* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download AN OPEN STUDY TO ASSESS THE SAFETY AND TOLERABILITY
Survey
Document related concepts
Transcript
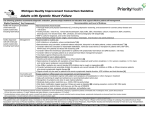
British Journal of Rheumatology 1996;35(suppL l):56-60 AN OPEN STUDY TO ASSESS THE SAFETY AND TOLERABILITY OF MELOXICAM 15 mg IN SUBJECTS WITH RHEUMATIC DISEASE AND MELD RENAL IMPAIRMENT P. J. R. BEVIS,* HA. BIRDt and G. LAPHAM* *BoehringerIngelheimLtd, Ellesfield Industrial Estate, Bracknell, Berkshire RG128YS and f Chapel Allerton Hospital, Leeds, University of Leeds, Chapeltown Road, Leeds, West Yorkshire LSI'4SA SUMMARY Meloxicam is a new non-stcroidal anti-inflammatory drug (NSAID) which has shown potent anti-inflammatory properties but good gastrointestinal (GI) and renal tolerability. The safety and tolerability profile of orally administered meloxicam 15 mg given once daily over a 28 day treatment period in renally impaired patients with rheumatic disease is presented here. A total of 25 patients (aged 43-78 yr, mean age 70 yr) with rheumatic disease and mild renal impairment were enrolled in this multicentre, open-label study, with 22 patients completing the 28 day treatment period. The median estimated creatinine clearance and ^-acetyl-P-glucosaminidase/creatinine ratios (a marker of renal tubular damage) recorded at day 14, day 28 or 4-7 days after meloxicam treatment was terminated, were not statistically significantly different from baseline values. There was no evidence of accumulation of meloxicam. Overall, meloxicam was well tolerated. The most common adverse events were GI complaints of abdominal pain and dyspepsia. No adverse events related to the urinary system, or increases in serum urea or potassium were recorded. The results suggest that meloxicam, 15 mg once daily, does not further compromise renal function or result in accumulation of meloxicam over this treatment period in patients with pre-existing mild renal impairment. Non-steroidal anti-inflammatory drugs (NSAIDs), Rheumatic disease, Meloxicam, Renal function, Renal impairment, Tolerability. KEY WORDS: MELOXICAM is an enolic acid derived non-steroidal anti-inflammatory drug (NSAID) developed for the treatment of rheumatic disease. In animal studies [1] meloxicam has shown potent anti-inflammatory properties in combination with good gastrointestinal (GI) and renal tolerability. Promising results, suggesting these characteristics, have also been observed in early clinical studies conducted in patients with rheumatoid arthritis (RA) and osteoarthritis (OA) [2-6]. In a double-blind comparison over a treatment period of 6 months, patients with RA treated with meloxicam 7.5 mg had no changes in creatinine or urea plasma levels, whereas there was a significant increase in these parameters in patients treated with naproxen 750 mg [7]. Like other NSAIDs, meloxicam is highly plasma protein bound (>99%). Following oral administration, meloxicam is extensively metabolized in the liver and excreted approximately equally via renal and hepatic routes [8]. All metabolites are pharmacologically inactive. Steady-state plasma levels of meloxicam are achieved within 3-5 days after the start of once-daily oral administration [8]. This study represents the first clinical study of meloxicam conducted in patients with rheumatic disease and pre-existing renal impairment. The design of this study is based on a review of similar studies conducted with other NSAIDs over a 2-week period [9-11]. This study was conducted over a 4-week period with a washout period at the end of treatment in order to observe at least a partial recovery in renal function Correspondence to: Dr P. J. R. Bevis, Boehringer Ingclhnm Ltd, Ellesfield Industrial Estate, Bracknell, Berkshire RG12 8YS. should an initial fall in renal function be observed in association with meloxicam treatment. Improvement in renal function has been observed in previous studies following withdrawal of NSAID therapy [12]. Renal function was assessed by two methods commonly used in studies of this nature: estimated creatinine clearance and TV-acetyl-P-glucosaminidase (NAG)/creatinine ratio. Consequently, the aim of this study was to evaluate the safety and tolerance of meloxicam, 15 mg once daily, in patients with rheumatic disease and mild renal impairment (creatinine clearance 25-60 ml/min). PATIENTS AND METHODS This study was an open-label, multicentre study in which patients received a meloxicam 15 mg capsule once daily, with a glass of water after food, for 28 days. Further details of the six centres involved, and the number of patients entered by each centre, are given in the Acknowledgements. All patients had a diagnosis of arthritic disease, defined as RA, either seropositive or seronegative, OA or other rheumatic disease requiring NSAID therapy and had mild renal impairment as defined by an estimated creatinine clearance of 25-60 ml/min. Pretreatment phase and exclusion criteria Patients attended an initial pretreatment screening examination consisting of weight and height measurements, and blood and urine sampling for routine monitoring and determination of creatinine clearance. Patients were excluded from the study, at this stage, for the following reasons: participation in clinical trials O 1996 British Society for Rheumatology BEVIS ETAL: MELOXICAM IN RENAL IMPAIRMENT 57 with an investigational new drug in the month prior to the screening visit and during the study period itself; participation in any previous studies with meloxicam; pregnancy and risk of pregnancy; clinical evidence of severe cardiac, pulmonary, GI, hepatic or neurological disease; allergic bronchial asthma; a known hypersensitivity to analgesics, antipyretics and NSAIDs; clinical evidence of active peptic ulceration during the previous 6 months; requirement for dialysis; taking concomitant piroxicam or tenoxicam; treatment with anticoagulants, lithium, angiotensin-converting enzyme (ACE) inhibitors or hydantoins; clinically relevant abnormal baseline laboratory results not associated with rheumatic disease or renal impairment; treatment with second-line antixheumatic drugs such as methotrexate or sulphasalazine which had not been stabilized for at least 1 month prior to screening; treatment with cyclosporin, pencillamine or gold which had not been stabilized for at least 3 months prior to screening. Patients were allowed to continue with second-line antirheumatic drugs at a dose stabilized for at least 1 month before the study or not otherwise stipulated in the exclusion criteria. Paracetamol 500 mg or coproxamol (dextropropoxyphene 32.5 mg and paracetamol 325 mg) were supplied as rescue medication (dose limited to eight tablets per day) for pain relief when appropriate, during washout and treatment periods. A second screening visit was conducted no less than 4 days after the first screening visit and patients were not included in the study if the calculated creatinine clearance values differed by greater than 10 ml/min on the two occasions. excreted in patients with renal dysfunction [14, 15]. The excretion of NAG is a sensitive indicator of early renal damage [15], and was therefore measured as one of the secondary endpoints. Dipstick urine tests were performed at a screening visit, the first and last treatment follow-up days, and at either 4 or 7 days after meloxicam treatment was terminated. Trough plasma meloxicam concentrations (blood samples taken prior to dosing) were also determined on the three follow-up days. Meloxicam plasma levels were determined using a validated, specific high-performance liquid chromatography (HPLQ method with a lower quantification limit of 0.05 g/ml [U. Busch, data on file, Boehringer Ingelheim]. Comparisons of creatinine clearances and NAG/ creatinine clearance ratios before and after treatment and plasma meloxicam trough levels during treatment were statistically analysed by paired Mests and 95% confidence intervals for within-patient differences. Washout and treatment phase Patients who were eligible for the study and taking a NSAID entered a washout period (4 days for nabumetone and 3 days for other NSAIDs) after the second screening visit. After the washout phase, patients entered the meloxicam treatment phase and underwent a pretreatment examination including weight, height, blood pressure and heart rate measurements, a complete physical examination and laboratory tests. Patients were then followed up at day 14, 21 and 28 of meloxicam treatment. A further clinic visit was arranged 4 or 7 days after meloxicam treatment was finished so that renal function assessments could be made after treatment washout. This study was conducted according to the Declaration of Helsinki (amended 1983) and guidelines for Good Clinical Practice. Sample size estimation It was calculated that a sample size of 25 evaluable patients would be needed to detect a difference in creatinine clearance of at least 15 ml/min by means of a paired f-test (a = 5%, P = 10%, two-tailed). Assessment of renal function Blood and urine samples were collected at the two screening visits and at each follow-up visit Creatinine clearance was estimated from serum creatinine levels using equations described by Mawer et al. [13]. Renal function was also assessed using estimation of NAG derived from a 4 h urine collection and comparison with creatinine clearance. NAG is an enzyme found in high concentrations in the epithelial cells of renal tubules and it has been observed that increased quantities are Tolerability and efficacy assessments Adverse events occurring during the study were recorded by the investigator and coded using the WHO-ARTL system. Adverse events were also recorded during the study by intensity (mild, moderate or severe) and frequency. In addition, the mean time to onset of each event was calculated. At either 4 or 7 days after meloxicam treatment discontinuation, patients and investigators completed a questionnaire where efficacy and tolerability of meloxicam treatment were rated on a scale of very well, well, average, poorly or very poorly. RESULTS Twenty-five patients, five men and 20 women, mean age 70 yr (range 43-78 yr), were included in the intentto-treat population. Twenty-two patients completed the 28 day study-treatment period. Three patients were withdrawn from the study prematurely: one due to an adverse event (abdominal pain) thought to be related to meloxicam, one was lost to follow up and for the third no reason was specified by the patient. Baseline characteristics relating to demographics, disease characteristics and concomitant treatment are listed in Table I. The majority of patients suffered from either RA (63%) or OA (29%), with the remaining 8% of patients suffering from other rheumatic diseases. A mean duration of 12 yr was recorded for all arthritic conditions. Renal function assessments Assessments of renal function conducted throughout the study period revealed no deterioration in renal function in this group of patients with mild renal impairment. Creatinine clearances and NAG/creatinine STUDIES ON MELOXICAM (MOBIQ 58 TABLE I Patient characteristics Parameter TABLE II Creatinine clearance (ml/min) No. (%) patients Number of patients Age (yr) Mean sx>. Median Sex Male Female Duration of rheumatic Mean disease (yr) SJ>. Median Type of rheumatic Rheumatoid arthritis i Osteoarthritis Mined connective tissue Duration of renal disease (yr) Aetiology of renal disease Ankylosing spondylitis n Mean SJ>. Median Age related Mixed connective tissue disease Possible diabetes mellitus Investigation of glornerular nephritis Chronic pyelonephritis Nephrocalcinosis Unknown Number of patients reporting at least one concomitant therapy Antihypertensives Diuretics Antarids/antiulccrarjt P*ychotropics Anti-inflammatories Analgesics 25* 70 7 71 5(20) 20(80) 12.0 8.5 11.3 15(63) 7(29) 1(4) 1(4) 24 1.8 1.7 1.7 4(18) 1(5) 1(5) 1(5) 1(5) 1(5) 13(59) 22* No. of patients Visit Baseline Day 14 Day 21 Day 28 Last visit (days 32/35) 25 24 22 22 22 Mean 48.1 46.7 50.0 48.9 50.7 (NS) (NS) (NS) (NS) Median 11.0 10.6 10.6 50.4 49.0 54.9 50.5 52.1 9.7 10.9 NS, difference from baseline not statistically significant. TABLEm NAG/creatinine ratio (umol/min/g) • No. of Mean SJ>. patients Visit Baseline Day 14 Day 21 Day 28 19* 20 18 18 9.16 9.68 (NS) 9.50 (NS) 10.26 (NS) Median 7.28 10.30 9.53 9.05 6.79 6.99 6.97 6.71 T h e shortfall in collected results for evaluation of NAG/creatinine ratios resulted in smaller comparison groups at later study visits. NS, difference from baseline not statistically significant 21(84) 7(28) 5(20) 6(24) 5(20) 4(16) 3(12) •Aetiology of renal disease unknown in two patients. ratios were compared at baseline (before treatment initiation) and at 14, 21 and 28 days of meloxicam, 15 mg once daily, treatment. Creatinine clearances are presented in Table II. There was no significant difference in the median creatinine clearance recorded at baseline (50.4 ml/min) compared to 14, 21 or 28 days of meloxicam treatment. Increased median NAG/ creatinine ratios were recorded at days 14, 21 and 28 of treatment compared with baseline values; however, the differences were not statistically significant (Table HI). No rises in serum urea or potassium were observed throughout the study. Trough plasma meloxicam levels There were no statistically significant differences in mean trough plasma meloxicam levels recorded at study days 14 (1.72 M£/ml), 21 (1.71 ng/ml) and 28 (1.52ug/ml). Adverse events Overall adverse events assessed by the investigator as probably, possibly or definitely related to meloxicam treatment were recorded in 5% of patients, with GI disorders occurring most frequently (Table IV). No serious adverse events or GI perforations, ulcers or TABLE IV Adverse events assessed by investigator as drug related, intent-to-treat population Adverse event Gastrointestinal Abdominal pain Epigastric pain Dyspepsia Headache Rash No. of patients (%) 3(12) 1(4) 1(4) 1(4) 1(4) 1(4) bleeds were reported. One patient was withdrawn from the study experiencing epigastric pain of moderate intensity 3 days after starting meloxicam treatment. There were no clinically significant abnormal trends in haematological or biochemical parameters recorded at any study day. Efficacy and tolerability The majority of patients tolerated their medication 'very well' or 'well' (96% as assessed by the patient, 88% as assessed by the investigator) and efficacy was assessed as 'very good' or 'good' (52% as assessed by the patient and 75% as assessed by the investigator). Use of rescue analgesia during the study was minimal DISCUSSION This study is the first to investigate the effects of a new NSAID, meloxicam, in older patients with rheumatic disease and mild renal impairment. Clinical studies of meloxicam have been conducted largely in patients with normal renal function and a very favourable safety profile has been observed. Studies with other NSAIDs have indicated that some BEVIS ETAL.: MELOXICAM IN RENAL IMPAIRMENT patients treated with NSAID therapy show an asymptomatic, reversible impairment of renal function [12], characterized by reductions in creatinine clearance and corresponding rises in plasma creatinine, urea and potassium. Meloxicam has shown good renal tolerability in early preclinical studies [1] and in a clinical double-blind trial vs naproxen [7]. The occurrence of adverse renal events induced by NSAIDs in general has been extensively reviewed [16-18]. The majority of renal adverse events observed in association with NSAIDs result from the inhibition of cyclooxygenase (COX) leading to a decreased concentration of the vasodilating prostaglandins, PGE2 and prostacyclin, within the kidney. These mediators are responsible for maintaining renal plasma flow and glomerular filtration rate [19]. Consequently, NSAID intervention may cause acute intrarenal haemodynamic changes in patients whose renal blood flow is dependent on prostaglandins, and this can result inreversibleacute renal failure. Certain patients are particularly at risk of NSAID-associated renal adverse events, such as patients with reduced circulating volume, the elderly and those with pre-existing renal dysfunction [20]. Allergic reactions, such as interstitial nephritis, have also been reported [16, 18]. Other studies have considered the effects of various NSAIDs, given over a short term (11 days-3 months), on renal function in patients with rheumatic disease and minor renal dysfunction [9-11]. In an 11 4ay study comparing ibuprofen 800 mg td.s., sulindac 200 mg b.d. and piroxicam 20 mg o.d., only ibuprofen showed changes in renal function necessitating premature withdrawal [11]. In a 4-week study of naproxen, increasing the dose at 2 weeks after initiation resulted in small, transient changes in renal function [10]. In a 3-month study of tenoxicam, creatinine clearances were significantly lower after 12 weeks, with the NAG/creatining ratio showing a trend toward improvement at week 12 [9]. In this study of meloxicam IS mg once daily for 28 days, no significant differences between creatinine clearance or NAG/creatinine ratios measured at baseline and during treatment were observed. Recently, two isomers of COX, known as COX-1 and COX-2, have been identified [21]. COX-1 is a constitutive COX found in the gastric mucosa and intrarenally where it is involved in maintaining the haemodynamic balance [22]. COX-2 is inducible in conditions associated with the acute inflammatory response. It is likely that preferential selectivity for one COX isomer over another is implicated in the differing incidence of renal toxicity observed between various NSAIDs [20]. Interestingly, meloxicam has shown preferential selectivity for the inducible COX-2 over constitutive COX-1 [23, 24]. Over the 28 day treatment period trough meloxicam plasma levels remained similar, indicating a lack of accumulation in patients with mild renal impairment. Meloxicam undergoes extensive hepatic metabolism and the pharmacologically inactive metabolites are excreted approximately equally via the kidney and liver. 59 Only trace amounts, <1%, are eliminated unchanged in the urine and faeces [8]. In addition, like other NSAIDs, >99% meloxicam is plasma protein bound [8]. Reassuringly, no serious adverse events were reported during the study and the most common adverse events—abdominal pain and dyspepsia—were among those previously observed in patients with normal renal function [2-4]. In addition, and importantly, no renal adverse events occurred in any patient, and no laboratory changes (serum creatinine, serum urea or serum potassium) indicative of deteriorating renal impairment were recorded at any time during the study. ACKNOWLEDGEMENTS We would like to thank the following investigators involved in this trial: Dr J. Belch, NineweUs Hospital Medical School, Dundee (six patients); Dr P. J. Prouse, Basingstoke District Hospital, Basingstoke (one patient); Dr B. E. Bourke, St George's Hospital, London (five patients); Dr B. Williams, University Hospital of Wales, Cardiff (10 patients); Dr H. A. Bird, Royal Bath Hospital, Harrogate (seven patients); Dr D. L. Scott, Homerton Hospital, London (four patients). REFERENCES l.Engelhardt G, Homma D, Schlegel K, Utzmann R, Schnitzler Chr. Anti-inflammatory, analgesic, antipyretic and related properties of meloxicam, a new non-steroidal anti-inflammatory agent with favourable gastrointestinal tolerance. Inflamm Res 1995;44:423-33. 2. Huskisson EC, Ghozlan R, Kurthen R, DegneT FL, Bluhmki E. A long term study to evaluate the safety and efficacy of meloxicam therapy in patients with rheumatoid arthritis. BrJ Rheumatol 1996;35(suppl. l):29-34. 3. Regjnster JY, Distel M, Bluhmki E. A double-blind study to compare the efficacy and safety of meloxicam 7.5 mg and meloxicam 15 mg in patients with rheumatoid arthritis. Scand J Rheumatol 1994;Snppl 98:abstract no. 112. 4. Hosie J, Distel M, Bluhmki E. A six month trial comparing meloxicam 7.5 mg with diclofenac 100 mg SR in osteoarthritis. Rheumatol Eur 1995;24(suppL 3):abstract no. E49. 5. Lemmel EM, Boltcn W, Burgos-Vargas Retal \ doubleblind placebo controlled study of 7.5 mg and 15 mg of meloxicam in patients with rheumatoid arthritis. Scand J Rheumatol 1994jSuppl 98:abstract no. 111. 6. Lund B, Distel M, Bluhmki E. A double-blind placebo controlled study of three different doses of meloxicam in patients with osteoarthritis (OA) of the knee. Scand J Rheumatol 1994;Snppl 98:abstract no. 117. 7. Wojtulewski JA, Schattenkirchner M, Barcel6 P r t a / . A six-month double-blind trial to compare the efficacy and safety of meloxicam 7.5 mg daily and naproxen 750 mg daily in patients with rheumatoid arthritis. Br J Rheumatol 1996;35(suppl. l):22-8. 8. Schmid J, Busch U, Heinzel G, Bozler G, Kaschke S, Kummer M. Meloxicam: pharmacokinetics and metabolic pattern after intravenous infusion and oral administration to healthy subjects. Drug Me tab Disp 1995^3:1206-13. 9. Bird HA, Clarke AK, Fowler PD, Little S, Podgorski MR, Steiner J. An assessment of tenoxicam, a nonsteroidal antiinflammatory drug of long half-life, in patients with impaired renal function suffering from osteoarthritis or rheumatoid arthritis. Clin Rheumatol 1989;8:453-60. 60 STUDIES ON MELOXICAM (MOBIC) 10. Watson WA, Freer JP, Katz RS, Basch C. Kidney function during naproxen therapy in patients at risk for renal insufficiency. Semin Arthritis Rheum 1988;17(suppl. 2):12-6. 11. Whelton A, Stout RL, Spilman PS, Klassen DK. Renal effects of ibuprofen, piroxicam, and sulindac in patients with asymptomatic renal failure. Ann Intern Med 1990; 112:568-76. 12. Unsworth J, Sturman S, Lunec J, Blake DR. Renal impairment associated with non-steroidal anti-inflammatory drugs. Ann Rheum Dis 1987;46:233-6. 13. Mawer EG, Knowles BR, Lucas SB, Stirlanol RM, Tooth JA. Computer assisted prescribing of kanamycin for patients with renal insufficiency. Lancet 1972;i:12-5. 14. Ellis BG, Tucker SM, Thompson AE, Price RG. Presence of serum and tissue forms of 7V-acetyl-beta-glucosaminidase in urine from patients with renal disease. Clin Chim Ada 1975;64:195-202. 15. Dieppe PA, Doyle DV, Burry HC. Renal damage during treatment with antirheumatic drugs. Br MedJ 1978;2:664. 16. Clive DM, Stoff JS. Renal syndromes associated with nonsteroidal antiinflammatory drugs. N Engl J Med 1984;310:563-72. 17. Blackshear JL, Napier JS, Davidman M, Stillman MT. Renal complications of nonsteroidal antiinflammatory drugs: identification and monitoring of those at risk. Semin Arthritis Rheum 1985;14:163-75. 18. Henrich WL. Nephrotoxicity of nonsteroidal antiinflammatory agents. Am J Kidney Dis 1983;ll:478-84. 19. Vane JR, Botting RM. New insights into the mode of action of anti-inflammatory drugs. Inflamm Res 1995; 44:1-10. 20. Anon. Relative safety of oral non-aspirin NSAIDS. Curr Probl Pharmacol 1994;2(h9-12. 21. Xie W, Robertson DL, Simmons DL. Mitogen-inducible prostaglandins G/H synthase: a new target for nonsteroidal antiinflammatory drugs. Drug Dev Res 1992;25: 249-65. 22. Appleton I, Tomlinson A, Willoughby DA. Inducible cyclooxygenase (COX-2): a safer therapeutic target? Br J Rheumatol 1994^3:410-2. 23. Engelhardt G, B6gel R, Schnitzler Chr, Utzmann R. Meloxicam: Influence on arachidonic acid metabolism. Part I. In vitrofindings.Biochem Pharmacol 1996;51:21-8. 24. Engelhardt G, Bogel R, Schnitzler Chr, Utzmann R. Meloxicam: influence on arachidonic acid metabolism. Part II. In vivo findings. Biochem Pharmacol 1996;51: 29-38.