ICD-9 CM codes relevant to the diagnosis of Depression*
... http://www.cdc.gov/nchs/icd9.htm. Published copies of ICD-9-CM are available from a variety of sources and should be found in any medical library. From the ...
... http://www.cdc.gov/nchs/icd9.htm. Published copies of ICD-9-CM are available from a variety of sources and should be found in any medical library. From the ...
Mental Health in Schools (Rohr)
... Be aware of your environment Collaborative Processing Have plan in place ...
... Be aware of your environment Collaborative Processing Have plan in place ...
disorders usually first diagnosed in infancy, childhood, or adolescence
... • Different from autism because no significant delay in language & communication • Some idiosyncratic features similar to autism; repetitive patterns of behavior, interests and ...
... • Different from autism because no significant delay in language & communication • Some idiosyncratic features similar to autism; repetitive patterns of behavior, interests and ...
Personality Disorder
... • Read the case study of Judy Smith. • Analyze the case to determine how Judy Smith suffers from a psychological disorder by answering the questions on the back of your paper. • Keep in mind the definitions of – Atypical (Deviant): behavior differing from the norm – Disturbing (Distressful): causing ...
... • Read the case study of Judy Smith. • Analyze the case to determine how Judy Smith suffers from a psychological disorder by answering the questions on the back of your paper. • Keep in mind the definitions of – Atypical (Deviant): behavior differing from the norm – Disturbing (Distressful): causing ...
201lecture32010Somat..
... flaws of face or head • Symptoms of depression and characteristics associated with OCD common in people with body dysmorphic disorder ...
... flaws of face or head • Symptoms of depression and characteristics associated with OCD common in people with body dysmorphic disorder ...
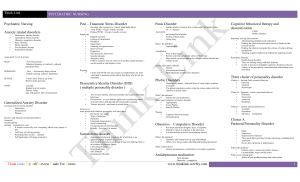
PSychiatric NurSing - Think Link
... Avoid challenging activities – confusion and overwhelm the client Do not argue or change the delusional thinking – redirect the client to a reality based subject Example: Hearing Voices - acknowledge the voice – face with reality – medication ...
... Avoid challenging activities – confusion and overwhelm the client Do not argue or change the delusional thinking – redirect the client to a reality based subject Example: Hearing Voices - acknowledge the voice – face with reality – medication ...
Abnormal Psychology
... bad habits learned early on in life. Biological explanations look at the lower than normal stress hormones in antisocial personality disordered persons as responsible for their low responsiveness to threatening stimuli. Other possible causes of personality disorders may include disturbances in f ...
... bad habits learned early on in life. Biological explanations look at the lower than normal stress hormones in antisocial personality disordered persons as responsible for their low responsiveness to threatening stimuli. Other possible causes of personality disorders may include disturbances in f ...
Abnormal Psychology
... and allows them to remain undismayed at the proximity of "normal" to average and ...
... and allows them to remain undismayed at the proximity of "normal" to average and ...
Chpt_13_Psychologica..
... How do we decide when a set of symptoms are severe enough to be called a disorder that needs treatment? Can we define specific disorders clearly enough so that we can know that we’re all referring to the same behavior/mental state? Can we use our diagnostic labels to guide treatment rather than to s ...
... How do we decide when a set of symptoms are severe enough to be called a disorder that needs treatment? Can we define specific disorders clearly enough so that we can know that we’re all referring to the same behavior/mental state? Can we use our diagnostic labels to guide treatment rather than to s ...
Chapter 3 CLASSIFICATION OF MENTAL DISORDERS This chapter
... Schizophrenia is the archetypal psychosis. The symptoms of this disorder include hallucinations, delusions, reduced ability to think logically (thought slippage), behavioural signs such as the holding of bizarre postures, the loss of the ability to experience emotions and spontaneity, social withdra ...
... Schizophrenia is the archetypal psychosis. The symptoms of this disorder include hallucinations, delusions, reduced ability to think logically (thought slippage), behavioural signs such as the holding of bizarre postures, the loss of the ability to experience emotions and spontaneity, social withdra ...
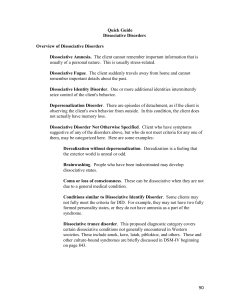
Quick Guide
... observing the client's own behavior from outside. In this condition, the client does not actually have memory loss. Dissociative Disorder Not Otherwise Specified. Client who have symptoms suggestive of any of the disorders above, but who do not meet criteria for any one of them, may be categorized h ...
... observing the client's own behavior from outside. In this condition, the client does not actually have memory loss. Dissociative Disorder Not Otherwise Specified. Client who have symptoms suggestive of any of the disorders above, but who do not meet criteria for any one of them, may be categorized h ...
Class 8: Mental Illness and Diagnosis
... mirroring those of psychiatric disorders – The psychiatric disorder is not diagnosed if the symptoms disappear upon treatment of the medical condition ...
... mirroring those of psychiatric disorders – The psychiatric disorder is not diagnosed if the symptoms disappear upon treatment of the medical condition ...
Disorders
... Cognitive-behavioral model: Disorders result from learning maladaptive ways of thinking and behaving. ...
... Cognitive-behavioral model: Disorders result from learning maladaptive ways of thinking and behaving. ...
Mood Stabilizers in the Treatment of Bipolar Disorder: High Yield
... For less ill patients monotherapy with lithium, valproate or antipsychotic (olanzapine*) Mixed episodes = valproate over lithium Benzodiazepines (short term) Antidepressants should be d/c if possible If first line med fails, add another first line med ECT ...
... For less ill patients monotherapy with lithium, valproate or antipsychotic (olanzapine*) Mixed episodes = valproate over lithium Benzodiazepines (short term) Antidepressants should be d/c if possible If first line med fails, add another first line med ECT ...
Personality Disorder
... • Read the case study of Judy Smith. • Analyze the case to determine how Judy Smith suffers from a psychological disorder by answering the questions on the back of your paper. • Keep in mind the definitions of – Deviant: behavior differing from the norm – Distressful: causing misery or suffering to ...
... • Read the case study of Judy Smith. • Analyze the case to determine how Judy Smith suffers from a psychological disorder by answering the questions on the back of your paper. • Keep in mind the definitions of – Deviant: behavior differing from the norm – Distressful: causing misery or suffering to ...
An Overview of Mood Disorders/Depression
... person will also show mild psychotic behaviors. Suicidal ideation is also common, and the greatest risk of not treating Major Depressive Disorder is completed suicide. Persistent Depressive Disorder (Dysthymia). Dysthymia is often considered a milder form of Major Depression, yet the greatest sympto ...
... person will also show mild psychotic behaviors. Suicidal ideation is also common, and the greatest risk of not treating Major Depressive Disorder is completed suicide. Persistent Depressive Disorder (Dysthymia). Dysthymia is often considered a milder form of Major Depression, yet the greatest sympto ...
Psychological factors affecting other medical
... • A general medical symptom or disorder is present • Psychological or behavioral factors negatively affect the medical condition in one or more of the following ways, such that the factors: -Pose additional health risks for the patient -Aggravate the underlying pathophysiology of a medical condition ...
... • A general medical symptom or disorder is present • Psychological or behavioral factors negatively affect the medical condition in one or more of the following ways, such that the factors: -Pose additional health risks for the patient -Aggravate the underlying pathophysiology of a medical condition ...
Early Onset Psychosis
... 40% of Individuals reported initial insight came from themselves, and 18% reported family and friends identified symptoms first. 50% Family/friends reported initial insight came from family and only 13% said the individual recognized their symptoms first. NAMI suggests, this disparity may illust ...
... 40% of Individuals reported initial insight came from themselves, and 18% reported family and friends identified symptoms first. 50% Family/friends reported initial insight came from family and only 13% said the individual recognized their symptoms first. NAMI suggests, this disparity may illust ...
Abnormal and treatment
... 3. Margaret has hardly gotten out of bed for weeks, although she’s troubled by insomnia. She doesn’t feel like eating and has absolutely no energy. She feels dejected, discouraged, spiritless, and apathetic. Friends stop by to try and cheer her up, but she tells them not to waste their time on “pon ...
... 3. Margaret has hardly gotten out of bed for weeks, although she’s troubled by insomnia. She doesn’t feel like eating and has absolutely no energy. She feels dejected, discouraged, spiritless, and apathetic. Friends stop by to try and cheer her up, but she tells them not to waste their time on “pon ...
15 - Chapter 14 - Psychological Disorders
... depression that will suggest ways to treat it. Lewinsohn et al., (1985, 1998) note that a theory of depression should explain the following: 1. Behavioral and cognitive changes 2. Common causes of depression ...
... depression that will suggest ways to treat it. Lewinsohn et al., (1985, 1998) note that a theory of depression should explain the following: 1. Behavioral and cognitive changes 2. Common causes of depression ...
Abnormal Psychology Modules 48-55
... recurrent suicidal behavior, gestures, or threats, or self-mutilating behavior affective instability due to a marked reactivity of mood (e.g., intense episodic dysphoria, irritability, or anxiety usually lasting a few hours and only rarely more than a few days) chronic feelings of emptiness inapprop ...
... recurrent suicidal behavior, gestures, or threats, or self-mutilating behavior affective instability due to a marked reactivity of mood (e.g., intense episodic dysphoria, irritability, or anxiety usually lasting a few hours and only rarely more than a few days) chronic feelings of emptiness inapprop ...
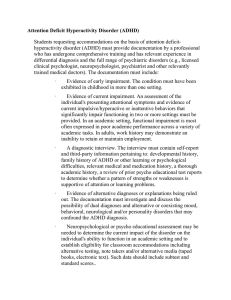
Attention Deficit Hyperactivity Disorder (ADHD)
... establish eligibility for classroom accommodations including alternative testing, note takers and/or alternative media (taped books, electronic text). Such data should include subtest and standard scores.. ...
... establish eligibility for classroom accommodations including alternative testing, note takers and/or alternative media (taped books, electronic text). Such data should include subtest and standard scores.. ...
Pediatric Bipolar Disorder
... school, or sexually) or psychomotor agitation; 7. excessive involvement in pleasurable activities that have a potential for dangerous consequences. ...
... school, or sexually) or psychomotor agitation; 7. excessive involvement in pleasurable activities that have a potential for dangerous consequences. ...
Schizoaffective disorder

Schizoaffective disorder (abbreviated as SZA or SAD) is a mental disorder characterized by abnormal thought processes and deregulated emotions. The diagnosis is made when the patient has features of both schizophrenia and a mood disorder—either bipolar disorder or depression—but does not strictly meet diagnostic criteria for either alone. The bipolar type is distinguished by symptoms of mania, hypomania, or mixed episode; the depressive type by symptoms of depression only. Common symptoms of the disorder include hallucinations, paranoid delusions, and disorganized speech and thinking. The onset of symptoms usually begins in young adulthood, currently with an uncertain lifetime prevalence because the disorder was redefined, but DSM-IV prevalence estimates were less than 1 percent of the population, in the range of 0.5 to 0.8 percent. Diagnosis is based on observed behavior and the patient's reported experiences.Genetics, neurobiology, early and current environment, behavioral, social, and experiential components appear to be important contributory factors; some recreational and prescription drugs may cause or worsen symptoms. No single isolated organic cause has been found, but extensive evidence exists for abnormalities in the metabolism of tetrahydrobiopterin (BH4), dopamine, and glutamic acid in people with schizophrenia, psychotic mood disorders, and schizoaffective disorder. People with schizoaffective disorder are likely to have co-occurring conditions, including anxiety disorders and substance use disorder. Social problems such as long-term unemployment, poverty and homelessness are common. The average life expectancy of people with the disorder is shorter than those without it, due to increased physical health problems from an absence of health promoting behaviors including a sedentary lifestyle, and a higher suicide rate.The mainstay of current treatment is antipsychotic medication combined with mood stabilizer medication or antidepressant medication, or both. There is growing concern by some researchers that antidepressants may increase psychosis, mania, and long-term mood episode cycling in the disorder. When there is risk to self or others, usually early in treatment, brief hospitalization may be necessary. Psychiatric rehabilitation, psychotherapy, and vocational rehabilitation are very important for recovery of higher psychosocial function. As a group, people with schizoaffective disorder diagnosed using DSM-IV and ICD-10 criteria have a better outcome than people with schizophrenia, but have variable individual psychosocial functional outcomes compared to people with mood disorders, from worse to the same. Outcomes for people with DSM-5 diagnosed schizoaffective disorder depend on data from prospective cohort studies, which haven't been completed yet.In DSM-5 and ICD-9 (which is being revised to ICD-10, to be published in 2015), schizoaffective disorder is in the same diagnostic class as schizophrenia, but not in the same class as mood disorders. The diagnosis was introduced in 1933, and its definition was slightly changed in the DSM-5, published in May 2013, because the DSM-IV schizoaffective disorder definition leads to excessive misdiagnosis. The changes made to the schizoaffective disorder definition were intended to make the DSM-5 diagnosis more consistent (or reliable), and to substantially reduce the use of the diagnosis. Additionally, the DSM-5 schizoaffective disorder diagnosis can no longer be used for first episode psychosis.