* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Sinha (presentation)
Survey
Document related concepts
Transcript
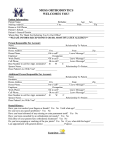
Understanding Hospitalization Among Insured Women Tara Sinha and Sapna Desai Self Employed Women’s Association (SEWA) Research Conference on Microinsurance University of Twente April 11-13, 2012 Location of Study The National Insurance VimoSEWA Cooperative – Gujarat, India – Voluntary MI scheme since 1992. – Offers health, life, accident and asset insurance • Health microinsurance requires 24 hosp’n – Aimed at women workers in the informal economy and their families – Urban and rural 2 Research Issue and Question • Research Issue: Higher rate of hospitalization among insured compared to uninsured persons • Research question: Does higher hospitalization among insured urban women for common illnesses mean improved access to health care or unnecessary hospitalization? 3 Data (1/2) Mixed Methods 1. Study situated in a larger study 2. Baseline survey 954 insured and 980 uninsured households in rural and urban areas – random selection 3. Ten case studies of insured urban women hospitalized for common illnesses – systematic sampling 4. Five doctor interviews 5. Administrative data from Vimo SEWA 4 Data (2/2) Issues examined in paper 1. Comparing insured and uninsured on • Incidence of illnesses and common illnesses*** • Rates for all hospitalization • Rates for hospitalization for common illnesses 2. Factors affecting hospitalization decision • • • Deterrents Precipitating Factors Facilitating Factors 5 Baseline Survey Findings (1/2) Urban adult women reporting illness in last month and type of illness (%) 6 Baseline Survey Findings (2/2) Urban adult women reporting hospitalization in last 6 months and reasons for hospitalization (%) 6 4.7 (2.94 6.0 2.8 (2.23.4) 2 0 Insured Uninsured 20 18 16 14 12 10 8 6 4 2 0 18 4 0 Fever 5 4 0 Diarrhoea Malaria Insured Uninsured 7 Profile of Cases (1/2) No. Days in Yrs. with Hosp. Insurance Previous claims Age Reason Claim paid for hosp’n (Rs.) 1 1 8 0 46 Viral Fever 2 3 4 5 2 2 2 2 3 4 4 5 0 0 0 0 48 35 41 54 Acute Gastro Viral Fever 1,973 1,915 2,000 3,977 6 2 6 1 (resp'y tract inf.) 32 Viral Fever 2,605 7 2 7 1 (husband's cataract) 54 Viral Fever 4,085 8 9 10 3 3 4 3 5 5 0 3 (RTI, VF) 1 (uterine fibroid) 37 35 50 Viral Fever 1,548 1,848 3,654 Viral Fever Fever Viral Fever Acute Gastro 995 8 Case Study Findings (1/3) Deterrents: Fear, Household disruption and costs All had sought out-patient treatment at non-listed hospital before hosp’n (except one acute case) Precipitating Factors - Minor persisting inappropriate treatment - Minor turning acute improper adherence - Acute symptoms 9 Case Study Findings (2/3) Facilitating Factors 1. Insurance – Insured going to listed hospital for consultation – Insured more willing to be hospitalized 2. Providers’ Perspective - Criteria for admission - Perception of members as having poor living conditions, poor awareness - If patient willing, admission covers risk 10 Case Study Finding (3/3) Given: a)Six of ten cases first time admissions b)Two of four previous claims for non-common illnesses c) Nine of ten cases sought out patient care at non-listed hospital prior to hospitalization d)Deterrents to hospitalization 1. Strong indication of poor quality primary care 2. Little indication of member moral hazard 3. Indication of insurance promoting health care seeking in hospital/improved access 4. Adverse member selection a possibility 11 5. Provider moral hazard a possibility Implications for Practice and Policy Health Microinsurance Include out-patient care? Only catastrophic illness? Sustainability vs. need Health Systems – Quality of Care Poor quality of primary care Should insurance be a substitute for lack of universal health care? Women’s Health and Health Education Need for education re. preventive and ‘promotive’ health Need for education re. symptoms, tests done, diagnosis, first line of treatment 12 Discussion Points 1. Future research How best can one integrate the health perspective into health microinsurance research? 2. Design of Health MI Programme Is inclusion of out-patient care needed to prevent hospitalization for common illnesses? 3. Health Education Can health education prevent hospitalization for common illnesses? 13 THANK YOU 14