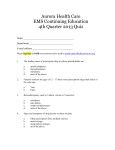
* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Adult Emergency Response Guidelines
Survey
Document related concepts
Transcript
Adult Emergency Response Guidelines
Instructions & Abbreviations
Standing Orders Policy
DRS ABCD – Basic Life Support Flow Chart
Rapid Assessment Guide for Emergency Response
Dyspnoea & Cyanosis
Disorganised Speech / Behaviour
Coma / Altered Level of Consciousness
Acute Asthma
Acute Dystonic Reaction
Anaphylaxis
Chest Pain
Haemorrhage / Hypovolemia
Hypoglycaemia
Meningococcal Disease
Opioid Overdose
Status Epilepticus
Stab Wounds
Suicide Attempt
Version Control
The Adult Emergency Response Guidelines is a version controlled
document. Version status, amendments and the distribution list are
given below
1. BUILD STATUS:
Author/s/Edit
or
Version
Date
Reason
Sections
1
2003
Clinical and
Nursing
Services
Original
2
2009
Clinical and
Nursing
Services
Review
All
Amended
2010
Clinical and
Nursing
Services
Update to
Midazolam
Standing Order
Status
Epilepticus
Amended
2011
Clinical and
Nursing
Services
Update of DRS
ABCD from
Australian
Resuscitation
Council
DR ABCD
Amended
2012
Clinical and
Nursing
Services
Update to
Benzylpenicillin
(Sodium)
Standing Order
Meningococcal
Amended
2012
Clinical and
Nursing
Services
Removal of
Hartmanns
Solution from
Standing
Orders
Haemorrhage/
Hypovolemia
Amended
2012
Clinical and
Nursing
Services
Removal of
Hartmanns
Solution from
Standing
Orders
Stab Wound
Amended
2012
Clinical and
Nursing
Services
Updated as per
PD2011_037
NSW Chest
Pain Pathway
Chest Pain
2
2. DISTRIBUTION:
Copy No Version
2
Issue Date
Issued To
February 2011
All Justice Health
Emergency
Response Equipment
Packs
3
Introduction
The Emergency Response Guidelines have been developed to guide
the clinical practice of nurses working in Justice Health and Forensic
Mental Health Network. It is important to note that the Emergency
Response Guidelines contain information that has been assessed as
being pertinent to the Correctional Environment. The Emergency
Response Guidelines have been developed for Registered Nurses to
assist in the assessment, management and referral process for
general emergency situations. Information contained has been
developed in accordance with the Justice Health and Forensic Mental
Health Network Adult Standing Orders.
The Emergency Response Guidelines have been developed in
consultation with the Primary Health Clinical Stream. Every effort has
been made to ensure that the information contained in the package
meets evidence based best practice standards.
The Emergency Response Guidelines are to be placed in both the
Airway Management Backpack and the First Aid Bag in each Health
Centre for reference when attending to an Emergency response
situation.
For information related to medications, Registered Nurses should refer
to the MIMS, for verification of indications, dosages and possible side
effects of medications administered.
This document is a formal publication of Justice Health and Forensic
Mental Health Network; all rights are reserved by the organisation. The
document may, be freely reviewed, abstracted, reproduced or
translated, in part or in whole, but not for sale nor for use in conjunction
with commercial purposes.
Justice Health and Forensic Mental Health Network
PO Box 150
Matraville NSW 2036
Version 2.0 - 2009
4
REFERENCES
Australian Resuscitation Council Guidelines www.resus.org.au
Diabetes Australia www.diabetesaustralia.com.au
Heart Foundation www.heartfoundation.com.au
National Asthma Council Australia. Asthma Management Handbook,
2006. www.asthmafoundation.com.au
Expert advice was provided by:
Prince of Wales Hospital, Emergency Staff Specialist, Dr Kenneth
Abraham
Ambulance Service of NSW, Senior Medical Adviser / Director of
Research, Associate Professor Paul M Middleton, RGN MBBS FRCS
(Eng) Dip IMCRCS (Ed) FCEM FACEM
Further information
Inquiries pertaining to Adult Standing Orders contained in these
guidelines should be directed to the Chief Pharmacist on
(02) 9700 3088
Inquiries pertaining to clinical information or formatting contained in
these guidelines should be directed to the Project Officer C&NS
(02) 9700 3024
5
Instructions and Abbreviations for the
Emergency Response Guidelines
The Emergency Response Guidelines contains key Emergency
Response situations that are clearly identified by a colour coding
system identified on the front page of the Emergency Response
Guidelines and the corresponding colour coded tab at the right hand
side of the folder.
An algorithm is presented on the first page of each of the identified
sections with pertinent information regarding the Justice Health and
Forensic Mental Health Network Standing Orders and Nurse Initiated
Medications.
All health care professionals should ensure that they are familiar with
the information contained in the Justice Health and Forensic Mental
Health Network Adult Standing Orders, as the algorithms are a
supplement to guide care in an emergency situation. They do not
provide education regarding the aetiology of the illness or disease.
The Primary Survey should be carried out in all Emergency Response
situations prior to the management of the identified emergency. This
assessment should proceed quickly, within 1-2 minutes. Nothing
should interrupt this assessment except treatment of airway
obstruction or cardiac arrest.
Patients who require active resuscitation, are assessed as medically
unstable or have sustained a significant injury should be transferred to
hospital. Appropriate medical advice is to be obtained by telephone in
cases where the condition of the patient is serious or in cases where
the condition of the patient is beyond the scope of practice and
expertise of the health care professional to manage.
6
Abbreviations
ABCD
Airway, Breathing, Compression and Defibrillation
BGL
Blood Glucose Level
BP
Blood Pressure
COPD
Chronic Obstructive Pulmonary Disease
CPR
Cardiopulmonary Resuscitation
EAR
Expired Air Resuscitation
ECG
Electrocardiograph
GCS
Glasgow Coma Scale
LOC
Level of Consciousness
IMI
Intramuscular Injection
MO
Medical Officer
NIM
Nurse Initiated Medication
NRM
Non Re-breathing Mask
PEF
Peak Expiratory Flow (Peak Flow)
PO
Per Oral
PRN
As required
R.R.
Respiratory Rate
Sp O2
Oxygen Saturation
SCI
Sub-Cutaneous Injection
SO
Standing Order
7
ADULT STANDING ORDERS
PREFACE
A specific prescriber should provide the majority of clinical care to a specific
individual patient. However, the NSW Health Department Policy Directive,
PD2007_077, Medication Handling in NSW Public Hospitals – October 2007,
section 5.2 - Standing Orders, authorises the development of protocols for
medications, which may be supplied or administered by a registered nurse to a
patient with an identified clinical condition without a medical officer’s
authorisation, provided appropriate written protocols for its use are also
developed.
Justice Health and Forensic Mental Health Network Standing Orders provide
authorisation for Registered Nursing staff to administer medication in defined
situations to individual patients without a prior written order by a medical
practitioner on a medication chart.
Standing Orders apply to persons over the age of eighteen years and in the
adult correction facilities, and are not to be utilised in the Adolescent
Healthcare Centres.
Standing Orders apply to life saving situations and when access to medical
officer is not possible and is not to be utilised for routine day to day
requirement.
Each Standing Order has been approved for use by the Justice Health and
Forensic Mental Health Network Drugs and Therapeutics Committee (D&TC)
and is in the form of a written instruction, signed and dated by the Chief
Executive. Standing Orders are reviewed every year by the D&TC.
OBJECTIVES
Standing Orders have been developed for the administration of medication in
life saving or other specific situations within Justice Health and Forensic
Mental Health Network.
OUTCOMES
•
Appropriate and timely response to identified life threatening and other
medical situations that can occur when medical officers are not
available.
•
Best practice in health management of identified medical situations
occurring within the constraints of the environment.
•
Improved patient care and individual patient outcomes.
•
Reduction of adverse incidents or severity of consequences of the
incident.
•
High quality treatment and care, which is evident through timely
intervention for, identified medical concerns.
8
DOCUMENTATION
When a Registered Nurse administers medication/s according to one of these
Standing Orders they must be recorded in black ink on a Justice Health and
Forensic Mental Health Network Standing Order medication chart (in-patient
and out-patient) and a note made in the patient’s medical record explaining the
rationale for use.
Whenever a Registered Nurse uses a Standing Order a Medical Officer must
be contacted within 24 hours to provide advice on treatment. This
communication along with any treatment advice or changes to a patient’s
management plan must be documented in the patient’s medical record. The
date and time of the discussion with the Medical Officer must be noted on the
Standing Order medication chart and in the patient’s medical record.
A Medical Officer must check this record and confirm it in writing within 7 days
of initiating treatment (reference therapeutic act verbal medication order
requirement).
A Medical Officer must review the use of a Standing Order applied more than 3
times in a four-week period.
It is the responsibility of the NUM or NIC to establish a system and to arrange
for the Medical Officers of their ward or healthcare centre to perform this
function.
Refer also the Justice Health and Forensic Mental Health Network Medication
Guidelines, Sections 6.19 Standing Orders and 6.20 Emergency Telephone
Orders.
The Justice Health and Forensic Mental Health Network Standing Orders are
available on the Justice Health and Forensic Mental Health Network Intranet:
Procedures / Policies > Medications > Adult Standing Orders.
The Airway Management Backpack and First Aid Bag as well
as AED (if available) should be taken to all Emergency
situations. The Backpack and First Aid Bag should be carried
in the correct manner.
9
10
11
12
DRS ABCD – Basic Life Support Flowchart
D
Check for DANGER
Hazards / Risks / Safety?
R
Check for RESPONSE
(If unresponsive)
S
SEND for help – ring 000
A
Open the AIRWAY
B
Normal BREATHING?
(If not breathing / abnormal
breathing)
C
Give 30 chest COMPRESSIONS
(almost 2 compressions per
second) followed by 2 breaths
then continue
D
Attach AUTOMATED EXTERNAL
DEFIBRILLATOR (AED) as soon
as available and follow prompts
If spinal injury is
suspected, apply stiff
neck collar and
maintain spinal
precautions
Suction with V-Vac suction
device if required and
Consider
clear airway
Chin lift / jaw thrust while
maintaining spinal
precautions
*When using
bag valve
device, it is
recommended
for use with two
operators.
Attach pocket
mask without
filter to Bag
valve device for
more secure
connection
LOOK
LISTEN
FEEL
Call Ambulance and notify
Emergency Department
Continue CPR until responsiveness or
normal breathing return
Discuss with MO on call, if the patient is breathing and normal cardiac
rhythm has returned, further assess causation of incident – Give O2 15L/min
via a non re-breathing mask.
Refer to Dyspnoea and Cyanosis Algorithm if altered breathing patterns
(Refer to: Adult Standing Orders and Nurse Initiated Medications)
Organise transfer to hospital if indicated
11
13
Defibrillation
•
An Automated Electronic Device (AED) is a portable device that
monitors the heart.
•
The AED’s computer assesses the patient’s heart rhythm and prompts
the rescuer to provide the correct treatment, guiding the rescuer at every
stage.
•
The AED will prompt the user to deliver a shock to the patient only when
the patient is in a shockable rhythm. It will not allow the operator to
shock the patient unless the patient is in a shockable rhythm.
•
Voice prompts guide the user throughout the emergency including CPR
coaching via audible prompts.
•
For every minute defibrillation is delayed the patients chance of survival
decreases by 10%.
14
Rapid Assessment Guide for Emergency
Response
PRIMARY SURVEY
A
B
C
D
E
AIRWAY
BREATHING
CIRCULATION
DISABILITY
EXPOSURE
SECONDARY SURVEY
HEAD TO TOE - head, neck, neurological,
chest, abdominal, pelvis and limbs
FRONT TO BACK
ANY PATIENT WITH A SIGNIFICANT HEAD
INJURY ALSO HAS A CERVICAL SPINAL INJURY
UNTIL PROVEN OTHERWISE
CAUSE OF COMA
A
E
I
O
U
T
I
P
S
ALCOHOL, ASPHYXIA
EPILEPSY
INSULIN (OVER / UNDERDOSE)
OVERDOSE
URAEMIA
TRAUMA
INFECTION
PSYCHIATRIC
STROKE / SHOCK
SAMPLE HISTORY
S
A
M
P
L
E
SYMPTOMS
ALLERGIES
MEDICATIONS
PREVIOUS INJURY
LAST MEAL
EVENT LEADING TO INCIDENT
PAIN ASSESSMENT
P
Q
R
S
T
PAIN
QUALITY
REGION/RADIATION
SEVERITY
TIME
GLASGOW COMA SCALE
EYE OPENING
NONE
TO PAINFUL STIMULUS
TO VERBAL STIMULUS
SPONTANEOUS
BEST VERBAL RESPONSE
NONE
INCOMPREHENSIBLE SOUND
INAPPROPRIATE WORDS
CONFUSED
ORIENTATED
BEST MOTOR RESPONSE
NONE
ABNORMAL EXTENSION
ABNORMAL FLEXION
WITHDRAWS FROM PAIN
LOCALISES PAIN
OBEYS COMMAND
POINTS
1
2
3
4
POINTS
1
2
3
4
5
POINTS
1
2
3
4
5
6
POISONS INFORMATION CENTRE
PHONE: 13 11 26
Refer to the following JH&FMHN Policies:
Policy No 1.010 Access to inmates – Emergencies
Policy No 1.032 Admission to Public Hospitals – Emergency
Policy No 1.020 Administration of Medications
Policy No 5.040 Emergency, First Aid
Policy No 5.070 Infection Control
15
ABCDE – Primary Survey
Mobilise resources quickly and designate one person to each of the following:
•
Take charge of the assessment process
•
Begin resuscitation interventions as required
•
Make phone calls
Prior to proceeding with assistance ensure personal safety, assess for
any signs of danger:
•
Other patients in the vicinity are secured (DCS)
•
Blood or fluids
•
Electricity
•
Unstable foundations
•
Don gloves, goggles and face mask
•
Apply a gown if necessary
•
Sharp objects, place any sharp objects into a sharps container
The primary survey is a prioritised assessment and treatment of lifethreatening injuries which is approached in an orderly fashion and should take
no more than 2-5 minutes to complete.
A for airway management and cervical spine protection
B for breathing and ventilation
C for circulation and haemorrhage control
D for disability: Neurological status
E for exposure / environmental control: completely expose patient
Airway management and cervical spine protection
•
Attempt to elicit a response from the patient
•
Give an audible command e.g. ‘Can you hear me?’
•
Giving a tactile stimulus e.g. grasp the casualty’s hands and say ‘if you
can hear me squeeze my hands and let them go’
•
Ask patient what happened. If the person can answer, you have valuable
information about patency of the airway and level of consciousness
•
Make a brief assessment of the patient’s level of consciousness
(conscious/altered level of consciousness/unconscious)
•
Facial or mandibular, tracheal / laryngeal injuries
•
Oxygen
•
Keep cervical spine in neutral position while managing airway if you
suspect a cervical spine injury (cervical spine injuries should be
suspected in all patients with a blunt injury above the clavicle)
16
•
Use backward head tilt/chin lift (head and neck slightly extended and line
from chin to jaw angle perpendicular to the floor-do not use if cervical
spine injury suspected) or jaw thrust (place 2-3 fingers under each side
of lower jaw angle and lift jaw upward and outward) manoeuvres to open
airway. Ensure that the tongue does not fall back into pharynx and
obstruct the airway
Insert an oropharyngeal airway if patient is unconscious and it is
clinically indicated. Measure from the corner of the mouth to the tip of the
ear lobe for size required. Insert with end uppermost, turning the Guedel
airway 180 degrees when you reach the soft palate.
Signs of airway obstruction may include but are not limited to:
•
•
Snoring or gurgling
•
Stridor or abnormal breath sounds
•
Agitation (hypoxia)
•
Using the accessory muscles of ventilation/paradoxical
•
Chest movements
•
Cyanosis
Attempt to elicit a verbal response from patient
•
Look for blood, vomitus or foreign objects
•
Use V-Vac to assist in clearing the patients airway
Breathing
Look and feel for movement
•
Your ear is placed close to the mouth of the patient with the head turned
looking for chest wall movement.
•
Ascertain if the patient is breathing?
•
If the patient is not breathing immediately commence EAR. Give 2
‘rescue breaths’ with a bag valve device or with the pocket facemask.
•
Ensure that the chest is rising with each inhalation.
•
Ensure effective head tilt to allow for exhalation.
If the patient is breathing spontaneously, ensure the patient is breathing
effectively and check respiratory effort and use of accessory muscles (look,
listen and feel).
Assist ventilation if breathing is not effective with the mask and bag valve
device.
17
•
Ventilate with oxygen using a mask and bag valve device at 12
breaths/min
Ensure ventilations are performed with a slow inspiratory flow rate to
reduce the incidence of gastric distension, regurgitation and aspiration.
If patient is breathing spontaneously (12-18 breaths/min), improve oxygenation
of vital tissues - Give oxygen at 15 L/min by non re-breathing mask; maintain
oxygen saturation > 98%
•
•
Ensure effective ventilations are being achieved
•
If ventilation is ineffective due to possible airway obstruction, reassess
the airway and attempt to clear the obstruction.
•
Inspect chest for crepitus and open wounds
Circulation
‘Shock’ is defined as inadequate tissue perfusion and tissue oxygenation. In
the trauma patient it is most often due to hypovolaemia. The diagnosis of
shock is based on clinical findings: hypotension, tachycardia, tachypnoea, as
well as hypothermia, pallor, cool extremities, decreased capillary refill and
decreased urine production.
There are different types of shock including:
Haemorrhagic (hypovolaemic) shock: Due to acute loss of blood or fluids. The
amount of blood loss after trauma is often poorly assessed and in blunt trauma
is usually underestimated. Remember:
•
Large volumes of blood may be hidden in the peritoneal and pleural
cavities
•
Femoral shaft fracture may lose up to 2 litres of blood
•
Pelvic fracture often lose in excess of 2 litres of blood
Cardiogenic shock: Due to inadequate heart function.
This may be from:
•
Myocardial contusion (bruising)
•
Cardiac tamponade
•
Tension pneumothorax (preventing blood returning to heart)
•
Penetrating wound of the heart
•
Myocardial infarction
Neurogenic shock: Due to the loss of sympathetic tone, usually resulting from
spinal cord injury, with the classical presentation of hypotension without reflex
tachycardia or skin vasoconstriction.
18
Septic shock: Rare in early phase of trauma but is a common cause of late
death (via multi-organ failure) in the weeks following injury. Common in
untreated or unrecognised infections, often seen in penetrating abdominal
injury and burns patients.
Haemorrhage Control
•
Identify and control external bleeding, this should be performed by a
second rescuer if the patient is requiring CPR
•
Apply direct pressure and dressings to external bleeding
•
If the wound continues to bleed apply a further dressing over the original
dressing. Never remove the original dressing
If a foreign object or knife is protruding from the wound, do not remove,
stabilise the object. (Refer to: Stab Wound Algorithm)
Tourniquets should not be used; they can cause reperfusion syndromes and
add to primary injury.
•
Disability
Rapid neurological assessment (is patient awake, vocally responsive to pain or
unconscious)
•
A – awake
•
V – verbal response
•
P – painful response
U – unresponsive
System at this stage is clear and quick.
If time allows a Glasgow Coma Scale could be used.
Any change in level of consciousness or depreciation in the GCS should
prompt a return to the beginning of primary survey.
•
Exposure
Expose patient entirely to allow global assessment. If the patient is suspected
of having a neck or spinal injury, in-line immobilisation is important. Patient
privacy must be considered.
19
Dyspnoea and Cyanosis Algorithm
Is the patient post-ictal?
Place in recovery position
Assess Neurological Status
Conduct Primary Survey – ABCDE
(Refer to: Adult Standing Orders
Asthma, Anaphylaxis, Opioid
overdose)
Record BP, PR, RR, Temp, BGL,
Sp O2
Is asthma suspected?
Go to: Asthma Algorithm
Administer O2 15L via non re-breathing
mask
Is Anaphylaxis suspected?
Go to: Anaphylaxis Algorithm
No
Is Dyspnoea and Cyanosis due to other
causes?
Consider: Exacerbation of COPD, opioid
overdose, smoke inhalation, aspiration,
pulmonary oedema, etc and discuss with
Medical Officer
Has the patient sustained a chest
injury?
Yes
Cover any chest wounds with threesided dressing
Is the trachea midline?
Suspect tension pneumothorax
Call ambulance, requires urgent transfer to
hospital
No
Yes
Reassess Circulation:
Quality, location rate
Is Carotid Pulse present?
Position patient in comfortable
position and maintain cervical spine
precautions
Commence CPR
(30 compressions then 2 breaths)
Administer 2 breaths
(with high flow O2, using mask and
*bag valve device)
Call Ambulance and notify Emergency
Department
No
Yes
Further assess causation of
incident – Give O2 15 L/min
Discuss with MO
If symptoms do
not improve then
call Ambulance
000
Insert Guedal airway (Measuring from
tip of ear to corner of mouth)
If spinal injury suspected apply stiff neck
collar, observe cervical spine precautions
*When using bag valve device, it is
recommended for use with two operators.
Attach pocket mask without filter bag to
device for more secure connection.
19
20
Disorganised Speech / Behaviour Algorithm
Conduct Primary Survey – ABCDE
Indications: required for patients with acute disturbance of speech or behaviour
Record BP, PR, RR, Temp, BGL, Sp O2
Administer O2 15L/min via
non-re-breathing mask.
Assess: BP, PR, RR, Temp, BGL, Sp O2, AVPU
Is BGL < 4 mmol/L?
No
Yes
Possible drug induced behavioural
change
Refer to: Hypoglycaemia Algorithm
No
Administer O2 15L/min via non
re-breathing mask
Insert IV Cannula
Assess GCS
Discuss with MO
Transfer to hospital for assessment
Yes
Has patient
received a recent
head injury?
Yes
If patient is unconscious or
very drowsy refer to Opioid
overdose algorithm
No
Face, Arm and Speech Test (FAST)
Suspect stroke if any of the following are abnormal
A) Facial movements
Ask patient to smile or show teeth. Look for
asymmetry – unequal smile or grimace or obvious
facial asymmetry
B) Arm movements
Lift the patient’s arm together to 90O if sitting, or 45O
if supine. Ask patient to hold that position for 5 sec
and then let go it is abnormal if one drifts down or
falls more rapidly
C) Speech impairment
Look for new disturbances in speech. Look for
slurred speech and word-finding difficulties. Ask the
patient to name common nearby objects such as a
cup, chair, key and pen.
If there is a severe visual disturbance, place an
object in the patients hand and ask them to name it.
Discuss patient with Psychiatrist
or Medical Officer
Assess GCS, cognitive function,
perceptual disturbances and
complete the FAST
No
Fluctuating LOC?
Administer O2
15L/min via non
re-breathing mask.
Call Ambulance
Refer to: Coma / altered
level of consciousness
algorithm
Yes
Perform Mental State Examination
Appearance / behaviour
Rate & content of speech
Form and content of thought
Mood & affect
Perceptual abnormalities
Insight & judgement
21
Coma / Altered Level of Consciousness Algorithm
Conduct Primary Survey – ABCDE
(Refer to: Standing Orders: Hypoglycaemia, Anaphylaxis, Opioid overdose)
Record BP, PR, RR, Temp, BGL, Sp O2
Administer O2 15L/min via non-breathing
mask
Assess blood glucose level
Is the Blood Glucose Level less than
4 mmol/L?
Yes
Hypoglycaemia
Go to: Hypoglycaemia Algorithm
(Refer to: Adult Standing Order,
Hypoglycaemia)
No
Is alteration in level of
consciousness (LOC) due to
possible overdose?
Yes
No
Is alteration in LOC due to head
injury, cardiac or unknown cause?
Yes
Opioid overdose
Go to: Opioid Overdose Algorithm
(Refer to: Standing Order: Opioid
Overdose)
Organise urgent transfer to hospital
Administer O2 at 15 L/min via non
re-breathing mask
Regularly assess:
Respiratory rate, radial pulse rate,
blood pressure and level of
consciousness (GCS)
Monitor:
Airway, Breathing and Circulation
Contact on call Medical Officer
Notify Emergency Department of
transfer.
POSSIBLE CAUSES OF COMA
A – Alcohol, asphyxia
E – Epilepsy
I – Insulin (overdose / underdose)
O – Overdose
U - Uraemia
T – Trauma
I – Infection
P – Psychiatric
S – Stroke, shock, seizures
22
Management of Coma / Altered Level of
Consciousness
Non Pharmacologic Interventions
•
•
•
•
•
Assess and stabilise ABCDE including cervical spine
Insert oropharyngeal airway (size is determine by measuring from the
edge of the patients mouth to the ear lobe)
Place in recovery position, unless there are contraindications such as a
suspected cervical spine fracture. (If the patient is already in the
recovery position then you should attempt to manage the patient in this
position provided they do not require active resuscitation)
Check Blood Glucose Level (BGL) - If BGL < 4 mmol/L, assume
hypoglycaemia
NB. Unstable diabetics with a normally high blood glucose level can
experience the symptoms of hypoglycaemia > 4 mmol/L.
Pharmacologic Interventions
If BGL < 4 mmol/L:
•
Administer 1mg glucagon IMI
•
Check BGL after 10 minutes, if BGL remains below 4 mmol/L administer
a second dose of 1mg glucagon IMI.
If BGL > 4mmol/L:
•
Suspect opioid overdose
Give
Naloxone (Narcan) (D class drug), initially 2mg IMI or SCI; repeat every 2-3
minutes if necessary to a maximum dose of 10 mgs.
The routine use of naloxone for patients without evidence of opioid intoxication
should be considered for patients who present with an altered level of
consciousness where the cause is unknown. If you are unsure, discuss with a
physician before administering. Monitor vital signs, including pulse oximetry (if
available)
•
Obtain a brief history focusing on the presenting problem. Try to clarify
the cause of the incident
•
In particular, determine if person has had any recent illness, fever, rash,
vomiting or trauma or has the patient been diagnosed with a chronic
illness
•
Attempt to ascertain if the patient has experienced any recent symptoms
of illness or substance withdrawal which could be linked to the current
presentation.
Observations in the secondary survey should attempt to uncover signs of
infection, trauma, or toxic or metabolic derangements. Signs suggestive of
drug overdose should be sought.
Adjuvant Therapy
•
Give oxygen (15 L / min) via a non-re-breather mask; keep oxygen
saturation > 97%.
23
Acute Asthma Algorithm
Conduct Primary Survey – ABCDE
(Refer to: Adult Standing Order Acute Asthma)
Record: BP, PR, RR, Temp, BGL, Sp O2
Assess Asthma Severity
Severe and life threatening
Mild
Moderate
Talks in sentences
Pulse < 100/min
Variable wheeze
PEF > 75% predicted
(or best if known)
Sp O2 over 97%
Talks in phrases
Pulse 100-120/min
Moderate to loud wheeze
PEF 50-75% predicted (or
best if known)
Sp O2 between 95-97%
5mg nebulised
salbutamol +2.5 mls
saline with O2 8L/min
Repeat dose 4th hourly
monitoring changes in
severity
5mg nebulised
salbutamol +2.5 mls
saline, 3 nebs over one
hour and 500mcg
Ipratropium Bromide 4th
hourly with continuous O2
8L/min
Regularly monitor for
changes in severity
Tallks in words
Pulse > 120/min
Often quiet wheeze
Altered LOC
Physical exhaustion
PEF <50% predicted (or best if known)
or less than 100 L/min
Sp O2 less than 95%
(Do not attempt PEF if patient
is cyanosed)
5mg Nebulised Salbutamol
+2.5mls saline continuously and
500mcg Ipratropium Bromide 2nd
hourly with Continuous O2
15L/min
Requires continuous monitoring
Refer to MO and issue patient with
salbutamol puffer if required.
Advise patient to notify Health
Centre staff if symptoms return
Urgently transfer patient to
hospital.
Inform Medical Officer
24
PRIMARY HEALTH
ACUTE ASTHMA
CLINICAL STREAM
SALBUTAMOL
STANDING ORDERS
Asthma can be life threatening. Spirometry is the lung function test of choice
for diagnosing asthma and for assessing asthma control in response to
treatment. Perform spirometry and/or peak expiratory (PEF) measurement as
soon as possible to gain an objective measure of airflow limitation. Severe
asthma should receive continuous oxygen at 15L/min. Oxygen therapy may be
associated with respiratory depression and arrest in patients with chronic CO2
retention, particularly those with Chronic Obstructive Pulmonary Disease
(COPD).
Drug Name
SALBUTAMOL
Common Brand Names
Ventolin inhaler or Nebules
Strength
100mcg / dose 200
2.5 mg and 5 mg solution
Dose
For the inhaler use 1-2 inhalations, repeat
every 3-6 hours if necessary
For the Nebules use 5mg in normal saline
every 3-6 hours for mild and 1-4 hours for
moderate asthma or every 15 minutes for
severe asthma with oxygen at 8L/min
Administration / Route
Inhalation via metered dose Inhaler (MDI)
with volumatic inhaler device (spacer
device for metered dose inhalers, if
available) or nebuliser for the Nebules
doses
inhaler
FOR MODERATE ASTHMA THAT IS NOT RESPONSIVE TO THERAPY AND FOR SEVERE
ASTHMA, CONTACT THE AMBULANCE SERVICE of NSW FOR EMERGENCY TRANSFER
TO HOSPITAL AND INFORM THE LOCAL MEDICAL OFFICER OR CMO ON CALL.
25
Initial assessment of acute asthma in adults
Findings
Mild
Moderate
*Severe & life
threatening
Yes
Paradoxical chest wall
movement may be
present
Physical
exhaustion
No
No
Talks in
Sentences
Phrases
Words
Pulse rate
< 100
100-120/min
More than 120/min
Pulsus paradoxus
Not palpable
May be palpable
Palpable
Wheeze intensity
Variable
Moderate to loud
Often quiet
Peak Expiry Flow
(PEF)
More than 75%
predicted (or best if
known)
50 - 75% predicted
(or best if known)
Less than 50%
predicted (or best if
known) or less than
100 L per min
Forced Expiratory
Volume (FEV1)
More than 75%
predicted
50-75% predicted
Less than 50%
predicted or less than
1L
INDICATIONS
Relief of acute bronchospasm (acute asthma).
4X4X4 FIRST AID PLAN
Inhaler with Spacer
•
Shake inhaler and insert mouthpiece into spacer.
•
Place spacer mouthpiece in person’s mouth and fire 1 puff.
•
Ask the person to breathe in and out normally for about 4 breaths.
•
Repeat in quick succession until 4 puffs have been given.
Inhaler without Spacer
•
Shake inhaler
•
Place mouthpiece in person’s mouth. Fire 1 puff as the person inhales
slowly and steadily
•
Ask the person to hold that breath for 4 seconds, then take 4 normal
breaths
•
Repeat until 4 puffs have been given.
(National Asthma Council Australia, 2006)
26
CONTRAINDICATIONS
Known allergy to main ingredient or preservatives.
DRUG INTERACTIONS
Beta-Blockers; other sympathomimetics, beta-adrenergic stimulants;
ipratropium bromide; xanthines; steroids; diuretics; digitalis.
ADVERSE EFFECTS
Hypokalaemia, arrhythmias; tremor; tachycardia, palpitations; headache;
hypotension; nausea; sensation of warmth; nervousness.
DOCUMENTATION
•
Physical Observations including: pulse, blood pressure, respiratory rate,
spirometry (if available) or PEF (if able), oxygen saturation, physical
assessment
•
Document medication on Standing Order chart.
The nurse must record the administration in black ink on the Standing Order
medication chart. A Medical Officer must be consulted as soon as possible
regarding ongoing management and this must be documented in the patient’s
medical record.
REFERENCES
Landau, P. (Ed) (1999). The Medical Officer’s Handbook. Sydney: Westmead Hospital
(accessed August 2007).
MIMS Online
Available at: http:// www.ciap.health.nsw.gov.au [accessed August 2007].
National Asthma Council Australia, Asthma Management Handbook, 2006.
27
PRIMARY HEALTH
ACUTE ASTHMA
CLINICAL STREAM
IPRATROPIUM BROMIDE
(ATROVENT)
STANDING ORDERS
Asthma can be life threatening. Spirometry is the lung function test of choice
for diagnosing asthma and for assessing asthma control in response to
treatment. Perform spirometry and/or peak expiratory (PEF) measurement as
soon as possible to gain an objective measure of airflow limitation. Severe
asthma should receive continuous oxygen at 15L/min. Oxygen therapy may be
associated with respiratory depression and arrest in patients with chronic CO2
retention, particularly those with Chronic Obstructive Pulmonary Disease
(COPD).
Drug Name
IPRATROPIUM BROMIDE
Common Brand Names
Atrovent,
Ipratrin,
(Nebuliser Solution)
Strength
250cmg/ml and 500mcg/ml nebules
Dose
Mild asthma: nil indicated
Moderate asthma: 500mcg 4th hourly
Severe asthma:500mcg by nebuliser driven
by oxygen (at least 8L/min) every 2-4 hours
DBL
Ipratropium
To be used with salbutamol in moderate to severe asthma.
Do not use ipratropium bromide alone for immediate relief of
symptoms.
Administration / Route
Nebulised with oxygen and salbutamol at >
8L/min
FOR MODERATE ASTHMA THAT IS NOT RESPONSIVE TO THERAPY AND FOR
SEVERE ASTHMA, CONTACT THE AMBULANCE SERVICE of NSW FOR EMERGENCY
TRANSFER TO HOSPITAL AND INFORM THE LOCAL MEDICAL OFFICER OR CMO ON
CALL
28
Initial assessment of acute asthma in adults
Findings
Mild
Moderate
*Severe & life
threatening
Yes
Paradoxical chest wall
movement may be
present
Physical
exhaustion
No
No
Talks in
Sentences
Phrases
Words
Pulse rate
< 100
100-120/min
More than 120/min
Pulsus paradoxus
Not palpable
May be palpable
Palpable
Wheeze intensity
Variable
Moderate to loud
Often quiet
Peak Expiry Flow
(PEF)
More than 75%
predicted (or best
if known)
50 - 75% predicted (or
best if known)
Less than 50%
predicted (or best if
known) or less than
100 L per min
Forced Expiratory
Volume
(FEV1)
More than 75%
predicted
50-75% predicted
Less than 50%
predicted or less than
1L
INDICATION
Relief of moderate asthma attacks.
CONTRAINDICATIONS
Known allergy, hypersensitivity to soya lecithin or related foods (soya beans,
peanuts), atropine hypersensitivity.
PRECAUTIONS
Closed angle glaucoma, prostatic hyperplasia, urinary retention, avoid contact
with eyes.
DRUG INTERACTIONS
•
Xanthines
•
Beta-mimetics (especially if there is a risk of glaucoma).
29
ADVERSE EFFECTS
•
Care is recommended during pregnancy and lactation (Category B1)
•
Headache; nausea; dry mouth; throat irritation; cough; anticholinergic
effects; GI motility disturbances; acute angle closure glaucoma (following
direct eye contact); rash; angioedema; urticaria; paradoxical
bronchoconstriction; allergic reaction
•
Avoid contact with eyes.
DOCUMENTATION
•
Physical Observations including: pulse, blood pressure, respiratory rate,
spirometry (if available) or PEF (if able), oxygen saturation, physical
assessment
•
Document medication on Standing Order chart.
The nurse must record the administration in black ink on the Standing Order
medication chart. A Medical Officer must be consulted as soon as possible
regarding ongoing management and this must be documented in the patient’s
medical record.
REFERENCES
Landau, P. (Ed) (1999). The Medical Officer’s Handbook. Sydney: Westmead Hospital
(accessed August 2007).
MIMS Online. Available at: http:// www.ciap.health.nsw.gov.au (accessed August 2007).
National Asthma Council Australia, Asthma Management Handbook, 2006.
30
PRIMARY HEALTH
ACUTE ASTHMA
CLINICAL STREAM
PREDNISOLONE
STANDING ORDERS
Asthma can be life threatening. Spirometry is the lung function test of choice
for diagnosing asthma and for assessing asthma control in response to
treatment. Perform spirometry and/or peak expiratory (PEF) measurement as
soon as possible to gain an objective measure of airflow limitation. Severe
asthma should receive continuous oxygen at 15L/min. Oxygen therapy may be
associated with respiratory depression and arrest in patients with chronic CO2
retention, particularly those with Chronic Obstructive Pulmonary Disease
(COPD).
This Standing Order is for a single initial dose of oral steroid until the on call
doctor is contacted. It should be used following initial treatment with nebulised
salbutamol and ipratropium bromide (atrovent).
Drug Name
PREDNISOLONE
Common Brand Names
Solone, Panafcortelone
Strength
5mg tablets/25mg tablets
Dose
Mild asthma: nil indicated
Moderate asthma: 50mg orally
Severe asthma:50mg orally
Administration / Route
Orally. To be taken with food to minimise GI
upset
This Standing Order is for a single dose only. Ring on call doctor
following administration for advice regarding acute asthma
management.
FOR MODERATE ASTHMA THAT IS NOT RESPONSIVE TO THERAPY,
AND FOR SEVERE ASTHMA, CONTACT THE AMBULANCE SERVICE OF
NSW FOR EMERGENCY TRANSFER TO HOSPITAL AND INFORM THE
LOCAL MEDICAL OFFICER OR CMO ON CALL.
31
Initial assessment of acute asthma in adults
Findings
Mild
Moderate
Physical
exhaustion
No
No
Severe & life
threatening
Yes. Paradoxical
chest wall
movement may be
present
Talks in
Sentences
Phrases
Words
Pulse rate
< 100
100-120/min
More than 120/min
Pulsus paradoxus
Not palpable
May be palpable
Palpable
Wheeze intensity
Variable
Moderate to loud
Often quiet
Peak Expiry Flow
(PEF)
More than 75%
predicted (or best if
known)
50 - 75% predicted
(or best if known)
Less than 50%
predicted (or best if
known) or less than
100 L per min
Forced Expiratory
Volume
(FEV1)
More than 75%
predicted
50-75% predicted
Less than 50%
predicted or less
than 1L
INDICATION
Antiinflammatory in asthma exacerbation
CONTRAINDICATIONS
•
Known allergy
•
Uncontrolled infections
•
Peptic ulcer; osteoporosis; psychoses, psychoneuroses; TB
•
Uncontrolled infections (bacterial and viral).
PRECAUTIONS
Diabetes, infection, stress, peptic ulcer, fresh intestinal anastomoses, cirrhosis,
hypothyroidism, ulcerative colitis, osteoporosis, elderly, active TB, ocular
herpes simplex, diverticulitis.
32
DRUG INTERACTIONS
Antacids; oral hypoglycaemics; insulin; digitalis glycosides; diuretics;
barbiturates; phenytoin; rifampicin; potassium supplements; ritodrine; Na+
containing drugs or food; somatrem, somatropin; vaccines, immunisations;
troleandomycin; ketaconazole; aspirin; oral anticoagulants; cyclosporine;
phenobarbitone.
ADVERSE EFFECTS
Fluid retention; dyspepsia; oedema; metabolic disturbances; hypertension;
hyperglycaemia, delayed wound healing; peptic ulcer; mental, neurological
changes; Cushingoid states; muscle weakness.
DOCUMENTATION
•
Physical Observations including: pulse, blood pressure, respiratory rate,
spirometry (if available) or PEF (if able), oxygen saturation, physical
assessment
•
Document medication on Standing Order chart.
The nurse must record the administration in ink on the Standing Order
medication chart. A Medical Officer must be consulted as soon as possible
regarding ongoing management and this must be documented in the patient’s
medical record.
REFERENCES
Landau, P. (Ed) (1999). The Medical Officer’s Handbook. Sydney: Westmead Hospital.
(accessed August 2007)
MIMS Online. Available at: http:// www.ciap.health.nsw.gov.au (accessed August 2007).
National Asthma Council Australia, Asthma Management Handbook, 2006.
33
Acute Dsytonic Reaction Algorithm
Conduct Primary Survey – ABCDE – Reassure the patient
(Refer to: Adult Standing Order, Acute Dystonic Reaction)
Indications – oculogyric crisis, torticollis or retrocollis, trismus, opisthotonos, laryngeal spasm
Assess type and severity of dystonia
Administer 2mg benztropine (Cogentin) IMI
Assess temperature, pulse, blood pressure, respiratory rate, Sp O2, level of consciousness
Assess response to benztropine
If dsystonia persists, assess severity
Severe dystonia (potential
for airway compromise)
Discuss with psychiatrist
Repeat benztropine 2 mg
IMI after 30 minutes.
Reassess vital signs,
monitor respirations
Maximum of 4 mg
benztropine in 24 hours
Patient is febrile, confused
and has muscle rigidity?
Yes
Assess differential diagnosis.
Assess mental status
??? Neuroleptic Malignant
Syndrome in patients taking
neuroleptic medication.
Also suspect serotonin syndrome
for patients on antidepressants.
Mild dystonia
Discuss with Psychiatrist on
call
Repeat benztropine 2mg
IMI after 30 minuutes if
dystonia persists
Maximum 4mg benztropine
in 24 hours
No
No
Assess for signs of injury
and differential diagnosis,
check BGL.
Discuss with psychiatrist
or Medical Officer
(If dystonia is due to
metoclopramide
(Maxalon), cease
treatment immediately.
If dystonia is due to
Neuroleptic Malignant
Syndrome, discuss with
Psychiatrist)
Ring psychiatrist or Medical Officer
Transfer to hospital for further assessment
Continue O2 > 8L/min
34
MENTAL HEALTH
ACUTE DYSTONIC REACTION
CLINICAL STREAM
BENZTROPINE
STANDING ORDERS
Acute dystonic reactions are caused mainly by antipsychotic medication and
occur most commonly with high potency antipsychotics (e.g. haloperidol).
These adverse effects can be extremely distressing. Acute dystonic reactions
are a medical emergency. Symptoms include oculogyric crisis (‘look-ups’),
torticollis, trismus, opisthotonos and laryngeal spasm. They generally develop
within hours to days of administration of antipsychotic medication and affect
the face, neck and trunk. In an emergency situation where respiratory
compromise or arrest occurs, follow resuscitation procedures.
Drug Name
BENZTROPINE
Common Brand Names
Cogentin
Strength
2mg/2ml ampoule
Dose
2mg IMI maximum of 4mg in 24 hours
Intramuscular injection. If the patient does not
improve in another 20-30 minutes, the drug
should be administered again.
•
Check patients treatment sheets for
current medication orders, i.e., is the
patient already on a regular order of
benztropine or any other antiparkinsonian
medication either as an ongoing or as a
PRN medication
•
Reassure and keep the patient calm
and provide supplementary oxygen if
required. If there is respiratory
compromise follow resuscitation
procedures
•
Request Medical Officer to asses or
review the patient and their medication as
soon as possible. To preclude the
reappearance of symptoms it is advised
that a medical officer prescribe oral
anticholinergic medication for 2-3 days
after the onset of the acute dystonic
reaction
• Observe and remain with the patient
following administration.
Administration / Route
35
INDICATIONS
Acute dystonic reaction causing severe distress, or moderate distress lasting
45 to 60 minutes, as evidenced by oculogyric crisis (‘look-ups’), torticollis or
retrocollis (spasm of the neck muscles), trismus (‘lock-jaw’, spasm of tongue
and floor of mouth), opisthotonos / tardive dyskinesia (spasm/arching of the
back), laryngeal spasm (difficulty swallowing, talking or breathing).
CONTRAINDICATIONS
Known allergy or hypersensitivity.
PRECAUTIONS
Tardive dyskinesia, prostatic hyperplasia, psychoses, tachycardia, high doses,
narrow angle glaucoma, symptoms that are only causing moderate distress (in
this case, monitor the patient and/or contact the on call medical officer.
ADVERSE EFFECTS
Anticholinergic effects, tachycardia, disorientation, hyperthermia (use with
caution in hot weather), GI upset, blurred vision, urinary retention, dysuria,
bowel obstruction, may aggravate tardive dyskinesia, idiosyncratic reactions
(abnormal behaviour, confusion, hallucinations), headache, dizziness,
drowsiness, numbness of fingers, cramps, memory problems and muscle
weakness.
DRUG INTERACTIONS
Benztropine may decrease the effects of:
•
Haloperidol and phenothiazines (chlorpromazine) – decreases the
antipsychotic effect therefore increasing psychotic symptomatology.
The following drugs may increase the effects of benztropine:
•
Amantidine (antiparkinsonian medication) may increase confusion and
hallucinations
•
MAOI type A inhibitor (Moclobemide) intensifies the effect of the
benztropine
•
Tricyclic antidepressants – adds to eye effects, increases internal eye
pressure (dangerous in glaucoma)
•
Levodopa – possible reduction in levodopa efficacy
•
Clozapine, phenothiazine and haloperidol– can cause increased risk of
elevated temperatures, neurological adverse effects and bowel
obstructions (paralytic ileus) and
•
Serum levels of Digoxin are increased.
36
DOCUMENTATION
Physical observations including:
•
Pulse, blood pressure, respiratory rate, and physical assessment.
•
Type and severity of dystonic reaction symptoms
•
Current mental state in medical record
•
Document medication on Standing Order chart.
The nurse must record the administration in black ink on the Standing Order
Treatment chart. A Medical Officer must be consulted as soon as possible
regarding ongoing management and this must be documented in the patient’s
medical record.
REFERENCES
Drugdex Drug Evaluations. Available at: http:// www.ciap.health.nsw.gov.au (accessed
August 2007).
MIMS Online. Available at: http:// www.ciap.health.nsw.gov.au (accessed August 2007).
37
Anaphylaxis Algorithm
Conduct Primary Survey – ABCDE
(Refer to: Adult Standing Order Anaphylaxis
Indications: +/- itching, rash, widespread vasodilatation and
extravasations (swelling), acute allergic reaction with shortness of
breath, facial swelling, oral cavity swelling, shock, cardiac
arrhythmia, respiratory compromise, hypotension
NB
Please ensure that this is
the correct clinical
diagnosis before
proceeding with drug
administration. If in doubt
about diagnosis, seek
advice from the on call
medical officer.
Assess Severity of reaction and differential diagnosis
If anaphylaxis is severe immediately organise transfer to hospital
Administer continuous O2 15L/min via non re-breathing mask
Mild allergic
reaction
Sensations of
warmth
Itching
Rash
Observe for
changes in
severity
Discuss with MO
on call
Moderate allergic
reaction
Erythematous
Urticarial rash
Oedema of face,
neck, soft tissues
0.5 ml Adrenaline
1:1000 (0.5mg) IMI
Observe for changes
in severity
Discuss with MO on
call and organise
transfer to hospital
Administer continuous O2 > 8L/
min
Call Ambulance and transfer
patient to hospital
Assess for signs of hypotension
or respiratory distress
Discuss with MO on call
Signs of respiratory distress?
Administer 0.5 ml Adrenaline
(1:1000 0.5mg) IMI
Severe reaction / Anaphylaxis
Hypotention (shock)
Angioedema
- Oedema of face, neck, soft
tissues
Bronchospasm
- Dyspnoea, Wheeze Cough
Cyanosis
- Shortness of breath
Laryngeal oedema
- Laryngeal stridor, hoarseness
Urticarial rash - Wheals
- Pruritus
Arrhythmia, weak pulse
Laryngeal oedema
Administer 5mg (5mls 1:1000)
nebulised adrenaline with continuous
O2 > 8L/min
Bronchospasm
2.5-5mg nebulised salbutamol
1ml normal saline PRN with O2 > 8L/min
Hypotension systolic BP < 100 mmHg
Rapid fluid resuscitation, normal
saline stat
See Haemorrhage / hypovolaemia
algorithm
38
PRIMARY HEALTH
ANAPHYLAXIS
CLINICAL STREAM
ADRENALINE
STANDING ORDERS
An anaphylactic reaction is an immediate (type 1 IgE mediated)
systemic allergic reaction to allergens including drugs e.g. penicillin, and insect
toxins, e.g. bee stings. It is characterized by widespread vasodilatation and
extravasations of fluid from the vascular compartment into the body's tissues,
especially into the head, neck and chest, and at times the tongue. When
severe, such a reaction is called anaphylaxis. A severe anaphylactoid reaction
is a life-threatening emergency. As in all medical emergencies; initial
management should be ABC of resuscitation, namely: Airway, Breathing and
Circulation. All patients with anaphylaxis should be transferred out to hospital
for medical assessment.
Drug Name
ADRENALINE
Common Brand Names
Adrenaline 1:1000
Strength
1mg/1ml ampoule
Dose
0.5mL IMI
Administration / Route
Intramuscular injection
•
If there has been little or no response to
the initial dose of adrenaline, this may be
repeated at 20 minute intervals depending on
the response of the patient and the severity of
the condition.
•
Adrenaline must be used at the first
suspicion of anaphylaxis. It is safe and
effective, and can be life saving.
Withholding adrenaline due to concerns of
adverse effects can result in death of the
patient.
•
Establish at least one, preferably two IV
lines 18g or larger cannula.
•
All efforts should be made to insert 2
large bore IV cannula (18g or larger) and to
commence Normal Saline.
If there is hypotension replace fluid rapidly
i.e. open IV line valves fully.
39
INDICATIONS
Following clinical recognition of anaphylactic reaction:
Early
•
o
sensations of warmth, itching, especially in the axillae and
groins.or at point of exposure
Progressive
•
o
o
erythematous or urticarial rash
oedema of face, neck, soft tissues
Severe
•
o hypotension (shock) bronchospasm (wheezing)
o laryngeal oedema (dyspnoea, stridor, aphonia, drooling)
o arrhythmia, cardiac arrest.
PRECAUTIONS
High doses, cardiovascular, cerebrovascular, lung disorders including asthma,
Parkinsonism, prostatic hypertrophy.
CONTRAINDICATIONS
N.B. In anaphylaxis, ALL contraindications are relative.
•
Known allergy or hypersensitivity
•
Hyperthyroidism; hypertension; ischaemic heart disease; diabetes;
glaucoma; cardiac dilatation; arrhythmias; cerebral arteriosclerosis
•
Obstetrics when maternal BP > 130/80 mmHg
•
Shock (other than anaphylactic)
•
Organic brain damage.
DRUG INTERACTIONS
Sympathomimetics; vasodilators; tricyclic antidepressants; antihistamines;
thyroid hormones; halothane, cyclopropane, trichloroethylene; MAOIs,
hypoglycaemics.
ADVERSE EFFECTS
Anxiety; restlessness; tachycardia; tremor; weakness; dizziness; headache;
dyspnoea; cold extremities; pallor; sweating; nausea, vomiting; flushing;
disorientation; impaired memory; psychosis; ventricular fibrillation; severe
hypertension.
40
OTHER MEASURES IN THE TREATMENT OF ANAPHYLAXIS
1.
2.
The ABC's of resuscitation - Airway, Breathing and Circulation
Cease administration of any suspected medication or diagnostic material
immediately
3. Administer oxygen by facemask at 15 L/minute
4. Call for an ambulance and a Medical Officer. If unstable, transfer to
hospital
5. Bronchospasm may be relieved or improved by giving nebulised
salbutamol (2.5-5mg solution) and Normal Saline 1:1 ml prn
6. Try to reassure the patient
7. Nebulised adrenaline 5 ml of 1:1000 solution (1 mg/1ml) may be tried in
laryngeal oedema
8. Observe vital signs frequently and, if available, monitor ECG.
DOCUMENTATION
•
Physical Observations including: pulse, blood pressure, respiratory rate,
oxygen saturations and physical assessment in patient notes
•
Type and severity of anaphylactic symptoms
•
Document medication on Standing Order chart.
The nurse must record the administration in black ink on the Standing Order
chart. A Medical Officer must be consulted as soon as possible regarding
ongoing management and this must be documented in the patient’s medical
record.
REFERENCES
Drugdex Drug Evaluations. Available at: http:// www.ciap.health.nsw.gov.au (accessed
August 2007).
41
Chest Pain Algorithm
Conduct Primary Survey – ABCDE
(Refer to: Adult Standing Order, chest pain)
Chest Pain / Angina / Possible Acute Myocardial Ischaemia / Infarction
Symptoms e.g. sweating, sudden orthopnea, syncope, dyspnoea, epigastric discomfort, jaw
pain, arm pain
Be aware: High risk atypical presentations (e.g. diabetes, renal failure, female, elderly or
Aboriginal
Administer O2 at 15L/min via a non-re-breathing mask.
∗
Assess: temperature, pulse, blood pressure, respiratory rate, pulse oximetry.
∗
Assess for signs of shock
∗
Patients who are cool and tachycardic should be considered as being in hypovolaemic
shock until proven otherwise
Yes
Is systolic BP > 90mmHG
Give ½ - 1 tablet GTN
(Anginine) sublingually.
Continue O2 therapy.
No
Give 300 mg *Aspirin PO
If possible perform ECG
Discuss with Medical Officer
Call Ambulance
Give 300mg *Aspirin PO
Continue O2 therapy
Give further ½ to 1 tablet GTN
(Anginine) sublingually, only if
systolic BP remains > 90mnHg
repeat every 3-5 mins (max 3
tablets) Continue O2 therapy
Pain relieved?
Yes
No
No
Pain relieved?
Yes
Insert 16-14g IV cannula
Notify Emergency Department
If possible perform ECG and send
a copy with patient and a copy of
previous ECG’s (if any)
Reassess vital
signs
ECG abnormal
Yes \ Unsure
Notify Medical Officer and
NUM or AHNM
No
Discuss with Medical
Officer regarding further
action
Regularly assess changes in vital signs
Airway, Breathing and Circulation.
Transfer to hospital for further assessment if
ECG changes apparent
*Contraindicated if history of allergy to aspirin, active Gastro-intestinal bleed or taking warfarin
NOTE: If patient has a supply of GTN (Anginine), always replace
43
42
PRIMARY HEALTH
CHEST PAIN
CLINICAL STREAM
GLYCERYL TRINITRATE
STANDING ORDERS
CONTACT MEDICAL OFFICER URGENTLY IF PAIN PERSISTS FOR MORE
THAN 15 MINUTES OR TRANSFER TO LOCAL CASUALTY IF ANY
SUSPICION OF A MYOCARDIAL INFARCT. REMEMBER ABORIGINAL
MALES MAY HAVE HEART ATTACKS IN THEIR EARLY TWENTIES AND
THE ISCHAEMIC PAIN MIGHT BE IN ATYPICAL LOCATIONS.
Angina is the paroxysmal pain caused by transient myocardial ischaemia. The
pain occurs when the oxygen demands of the myocardial tissues exceed the
ability of the coronary vessels to supply the affected area with enough blood to
meet the oxygen needs of the myocardial tissues.
Atherosclerosis of the coronary arteries, vasospasm of the coronary arteries or
a combination of these two factors can be the causation. Investigations in
clinical practice provide limited supporting evidence for Angina, as a resting
ECG can show no cardiac changes, unless there is a history of coronary artery
disease.
If an arrhythmia is present organise immediate transfer of the patient to
hospital.
THE FIRST-AID MANAGEMENT of CHEST PAIN consists of:
1.
Maintenance of the airway,
2.
Oxygen at 10 to 15 L/min and
3.
Administration of Anginine.
Drug Name
GLYCERYL TRINITRATE / GTN
Common Brand Names
Anginine
Strength
600mcg
Dose
600mcg sublingually (half a tablet in the
elderly initially).
Repeat every 3-5 minutes if unresolved.
Administration / Route
PO
•
Sit/lie patient down as GTN may cause
dizziness.
•
Ensure blood pressure is checked prior
to
administration
and
continuing
monitoring and observations after
administration.
•
The advice of a Medical Officer must
43
always be sought, as soon as
practicable,
regarding
further
management. The patient should be
transferred to hospital if the pain persists
after 2 tablets over 10 minutes.
•
Advise patient not to swallow the tablet
and to place the tablet under the tongue
or in the cheek and allow it to dissolve.
•
Advise patient to spit tablet out once the
pain has been relieved.
INDICATIONS
Chest Pain of suspected cardiac origin (Angina or Myocardial Infarction). The
most characteristic features of Acute Myocardial Infarction are:
1. Angina of severe, sustained or unusual intensity
2. Any ischaemic chest pain which does not abate with rest
3. Any angina with a drop in blood pressure or onset of an irregular
pulse
4. Sudden onset of central chest pain which may or may not radiate to
the neck, jaw, arms or back.
The most characteristic features of classic angina are:
1. Retrosternal or banding chest pain precipitated by physical or
emotional exertion
2. Pain is relieved by rest
3. Pain or discomfort may be felt alternatively or additionally in the arms,
epigastrium, jaw or back.
Atypical Angina can present as pain in the jaw, neck, shoulders, arm or
epigastric region.
Other associated features that may be present in acute myocardial infarction or
Angina include:
•
Dyspnoea
•
Nausea
•
Diaphoresis
•
Palpitations
•
Faintness
CONTRAINDICATIONS
•
Blood Pressure <90 mmHg
•
Cerebral Haemorrhage
•
Head Injury
•
Hyper tropic Obstructive Cardiomyopathy
44
DRUG INTERACTIONS
Alcohol, Antihypertensives, Levodopa, Opioid analgesics, Hydralazine,
Calcium channel blockers, Minoxidil, Prazosin, Sympathomimetics, Sildenafil,
Tadalafil, tricyclic antidepressants.
ADVERSE EFFECTS
•
Vascular headache
•
Flushing
•
Tachycardia
•
Dizziness
•
Hypotension
•
Syncope
•
GI upset
•
Restlessness
OBSERVATIONS
•
Pulse
•
Temperature
•
Blood pressure
•
Respiratory rate
•
Oxygen saturation
•
Listen to chest for air entry and wheeze
•
ECG
DOCUMENTATION
•
Document clinical reason for administration in patient’s notes
Monitor and document physical observations including: Pulse, blood
pressure, oxygen saturations, respiratory rate and ECG.
The registered nurse must record the administration in black ink on the
Standing Order chart. A Medical Officer must be consulted as soon as
possible regarding ongoing management and this must be documented in the
patient’s medical record.
•
REFERENCES
MIMS Online. Available at: http:// www.ciap.health.nsw.gov.au (accessed August 2007).
45
PRIMARY HEALTH
CHEST PAIN
CLINICAL STREAM
ASPIRIN
STANDING ORDERS
Aspirin commenced within 24 hours of the onset of an acute MI can be
effective in reducing the overall mortality from acute MI, reduces non-fatal reinfarction and reduces nonfatal stroke.
Drug Name
ASPIRIN
Common Brand Names
Solprin, Disprin
Strength
300mg tabs
Dose
300mg dissolved in 100mls water STAT
Administration / Route
PO with food
•
Caution should be used when
administering to patients with active
gastric bleeding or Asthma
•
Contraindicated in patients with known
hypersensitivity to Aspirin
INDICATIONS
Aspirin is standard therapy for all patients with pain suggestive of acute MI to
prevent coronary re-thrombosis and reducing the incidence of mortality
CONTRAINDICATIONS
Known allergy or hypersensitivity to aspirin or NSAIDS. Active peptic ulcer,
bleeding tendency, severe hepatic dysfunction, third trimester of pregnancy.
DRUG INTERACTIONS
Anticoagulants, hypoglycaemics, uricosurics, methotrexate, NSAIDs, antacids,
frusemide.
46
ADVERSE EFFECTS
Gastro Intestinal irritation, increased bleeding time, sensitivity, rashes,
urticaria, heartburn, nausea and vomiting.
DOCUMENTATION
•
Document clinical reason for administration in patient’s notes.
•
Monitor and document physical observations including: Pulse, blood
pressure, oxygen saturations, respiratory rate and ECG.
The registered nurse must record the administration in black ink on the
Standing Order chart. A Medical Officer must be consulted within 24 hours for
ongoing management and this must be documented in the patient’s medical
record.
REFERENCES
MIMS Online. Available at: http:// www.ciap.health.nsw.gov.au (accessed August 2007).
47
Haemorrhage / Hypovolemia Algorithm
Control any external
bleeding, apply pressure
dressing. Stabilise and
penetrating objects
Conduct Primary Survey – ABCDE
Assess severity of haemorrhage / shock
(Refer to: Adult Standing Order Hypovolemia))
Early Shock (compensated)
Loss of 15% to 25% of blood volume
η
Tachycardia, postural drop in BP,
narrowed pulse pressure, pallor,
thirst, diaphoresis, delayed
capillary refill time > 3 secs,
anxiety, restlessness
η
η
η
η
Administer O2 > 15 litres via non
re-breathing mask
Control external bleeding and
stabilise any penetrating objects,
if present
Insert two large bore IV cannulas
(14-16g)
Administer normal saline 500mls
over 30 minutes
Late Shock (uncompensated)
Loss of > 30% to 45% of blood volume
η
Hypotension, tachycardia,
delayed capillary refill time > 3
secs, cool/cold peripheries
altered level of consciousness
η
η
η
η
η
η
Assess severity and location of injury if
hypovolaemia is secondary to injury.
Stabilise any pelvic or long bone
fractures
Call an Ambulance
Administer O2 15 litres via non rebreathing mask
Control external bleeding and
stabilise any penetrating objects,
if present
Insert two large bore IV cannulas
(14-16g)
Commence IV normal saline 1
litre stat, (titrate to aim for heart
rate <100bpm, systolic blood
pressure > 90 mmHg)
Assess neurological status and
regularly evaluate Airway,
Breathing and Circulation
Organise transfer to hospital
Notify Emergency Department
Notify Medical Officer and NUM and AHNM
49
48
PRIMARY HEALTH
CLINICAL STREAM
HYPOVOLEMIA
STANDING ORDERS
NORMAL SALINE 0.9%
(Sodium Chloride)
Sodium Chloride is a fluid replacement in severe blood loss – more
than 500mLs (approximate area equal to surface of a hospital
towel). Sodium Chloride is infused to a patient with the use of a
wide bore cannula. This procedure can only be undertaken by
nursing staff accredited in inserting a cannula (does not include
scalp vein needle). Normal Saline is an intravenous solution
intended for restoring hydration.
DRUG NAME:
COMMON BRAND NAMES:
STRENGTH:
NORMAL SALINE
Baxter
Normal Saline (0.9%)
DOSE: The dose of Normal Saline is dependant upon the
age, weight and clinical condition of the patient as
well as laboratory determinations. Parenteral drug
products should be inspected visually for particulate
matter and discolouration prior to administration.
Additives may not be compatible.
ADMINISTRATION/ROUTE:
Intravenous infusion via
cannula. Titrate to aim for heart rate <100bpm and
systolic blood pressure >90mm Hg
INDICATIONS:
• Intravenous fluid replacement
• Metabolic acidosis
• Restoring, maintaining NaCl; 3% (hypertonic)
• Severe NaCl depletion
CONTRAINDICATIONS:
• Congestive Cardiac Failure
49
•
•
•
Severe renal impairment
Oedema with Na retention
Raised, normal or slightly decreased electrolyte levels
PRECAUTIONS:
The intravenous administration of Normal Saline can cause fluid
and/or solute overload resulting in dilution of serum electrolyte
concentrations, over hydration, congested states or pulmonary
oedema. The risk of dilution is inversely proportional to the
electrolyte concentration of the infusion.
The effect of the normal saline component on patients with
metabolic or respiratory alkalosis should be monitored closely.
Normal Saline should be administered with extreme caution.
DRUG INTERACTIONS:
Normal Saline should not be administered simultaneously with
blood preparations through the same administration set because of
possibility of coagulation. These products should not be
administered concomitantly with potassium sparing diuretics and
angiotension converting enzymes (ACE) inhibitors. Simultaneous
administration of these drugs can result in severe hyperkalaemia.
ADVERSE EFFECTS:
Allergic reactions or anaphylactic/anaphyloid symptoms such as
localised or general urticaria, skin rash and erythema and
itching/pruritis; skin swelling, peri orbital, facial and/or laryngeal
oedema (Quincke’s oedema); chest tightness, chest pain with
tachycardia or bradycardia; nasal congestion, coughing, sneezing,
bronchospasm and/or difficulty breathing have been reported
during administration of Normal Saline.
Adverse reactions may occur due to the solution of the technique
of administration including fever response or infection at the site of
injection. Prolonged intravenous infusion of this type of product
may cause venous thrombosis or phlebitis extending from the site
of injection, extravasation and hypovolaemia. If an adverse
reaction does occur, discontinue the infusion and evaluate the
patient, institute appropriate therapeutic countermeasures and
save the remainder of the fluid for examiniation if deemed
necessary.
50
OVERDOSE:
Symptoms of overdosage with intravenous solutions are related to
disturbed electrolyte levels and fluid imbalance. Symptoms
indicative of overdose include shortness of breath, peripheral
oedema, nausea, vomiting and diarrhoea, abdominal cramps,
weakness, paraesthesia, paralysis, mental confusion, tachycardia
and other cardiac abnormalities.
Overdose requires immediate clinical assessment, cessation or
slowing of intravenous fluids, laboratory assessment of electrolyte
levels, calculation of fluid balance, electrocardiogram (ECG)
monitoring and commencement of appropriate supportive
treatment.
DOCUMENTATION:
• Document observations, including Glasgow Coma Score in
patients’ notes.
• Document response to treatment
The nurse must record the administration in black ink on the
Standing Order chart. A Medical Officer must be consulted as soon
as possible regarding ongoing management and this must be
documented in the patient’s medical record.
REFERENCES:
MIMS Online. Available at http://www.ciap.health.nsw.gov.au
51
Hypoglycaemia Algorithm
Conduct Primary Survey – ABCDE
(Refer to: Adult Standing Order Hypoglycaemia)
Indications – deteriorating level of consciousness or coma especially in known diabetic
patients, low BGL <4mmol/L)
Consider opioid
overdose if BGL
not < 4mmol/l
(Refer to Opioid
overdose
algorithm)
Administer O2 15 L/min. Check BGL < 4mmol/L)
Altered level of Consciousness?
No
Yes
Talking normally (swallow reflex present)?
Yes
1mg glucagon hypokit SCI
No
Assess response
(post glucagon vomiting is not
unusual)
Give oral glucose drink
Reassess Blood Glucose Levels and
Glasgow Coma Scale.
Yes
Follow the Justice Health Hypoglycaemia
Action Plan (See over page)
Altered level of consciousness?
Responsive to Glucagon?
No
Yes
Administer 50mls of 50%
Dextrose
IVI
Rate of infusion should not exceed
0.5g/kg/hr to avoid glycosuria
Reassess response
No
Assess neurological status and regularly
evaluate Airway, Breathing and Circulation
Assess causation of hypoglycaemic episode.
If concerned, ring Medical Officer and/or
organise transfer to hospital.
Observe and regularly check BGL for 4 hours
Contact MO for advice re ongoing management
Arrange emergency transfer to
hospital
52
Hypoglycaemia Action Plan
What is hypoglycaemia?
Hypoglycaemia (also called a ‘hypo’ or low blood glucose) is when blood
glucose level has dropped too low. Usually this occurs when the level falls
below 4 mmol/L although this can vary. While people taking certain tablets for
their diabetes can experience hypoglycaemia, it is more common in people
who inject insulin.
What are the main causes of hypoglycaemia?
Delaying or missing a meal
Not eating enough carbohydrate
Unplanned physical activity
More strenuous exercise than normal
Drinking alcohol
Too much insulin or tablets
What are the symptoms?
(symptoms vary from person to person)
Weakness, trembling or
shaking
Sweating
Light headedness
Headache
Dizziness
Lack of concentration / behaviour change
Tearful / crying
Irritability
Hunger
Numbness around the lips and fingers
If you feel any of these symptoms, test your blood glucose level. If you are not
able to do this, treat as a hypo.
How is a “hypo” treated?
Have some quick acting carbohydrate:
•
3 glucose tablets.
Plus (only 1 of the following) longer acting carbohydrate:
1 small can baked beans OR 6 small dry biscuits in sealed pack
OR 1/2 sandwich OR 1 glass milk or soy drink OR 1 piece of fruit
OR 2-3 pieces of dried apricots, figs or other dried fruit OR 1
small tub of low fat yogurt.
Wait 10-15 minutes. Retest your blood glucose - if it isn't rising, repeat
treatment with a quick acting carbohydrate as described above. If your next
meal is more than 20 minutes away, eat some longer acting carbohydrate.
Two hypo kits will be issued. The Hypo Kit should only be used in the event of
a hypo. Go to the clinic for replacement Hypo Kit if the kit is used for a hypo or
if the “use by date” on the rations has expired.
Adapted from Diabetes Australia resources,
accessed from
www.diabetesaustralia.com.au
•
53
PRIMARY HEALTH
HYPOGLYCAEMIA
CLINICAL STREAM
GLUCAGON
STANDING ORDERS
Nursing staff may use IM glucagon and IV dextrose for severe hypoglycaemia
under the provisions of this policy.
Be mindful of other causes of unconsciousness e.g. narcotic overdose.
Drug Name
GLUCAGON HYDROCHLORIDE
Common Brand Names
Glucagen Hypokit, Glucagen
Strength
1mg Injection
Dose
1mg SC, IM or IVI
Administration / Route
Subcutaneous, intramuscular or intravenous
injection
If possible check blood glucose and if less
than 4mmol / litre then:
•
If conscious with adequate swallowing
reflex give a glucose drink or jelly
beans.
•
If
level
of
consciousness
is
deteriorating or if unconscious, give
Glucagon SC, IMI or IVI.
Administer IV Dextrose as per
Standing Order.
Give oral carbohydrates when patient has
responded
to
prevent
recurrent
hypoglycaemia.
•
INDICATIONS
If hypoglycaemia is suspected in a known diabetic or level of consciousness is
deteriorating.
CONTRAINDICATIONS
•
Known allergy or hypersensitivity
•
Phaeochromocytoma
•
Insulinoma
•
Glucagonoma
54
PRECAUTIONS
Fasting, adrenal insufficiency, chronic alcohol induced hypoglycaemia.
DRUG INTERACTIONS
•
Warfarin
•
Beta-blockers
•
Insulin (antagonise glucagon)
•
Secondary hypoglycaemia
ADVERSE EFFECTS
•
Nausea and/or vomiting
•
Secondary hypoglycaemia
DOCUMENTATION
•
Document observations, including Glasgow Coma Score (GCS) and
BGL in patient’s notes
•
Document response to treatment.
The registered nurse must record the administration in black ink on the
Standing Order chart. A Medical Officer must be consulted as soon as
possible regarding ongoing management and this must be documented in the
patient’s medical record.
REFERENCES
MIMS Online. Available at: http:// www.ciap.health.nsw.gov.au (accessed August 2007).
55
PRIMARY HEALTH
HYPOGLYCAEMIA
CLINICAL STREAM
DEXTROSE
STANDING ORDERS
Nursing staff may use IM glucagon and IV dextrose for severe hypoglycaemia
under the provisions of this policy.
Be mindful of other causes of unconsciousness e.g. narcotic overdose.
In an emergency situation e.g. respiratory compromise or arrest, follow
resuscitation procedures.
Administration of 50mg Thiamine IMI may be necessary to prevent the
precipitation of acute Wernicke’s encephalopathy in patients with alcohol
dependency and should be administered prior to the administration of Glucose.
Drug Name
Common Brand Names
Strength
Dose
Administration / Route
50% GLUCOSE
50% Dextrose, 50% Glucose BP Injection
50ml Mini-jet Injection
50ml of 50% Glucose IVI. Rate of infusion
should not exceed 0.5g/kg/hr to avoid
glycosuria.
Intravenous injection ONLY.
•
If conscious with adequate swallowing
reflex give 10-20g of glucose orally.
•
If level of consciousness is deteriorating
or if unconscious, give IMI, IVI or SC
glucagon.
•
If comatose or patient’s level of
consciousness does not improve
administer IV Dextrose as per Standing
Order.
•
If comatose, cannulate using 21g scalp
vein set and administer 50 mls of 50%
Dextrose intravenously. Flush cannula
with 10 mls of normal saline 0.9%
intravenously.
•
If patient remains unconscious, contact
medical officer and urgently transfer to a
local hospital.
•
As patient recovers, contact medical
officer for further treatment.
•
NB: extra care should be taken to
avoid local site tissue necrosis
56
INDICATIONS
•
If hypoglycaemia is suspected in a known diabetic or otherwise level
of consciousness is deteriorating
•
Comatose patient
CONTRAINDICATIONS
•
Diabetic (hyperglycaemic) coma
•
Anuria
•
Intraspinal / intracranial haemorrhage
•
Dehydrated delirium tremors
•
Corn (maize) allergy
•
High ischaemic stroke risk
•
Glucose – galactose malabsorption syndrome
DRUG INTERACTIONS
Corticosteroids, check compatibility of additives.
ADVERSE EFFECTS
•
Tissue necrosis if extravasations from vein occurs
•
May aggravate brain damage in head injuries and strokes
•
Fluid, electrolyte, acid-base disturbances
•
Injection site reactions
•
Vitamin B deficiency
•
Anaphylaxis
•
Flushing
May precipitate Wernicke's encephalopathy in alcoholics with
Thiamine deficiency.
DOCUMENTATION
•
•
Document observations, including Glasgow Coma Score (GCS) and
BGL in patient’s notes.
•
Document response to treatment.
The registered nurse must record the administration in black ink on the
Standing Order chart. A Medical Officer must be consulted as soon as
possible regarding ongoing management and this must be documented in the
patient’s medical record.
REFERENCES
MIMS Online. Available at: http:// www.ciap.health.nsw.gov.au (accessed August 2007).
57
Meningococcal Disease Algorithm
Conduct Primary Survey – ABCDE
Ensure Differential Diagnosis assessed
(Refer to: Adult Standing Order Suspected Cases of Meningococcal Disease)
Suspected case of meningococcal disease (Droplet precautions: gloves and mask)
PATIENT with sudden onset of:
ν
Fever, prostration
ν
Nausea, vomiting
ν
+/- Rash (e.g. petechial, purpuric, maculopapular) – check patient’s body carefully
ν
+/- Headache, drowsiness, with or without neck stiffness
ν
Irritability, confusion, seizures, photophobia
Suspect bacterial sepsis
ν
Arrange immediate transfer to hospital by Ambulance
ν
Discuss with Medical Officer on call with view to immediate administration of
penicillin
ν
Notify NUM or Nurse Manager on call
Benzylpenicillin should be withheld ONLY if an individual has a clear history of either an
anaphylactic or an immediate hypersensitivity reaction (such as difficulty in breathing,
angioedema or a generalised urticarial rash) after a previous dose of penicillin, use
Ceftriaxone.
Reconstitute 1.2g Benzylpenicillin with 3.2mls water for injection or
2 X 600mg vials each with 1.6mls water for injection (total 3.2mls)
Administer Benzylpenicillin IMI
or
Ceftriaxone 2g reconstitute 1g in 3.5mls water for injection, administer by deep
intra-gluteal injection, recommend maximum 1 g per side
Assess: temperature, pulse, blood pressure, respirations, O2 saturations
Observe for signs of anaphylaxis
(Refer to: Standing Order Anaphylaxis)
Discuss with Medical Officer on call
Await transfer to hospital
Notify Justice Health,
Population Health Unit
59
58
POPULATION HEALTH
CLINICAL STREAM
STANDING ORDERS
SUSPECTED CASES OF
MENINGOCOCCAL DISEASE
BENZYLPENICILLIN (SODIUM)
Refer to the JH&FMHN Policy for the Management of Suspected
Cases of Meningococcal disease Policy No 1.275.
CLINICAL RECOGNITION OF MENINGOCOCCAL DISEASE:
•
•
•
Meningococcal disease usually presents as meningitis,
septicaemia, or as a combination of the two.
The hallmark of meningococcal septicaemia is a petechial rash.
However, a rash is not always present, especially in the early
stages.
Any patient with a systemic febrile illness should be observed
and reassessed frequently.
DRUG NAME:
BENZYLPENICILLIN (SODIUM)
COMMON BRAND NAMES: BenPen (injection)
STRENGTH/PRESENTATION: 1.2 g vials or 600 mg vials
DOSE:
1.2g IMI STAT
ADMINISTRATION/ROUTE:
Reconstitute with 1.6mls
Water for each 600mg of Benzylpenicillin powder. Dissolve
Benzylpenicillin in Water for Injections and use immediately.
PATIENTS HYPERSENSITIVE
Ceftriaxone 2 x 1g IM
TO PENICILLIN
IMI: dissolve 1g in water for
injection 3.5mL, administer by deep intragluteal injection,
recommend maximum 1g per side.
N.B. Ceftriaxone is usually administered in lignocaine to
minimise pain associated with intramuscular injection. As
lignocaine is not approved for injection without a medical
officer’s approval in Justice Health, and medical officers are
not immediately available on site in all Justice Health
facilities, the Drugs and Therapeutics Committee approved
its reconstitution in water.
59
All Health Centres should have a supply of Benzylpenicillin 1.2g or
600mg x 2, Ceftriaxone 1g x 2 plus Water for Injections x 10.
Reconstitution Benzylpenicillin
Reconstitution
fluid
Intramuscular
For each 600mg
of
Benzylpenicillin
powder
Dissolve in 1.6mL
of water for
injection
Maximum
concentra
tion
300mg /
ml
Recommended
route
As per usual
IM injection
TYPICAL SYMPTOMS AND SIGNS OF MENINGOCOCCAL
DISEASE INCLUDE:
•
Sudden onset of fever
•
Leg pain, cold extremities, and abnormal skin colour (early
signs in children aged under 16 years)
•
Headache
•
Nausea, vomiting
•
Irritability, photophobia, with or without neck stiffness
•
Drowsiness, decreased level of consciousness
•
Swollen or painful joints, difficulty walking
•
Rash, however a rash may not appear until later, may be
haemorrhagic (i.e. petechial or purpuric) or less commonly
maculopapular
•
Signs of sepsis or cardiovascular shock (tachypnoea, fever
or hypothermia)
INDICATIONS:
• If a patient is suspected of having meningococcal disease urgent
transfer by ambulance to hospital and immediate administration
of Benzylpenicillin is essential.
• Any patient with an acute systemic febrile illness, and a petechial
or purpuric rash should receive immediate antibiotic treatment
with Benzylpenicillin.
CONTRAINDICATIONS:
Benzylpenicillin should be withheld only if an individual has a clear
history of either an anaphylactic or an immediate hypersensitivity
reaction (such as difficulty in breathing, angioedema, or a
generalised uticarial rash) after a previous dose of penicillin.
Most people with a penicillin allergy do not have such a history and
can safely be given Benzylpenicillin. If there is a history of either
60
an anaphylactic or an immediate hypersensitivity reaction, do
not administer penicillin, use Ceftriaxone as per the standing
order above. Seek urgent advice from the on-call clinician at the
referral hospital, but do not delay ambulance transfer.
PRECAUTIONS:
Although penicillin’s are generally well tolerated the possibility of
allergic reactions must always be considered. Serious, and
occasionally fatal hypersensitivity reactions (anaphylaxis) have been
reported. Serious anaphylactic reactions require emergency
treatment with adrenaline.
Refer to the Standing Order and Protocol for the management of
Anaphylaxis, and ensure that adrenaline is available.
DRUG INTERACTIONS:
Probenecid, chloramphenicol,
contraceptives.
tetracyclines,
erythromycin,
oral
ADVERSE EFFECTS:
Sensitivity, superinfection, GI upset, renal hepatic, haematological,
CNS effects, fever localized effects.
DOCUMENTATION:
• Physical Observations including: pulse, blood pressure,
respiratory rate, oxygen saturation, and physical assessment
must be noted in patient’s medical record.
The registered nurse must record the administration in ink on the
Standing Order chart. A Medical Officer must be consulted as soon
as possible regarding ongoing management and this must be
documented in the patient’s medical record.
REFERENCES:
Guidelines for the early clinical and public health management of
meningococcal disease in Australia, CDNA, Commonwealth
Department of Health and Aging, 2007
MIMS Abbreviated prescribing Information for BenPen. (accessed
August 2010). Australian Medicines Handbook 2007
61
MIMS online. Available at http://ciap.health.nsw.gov.au (accessed
March 2011)
Therapeutic Guidelines, Revised June 2010 (accessed March 2011).
Available at http://ciap.health.nsw.gov.au
62
63
PRIMARY HEALTH
OPIOID OVERDOSE
CLINICAL STREAM
NALOXONE (NARCAN)
(Likely Opioid Overdose)
STANDING ORDERS
Respiratory depression is a principal feature not only of opioid overdose but
also of overdose of other substances such as sedatives and hypnotics.
Any patient found unconscious with no apparent cause should be treated as a
potential drug overdose.
Any patient who is suspected of being intoxicated or having an altered state of
consciousness should be moved to the main clinic for optimal ongoing clinical
review. Where access remains difficult, arrangements should be made to
transfer the patient to the nearest general hospital, as per normal
organizational protocol.
Where there is any altered state of consciousness oxygen should be
administered via mask at 15 litres per minute. In many instances opioid
overdose can be managed successfully with oxygen administration via mask
without requiring naloxone administration. Oxygen saturation levels should be
monitored using a pulse oximeter where available. Oxygen saturation levels
should be provided to the treating Medical Officer.
Drug Name
NALOXONE
Common Brand Names
Narcan
Strength
2 mg in 5ml minijet
Dosage Regimen
Suspected or known opioid overdose
Administration / Route
Adults:
Initially 2 mg IMI or SCI
Repeat every 2-3 minutes if necessary to a
maximum dose of 10mg
Do not give to persons with a primary head
injury or with known cardiac conditions or if
myocardial infarction is suspected
ADMINISTRATION
In the absence of a Medical Officer, a
Registered Nurse may commence treatment
for suspected drug overdose where there is
no other obvious cause for change in
consciousness in the patient, such as
diabetes or head injury. The effective use of
naloxone allows time to further assess the
patient and to consult for medical advice and
arrange ongoing treatment
64
•
If a patient’s life is assessed to be
seriously at risk due to suspected opioid
overdose, then naloxone is to be used
irrespective of the patient’s wishes or
consent. In emergency circumstances it
is not necessary to seek an order for
enforced medication. This can always
be obtained retrospectively.
•
In cases of buprenorphine suspected
overdose, the dose of naloxone required
is much greater
•
The patient is monitored as per
JH&FMHN&FMHN Drug and Alcohol
Procedure No. W1-Management of
Intoxication and Withdrawal – Broad
Principles
INDICATIONS
Suspected Opioid Overdose
Naloxone is an opioid antagonist. If administered to someone suspected of an
opioid overdose, it effectively and rapidly reverses respiratory depression and
other overdose effects. If administered to a person who is opioid drug free it
exerts little or no pharmacological action.
Naloxone also induces withdrawal symptoms when administered to an opioid
dependent user. In these cases, the naloxone induced withdrawal is more
severe because its opioid blocking effect is immediate -- in unprecipitated
withdrawal the body has some time to compensate for the absence of the drug.
Reversal of opioid overdose effects can occur in as little as one to two minutes.
Naloxone does not produce dependence and has no potential for abuse. There
have been no reported deaths attributed to naloxone overdose. Tolerance to
its antagonist actions does not appear to occur.
Where the opioid overdose is due to methadone or other long acting opioids,
the patient must be monitored for at least four hours as the half life of naloxone
is substantially less than that of methadone and other long-acting opioids.
Therefore the patient may experience respiratory depression again, once the
initial dose of naloxone is no longer effective. These patients may require a
naloxone infusion and should be transported to hospital.
DOCUMENTATION
The nurse must record the administration in black ink on the Standing Order
chart. A Medical Officer must be consulted as soon as possible regarding
ongoing management and this must be documented in the patient’s medical
record.
REFERENCES
MIMS Online. Available at: http:// www.clininfo.health.nsw.gov.au
65
Status Epilepticus Algorithm
Conduct Primary Survey – ABCDE
(Refer to: Adult Standing Order Status Epilepticus)
Indications – a succession of tonic-clonic “grand mal” convulsions without the patient regaining
consciousness
Seizure activity lasting greater than 3
minutes
Seizure activity lasting less than 3
minutes
Administer O2 15L/min via non rebreathing mask
Place patient in recovery position
Regularly assess airway and breathing
Reassure the patient
Assess for signs of injury
Check BGL
Conduct GCS assessment
Administer O2 15L/min via non rebreathing mask
Administer 5mg midazolam (Hypnovel)
IMI- half dose for head injuries,
advanced age, smaller than average size,
CAL and general debility
May be repeated once after 5 minutes if
seizure activity continues
Organise an ambulance to transport to
hospital
Continue monitoring ABC and
maintaining airway with chin lift/jaw thrust
maneuvers, if required
NB. Do not attempt to force an airway into the
mouth of a fitting patient
If able, discuss with Medical Officer
the need for further treatment whilst
awaiting ambulance
Notify NUM or AHNM
Assess differential diagnosis
Consider alcohol / benzodiazepine withdrawal seizure
(Discuss with Drug and Alcohol Medical Officer on call if drug withdrawal seizure suspected)
Discuss with Medical Officer
Monitor GCS for 4 hours post seizure if transfer to hospital is not indicated
67
66
PRIMARY HEALTH
CLINICAL STREAM
STATUS EPILEPTICUS
MIDAZOLAM
STANDING ORDERS
A single epileptic attack is seldom fatal except on the rare occasions when it
causes an accident to the patient, such as drowning or falling from a height.
Convulsions of CLINICAL SIGNIFICANCE, in emergency situations, are almost
always of the tonic-clonic ("Grand Mal”) type; rarely are they of the "complex
partial" type. Midazolam is an extremely potent benzodiazepine and this group
of drugs has the potential for abuse.
"Status epilepticus" is a succession of generalised tonic-clonic ("grand mal")
convulsions, without the patient regaining consciousness. It is potentially fatal,
unless the fits are arrested, because of hypoventilation and/or apnoea. THE
FIRST-AID MANAGEMENT of status epilepticus consists of:
•
•
•
Maintenance of the airway,
Oxygen at 10 to 15 L/min and
Prevention of injury to the patient
If the seizures persists for more then 2-3 minutes, nursing staff are authorised
to administer Midazolam under the following Standing Order.
67
DRUG NAME:
COMMON BRAND NAMES:
STRENGTH:
DOSE:
MIDAZOLAM
Hypnovel
5mg/1ml Ampoule
5mg IMI
With head injuries,advanced age,smaller than average size,CAL and
general debility the dose MUST be Halved
ADMINISTRATION/ROUTE:
Intramuscular injection
•
May be repeated once after 5 minutes if fitting persists up to a
maximum of 10mg
•
Depression of the respiratory centre may result in the need for
assisted ventilation.
•
The advice of a Medical Officer must always be sought, as soon as
practicable, regarding further management. The patient should be
transferred to hospital.
•
Continuous monitoring of the patient during and after administration
is required.
INDICATIONS:
Seizures that continue unabated for more than 2 – 3 minutes.
CONTRAINDICATIONS:
•
Known allergy
•
Myasthenia gravis
•
Shock
•
Coma
•
Acute alcohol intoxication
•
Narrow angle glaucoma
DRUG INTERACTIONS:
•
Alcohol
•
CNS depressants
•
Anaesthetics
•
Cimetidine
•
Erythromycin
•
Sodium Valproate
ADVERSE EFFECTS:
•
Respiratory depression
•
Cardiac/respiratory arrest
68
•
Hypotension
•
Hiccup, cough
•
Elderly – increased risk of over-sedation, ataxia, confusion,
falls,
respiratory depression and short term memory impairment, reduce
dose as above and monitor closely
•
Critically ill – Midazolam elimination half life is prolonged,
reduce dose as above and monitor closely.
DOCUMENTATION:
•
Document clinical reason for administration in patient’s notes.
•
Monitor and document physical observations including: GCS,
pulse, blood pressure, oxygen saturations, and respiratory rate.
The registered nurse must record the administration in black ink on the
Standing Order chart. A Medical Officer must be consulted as soon as possible
regarding ongoing management and this must be documented in the patient’s
medical record.
REFERENCES:
MIMS Online. Available at: http:// www:ciap.health.nsw.gov.au (accessed
2010)
APPENDICIES:
1. A Very Brief Overview of Epilepsy
69
APPENDIX 1: A Very Brief Overview of Epilepsy
Epilepsy is a brief paroxysmal disturbance of cerebral function that occurs
periodically and is due to paroxysmal neuronal discharges resulting in fits that
are often, but not always, accompanied by loss of consciousness.
There are many different forms of epilepsy and attacks may consist of: sudden
onset of sustained muscular contractions (tonic):
o
Rhythmic jerking of the face, trunk, or limbs (clonic)
o
Contractions and jerking (tonic-clonic, or "GRAND MAL")
o
Transient loss of consciousness ("petit mal")
o
A muscular jerk (myoclonus)
o
Sudden impairment of postural tone, causing a falling
attack (atonic or akinetic)
o
Unilateral motor or sensory symptoms (focal)
o
Hallucinations of the special senses and disturbances of
memory or emotion ("complex partial")
o
Tonic-clonic ("GRAND MAL") seizures have the following
features:
o
Patients infrequently have premonitory symptoms, the
"aura", e.g. elation, depression, irritability, headache, odd sensations (e.g.
feeling a breeze)
o
There is apnoea during the tonic phase
o
There is often incontinence of urine
o
Some form of self-injury often occurs e.g. tongue biting, injury to the
head or a limb by striking a hard object etc.
o
There may be incontinence of faeces
o
Stupor and confusion for minutes or hours usually follow
the convulsion.
DRUG WITHDRAWAL FITS and PSEUDO FITS are CLASSICALLY TONICCLONIC ("GRAND MAL"). Management rarely requires more than airway
maintenance and prevention of self-injury. They usually cease in a couple of
minutes with the patient regaining consciousness, partially or completely,
(these times may SEEM longer). Recurrence is not unusual but, again,
observation and maintenance of the airway and prevention of self-injury is all
that is usually necessary. In the rare event that a drug withdrawal fit is so
prolonged and severe that it can be classed as status epilepticus, the above
Standing Order is indicated.
70
Stab Wound Algorithm
Conduct Primary Survey – ABCDE
NOTE: Ensure Personal Protective Equipment is donned
prior to treatment
Assess: temperature, pulse, respiration rate, oxygen saturations and extremity observations
Commence O2 at 15L/minute via non re-breathing mask
Assess wound
Knife or foreign object in wound?
Do not remove.
Stabilise object
with normal saline
soaked gauze
Yes
No
Apply pressure dressing to stop bleeding, or
reassess dressing if already applied, do not
remove
Assess blood loss /
signs of shock
Assess blood loss / signs of shock
Are there signs of shock?
(Refer to: Haemorrhage / hypovolaemia algorithm
Yes
No
Stab wounds to head, neck, chest, back or
abdomen; require urgent transport to hospital for
investigation. Assess extremity injuries for
neurovascular impairment
Does patient require transfer to hospital?
No \ Unsure
Discuss further
management with
Medical Officer
Yes
Insert 16-14g IV
cannula
Organise transport to
hosiptal, notify
Emergency Department
Notify NUM or AHNM
Regularly assess changes in vital
signs, signs of shock, airway,
breathing and circulation
Administer O2 at 15 L/minute via
non re-breathing mask
ϕ
Control external bleeding if
present
ϕ
Insert two large bore IV cannulas
(16-14g)
ϕ
Do not administer fluids for
penetrating trauma unless seen
to be only external haemorrhage
i.e. to a limb
ϕ
Commence IV normal saline at
20ml/kg over 15 minutes (titrate
to aim for heart rate<100bpm,
systolic blood pressure
>90mmHg
Organise urgent transport to hospital
via Ambulance
ϕ
71
71
Suicide Risk / Attempt Algorithm
For completed suicide
Refer to JH Policy 1.120,
Death in Custody
Conduct Primary Survey – ABCDE
Identified as having increased suicide risk factors
Is this an Acute Suicide attempt?
No
Yes
Is patient
expressing
suicidal ideation?
Assess patient
and treat any
injuries
If patient has attempted
hanging, a cervical spine
injury must be suspected.
Apply stiff neck collar and
maintain cervical spine
precautions
Is patient
medically stable?
No
Is patient able to
ensure their own
safety?
No
Activate
Mandatory
Notification Form
No
Yes
Yes
Exclude / stabilise physical
health, mental health and / or
substance use problems
Refer via PAS to appropriate
stream
Consider safe environment /
assessment / group cell
placement
Consider need for human
contact
Assess need for mandatory
notification
Refer to Mental Health
clinician if patient has a
mental health issue
Complete health problem
notification form
Consider assessment / two
out cell placement with
minimal possessions
(JH Policy 1.340,
Accommodation; Clinical
Recommendations (Adult)
Discuss patient with
psychiatrist
Organise transfer to
hospital for further
assessment
Discuss with Medical
Officer
Notify NUM/AHNM
Educate re services and how to
access them
Refer for psychosocial support
(JH Policy 1.1380, Suicidal and
self harm behaviour management)
Ensure ongoing supervision and reassessment for changes in mental
health status
If concerned discuss patient with psychiatrist or Medical Officer
72