* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Heart Anatomy Approximately the size of your fist Location
Survey
Document related concepts
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
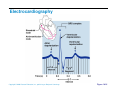
Electrocardiography wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Coronary artery disease wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Atrial septal defect wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Heart arrhythmia wikipedia , lookup
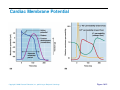
Dextro-Transposition of the great arteries wikipedia , lookup
Transcript
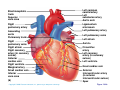
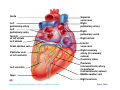
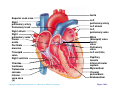
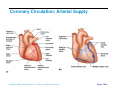
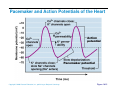
Heart Anatomy Approximately the size of your fist Location Superior surface of diaphragm Left of the midline Anterior to the vertebral column, posterior to the sternum Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Heart Anatomy Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.1 Coverings of the Heart: Anatomy Pericardium – a double-walled sac around the heart composed of: The visceral layer or epicardium lines the surface of the heart A superficial fibrous pericardium A deep two-layer serous pericardium The parietal layer lines the internal surface of the fibrous pericardium They are separated by the fluid-filled pericardial cavity Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Coverings of the Heart: Physiology The pericardium: Protects and anchors the heart Prevents overfilling of the heart with blood Allows for the heart to work in a relatively frictionfree environment Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Pericardial Layers of the Heart Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.2 Heart Wall Epicardium – visceral layer of the serous pericardium Myocardium – composed of aerobic muscle (contractile layer) Composed of cardiac muscle bundles Fibrous skeleton of the heart – crisscrossing, interlacing layer of connective tissue Endocardium – endothelial layer of the inner myocardial surface Lines the heart chamber and is continuous with the endothelial linings of the blood vessels Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Brachiocephalic trunk Superior vena cava Left common carotid artery Left subclavian artery Aortic arch Right pulmonary artery Ligamentum arteriosum Left pulmonary artery Ascending aorta Pulmonary trunk Right pulmonary veins Right atrium Right coronary artery (in coronary sulcus) Anterior cardiac vein Right ventricle Marginal artery Small cardiac vein Inferior vena cava (b) Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Left pulmonary veins Left atrium Auricle Circumflex artery Left coronary artery (in coronary sulcus) Left ventricle Great cardiac vein Anterior interventricular artery (in anterior interventricular sulcus) Apex Figure 18.4b Aorta Left pulmonary artery Left pulmonary veins Auricle of left atrium Left atrium Superior vena cava Right pulmonary artery Right pulmonary veins Right atrium Great cardiac vein Inferior vena cava Posterior vein of left ventricle Right coronary artery (in coronary sulcus) Coronary sinus Apex Posterior interventricular artery (in posterior interventricular sulcus) Middle cardiac vein (d) Right ventricle Left ventricle Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.4d Aorta Superior vena cava Right pulmonary artery Pulmonary trunk Right atrium Right pulmonary veins Fossa ovalis Pectinate muscles Tricuspid valve Right ventricle Chordae tendineae Trabeculae carneae Inferior vena cava (e) Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Left pulmonary artery Left atrium Left pulmonary veins Mitral (bicuspid) valve Aortic valve Pulmonary valve Left ventricle Papillary muscle Interventricular septum Myocardium Visceral pericardium Endocardium Figure 18.4e Atria of the Heart Atria are the receiving chambers of the heart Each atrium has a protruding auricle Atria are relatively small, thin walled chambers Atria contribute little to the propulsive pumping of the heart Blood enters right atria from superior and inferior venae cavae and coronary sinus Blood enters left atria from pulmonary veins Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Ventricles of the Heart Ventricles are the discharging chambers of the heart Make up most of the volume of the heart Trabeculae carnae are irregular ridges of myocardium Papillary muscles are involved with valve function Right ventricle pumps blood into the pulmonary trunk Left ventricle pumps blood into the aorta Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Pathway of Blood Through the Heart and Lungs Right atrium tricuspid valve right ventricle Right ventricle pulmonary semilunar valve pulmonary arteries lungs Lungs pulmonary veins left atrium Left atrium bicuspid valve left ventricle Left ventricle aortic semilunar valve aorta Aorta systemic circulation Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Pathway of Blood Through the Heart Pulmonary circuit is involved with gas exchange Systemic circuit pumps oxygenated blood to the body The two ventricles have unequal work loads Right ventricle: short, low-pressure circulation Left ventricle: long, high-pressure circulation, 5x more resistance than r. ventricle Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Coronary Circulation Blood in the heart provides little nourishment to the heart Coronary circulation is the shortest circulation in the body Provided by the r. & l. coronary arteries arising from the base of the aorta & encircling the heart in the coronary sulcus These vessels lie in the epicardium and send branches inward towards the myocardium Venous blood is collected by the coronary veins following the same path as the arteries leading to the coronary sinus and then the r. atrium Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Coronary Circulation: Arterial Supply Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.7a Heart Valves Heart valves ensure unidirectional blood flow through the heart Atrioventricular (AV) valves lie between the atria and the ventricles & prevent backflow into the atria when ventricles contract R. AV: tricuspid valve (3 cusps) L. AV: bicuspid valve (2 cusps aka mitral valve) Chordae tendineae anchor AV valves (in the closed position) to papillary muscles Papillary muscles contract just prior to ventricular contraction Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Heart Valves Aortic & pulmonary semilunar (SL) valves prevent backflow into the associated ventricles Made of 3 cusps Ventricular contraction forces valves open Backflow fills the cusps thus moving (and closing them) backward Due to low back pressure, they are not reinforced with cordae tendinae Atrial contraction “pinches” off venae cavae and the pulmonary veins preventing substantial backflow through them Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Heart Valves Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.8a, b Heart Valves Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.8c, d Atrioventricular Valve Function Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.9 Semilunar Valve Function Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.10 Microscopic Anatomy of Heart Muscle Cardiac muscle is striated, short, fat, branched, and interconnected Contracts via the sliding filament mechanism Connective tissue is found in the intercellular space The connective tissue endomysium is connected to the fibrous skeleton and acts as both tendon and insertion The plasma membrane of adjacent muscle fibers interlock at intercalated discs The discs contain anchoring desmosomes & gap junctions Cardiac cells are electrically coupled through these gap junctions 30% of the cell volume is mitochondria 70% of the cell is myofibrils containing typical sarcomeres Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Microscopic Anatomy of Cardiac Muscle Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.11 Cardiac Muscle Contraction Heart muscle: Is stimulated by nerves and is self-excitable (automaticity) Contracts as a unit Has a long (250 ms) absolute refractory period (skeletal muscle = 1-2 ms) Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Cardiac Contraction Cardiac muscle contraction is similar to skeletal muscle contraction: Depolarization opens a few fast voltage-gated Na+ channels Presence of T-tubules Ca++, troponin binding, sliding myofilaments Cardiac muscle contraction differs from skeletal muscle contraction by: Sarcoplasmic reticulum Ca++ release: 20% Ca++ from extracellular space (slow Ca++ channels) 80% Ca++ from S.R. K+ permeability decrease preventing rapid repolarization As long as Ca++ is entering, contraction continues After 200ms, Ca++ channels close and K+ channels open Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Heart Physiology: Intrinsic Conduction System Autorhythmic cells: Initiate action potentials Have unstable resting potentials called pacemaker potentials Use calcium influx (rather than sodium) for rising phase of the action potential Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Energy & Electrical Requirements The heart relies exclusively on aerobic respiration Will use glucose and fatty acids, whichever is available The heart does not rely on the nervous system to contract However, autonomic nerve fibers can alter the basic rhythem Setting the basic rhythem: Intrinsic Conduction System: Presence of gap junctions “In house” conduction Consists of non-contractile cardiac cells that initiate and distribute impulses throughout the heart Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Action potential Initiation by Autorhythmic Cells Autorhythmic cells do not maintain a stable resting membrane potential Rather, they continuously depolarize drifting towards threshold initiating the action potential This is due to ion channels in the sarcolemma Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Action potential Initiation by Autorhythmic Cells Hyperpolarization closes K+ channels and opens slow Na+ channels At 40 mV, Ca++ channels open producing the rising phase of the action potential and reversal of the membrane potential Repolarization, as in skeletal muscle, reflects an increase in K+ permeability and efflux from the cell Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Pacemaker and Action Potentials of the Heart Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.13 Cardiac Membrane Potential Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.12 Heart Physiology: Sequence of Excitation 1) Sinoatrial (SA) node (located in the r. atrium) generates impulses about 100 times/minute Sets pace for the heart as a whole (pacemaker) 2) Atrioventricular (AV) node delays the impulse approximately 0.1 second 3) Impulse passes from atria to ventricles via the atrioventricular bundle Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Heart Physiology: Sequence of Excitation 4) AV bundle splits into two pathways in the interventricular septum (bundle branches) Bundle branches carry the impulse toward the apex of the heart 5) Purkinje fibers carry the impulse to the heart apex, ventricular walls, and papillary muscles Ventriclular contraction begins at the apex and moves superiorly SA node: 100x/min (dominates) AV node: 50x/min AVbunde (Purkinje fibers): 30x/min Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Cardiac Intrinsic Conduction Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.14a Heart Excitation Related to ECG SA node generates impulse; atrial excitation begins SA node Impulse delayed at AV node AV node Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Impulse passes to heart apex; ventricular excitation begins Bundle branches Ventricular excitation complete Purkinje fibers Figure 18.17 Extrinsic Innervation of the Heart Heart is stimulated by the sympathetic cardioacceleratory center Heart is inhibited by the parasympathetic cardioinhibitory center Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.15 Extrinsic Innervation of the Heart Cardiac centers are located in the medulla oblongata Cardioacceleratory center projects to sympathetic neurons in the T1-T5 level of the spinal cord Cardioinhibitory center sends impulses to the parasympathetic dorsal vagus nucleus in the medulla Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Electrocardiography Electrical activity is recorded by electrocardiogram (ECG) Electrical currents generated in the heart spread throughout the body 3 waves (deflections) P wave corresponds to depolarization of SA node thru the atria. QRS complex corresponds to ventricular depolarization T wave corresponds to ventricular repolarization Atrial repolarization record is masked by the larger QRS complex P-Q interval is the time from the beginning of atrial excitation to the beginning of ventricular excitation S-T segment is the time when the ventricle is depolarized Q-T interval is the beginning of ventricular depolarization thru ventricular repolarization Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Electrocardiography Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.16 Cardiac Cycle Cardiac cycle refers to all events associated with blood flow through the heart Systole – contraction of heart muscle Diastole – relaxation of heart muscle Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Heart Sounds Two sounds can be distinguished when the thorax is ausculated (listened to) w/ stethescope They are associated w/ the closing of heart valves First sound occurs as AV valves close and signifies beginning of systole Second sound occurs when SL valves close at the beginning of ventricular diastole Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Heart Sounds Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.19 Phases of the Cardiac Cycle Ventricular filling – mid-to-late diastole Heart blood pressure is low as blood enters atria and flows into ventricles AV valves are open but drift to closed position as blood fills ventricle (80%) Atrial systole fills remaining 20% of ventricle Atrial systole: depolarization (Pwave) Atria contract, rise in atrial pressure Ventricle in final part of diastole phase Atrial diastole Ventricles depolarize (QRS complex) Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Phases of the Cardiac Cycle Ventricular systole Atria are in diastole Ventricles begin contracting Rising ventricular pressure results in closing of AV valves Ventricular ejection phase opens semilunar valves Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Phases of the Cardiac Cycle Early diastole (following T wave) Ventricles relax SL valves close w/ backflow from aorta and pulmonary arteries When blood pressure on the atrial side excedes that in the ventricles, the AV valves open and ventricular filling begins again Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Phases of the Cardiac Cycle Notes: Blood flow thru the heart is controlled totally by pressure changes Blood flows down pressure gradients toward the lower pressure Right side is low pressure Left side is high pressure Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Cardiac Output (CO) and Reserve CO is the amount of blood pumped by each ventricle in one minute CO is the product of heart rate (HR) and stroke volume (SV) HR is the number of heart beats per minute SV is the amount of blood pumped out by a ventricle with each beat Cardiac reserve is the difference between resting and maximal CO Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Cardiac Output: Example CO (ml/min) = HR (75 beats/min) x SV (70 ml/beat) CO = 5250 ml/min (5.25 L/min) Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Regulation of Stroke Volume SV = end diastolic volume (EDV; fill) minus end systolic volume (ESV; contraction) EDV = End Diastolic Volume. Amount of blood collected in a ventricle during diastole ESV = End Systolic Volume. Amount of blood remaining in a ventricle after contraction Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Factors Affecting Stroke Volume Most important factors are: Preload – amount ventricles are stretched by contained blood (affects EDV) Contractility – cardiac cell contractile force due to factors other than EDV (affects ESV) Afterload – back pressure exerted by blood in the large arteries leaving the heart (affects ESV) Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Frank-Starling Law of the Heart Preload, or degree of stretch, of cardiac muscle cells before they contract is the critical factor controlling stroke volume Slow heartbeat and exercise increase venous return to the heart, increasing SV by allowing more time to fill Blood loss and extremely rapid heartbeat decrease SV Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Preload and Afterload Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Figure 18.21 Extrinsic Factors Influencing Stroke Volume Contractility is the increase in contractile strength, independent of stretch and EDV Enhanced contractility results in increased ejection from the heart (SV) Increase in contractility comes from: Increased sympathetic stimuli Certain hormones Ca2+ and some drugs Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Extrinsic Factors Influencing Stroke Volume Afterload: back pressure exerted by arterial blood The pressure that must be overcome for ventricles to eject blood Hypertension (high blood pressure) reduces the ability of ventricles to eject blood More blood remains in the heart after systole which increases ESV and decreases SV Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Regulation of Heart Rate Autonomic Nervous System is the most important controller NE binds to B-adrenergic receptors (GPCRs) in the heart causing threshold to be reached more quickly accelerating relaxation phase Pacemaker fires more rapidly, heart rate increases Also enhances Ca++ entry into contractile cells ESV & EDV fall (less time to fill) Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Heart Contractility and Norepinephrine Sympathetic stimulation releases norepinephrine and initiates a cyclic AMP second-messenger system Extracellular fluid Norepinephrine β1-Adrenergic receptor Adenylate cyclase Ca2+ Ca2+ channel Cytoplasm GTP GTP 1 GDP ATP cAMP Active protein kinase A Ca2+ Inactive protein kinase A 3 Ca2+ 2 Enhanced actin-myosin interaction Troponin uptake pump binds to Ca2+ SR Ca2+ channel Cardiac muscle force and velocity Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Sarcoplasmic reticulum (SR) Figure 18.22 Regulation of Heart Rate: Autonomic Nervous System Sympathetic nervous system (SNS) stimulation is activated by stress, anxiety, excitement, or exercise Parasympathetic nervous system (PNS) stimulation is mediated by acetylcholine and opposes the SNS PNS dominates the autonomic stimulation, slowing heart rate and causing vagal tone E.g. cutting the vagus nerve results in increased heart rate equal to that of the pacemaker (100 beats/min) Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Atrial (Bainbridge) Reflex Atrial (Bainbridge) reflex Increased atrial filling leads to increased heart rate by stimulating both the SA node and atrial stretch receptors This leads to reflex adjustments causing increased stimulation of the heart Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Chemical Regulation of the Heart The hormones epinephrine and thyroxine increase heart rate Intra- and extracellular ion concentrations must be maintained for normal heart function Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings Here endth the lesson Copyright © 2006 Pearson Education, Inc., publishing as Benjamin Cummings