* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download File
Survey
Document related concepts
Transcript
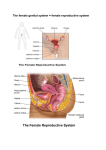
Female Internal Genital Organs Pelvis & Perineum Unit Lecture 4 حيدر جليل األعسم.د Anterior Pelvic Viscera in Female Ureters They cross over pelvic inlet in front of bifurcation of the common iliac artery. It runs downward and backward in front of internal iliac artery and behind the ovary until it reaches the region of ischial spine. It then turns forward and medially beneath base of broad ligament, where it is crossed by uterine artery. Ureter then runs forward, lateral to the lateral fornix of vagina, to enter the bladder. Urinary Bladder Urinary bladder is situated immediately behind pubic bones. Because of the absence of prostate, bladder lies at a lower level than in male pelvis. Neck rests directly on upper surface of urogenital diaphragm. Apex of bladder lies behind symphysis pubis. Base, or posterior surface, is separated by vagina from rectum. Superior surface is related to uterovesical pouch of peritoneum and to body of uterus. Inferolateral surfaces are related in front to retropubic pad of fat and the pubic bones. More posteriorly, they lie in contact with obturator internus muscle above and levator ani muscle below. Female internal Genital Organs Ovary Each ovary is oval shaped, measuring (4X2 cm), and is attached to back of broad ligament by mesovarium. That part of the broad ligament extending between attachment of mesovarium and lateral wall of pelvis is called suspensory ligament of ovary. Round ligament of ovary connects lateral margin of uterus to ovary. Ovary usually lies against lateral wall of pelvis in a depression (ovarian fossa) bounded by external iliac vessels above and by internal iliac vessels behind. Position of ovary is, however, extremely variable, and it is often found hanging down in rectouterine pouch (pouch of Douglas). During pregnancy, enlarging uterus pulls ovary up into abdominal cavity. Female internal Genital Organs Blood Supply of ovary: Arteries: ovarian artery from abdominal aorta at level of 1st lumbar vertebra. Veins: ovarian vein drains into inferior vena cava on right side & into left renal vein on left side. Lymph Drainage: follow ovarian artery & drain into para-aortic nodes at level of 1st lumbar vertebra. Nerve Supply: from aortic plexus and accompanies ovarian artery. Blood supply, lymph drainage, and nerve supply of the ovary pass over pelvic inlet and cross external iliac vessels to reach the ovary by passing through lateral end of broad ligament, part known as suspensory ligament of ovary. Vessels and nerves finally enter hilum of ovary via mesovarium. Uterine Tube (Fallopian Tubes) They are about 10 cm long and lie in upper border of broad ligament. Each connects peritoneal cavity to uterine cavity & divided into 4 parts Infundibulum: funnel-shaped lateral end that projects beyond broad ligament and overlies ovary. Its free edge has several fingerlike processes (fimbriae) which are draped over the ovary. Ampulla: widest part of the tube. Isthmus: narrowest part of the tube and lies just lateral to the uterus. Intramural part: is the segment that pierces the uterine wall. Arteries: uterine artery & ovarian artery from abdominal aorta. Veins: uterine vein & ovarian vein. Lymph Drainage: internal iliac and para-aortic nodes. Nerve Supply: Sympathetic and parasympathetic nerves from inferior hypogastric plexuses. Function: site of fertilization, Transport & nutrition of Fertilised ovum. Uterus It is a hollow, pear-shaped organ with thick muscular walls. In young nulliparous adult, it measures (8 cm long, 5 cm wide and 2.5 cm thick). Fundus is part of uterus that lies above entrance of uterine tubes. Body is part of uterus that lies below entrance of uterine tubes. Cervix is the narrow part of uterus. It pierces anterior wall of vagina and is divided into supravaginal and vaginal parts of cervix. Cavity of uterine body: is triangular in coronal section, but it is merely a cleft in sagittal plane. Cavity of cervix (cervical canal): communicates with cavity of body through internal os and with that of vagina through external os. Before the birth of first child, external os is circular. In a parous woman, vaginal part of cervix is larger, and external os becomes a transverse slit so that it possesses an anterior & posterior lips. Function: site for reception, retention, and nutrition of the fertilized ovum. Relations of uterus Anteriorly: body of uterus is related anteriorly to uterovesical pouch & superior surface of bladder. Vaginal cervix is related to anterior fornix of vagina. Supravaginal cervix is related to superior surface of bladder. Posteriorly: body of uterus is related posteriorly to rectouterine pouch (pouch of Douglas) with coils of ileum or sigmoid colon within it. Laterally: body of uterus is related laterally to broad ligament & uterine artery and vein. Supravaginal cervix is related to ureter as it passes forward to enter bladder. Vaginal cervix is related to lateral fornix of vagina. Uterine tubes enter superolateral angles of uterus, and round ligaments of ovary and of uterus are attached to uterine wall just below this level. Positions of Uterus In most women, long axis of uterus is bent forward on long axis of vagina (anteversion of uterus). Also, Long axis of body of uterus is bent forward at level of internal os with long axis of cervix (anteflexion of uterus). Thus, in erect position and with bladder empty, uterus lies in an almost horizontal plane. In some women, fundus and body of uterus are bent backward on vagina so that they lie in rectouterine pouch (pouch of Douglas). Uterus is therefore retroverted. If body of the uterus is, in addition, bent backward on cervix, it is also retroflexed. Structure of Uterus Uterus is covered with peritoneum except anteriorly, below level of internal os, where peritoneum passes forward onto bladder. Laterally, there is also a space between attachment of layers of broad ligament. Muscular wall (myometrium) is thick and made up of smooth muscle supported by connective tissue. Mucous membrane (endometrium) is continuous above with mucous membrane lining uterine tubes and below with mucous membrane of cervix. Endometrium is applied directly to muscle with no submucosa. Parametrium is visceral pelvic fascia surrounding supravaginal part of cervix and in which uterine artery crosses ureter on each side of the cervix. Uterus Arterial Blood Supply: mainly uterine artery & partially ovarian artery. Arteries: Uterine artery: is a branch of internal iliac artery. It reaches uterus by running medially in base of broad ligament. It crosses above ureter at right angles and reaches cervix at level of internal os. Then it ascends along lateral margin of uterus within broad ligament and ends by anastomosing with ovarian artery. Ovarian Artery: assists in supplying uterus & gives off small descending branch to cervix and vagina. Veins: Uterine vein follows artery into internal iliac vein. Lymph Drainage: Lymph vessels from fundus: accompany ovarian artery and drain into para-aortic nodes. Vessels from body & cervix: into internal & external iliac lymph nodes. Few vessels follow round ligament of uterus into superficial inguinal LNs Nerve Supply: (Sympathetic and Parasympathetic) inferior hypogastric plexuses. Supports of Uterus Uterus is supported mainly by tone of levatores ani muscles and condensations of pelvic fascia which form three important ligaments. A. Levatores Ani Muscles and the Perineal Body: perineal body is important in maintaining integrity of pelvic floor; if damaged during childbirth, prolapse of pelvic viscera may occur. Perineal body lies in perineum between vagina and anal canal. It is slung up to pelvis by levatores ani & supports vagina and, indirectly, uterus. Supports of Uterus B. Pelvic fascia: (Transverse Cervical, Pubocervical & Sacrocervical Lig.) They are subperitoneal condensations of pelvic fascia on upper surface of levatores ani muscle. They are attached to cervix and vault of vagina and play an important part in supporting uterus & keeping cervix in its correct position. Transverse Cervical Ligaments: (Cardinal) pass to cervix and upper end of vagina from lateral walls of pelvis. Pubocervical Ligaments: consist of two firm bands of connective tissue that pass to cervix from posterior surface of pubis & positioned on either side of bladder neck. Sacrocervical Ligaments: two firm fibromuscular bands of pelvic fascia that pass to cervix and upper end of vagina from lower end of sacrum. They form two ridges, one on either side of rectouterine pouch (pouch of Douglas). Supports of Uterus Broad ligaments of uterus are drap-like folds of peritoneum around the uterine tubes. Its upper border is related to uterine tubes and lower border is related to uterine artery. Round ligament of uterus extends between superolateral angle of uterus, through deep inguinal ring and inguinal canal, to subcutaneous tissue of labium majus. It helps keep uterus anteverted (tilted forward) and anteflexed (bent forward) but is considerably stretched during pregnancy. Broad & round ligaments of uterus are lax structures, and uterus can be pulled up or pushed down for a considerable distance before they become taut. So, they play a minor role in supporting uterus. Vagina It is a muscular tube that extends upward and backward from vulva to uterus. It measures about 8 cm long and has anterior & posterior walls, which are normally in apposition. At its upper end, anterior wall is pierced by cervix, which projects downward and backward into vagina. Upper half of vagina lies above pelvic floor and lower half lies within perineum. Vaginal lumen, which surrounds cervix, is divided into four fornices: anterior, posterior, right lateral, & left lateral. Vaginal orifice in a virgin possesses a thin mucosal fold Hymen perforated at its center. Relations of Vagina Anteriorly: bladder above and to urethra below. Posteriorly: upper 1/3 of vagina is related to rectouterine pouch (pouch of Douglas), middle 1/3 to ampulla of rectum & Lower 1/3 is related to perineal body (separates it from anal canal) Laterally: In its upper part, it is related to ureter; its middle part is related to anterior fibers of levator ani, as they run backward to reach perineal body and hook around anorectal junction (sphincter vaginae). Contraction of fibers of levator ani compresses walls of vagina together. In its lower part, vagina is related to urogenital diaphragm and bulb of vestibule. Functions: • female genital canal • excretory duct for menstrual blood • forms part of birth canal Vagina Blood Supply: Arteries: vaginal artery, a branch of internal iliac artery, and vaginal branch of uterine artery supply vagina. Veins: vaginal veins form a plexus around vagina that drains into internal iliac vein. Lymph Drainage: upper third of vagina drains to external and internal iliac nodes, middle third drains to internal iliac nodes, and lower third drains to superficial inguinal nodes. Nerve Supply: inferior hypogastric plexuses. Supports of the Vagina: Upper part of vagina is supported by levatores ani muscles and transverse cervical, pubocervical, and sacrocervical ligaments. Middle part of vagina is supported by urogenital diaphragm. Lower part of vagina, especially posterior wall, is supported by perineal body. Pelvic Peritoneum in Females Peritoneum passes down from anterior abdominal wall onto upper surface of urinary bladder. It then runs directly onto anterior surface of uterus, at level of internal os. Peritoneum now passes upward over anterior surface of body and fundus of uterus and then downward over posterior surface. It continues downward and covers upper part of posterior surface of vagina, where it forms anterior wall of rectouterine pouch (pouch of Douglas). Peritoneum then passes onto front of rectum, as in the male. In the female, the lowest part of abdominopelvic peritoneal cavity in erect position is rectouterine pouch Thank You