* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Dysuria - coreproblems
Swinging (sexual practice) wikipedia , lookup
Hookup culture wikipedia , lookup
Sexual reproduction wikipedia , lookup
Sex and sexuality in speculative fiction wikipedia , lookup
Female ejaculation wikipedia , lookup
Sexual attraction wikipedia , lookup
Human female sexuality wikipedia , lookup
Human mating strategies wikipedia , lookup
Female promiscuity wikipedia , lookup
Sex in advertising wikipedia , lookup
Sexual ethics wikipedia , lookup
Lesbian sexual practices wikipedia , lookup
History of human sexuality wikipedia , lookup
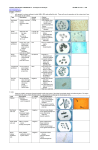
Dysuria Is painful micturition from urethral or bladder inflammation, typically from infection Strangury Is pain in the urethra referred from the base the of the bladder, associated with constant distressing desire to urinate even when there is little urine to void. Causes include; a stone, an indwelling catheter, cystitis, prostatitis and bladder cancer. Structure of the urinary tract Defence mechanisms against infections History Stinging/burning? Urgency? Change in smell of urine? Incontinence? Blood in urine? Abdominal pain? Frequency? Back pain? Regular flushing during voiding, removes organisms from the distal urethra Antibacterial secretions into urine and urethra Previous episodes of dysuria? Previous sexually transmitted diseases? Sexual history Firstly, set the agenda and state that you would like to ask some questions about sexual health, making it clear why asking for this information is relevant to the patient’s complaint. Make a simple statement such as, “I would like to ask you some personal questions about your sex life. Would that be okay?” When the patient has given you a verbal or non-verbal signal that he or she is happy to proceed, use the following structured approach: (1) When did you last have sex/sexual intercourse? (2) Was it with a man or a woman? (3) Was the person a casual or regular partner? (4) Where was the partner from, and what is his or her ethnicity? (5) In which country did you have sex? (6) What kind of sex did you have? (7) For each type—for example, oral, vaginal, anal—did you use a condom? (For heterosexual sex: was any contraception used? Relate to risk of pregnancy when asking about last menstrual period in gynaecology history). Assess whether they were the active/insertive partner or passive/receptive partner, as appropriate. (8) Does/did your partner have any symptoms? (9) When did you last have sex with someone different? Return to question 2. Repeat this for all sexual contacts in at least the preceding 12 weeks. Tip: never assume the sex of previous partners. For men who report recent sexual activity with women, it might be useful to ask if they have ever had sex with men in the past. (10) Have you ever had any previous sexually transmitted infections? (11) Have you ever had a sexual health check up before? (12) Have you, or have any of your sexual partners, ever injected drugs or shared injecting drug equipment? For women, have you ever had sex with a gay or bisexual man? For men, ask about any history of sex with men, as per point (9). (13) Have you ever had an HIV, hepatitis, syphilis test before? (Assess risk and offer tests as appropriate) (14) Have you been vaccinated against hepatitis B, or have you ever had hepatitis? (Assess risk and offer vaccination if appropriate) Investigations urinary dipstix; midstream urine; cervial swab/smear; urethral swab Sexually transmitted diseases NHS (Venereal Diseases) Regulations 1974 Allows limited disclosure of information for contact-tracing in the case of sexually transmitted diseases. Such disclosure can only be made to a doctor, or to someone working on a doctor’s instruction in connection with treatment or prevention. It forbids those working in a genito-urinary clinic to inform an insurance company of a patient’s sexually transmitted disease – even with the patient’s consent. GP’s are not routinely informed of the patient’s attendance at such clinics, although the patient may request that the GP be informed. When the first PN discussion takes place, a plan should be agreed with the index patient about which contacts to contact and, if so, how this should be done. All contacts in the appropriate lookback interval should be included. All contacts include those considered not traceable, as well as those who had attended a service for management of the relevant infection before the index patient was first seen. In deciding whether a contact is traceable, appropriate use of all information sources should be considered. Common index conditions Urinary tract infection >105 organisms/ml of fresh MSU Sites: Urethra Urethritis Baldder Cystitis Prostate Prostatitis Renal pelvis pyelonephritis UTIs are… Uncomplicated- normal renal tract + function Complicated- abnormal renal/GU tract, decreased renal function, impaired host defense, virulent organisms e.g. staph aureus NB. Assume UTI in men is complicated until proven otherwise Recurrent UTI- further infection different organism Relapse UTI- further infectionsame organism Organisms- in community >70% e. coli, <4% in hospital Other: staph saprphylicus, proteus mirabilis, Rarer: enterococcus faecalis, klebsiella, candida albicans, staph. Aureus Symptoms: Cystitis- frequency, dysuria, urgency, strangury, haematuria, suprepubic pain Prostatitis- flu-like symptoms, low backache, few urinary symptoms, swollen/tender prostate on DRE Acute pyelonephritis- high fever, rigors, vomiting, loin pain, tenderness, oliguria (if acute kidney injury) Signs: fever, abdominal or loin tenderness, foul smelling urine. Occasionally distended bladder, enlarged prostate Tests: Dipstick, MSU, MC+S, bloods-FBC, U+E, CRP and blood cultures, imaging- ultrasound or IVU/cystoscopy if failure to respond, recurrence, persistent haematuria, children Treatment: Fluids, urinate often, Cystitis- trimethoprim/cefalexin, 2nd line ciprofloxacin or co-amoxiclav Acute pyelonephritis- cefuroxime Prostatitis- ciprofloxacin Urinary tract infection in children Structual abnormalities of urinary tract identify children for investigation who are at the most risk of renal damage. Such children would be considered to be those who: have a known antenatal renal anomaly are infants are boys have had more than one UTI have had septicaemia have had a prolonged clinical course or fever >48 hours have a family history of reflux have unusual organisms (i.e. not E. coli). An initial ultrasound will identify: serious structural abnormalities and urinary obstruction renal defects. o Multicystic renal dysplasia o Autosomal recessive polycystic kidney disease o Autosomal dominant polycystic kidney disease o Horseshoe kidney o Duplex kidney o Hydronephrosis- relflux from anomaly of the vesicoureteric junction