour. Doses over 500mg maximum rate 5 10mg/minute. (C) IV infusion. Groups 24 hours Infusion pump 1,2,3,4 and is required. 5 Example IV calculations Intrathecal Injection COMMENTS Reconstitute 1g vial with 20ml W and 500mg vial with 10ml W. Dilute 500mg with at least 100ml N/S or G. Dilute 750mg with at least 150ml N/S or G. Dilute 1g with at least 200ml N/S or G. Dilute 1.5g with at least 300ml N/S or G. Dilute 2g with at least 400ml N/S or G. Flush with N/S or G. In practice 1g in 100ml may be used in fluid restricted patients; but the use of such high concentrations may increase the risk of infusion related events when administered via a peripheral vein. Note that the current recommended target trough level is higher than that in the SPC and is therefore unlicensed (See page 7). 500mg vancomycin (in 10ml W) added to a 100ml bag N/S = 110ml over 1 hour 750mg vancomycin (in 15ml W) added to a 250ml bag N/S = 265ml over 1½ hours 1g vancomycin (in 20ml W) added to a 250ml bag N/S = 270ml over 2 hours 1.5g vancomycin (in 30ml W) added to a 500ml bag N/S = 530ml over 2½ hours 2g vancomycin (in 40ml W) added to a 500ml bag N/S = 540ml over 3⅓ hours (200 minutes) Group 1 Intraperitoneal Groups 1 and 2 INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Set pump rate at : 110ml/hour 177ml/hour 135ml/hour 212ml/hour 162ml/hour Refer to the Neurosurgical Antibiotic Therapy Guidelines for Adults on Plymouth Healthnet (Under Clinical Guidelines) Follow the Renal Services Directorate Peritoneal Dialysis Peritonitis Protocol Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 194 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD Vasopressin =Argipressin (I) IV infusion. Groups 1 Infusion and 2 pump is required. Administer via a central IV line. For use in Critical Care to reduce noradrenaline requirements in patients with refractory septic shock. Regent and Sandoz brands must be kept at room temperature WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Dosage for use in Dilute 20 units to 50ml with G. critical care for refractory septic shock: 0.6–2.4 units/hour (= 1.5 -6ml/hour using 20 units/50ml dilution) COMMENTS Flush with G. Note that Regent and Sandoz brand vials are only labelled for IM and SC use. However, they are also suitable for IV use. Regent and Sandoz brands are unlicensed in the UK (see page 7). Note that Sandoz brand vials are multidose 40units in 2ml. Part-used vials should be stored at room temperature and discarded 28 days after initial use. (Unlicensed indication- see page 7). Pitressin ® - keep in the fridge Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 195 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE ADMINISTER OVER INSTRUCTION FOR DILUTION AND SUITABLE DILUENT COMMENTS Vecuronium IV bolus Group 1– must See Data Sheet Flush with N/S or G. The reconstituted solution can be injected or infused in to the line of a running infusion of Hartmann’s. If the patient is ventilated IV bolus can be administered by Group 2 staff. only be given by doctors proficient in advanced airway management. Also see Comments. The 10mg vial can be reconstituted with 5ml W to produce 2mg/ml solution. Alternatively reconstitute the 10mg vial with 10ml W, G, N/S or H to produce a 1mg/ml solution. The reconstituted solution can be given undiluted or diluted further with N/S or G to a maximum dilution of 4mg/100ml. Bolus of 40-100 (I) IV infusion. Groups 1 and 2 micrograms/kg Infusion followed by 48 - 84 pump is micrograms/kg/hour. required. Using a 2mg/ml dilution e.g. 100mg in 50ml 48 – 84micrograms/kg/hour = 0.024 – 0.042ml/kg/hour Using a 1mg/ml dilution e.g. 100mg in 100ml 48 – 84micrograms/kg/hour = 0.048 – 0.084ml/kg/hour Allow the vial to warm to room temperature All patients should be observed 30 minutes Vedolizumab (I) IV infusion. Groups 1 and 2 then reconstitute with 4.8 ml of W. Direct continuously during each infusion. For Infusion ▼ This product the stream of liquid to the wall of the vial to the first two infusions, they should also pump is is being avoid excessive foaming. Gently swirl the be observed for approximately two hours required. intensively vial for at least 15 seconds. Do not following completion of the infusion for monitored by vigorously shake or invert. Let the vial sit the CHM and for up to 20 minutes to allow for any foam signs and symptoms of acute hypersensitivity reactions. For all MHRA. Please to settle; the vial can be swirled and inspected for dissolution during this time. If subsequent infusions, patients should be report all observed for approximately one hour not fully dissolved after 20 minutes, allow suspected following completion of the infusion. another 10 minutes for dissolution. reactions Prior to withdrawing reconstituted solution Do not infuse down the same line as any (including nonfrom vial, gently invert vial 3 times. other drugs. serious ones) Withdraw 5 ml (300 mg) of reconstituted using a Yellow solution and add to 250ml N/S. Gently mix Card from the the infusion bag. BNF. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 196 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE ADMINISTER OVER Verapamil IV bolus Emergency use. Group 1 or 2 minutes (elderly patients minimum 3 minutes) Group 2 Vigam® See Immunoglobulin Human Normal Vitamins B and C High Potency IV injection Vitamin K Voriconazole See Pabrinex See phytomenadione (I) IV infusion. groups Infusion pump is 1,2,3,4 and 5 required. Over 1-2 hours. Maximum rate 3mg/kg/hour. Xiapex® See Collagenase Clostridium histolyticum X-ray Contrast IV bolus According to X-ray Groups Medium, Department protocol. 1 and 6 Non-ionic, tri-iodinated X-ray Contrast IV bolus According to X-ray Groups Medium, Department protocol 1and 6 Gadolinium based. Zanamivir (I) IV infusion groups 1,2,3,4 and 5 (Unlicensed product – see page 7) Approximately 30 minutes INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Ready diluted. COMMENTS ECG and blood pressure monitoring necessary. Flush with N/S. Sodium content 0.15mmol/ml. Add 19ml W to each 200mg vial. Do not infuse concomitantly with other Resulting concentration is 200mg drug solutions through the same in 20ml (Displacement 1ml/200mg lumen/Venflon. vial). Dilute the required dose with N/S, G, H or 0.45% saline to a final concentration of 0.5 to 5mg/ml. Do not dilute. Monitor for possible anaphylaxis or other allergic reactions. Resuscitation equipment should be immediately available. Do not dilute Monitor for possible anaphylaxis or other allergic reactions. Resuscitation equipment should be immediately available. Either give undiluted (10mg/ml), or Do not infuse down the same line/lumen dilute with N/S to a concentration as other IV medications, or glucose, or not less than 200 micrograms/ml. electrolytes other than N/S. Flush with N/S. Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 197 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 DRUG METHOD WHO MAY GIVE ADMINISTER OVER Zidovudine (I) IV infusion groups 1 hour 1,2,3,4 and 5 Zoledronic acid (Aclasta® 5mg in 100ml bags) (I) IV infusion Zoledronic acid (Zometa® 4mg in 5ml vials) (I) IV infusion 1,2,3,4,5 and 8 groups 1,2,3,4,5 and 8 GFR > 60 groups INSTRUCTION FOR DILUTION AND SUITABLE DILUENT Dilute the prescribed dose to 2mg/ml or 4mg/ml with G – see comments for examples. Infuse all doses over at Ready diluted. least 15 minutes. Set the pump rate at a maximum of 400ml/hour Infuse all doses over at Draw up the prescribed dose least 15 minutes. (dependent on renal function – see below) and add to 100ml N/S or G. When diluted with 100ml N/S set the pump rate at a maximum of 400ml/hour Dosing according to renal function 4mg dose COMMENTS Example: For a 63mg dose you would draw up 6.3ml of zidovudine injection(10mg/ml) and dilute to 31.5ml with G in a 50ml syringe to make a final concentration of 2mg/ml, and set the pump rate at 31.5ml/hour. Example for doses > 100mg: For a 130mg dose, you would draw up 13ml zidovudine injection(10mg/ml) and dilute to 32.5ml with G in a 50ml syringe to make a final concentration of 4mg/ml, and set the pump rate at 32.5ml/hour. Do not give by IM injection. Do not mix with magnesium or calcium containing solutions such as Hartmann’s. Do not mix with magnesium or calcium containing solutions such as Hartmann’s. For the treatment of tumour-induced hypercalcaemia ensure the patient is well hydrated before and after administration of zoledronic acid. Draw up 5ml from the vial GFR 50 – 60 3.5mg dose Draw up 4.4ml from the vial GFR 40 – 49 3.3mg dose Draw up 4.1ml from the vial GFR 30 -39 3mg dose Draw up 3.8ml from the vial Intravenous fluids and drug solutions prepared in clinical areas must be changed every 24 hours unless otherwise specified in the drug monograph. 198 Unless described in the monograph as “Multidose”, ALL injectable products, including bags of sodium chloride and glucose must be treated as single-use-only and discarded immediately after use. For additional paediatric and neonatal information refer to the Bristol Royal Hospital for Children guidelines http://nww.swretrieval.nhs.uk/DI_ALL.htm - for drug monographs click on “Intravenous Drug Administration Guide”), current BNF For children which is accessible via https://www.medicinescomplete.com/mc/ or the Neonatal Formulary. For more detailed information refer to the current BNF which is accessible via https://www.medicinescomplete.com/mc/ . For full details of the licensed indications, dosage, contraindications and side effects refer to www.medicines.org.uk Procedures for Administering Injectable Drugs, Pharmacy Department, Derriford Hospital, Version 11, December 2015. Version 11.4 (Interim amendmends & additions) May 2016 199 200 Protocol for subcutaneous morphine for acute pain Rationale Intermittent subcutaneous administration of morphine is an alternative to repeated intramuscular or intravenous injections for the management of acute severe pain. An indwelling subcutaneous cannula can reduce procedural pain and patient anxiety regarding repeated im injections. It can also reduce needle stick injuries associated with im analgesia. The cost of disposable needles is also reduced. Use where patient is unable to take oral medication and im or iv morphine boluses would have been previously considered. Do not give opioids via any other route when subcutaneous protocol in use. Long term oral or patch opioid use is an exception to this rule. This protocol is intended for use in surgical inpatients with acute pain. Do not use when peripheral perfusion is impaired such as shock, gross oedema or hypothermia. Equipment required 1. Sub-cutaneous cannula eg: BD Saf-T-Intima 2. Sharps bin 3. Appropriate skin cleaning device (Chloraprep) 4. Appropriate dressing (eg. C-View 6cm x 7cm) Procedure 1. Choose site for insertion (eg: upper arm). 2. Clean skin and allow to air dry 3. Pinch a fold of skin and subcutaneous tissue and insert cannula at base of fold 4. Dispose of sharps carefully 5. Cover insertion site with a clear dressing, label with date and time of insertion 6. Document date, time and place of cannula insertion in the medical or nursing notes. Prescription Please ensure that a specific dose is prescribed, not a range. Dosing frequency should be 2 hourly when required. Dose is age dependant. Morphine should be avoided if eGFR <30mls/min. Ensure that there are no other contra-indications to morphine use. Discuss with ACT if eGFR < 30mls/min – it may be appropriate to use an alternative opioid. Age Dose 18-59 10-15mg 60-69 5-10mg 70-89 2.5-5mg 90+ 2.5mg A 0.5ml saline flush should also be prescribed. Administration 1. Check morphine prescription according to trust opioid prescribing policy 2. Draw up prescribed dose of morphine 3. Check insertion site prior to administration: a. Cannula must be re-sited if red, painful, inflamed or has been in situ for more than 72 hours 4. Use 10mg/ml morphine undiluted 5. Inject morphine slowly 6. Flush the cannula with 0.5ml normal saline after each dose of morphine 7. If pain score acceptable to patient and last dose was 4-6 hours ago, remove cannula and switch to oral analgesia if appropriate Observations after each injection of morphine At 15 minutes, 30 minutes, 60 minutes and 4 hourly thereafter Author: Dr Mark Rockett Lead Inpatient Pain Consultant for the Acute Care Team, 04/2014. Version 5.0 Review date: 04/2016 201 202 203 Emergency Department Adult Intravenous Morphine Guideline This guideline is to be used in conjunction with BNF & PHNT joint formulary & Trust acute pain analgesic ladder. No intravenous morphine to be given in minors. Always take into account age, weight and co-morbidities – use with extreme caution in renal impairment. Give 1/2 or 1/3 of below doses in elderly and frail. Consider non-pharmacological methods of analgesia – eg splintage, LA blocks. Actively seek out times and doses of prior (including pre-hospital) analgesia. Patients with high pain scores should be asked if they require further pain relief. Only prescribe if the patient says they do. Seek senior advice for non-responsive pain. Severe Pain = 8-10 Moderate Pain = 4-7 Mild Pain = 1-3 No Pain = 0 Prescribe multi-modal analgesia (paracetamol +/-NSAIDs) to be given simultaneously. Assess with pain score & consider IV morphine for moderate or severe pain. Prescribe IV morphine on STAT section of the drug chart 0.1mg/kg titrated to effect over 2-3 minutes but see above Reassess at 20 minutes with observations including RR, conscious level & pain score Repeat up to above dose as required but no sooner than 20 mins If a second dose is given in ED apply monitoring – minimum of pulse oximetry 204 Author: Dr Mark Rockett 2012 Protocol for subcutaneous ketamine for difficult to manage pain Rationale Ketamine is an anaesthetic agent with analgesic properties. A low dose ketamine infusion provides safe and effective analgesia. Ketamine is usually used together with an opioid to improve pain relief and reduce opioid side effects. At low doses Ketamine may cause sedation; however respiratory depression is minimal and psychotomimetic effects are uncommon. There is evidence to support that ketamine has an opioid sparing effect in postoperative pain and NMDA receptor antagonist drugs show preventive analgesic effects. Ketamine is also effective in treating acute neuropathic pain and in reducing hyperalgesia and the transition to persistent post surgical pain. Ketamine may reduce opioid tolerance in patients already on high dose strong opioids, and reverse opioid induced hyperalgesia. Indications Where pain is inadequately controlled by opioids alone When opioid tolerance has developed i.e. patient requiring increasing amounts of opioids To reduce opioid side effects e.g. respiratory depression, nausea Acute neuropathic pain Subcutaneous administration of ketamine is an alternative to intravenous infusion for the management of complex acute severe pain. Do not use the subcutaneous route when peripheral perfusion is impaired such as shock, gross oedema or hypothermia. Equipment required 5. Sub-cutaneous cannula eg: BD Saf-T-Intima 6. Sharps bin 7. Appropriate skin cleaning device (eg Chloraprep) 8. Appropriate dressing (eg. C-View 6cm x 7cm) Procedure 7. Choose site for insertion (eg: upper arm). 8. Clean skin and allow to air dry 9. Pinch a fold of skin and subcutaneous tissue and insert cannula at base of fold 10. Dispose of sharps carefully 11. Cover insertion site with a clear dressing, label with date and time of insertion 12. Document date, time and place of cannula insertion in the medical or nursing notes. General Management Nursing staff caring for patients with advanced analgesic systems must attend the mandatory training every two years. Prescriptions should only be altered by a member of the Acute Care Team Use only the CME Medical TPCA pumps labelled ‘Ketamine infusion’ with lockable covers 205 Patients should remain on oxygen as prescribed Patients may mobilise with support as required Anti-syphon and anti-reflux lines must be used The ketamine infusion line must be clearly labelled A dedicated venous line is preferable as this reduces the risk of the patient receiving boluses of ketamine Ketamine syringe driver keys should be kept with controlled drug keys N.B Any patient receiving opioids via an analgesic system are not permitted to leave the ward, unless for medical investigation, x-ray etc. Prescription Use the pre-printed prescription label (White) and ketamine information sheet. 5mg/kg ketamine made up to 50mls with normal saline using 50mg/ml ketamine solution (0.1mls/kg of solution). Maximum dose in syringe 500mg (10mg/ml). Add 1mg dexamethasone (0.3mls of 3.3mg/ml solution) to the syringe. The ketamine infusion should be started at 1ml/hr. This delivers 0.1mg/kg/hr. If necessary, increase the rate in 0.5ml/hr increments until either good analgesia is obtained or the patient begins to experience dysphoria. Psychotomimetic reactions increase in parallel with plasma concentration. Therefore do not give boluses or increase above 2mls/hr. If the patient does experience mild dysphoria, stop the infusion for 30 minutes and recommence at a lower rate. If the dysphoria is more severe or there are hallucinations, contact the Acute Care Team. Dexamethasone is added to reduce tissue irritation. At this dose (1mg in 50mls) it will not adversely affect blood glucose levels. As a general rule, ketamine infusions should be run for no more than 48 hours (lack of evidence of ongoing benefit), although this can be extended after discussion with the Acute Care Team. In addition to the ketamine infusion, all patients should receive regular paracetamol and NSAID (unless contra-indicated). You should aim for a pain score of ‘none’ or ‘mild’ on movement . Professional Accountability As a Registered nurse, midwife or specialised public health nurse, you must maintain your professional knowledge and every nurse must adhere to the Plymouth Hospitals NHS Trust protocols on management of a ketamine infusion, in addition to all other relevant Trust policies. Observations after commencing ketamine infusion Use the PCA observation chart and record standard PCA observations Standard observations one hourly for 4 hours, 2 hourly for 8 hours & 4 hourly thereafter. Additionally, please record the ketamine infusion rate, the syringe volume remaining and each syringe change. Also record psychotomimetic side effects on a scale of 0-2: 0 = None 1 = Dysphoria 2 = Hallucinations Converting from Ketamine infusion to oral analgesia Review the need for ketamine infusion daily. Ketamine infusions will usually be limited to 24-48 hours duration. Expect opioid requirements to fall from day-2 post operatively 206 Ensure the patient has received a recent dose of paracetamol, NSAID (if appropriate) and an opioid (codeine / oramorph) Switch ketamine infusion off If pain If pain scores unacceptable call the ACT with view to restarting the ketamine infusion Risk management: Action to be taken following clinical incidents with ketamine infusions If the incident involves a drug error take the following action: Identify original source of error and take appropriate action to prevent further risk to patient Monitor patient for adverse effects and perform observations every 5 minutes until medical review Contact Ward Doctor urgently and inform ACT immediately Complete Datix incident form as per Trust guidelines and follow appropriate procedure Please forward a copy of the Datix incident form to the Acute Care Team Level 4 If the incident involves equipment error or failure, in addition to the guidelines above take the following action: Follow the MEMS guidelines for Accidents / Incidents / Near Misses Involving Medical Equipment (MEMS Medical Equipment Users’ Guide) For any other incidents take the following action: Establish whether there could be any adverse effects to the patient and monitor accordingly Contact the Ward Doctor urgently and inform the ACT Complete incident form as per Trust guidelines and follow appropriate procedure Authors: Dr Mark Rockett Lead Inpatient Pain Consultant for the Acute Care Team and Dr Tim Wilson, 07/2016 Version 5 Review date: 07/2018 References The Electronic Medicines Compendium 2012 published by Datapharm Communications Ltd (http://www.medicines.org.uk/emc/) The Injectable Medicines Guide produced by the network of UK hospital pharmacists, published by the Pharmacy Dept. Charing Cross Hospital, London, and endorsed by the UK Medicines Information service (http://medusa.wales.nhs.uk/) The British National Formulary No.64 (September 2012) (http://bnf.org/bnf/bnf/current/) The British National Formulary for Children (2012-2013) (http://bnfc.org/bnfc/bnfc/current/ UK Resuscitation Council Anaphylaxis Algorithm (http://www.resus.org.uk/pages/anaalgo.pdf) 207 Appendix 1 Protocol for administering intramuscular adrenaline 1:1000 (1mg/ml) for treating anaphylaxis, when there is no prescription available Date Version September 2013 1 Purpose To instruct staff on how to correctly identify when a person is suffering an anaphylactic reaction and to treat the person correctly with intramuscular adrenaline, when there is no prescription for this medication Scope of this document Applies to all non-medical clinical staff working in any area with the skill and competence to assess a patient’s condition and administer intramuscular medication. Key Message Non-medical clinical staff working for or on behalf of Plymouth Hospitals NHS Trust may legally administer adrenaline injection to treat anaphylaxis without a prescription. They must do so in accordance with this protocol. Accountabilities Production Peter Gray, Senior Pharmacist Review and approval Medicines Utilization and Assurance Committee Ratification Medicines Utilization and Assurance Committee Dissemination Peter Gray, Senior Pharmacist 208 Links to other policies and procedures Pharmacy Documents: PHNT Medicines Management Policy Procedures For Administering Injectable Medicines Other Documents: Emergency Treatment of Anaphylactic Reactions- Guidelines For Healthcare Providers: Working Group of the Resuscitation Council (UK) 2008 Medicinal products for parenteral administration in an emergency. The Human Medicines Regulations 2012, Regulation 238, Schedule 19. Version History Version 1 Version 2 1.1 October 2013 December 2015 Last Approval Due for Review Version 2 December 2017 Adrenaline (1:1000) can legally be administered without a prescription for the purpose of treating anaphylaxis Medicines legislation restricts the administration of Prescription-Only injectable medicines. Unless self administered, they may only be administered by in accordance with a prescription. However, in the case of 1:1000 adrenaline there is an exemption to this restriction which means in an emergency, a suitably trained person (eg. nurse or ODP) is permitted to administer it by (intramuscular) injection for the purpose of treating anaphylaxis without a prescription or instruction from a doctor. 1.2 Persons who can be treated under this protocol Individuals displaying the signs and symptoms described below who are: Hospital in-patients Hospital out-patients attending out-patient or diagnostic departments Visitors or members of staff 1.3 Anaphylaxis Anaphylaxis is a severe, life-threatening, generalised or systemic hypersensitivity reaction. This is characterised by rapidly developing life-threatening airway and/or breathing and/or circulation problems usually associated with skin and mucosal changes. Administration of intramuscular (IM) adrenaline should be considered for individuals who show signs and symptoms of an anaphylactic reaction. Anaphylaxis is likely when all of the following three criteria are met: 1.4 Sudden onset and rapid progression of symptoms. Life-threatening airway and/or breathing and/or circulation problems. Skin and/or mucosal changes (flushing, urticaria, angioedema). Assessing the patient 209 The ABCDE approach to assess and treat a patient should be followed, as patients can have an Airway, Breathing or Circulation Problem or any combination which is life threatening. Airway Airway swelling, e.g. throat and tongue Hoarse voice, unable to speak Stridor Breathing Shortness of breath Wheeze Confusion caused by hypoxia Patient becoming tired Cyanosis – late sign Respiratory arrest Circulation Signs of shock, pale, clammy Increased pulse rate Low blood pressure, feeling faint, collapse Decreased conscious level or loss of consciousness Cardiac arrest The above Airway, Breathing and Circulation problems can all alter the patient’s neurological status (Disability problems) because of decreased brain perfusion. There may be confusion, agitation and loss of consciousness. Patients can also have gastro-intestinal symptoms (abdominal pain, incontinence, vomiting) Exposure The patient must be exposed ensuring dignity to observe for skin and/or mucosal changes. This is often the first feature present in over 80% of anaphylactic reactions. 1.5 They can be subtle or dramatic. There may be just skin, just mucosal, or both skin and mucosa changes. There may be erythema – a patchy, or generalised, red rash. There may be urticaria which can appear anywhere on the body. The weals may be pale, pink or red, and may look like nettle stings. They can be different shapes and sizes and are often surrounded by a red flare. They are usually itchy. Angioedema is similar to urticaria but involves swelling of deeper tissues, most commonly in the eyelids and lips, and sometimes in the mouth and throat. Explanation of treatment to the patient Prior to the administration of adrenaline the patient should receive an explanation that they are having an allergic reaction and that IM adrenaline is going to be administered to relieve the symptoms and help reverse the reaction. 1.6 Patient Consent Prior to the administration of the drug, consent should be obtained either from the patient, parent, guardian or person with parental responsibility. Verbal consent is acceptable in the emergency scenario. This should be documented in the patient’s medical records once the patient’s 210 condition is stable. If the patient, parent or guardian does not wish treatment to be given under this protocol they should be advised of the potential risks. If the patient is unable to give consent due to a life-threatening situation, or if parents or guardians are not present, adrenaline should be administered where treatment is judged to be in the best interests of the patient. Exclusions from treatment under this protocol 1.7 None 1.8 Contra-indications to administration of adrenaline to treat anaphylaxis There are no absolute contra-indications to the administration of adrenaline under this protocol. Immediate Treatment – Also refer to treatment algorithm on page 195 1.9 1.10 Reassure and explain the situation to the patient. Assess airway and breathing and identify signs and symptoms of anaphylaxis (see 2.1). Identify and discontinue trigger factors. Call for help, e.g. 999, a doctor, 2222 Clinical Emergency Team. Patients with airway or breathing problems may prefer to sit up as this will make breathing easier. Assess circulation (see Section 2). Laying the patient flat with or without leg elevation may be helpful for patients with hypotension. If the patient feels faint, do not sit or stand them up as this may cause cardiac arrest. NB. A sudden change to a more upright position may be dangerous due to the effect on blood flow to the heart. If the patient presents with signs of clinical shock and/or stridor, administer IM adrenaline 1:1000 as recommended, noting the time given and the response. Continue to observe the patient supporting and maintaining a clear airway, observing breathing. Continuous assessment of the patient is important using the ABCDE approach. Patients who are breathing and unconscious should be placed in the recovery position. Pregnant patients should lie on their left side to prevent caval compression. If the patient is not breathing or has no pulse, commence cardio pulmonary resuscitation (CPR) using current guidelines. Continue until: o More qualified help arrives o You become exhausted o Patient shows signs of recovery Source of Adrenaline Use ampoules of adrenaline 1:1000 (1mg/1ml). If these are not available, use any pre-filled autoinjector (eg. Epipen or Anapen) that the patient may be carrying. 1.11 Dosage of Adrenaline Dose for Adults: 500micrograms (0.5mL) of adrenaline 1:1000 (1mg/mL). Dose for Infants and Children: 211 Age Under 6 years 6 - 12 years Over 12 years Dose of Adrenaline 150 micrograms IM 300 micrograms IM 500 micrograms IM (300 micrograms IM if the patient is small or pre-pubertal) Volume of 1:1000 (1mg/mL) solution 0.15mL 0.3mL 0.5mL (0.3mL) Frequency The dose stated above can be repeated once, as necessary after 5 minutes if there is no improvement in the patient’s condition or on assessment of the patient’s blood pressure, pulse and respiratory function. 1.12 Adverse Effects Adverse effects are extremely rare with correct doses injected intramuscularly 1.13 Follow-Up Hospital in-patients require close observation on the ward (or Theatre/Recovery). They may need to be transferred to HDU depending on the severity of reaction and medical decision. Any affected hospital out-patients, staff or visitors, patients in the community or those attending clinics/health centres/lectures/training need to be transferred to the Emergency Department. 1.14 Documentation of all events and actions once the patient is stable For patients, document all events and actions in the medical notes. For affected members of staff, visitors or other persons, all events and actions must be documented on admission to the Emergency Department. Details recorded should include: Full details of the event Time course of the reaction Whether consent to treatment has been given All drugs and treatments administered, including details of dose(s) given Resuscitative measures Patient’s response to treatment Any previous adverse reactions Signature and printed name of person administering treatment under this protocol Date Statement that adrenaline was administered to treat suspected anaphylaxis without a prescription in accordance with the hospital protocol. If the anaphylactic reaction is considered to be drug-induced, the medical practitioner should consider completing a “Yellow Card” from the BNF and sending it to the MHRA or reporting the reaction via the MHRA website at http://yellowcard.mhra.gov.uk 1.15 References Emergency Treatment of Anaphylactic Reactions- Guidelines For Healthcare Providers: Working Group of the Resuscitation Council (UK) 2008 Medicinal products for parenteral administration in an emergency. The Human Medicines Regulations 2012, Regulation 238, Schedule 19. 212 1.16 Management of Anaphylaxis 213 214 For more information please contact the Resuscitation Department on 52851 Appendix 2 Choice of Infusion device 2.1 Introduction All individuals that operate infusion devices within the remit of their role have a responsibility to ensure that they are competent to operate the equipment in a safe and effective manner, seek advice and training where necessary and complete relevant documentation with their assessor in line with the Trusts Policy and Procedure document for the ‘Training of Plymouth Hospitals NHS Staff in the Use of Medical Devices.’ It is the responsibility of the person administering the drug to select the appropriate infusion pump for the therapy required. Alterations to the pump setting may only be made and recorded by a person entitled to administer intravenous drugs. The volume of fluid administered must be recorded on the fluid chart. All pumps must be checked 2 hourly throughout the infusion and details of the infusion should be recorded on the relevant infusion chart. Infusion Devices must always be operated and serviced in accordance with the Manufacturers operating instructions and the MEMS Medical Equipment Users’ Guide. Every area should maintain a library of user manuals for commonly used equipment, which may be kept in the Ward Equipment File. Manuals for commonly used infusion devices can be found on the Medical Devices Training webpage on TrustNet. The MEMS Medical Equipment Users Guide is available on the Trust documents drive. 2.2 Choice of Infusion device The choice of infusion device should be based upon the clinical application it is intended for, and the safety features incorporated within the device. Infusion devices may be grouped into the following categories: a. Volumetric pumps Pump of choice for medium and high flow rates, and large volume infusions. Pressure sensitivity of pump: Some pumps have selectable occlusion pressure alarm levels. Selecting low levels will help to prevent excessive delivery pressures and possible vein damage. Some may allow for the addition of piggyback or secondary infusions. The majority of volumetric pumps will perform satisfactorily at rates down to 5 ml/hr. Although the controls can set rates below 1ml/hr, these pumps are not considered appropriate for delivering drugs at such low rates. 215 b. Once the infusion has been connected to the patient, the vertical position of the device should be altered as little as possible as an increase in height of the device above the infusion site may result in a bolus of infusate being delivered to the patient. Blood transfusions may be given through a Baxter Colleague Volumetric Pump safely if given with correct blood giving set. Most volumetric pumps also incorporate the following safety features: o Automatic alarm and stopping of infusion following detection of air in line, upstream/downstream occlusion, and reservoir/bag empty alert. o Facility to pre-set volume to be infused (VTBI) and digital read out of total volume infused. o Automatic switch to ‘keep vein open’ (KVO) rate towards end of infusion. o Automatic battery operations in the case of mains supply failure. PHNT has standardised on the Baxter Colleague pump as the volumetric pump of choice, although others may still be in service in some areas. Syringe pumps The preferred choice for lower volumes and low rate infusions. Capable of delivering very low flow rates of < 1ml/hr. Operated by driving a syringe plunger forward at a controlled rate to deliver the infusate to the patient. The syringe is located and clamped within the device, with the plunger attached to a moving carriage. Users should be aware that the flow delivered at the start of an infusion might be considerably less than the rate set on the device. At low flow rates, the mechanical slack must be taken up before the set rate is achieved. Mechanical slack can be eliminated by operating the syringe pump to purge the line prior to connection to the patient. Some pumps have a selectable occlusion pressure alarm levels. Selecting low levels will help to prevent excessive delivery pressures and possible vein damage. Additional features may include: o In line pressure monitoring o Syringe barrel clamp alarm o Syringe plunger disengagement alarm o ‘Volume to be infused’ (VTBI) display o ‘Volume infused’ (VI) display o Automatic ‘keep vein open’ (KVO) rate facility o Patient history log o Drug name library PHNT has standardised in the Alaris GH syringe pump of choice. Other syringe pumps may still be available in some areas. c. Patient Controlled Analgesia pumps (IVPCA) 216 Used specifically for the patient to administer a prescribed intravenous dose of opioid as required, by activating a demand button, which has a pre-set lockout interval. PCA pumps (the Alaris IVAC PCAM) contains a memory log, to enable the clinician to determine how frequently the patient has made a demand, and the total volume of drug infused over a given time. Monitoring of patients with PCA devices may only be performed by those individuals who have received formalised training from the Department of Pain Management or those that have already been deemed competent in the use of PCA. d. Ketamine Infusions Ketamine is an anaesthetic agent with analgesic properties. A low dose Ketamine infusion can provide safe and effective analgesia. It is usually used with IVPCA to improve pain relief and reduce opioid side effects. The Graseby 3300 pump must always be used for these infusions. This is a locked pump. The responsibility of Ketamine infusions falls to the Acute Care Team / Anaesthetic team. Ward areas should not be the key holder unless under specific instructions of the Pain Team. In an emergency situation ward nurses should be aware of how to stop the infusion pump. Specific guidelines / protocols are in place within the Trust on all Advanced Pain Management Systems and must be followed. Please refer to the Acute Pain Resource Manuals or on the Hospital Healthnet e. f. Ambulatory pumps Allows for the mobility of the patient due to the small nature of the device. Preferred pump of choice for treatment in palliative care. Ambulatory pumps may be powered by electricity or by other means. The previously used Graseby MS26 has now been replaced, in this Trust, with the Mckinley T34 ambulatory syringe pump. The T34 is calibrated in ml/hr in common with other types of infusion device. The ‘Syringe Driver Infusion Chart’ should be used in conjunction with every infusion given via an ambulatory syringe driver device. Gravity feed Gravity feed involves the control of infusion rate by means of the height of the infusion reservoir being sufficiently greater than the infusion site to allow a slow flow of the infusate. Control is further refined by use of a clamp on the infusion line. 217 2.3 2.4 Generally suited to the delivery of fluids containing no added drugs or drugs with no potential for vaso-irritation or damage. This is due to the poor reliability of flow rate and pressure sensing in the delivery system. Provides a cheap and readily available delivery system. Additional Information Only luer-lock syringes should be used within syringe pumps/drivers, PCA pumps. This is a standard instruction issued by all infusion device manufacturers, as there is a risk of the pressure generated in the infusion line causing the line to come apart from the syringe. Plymouth Hospital NHS Trust currently uses BD Plastipak syringes for this purpose. Anti-syphon lines must be used on all syringe pump infusions in all areas. Gravity lines may be used for administration of electrolytes and most antibiotics. If considered necessary however, an infusion device may be used. References Medical Devices Agency (2000) Equipped to Care CQC Essential Standards of Quality & Safety Medicines and Healthcare products Regulatory Agency (2008) Devices in Practice 218 Appendix 3 Copy of the PHNT Policy for maintenance of patency, flushing and locking of intravascular lines catheters or devices 3.1 Introduction This appendix contains tables of instructions which have been copied from the PHNT Medicines Management Policy. The full ratified copy of this policy can be found on Plymouth Healthnet using the link: http://nww.picts.nhs.uk/PHNetLive/Portals/57ad7180-c5e7-49f5-b282c6475cdb7ee7/prowsea_TRW.MMA.POL.265.6%20Medicines%20Management%20Policy.pdf These tables were produced following review of current local practice and extensive local consultation, and in response to the National Patient Safety Agency Rapid Response Alert No.2 (2008) “Risks with Intravenous Heparin Flush Solutions”. 3.2 Policy All flushes (Bolus and infusions) and line/catheter locks must be prescribed. Administration of all flushes and line/catheter locks must be recorded on the prescription chart. Always attempt to aspirate the heparin lock before use of the line. If unable to aspirate the heparin from the line, discuss with the duty consultant whether the heparin may be flushed into the patient. Heparin must not be used in a patient with recognised or suspected HIT, or at risk of HIT (Heparin-induced thrombocytopenia) without discussion with a Consultant Haematologist. Type of intravascular line, catheter or device Short-term Peripheral Venous Catheters (Adults and children) Cannula, venflon Arterial Lines (Adults and children) Central Venous Lines (Inpatient Adults) Tunnelled lines eg. Hickman or Broviac lines PICCs and Midlines Short-term CVCs Long Lines Short-term Central Venous Catheters (Children) Maintenance of Patency, Flushing and Locking Flush with 5 -10ml 0.9% sodium chloride Maintain patency with an infusion of 0.9% sodium chloride. Flush with 0.9% sodium chloride (at least 10ml for adult patients) and lock with 0.9% sodium chloride (volume stated on the line) using a positive pressure clamp technique. All lines without a continuous infusion running should be flushed with 0.9% sodium chloride 6-hourly. To avoid blood flashing back into the lumen, “positive pressure” is applied at the end of the flush. Above table continued on the next page 219 Type of intravascular line, catheter or device Table continued from the previous page Maintenance of Patency, Flushing and Locking 220 Long-term Central Venous Lines (Children) Long Lines (Children) Long Lines (Neonates) Umbilical Arterial Catheters (Neonates) Vascaths (In General and Cardiothoracic Intensive Care) Renal-type large bore lines (On Adult Renal and Haemodialysis Units, and in Adult Haematology patients) Dialysis lines Vascaths Ports (Adults and children) Totally implantable venous access devices eg. Portacaths Central Lumen of Intra-aortic Balloon Pump Catheter Central Venous Lines (Outpatient or Day Case Adults) Tunnelled lines eg. Hickman or Broviac lines Line lock in patients receiving TPN who have had a previous line infection Hickman, Cook & Broviac Lines: Flush with 0.9% sodium chloride and lock with 3ml of 10 units/ml heparin. Groshong Lines: Flush with 0.9% sodium chloride and lock with 5ml sodium chloride 0.9%. Use 10 units/ml heparin to flush and lock Long Lines in children Maintain patency with an infusion of 0.9% sodium chloride. In the case of an extremely premature infant maintain patency with an infusion of 0.45% sodium chloride. Maintain patency with an infusion of 1unit/ml heparin, prepared by diluting 10 units/ml heparin, according to the Neonatal ICU protocol. Lock the catheter with trisodium citrate 46.7% solution (If no allergy). The locking volume will be stated on the catheter. Before use, aspirate the trisodium citrate solution from the catheter and flush with 10ml of 0.9% sodium chloride. If unable to aspirate the trisodium citrate solution, discuss with the duty consultant whether the trisodium citrate solution may be flushed into the patient. Flush the line with at least 10ml 0.9% sodium chloride then lock the line/catheter with trisodium citrate 46.7% solution (If no allergy). The locking volume will be stated on the catheter. Before use, aspirate the trisodium citrate 46.7% solution from the line/catheter. If this is not possible, the trisodium citrate 46.7% solution may be slowly flushed into the patient. Then flush with at least 10ml 0.9% sodium chloride. When in use with the needle in, flush with at least 10ml 0.9% sodium chloride. Lock the device with the appropriate volume of 10 units/ml heparin. Before the needle is removed, flush with at least 10ml 0.9% sodium chloride then lock the device with the appropriate volume of 100 unit/ml heparin. Use Heparin Sodium 2000 units/L in 0.9% Sodium Chloride IV Infusion, 500mL bags, REF Baxter B0953, as a continuous flush of the central lumen of the Intra-Aortic Balloon Catheter, as per protocol. Flush the line with at least 10ml 0.9% sodium chloride then lock the line/catheter with trisodium citrate 46.7% solution (If no allergy). The locking volume will be stated on the catheter. Before use, aspirate the trisodium citrate 46.7% solution from the line/catheter. If this is not possible, the trisodium citrate 46.7% solution may be slowly flushed into the patient. Then flush with at least 10ml 0.9% sodium chloride. Lock the line with the appropriate volume of Taurolock® (This contains taurolidine and sodium citrate). 221 Appendix 5 Document accountability, responsibility and dissemination 4.1 Accountability Production Peter Gray, Pharmacist Review and approval Medicines Utilization and Assurance Committee Dissemination Peter Gray, Pharmacist 4.2 Overall responsibility for this document The Director of Pharmacy has overall responsibility for the safe preparation and administration of medicines in this Trust, and therefore has overall responsibility for this document. 4.3 Dissemination and Implementation Following approval and ratification by the Medicines Utilization and Assurance Committee this eleventh edition of the injectable drug monographs with appendices will be rolled out across the Trust. Publication of the eighth issue will be publicised in Vital signs and in the weekly staff news brief. The new edition will be held in the Pharmacy Dept. Section of PHNT StaffNet. Paper copies will be printed by the Print Room, and together with electronic copies for selected recipients, will be distributed according to a distribution list held in Pharmacy. 222 Approval by Medicines Governance Group (MGG) Chief Pharmacist (Chair of MGG) Name: Steve Cooke Signature:… Date: 20.07.2016 Final Approval by Plymouth Community Healthcare Medical Director Name: Dr. Adam Morris Signature Date: 20.07.2016