* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Oxygen - CriticalCareMedicine
Adenosine triphosphate wikipedia , lookup
Radical (chemistry) wikipedia , lookup
Gaseous signaling molecules wikipedia , lookup
Mitochondrial replacement therapy wikipedia , lookup
Light-dependent reactions wikipedia , lookup
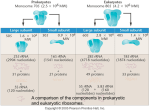
Mitochondrion wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Photosynthesis wikipedia , lookup
Electron transport chain wikipedia , lookup
Microbial metabolism wikipedia , lookup
Citric acid cycle wikipedia , lookup
NADH:ubiquinone oxidoreductase (H+-translocating) wikipedia , lookup
Lactate dehydrogenase wikipedia , lookup
Photosynthetic reaction centre wikipedia , lookup
Oxygen toxicity wikipedia , lookup
Biochemistry wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
Metalloprotein wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Oxygen: What’s it good for anyways? Outline Basic Concepts • • • • Diffusion Hemoglobin binding Oxygen equations Mitochondrial function Type IV Respiratory Failure • Critical DO2 • Cytopathic hypoxia • Microcirculation shunting Oxygen Diffusion Partial pressure of O2 at standard pressure and temperature is 21.3 kPa but falls to 14.7 kPa at the alveoli. Diffusion of O2 into the blood and then into the tissue is determined by Fick’s law. K=permeability of O2 within the diffusion medium S=surface area P=pressure gradient =diffusion distance S Diffusion K P Oxygen Diffusion In the lung, the diffusion barrier is the alveolar-capillary membrane. The PO2 is 100 mmHg on the alveolar side and 90 mmHg on the capillary side. At the tissue level, the capillary wall is the primary barrier. The diffusion distance can vary but the pressure gradient is much higher as the PO2 at the mitochondria is about 1 mmHg. Hemoglobin Binding Once oxygen has crossed the capillary membrane, it enters the red blood cells and binds to hemoglobin. Why is the oxyhemoglobin dissociation curve sigmoid? Cooperativity When the curve shifts to the left or right, it alters the P50 (oxygen tension at which hemoglobin is 50% saturated). Shift to the left – P50 decreases (i.e. lower PO2 needed to saturate 50% of the hemoglobin) Shift to the right – P50 increases (i.e. higher PO2 needed to saturate 50% of the hemoglobin). Hemoglobin Binding Name four conditions that shift the oxyhemoglobin curve to the left. Name four conditions that shift the oxyhemoglobin curve to the right. Hyperthermia Acidosis Hypercarbia Increased 2,3-DPG What happens to red cells from the blood bank? What is the purpose of 2,3 DPG? Hypothermia Alkalosis CO Decreased 2,3-diglycerophosphate Binds deoxyhemoglobin to stabilize the T-state and forces release of oxygen. A lack of 2,3 DPG mimics fetal hemoglobin. Trivia – What is the normal shifting of the oxyhemoglobin curve in the lungs and the tissue called? Oxygen Equations 1 gm of hemoglobin binds 1.34 mL of O2. The solubility of oxygen in serum is 0.03 mL of O2/ (L)(mmHg). Since there is no other way to transport oxygen, the total oxygen content of blood is the sum of: That bound to hemoglobin: (1.34 mL/g)(Hgb g/L)(Saturation) That dissolved in serum: (0.03 mL/(L)(mmHg))(PO2 mmHg) CaO2 1.34 Hgb SaO2 0.03 PaO2 Oxygen Equations In order to calculate the total amount of oxygen delivery (global), multiply the cardiac output by the oxygen content. DO2 CO( L / min) CaO2 (mL / L) Normal oxygen delivery is 1000 ml O2/min (assuming a cardiac output of 5 L/min and hemoglobin of 150 g/L) Oxygen Equations The amount of oxygen consumed in any tissue can be calculated by measuring the oxygen content in both the arterial and venous limb of the tissue. VO2 CO Ca O2 Cv O2 The normal global oxygen consumption is 250 mL/min. What would be the required cardiac output in the absence of hemoglobin to support a VO2 of 250 mL/min? Oxygen Equations The ratio of VO2/DO2 is the oxygen extraction ratio (ER). How can you calculate the ER without knowing the Hgb? The ER increases in conditions such as exercise, CHF, and anemia as a result of a lower CvO2. The converse occurs in sepsis. Each organ has its own metabolic needs so individual organ ER vary. The brain and the heart extract much more oxygen and thus are more susceptible to decreased delivery. Mitochondrial Function All reversible reactions proceed in the direction that results in a net decrease in the Gibbs energy for the system. (G=H-TS) In order for living systems to carry out reactions that require a positive Gibbs energy, they must be coupled to a reaction that is energically favorable. If the total Gibbs energy for the two reactions is negative then the reactions can proceed. Mitochondrial Function Aerobic generation of ATP occurs as a result of series of stepwise reactions that couple the oxidation of substrates to oxygen with the phosphorylation of ATP. To review: Reducing agents donate electrons. Oxidizing agents accept electrons. Oxygen is a very strong oxidizer while NADH and FADH are very strong reducers. Mitochondrial Function The reaction of oxygen to NADH or FADH has a very negative Gibbs energy whereas the phosphorylation of ADP to ATP has a low positive Gibbs energy. To capture the released energy efficiently, mitochondria step down the reaction. First it has to generate NADH and FADH via the citric acid cycle. Mitochondrial Function The electrons are transferred through a series of intermediate compounds that have progressively lower reducing potentials. This respiratory chain is located on the inner membrane of the mitochondria. The energy thus released is used to pump protons from the mitochondrial matrix to the intermembrane space. The protons then follow their gradient through the F0F1ATPase that catalyzes the formation of ATP. Oxygen’s only job is to act as the final electron acceptor in the respiratory transport chain. Type IV Respiratory Failure Critical DO2 With moderate reductions in DO2, the ER increases to satisfy VO2. What is the ER when DO2 is 1000 mL/min? (assume VO2 = 250 mL/min) What is the ER when DO2 is 500 mL/min? What is the ER when DO2 is 150 mL/min? The level at which VO2 begins to decline with declining DO2 is the critical DO2. At this point, VO2 becomes supply dependant and the tissues turn to anaerobic metabolism. The average critical DO2 is 4.2 mL/min/kg. Cytopathic Hypoxia There are four different but mutually compatible mechanisms to explain decreased oxygen consumption in sepsis: Inhibition of pyruvate dehydrogenase NO mediated inhibition of cytochrome a,a3 Peroxynitrite inhibition of mitochondrial enzymes Poly(ADP-ribose) polymerase Inhibition of Pyruvate Dehydrogenase (PDH) End product of glycolysis is pyruvic acid. It can be reduced to either lactate or enter TCA. PDH converts pyruvate to acetyl-coenzyme A in the presence of NAD+ and coenzyme A. PDH kinase phosphorylates PDH to inactive form. Inhibition of Pyruvate Dehydrogenase (PDH) In sepsis, the activity of PDH kinase is increased. The inactivation of PDH limits the flux of pyruvate through TCA cycle. Excess pyruvate accumulates and leads to increased production of lactate. Therefore, hyperlactatemia is not just evidence of low DO2. NO-mediated inhibition of Cytochrome a,a3 Sepsis induces iNOS to produce NO. When NO binds to cytochrome a,a3 (last step in the ETC) it out competes O2 for the same binding site. This causes a rapid but reversible inhibition of the enzyme. Since the reaction is reversible, this should not pose a major problem BUT… Peroxynitrite Inhibition of Mitochondrial Enzymes NO also can react with O2- to form peroxynitrite (ONOO-) with is a powerful oxidizing and nitrosating agent. ONOO- inhibits F0F1 ATPase and Complex I and II. ONOO- also inhibits aconitase (TCA enzyme). Unlike NO, these inhibitions are irreversible. Poly(ADP-ribose) Polymerase (PARP-1) PARP-1 is a nuclear enzyme involved in the repair of single strand breaks of DNA. It catalyzes the cleavage of NAD+ into ADP-ribose and nicotinamide and then polymerizes the ADP-ribose into homopolymers. ROS and ONOO- can induce single strand breaks in DNA which activates PARP-1. The PARP-1 causes the NAD+/NADH content to fall which impairs the cells ability to use O2 in ATP production. Microcirculation shunting The endothelium is an important regulator of oxygen delivery. In response to local blood flow and other stimuli, it signals upstream to dilate feeding arterioles. RBC can sense hypoxia and release vasodilators such as NO and ATP. The goal is to control local flow patterns to ensure global oxygenation. Microcirculation shunting In sepsis, endothelial cells: Are less responsive to vasoactive agents. Lose their anionic charge and glycocalyx. Become leaky Massively over express NO. RBC and WBC cell deformability reduces, causing plugging. The WBC and endothelium interact in ways to induce inflammation and coagulation pathways. Microcirculation shunting Inflammatory activation of NO is one of the key mechanism responsible for shunting. Inhomogeneous expression of iNOS interferes with regional blood flow and promotes shunting from vulnerable microcirculatory units. Inhomogeneous expression of endothelial adhesion molecules also contribute through their effects on WBC kinetics. Lactate Sympathy for the Devil Background For years lactate was considered a waste product of metabolism. Recent bench work points to its important role in intracellular signaling and energy transport in the muscle, brain and sperm. In sepsis, the classic explanation for hyperlactatemia has been anaerobic glycolysis due to insufficient oxygen delivery. The Case Recent it has been suggested that the hyperlactatemia in sepsis may be from an adrenaline surge that stimulates Na/K/ATPase activity and coupled aerobic glycolysis. To review, adrenaline binds B2-adrenoreceptors, activating adenylate cyclase, catalyzing ATP to cAMP. cAMP activates PKA which activates Na/K/ATPase. The ATPase pump derives its energy from glycolysis. Therefore, hyperlactatemia in the face of hemodynamic stability may be adrenaline stimulated aerobic glycolysis rather than tissue hypoxia. The Evidence Aerobically incubated muscle from septic rats had an increased rate of lactate production that was partially inhibited by ouabain (Na/K/ATPase inhibitor). Endotoxemia in heathy humans causes a rise in adrenaline and lactate levels. The lactate rise in the leg was matched by a fall in regional potassium levels in the blood and increase in uptake. No evidence of hypoxia or hypoperfusion. More Evidence A similar mechanism is in play with hemorrhage. Blocking adrenergic receptors in bleeding rats caused a significant fall in lactate levels with a increased Na/K ratio (implying decreased Na/K/ATPase activity). Administering ouabain to muscles that were either bled or infused with adrenaline reduced the lactate level equally compared to controls. Conclusion Tissue hypoperfusion, hypoxia and anaerobic glycolysis are probably not the only cause of increased lactate production in shock. Outline Basic Concepts • • • • Diffusion Hemoglobin binding Oxygen equations Mitochondrial function Type IV Respiratory Failure • Critical DO2 • Cytopathic hypoxia • Microcirculation shunting Lactate – Maybe not the boogie man after all. Questions???