* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Pediatric Dysrhythmias Board Review
Survey
Document related concepts
Remote ischemic conditioning wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Cardiac surgery wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Myocardial infarction wikipedia , lookup
Jatene procedure wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Electrocardiography wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Transcript
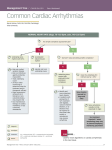
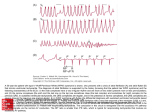
Pediatric Dysrhythmias Board Review February 11, 2008 Brad Rodrigue, M.D. Pediatric dysrhythmias Treatment not required Treatment is required Sinus arrhythmia Supraventricular tachycardia Wandering atrial pacemaker Isolated premature atrial contractions Isolated premature ventricular contractions First degree AV block Ventricular tachycardia Third degree AV block with symptoms Reproduced from Zitelli’s Atlas of Pediatric physical diagnosis, 2007, pg 140. Pediatric dysrhythmias Vital to be aware of arrhythmias that occur in otherwise healthy children Management is individualized Does child have history of heart disease? Are symptoms present? Sinus arrhythmia Most common irregularity of heart rhythm seen in children Normal variant Reflects healthy interaction between autonomic respiratory and cardiac control activity in CNS Heart rate increases during inspiration and decreases during respiration Sinus arrhythmia Wandering atrial pacemaker Atrial pacemaker shifts from sinus node to another atrial site Normal variant, irregular rhythm Isolated PAC’s Premature atrial contractions Benign in absence of underlying heart dz Common in newborn period Early p wave, sometimes with different morphology than a sinus p wave Can be either: – Not conducted to ventricle, apparent pause – Conducted to ventricle with aberrant or widened QRS complex ( careful not to mix up with PVC’s) Isolated PAC’s Premature Ventricular Contractions (PVC’s) Not very commonly seen in children Incidence of 0.3 to 2.2 % Early, wide QRS complexes T waves in opposite direction of QRS Unifocal PVC’s are most encountered type Bigeminy, sinus beat followed by PVC, repeating as a pattern, also frequently seen PVC’s If unifocal, disappear with exercise, and associated with structurally and functionally normal heart, then considered benign, no therapy needed PVC’s evaluation 12 lead EKG, Echocardiogram Perhaps Holter monitoring Brief exercise in office to see if ectopy suppressed or more frequent Multifocal or paired PVC’s more worrisome Medications usually not needed Advise patients to avoid caffeine and other stimulants First degree AV block Commonly seen (up to 6% normal neonates) PR interval is greater than upper limits of normal for a given age PR interval is age and rate dependent 70-170 msec in newborns is normal 80-220 msec in young children and adults Generally does not cause bradycardia since AV conduction remains intact First degree AV block Diseases that can be associated with first degree AV block: rheumatic fever, rubella, mumps, hypothermia, cardiomyopathy, electrolyte disturbances Third degree AV block AKA complete heart block Most common cause of abnormal bradycardia in infants and children Complete disassociation between P waves and QRS complexes Third degree AV block Can be congenital – in this case it is strongly associated with maternal SLE Mom of an infant should be worked up Most common structural heart defect associated is corrected transposition of great vessels Third degree AV block May be asymptomatic – follow clinically Slower the heart rate, and wide QRS escape rhythms place into high risk group May need implantable pacemaker: significant bradycardias, syncope, exercise intolerance, ventricular dysrhythmias, or ventricular arrhythmias, structural disease Possible acute treatment: isoproterenol Supraventricular tachycardia Most common abnormal tachycardia seen in pediatric practice Most common arrhythmia requiring treatment in pediatric population Most frequent age presentation: 1st 3 months of life, 2nd peaks @ 8-10 and in adolescense Rapid, regular, usually narrow QRS rhythm, originating above the ventricles SVT Figure 5-42 Supraventricular tachycardia. Note a normal QRS complex tachycardia at a rate of 214 beats/minute without visible P waves. SVT Paroxysmal, sudden onset & offset Rates of SVT vary with age Overall average rate for all ages: 235 bpm – 1st 9 months of life: avg rate is 270 bpm – Older children: avg rate is 210 bpm( 180-250) P waves difficult to define, but 1:1 with QRS Important to differentiate from sinus tach SVT Older kids can describe a sensation of a fast heart rate, palpitations, or chest tightness Hemodynamic compromise in newborns and those with structural heart disease Those with typical symptoms would benefit from cardiac consultation SVT - Treatment Goal: identify unstable patients, differentiate from sinus tachycardia, and terminate the rhythm Vagal maneuvers in stable patients Adenosine if IV access readily available – Stop conduction through AV node – Helps to define p waves if unsure of etiology – 0.1 mg/kg (max 6 mg), repeat 0.2 mg/kg ( max 12 mg) in line closest to central circulation – Need continuous ECG and BP monitoring Synchronized cardioversion Amiodarone, Procainamide if above unsuccessful Transesophageal atrial pacing can also be performed SVT - Treatment Need post conversion EKG – identify those with WPW syndrome ( 25 % pts with SVT) Will also need an echo – identify structural problems Radiofrequency catheter ablation – Frontline treatment – Very effective – Cutoff points usually are 5 y.o. and 15 kg, unless severe SVT Observation and expectant management Medications – Digoxin and beta blockers as first line – Flecainide, sotalol, amiodarone Other SVT’s A flutter, A fib, ectopic atrial tachycardia, junctional tachycardias Not commonly seen in pediatric patients Adenosine does not terminate these rhythms, originate above AV node Treatments: procainamide, amiodarone, cardioversion, or ablation SVT - WPW Figure 5-43 Wolff-Parkinson-White syndrome. Note the characteristic findings of a short P-R interval, slurred upstroke of QRS (delta wave), and prolongation of the QRS interval. Ventricular tachycardia Sustained V-tach is uncommon, needs workup Regular wide complex tachycardia Atrioventricular dissociation Life threatening arryhthmia Often presents in those who have had open heart surgical repair, or those with cardiomyopathies, myocarditis, or tumors V-Tach Treatment: IV lidocaine, procainamide, amiodarone If critically ill: synchronized cardioversion Long term: meds, ablation, or defibrillator Ventricular fibrillation Seen in children with EKG abnormalities such as long QT syndrome, or Brugada syndrome Cardiomyopathies, structural heart disease causing ventricular dysfunction Treatment: immediate defibrillation, CPR V-fib Brugada syndrome – inherited arrhythmia, autosomal dominant person goes into vfib, faints, dies suddenly Treatment: defibrillator, careful screening That’s all!