* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Unilateral, nontender, vulvar swelling as the presenting sign of
Marburg virus disease wikipedia , lookup
Meningococcal disease wikipedia , lookup
Trichinosis wikipedia , lookup
Bovine spongiform encephalopathy wikipedia , lookup
Creutzfeldt–Jakob disease wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Oesophagostomum wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Chagas disease wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Onchocerciasis wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Leptospirosis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Leishmaniasis wikipedia , lookup
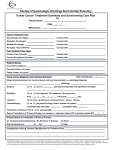
doi: 10.1111/j.1346-8138.2010.00991.x Journal of Dermatology 2011; 38: 303–307 LETTER TO THE EDITOR Unilateral, non-tender, vulvar swelling as the presenting sign of Crohn’s disease: A case report and our suggestion for early diagnosis Dear Editor, We report a patient with metastatic Crohn’s disease (MCD) who presented with vulvar swelling preceding the diagnosis of gastrointestinal disease. Vulvar involvement of Crohn’s disease (CD) is rare and difficult to diagnose, especially when it precedes the onset of overt gastrointestinal symptoms. In our case, the diagnosis was enigmatic because no radiological and laboratory examinations gave a clue for diagnosis. Here, we suggest two diagnostic clues which may help early diagnosis of vulvar MCD after reviewing reported cases of MCD in children whose vulvar swelling or edema preceded gastrointestinal symptoms in the English-language published work. A 10-year-old girl presented to our dermatological clinic with a 1-month history of unilateral, non-tender, vulvar swelling. Before visiting our clinic, she had been treated with empirical antibiotics for 2 weeks at local pediatric and gynecological clinics under the impression of infectious disease but her vulvar swelling had not improved. She and her parent denied any trauma, sexual abuse or a history of infectious disease. She had no notable medical history and did not have any systemic symptom. Physical examination revealed non-tender, erythematous swelling on the left vulva (Fig. 1a,b) and small skin tags on the anal orifice (Fig. 1c). Height and weight percentiles were normal for her age. Laboratory test results were within normal range except for a slightly increased erythrocyte sedimentation rate of 18 mm ⁄ h (reference range 0–15 mm ⁄ h). Magnetic resonance imaging of the pelvis showed focally enhancing subcutaneous tissue on the anterior portion of the left labia majora which primarily suggested focal cellulitis (Fig. 1d). We prescribed cefprozil 250 mg ⁄ day for 10 days under the impression of infection of the vulva. Ten days later, the lesion did not improve, so we decided to perform skin biopsy. The histopathological finding revealed non-caseating granulomatous inflammation throughout the dermis. The granulomas were composed of epithelioid histiocytes, a few giant cells and lymphocytes (Fig. 1e). Neither special stains and cultures for bacteria, fungus and mycobacterium nor polarizing light microscopy for foreign bodies were positive. Chest X-ray and tuberculin skin test were also normal. Even though the patient did not have overt abdominal symptom, diagnostic colonoscopy was performed to rule out CD. It disclosed multiple aphthous ulcers ranging from rectosigmoid colon to ascending colon with ileal involvement and biopsy specimens of the colon revealed granulomatous inflammation, consistent with CD. Treatment was commenced with oral corticosteroid and metronidazole with marked improvement in 2 months’ treatment. During one and half year follow up, several diarrheal episodes occurred but her symptom was generally tolerable. Crohn’s disease is a chronic relapsing, multisystemic, inflammatory disorder of uncertain etiology, characterized by non-caseating granulomatous inflammation that can affect any part of the gastrointestinal tract from mouth to anus. Twenty-two to forty-four percent of CD patients present four types of cutaneous manifestations: (i) direct extension from involved bowel leading to perioral or perianal diseases; (ii) MCD; (iii) nutritionally-associated skin lesions; and (iv) reactive lesions like pyoderma gangrenosum and erythema nodosum.1 Metastatic Crohn’s disease is defined as noncaseating, granulomatous skin lesions that are not contiguous to the gastrointestinal tract. It usually presents as solitary or multiple papules, nodules or Correspondence: Hyun-Chang Ko, M.D., Department of Dermatology, School of Medicine, Medical Research Institute, Pusan National University, 305 Guduk-ro, Seo-gu, Busan 602-739, Korea. Email: [email protected] 2010 Japanese Dermatological Association 303 J.-H. Mun et al. (a) (d) (b) (c) (e) Figure 1. Erythematous swelling on left vulva (a,b) and skin tags on the perianal region (c). Magnetic resonance imaging of pelvis showing focal subcutaneous thickening with low signal intensity in T1-weighted image (d). Histopathological examination of the vulva shows multiple non-caseating granulomas extending throughout the dermis and the granuloma consist of epithelioid histiocytes, lymphocytes and multinucleated giant cells (e) (hematoxylin–eosin, original magnification ·40). plaques that are red to purple or violaceous and commonly involves the limbs, especially legs, vulva, penis and face.2 MCD on the vulva in children is rare and difficult to diagnose. Furthermore, if a dermatological manifestation precedes gastrointestinal symptoms, the diagnosis becomes enigmatic. Only several cases of which vulvar swelling or edema antedates the clinical appearance of intestinal CD in children have been reported in the English-language published work.3–9 The diseases which can cause vulvar swelling include pregnancy, hidradenitis suppurativa, sexual abuse, tumor, vascular malformation, lymphedema, genital cheilitis granulomatosa, factitial dermatitis, 304 contact dermatitis, CD, mastocytosis and various infectious diseases. For differential diagnosis of vulvar swelling, prudent history taking and physical examinations are important. Laboratory and radiological examinations could also give some diagnostic clues. When clinical diagnosis cannot be made easily, skin biopsy is necessary. MCD is distinguished histologically by granulomatous inflammation. However, because various conditions can also cause granulomatous inflammation, diverse investigations are necessary.7 After common infectious or inflammatory diseases are excluded, performing diagnostic colonoscopy is warranted to check for CD. In our case, as 2010 Japanese Dermatological Association Letter to the Editor Table 1. Reported cases of vulvar swelling or edema precede gastrointestinal symptoms of Crohn’s disease in children in English-language published work Reference Age (years) Mountain3 14 Lally et al.4 Werlin et al.5 Guerrieri et al.6 Initial diagnosis Vulvar symptom Concomitant perianal lesion Edema and inflammation of labia Tuberculosis† N⁄D Anal fistula 8 Vulvar erythema and edema Non-tender Anal fistula 8 Erythematous, firm, unilateral, labial hypertrophy Swelling of right labium majus Contact dermatitis, candidiasis and sexual abuse Foreign body reaction Non-tender Skin tags Vulvitis granulomatosa Non-tender Anal tags Erythema and edema of the labial majora Cellulitis N⁄D Swelling of lower lip, vulvar swelling and perivaginal abscess Swelling and induration of the labia majora Erythematous, firm tumescence of left labial majora Left vulvar swelling N⁄D N⁄D Skin tags and fissures with anal hemorrhoids None Sexual abuse Genital itching Infectious disease Asymptomatic Cellulitis Non-tender 11 Ploysangam et al.7 6 Ploysangam et al.7 10 Porzionato et al.8 7 Pinna et al.9 10 Present case 10 Presentation Perianal fissures and skin tags Rose-grayish vegetations Skin tags Vulvar pathology Chronic inflammatory changes without tubercules or caseation Noncaseating granulomatous inflammation Non-caseating granulomatous inflammation Non-necrotizing granulomatous inflammation Granulomatous inflammation Granulomatous inflammation Non-caseating granulomatous inflammation Non-caseating granulomatous inflammation Non-caseating granulomatous inflammation † The author did not describe initial diagnosis but the lesion was treated with a 2-month course of streptomycin and isoniazid without benefit. N ⁄ D, Not described. the dermatological manifestation antedated the onset of typical intestinal symptoms, the diagnosis was difficult because no laboratory and radiological examinations gave a hint for MCD. After reviewing reported MCD cases in children including the present case whose vulvar swelling or edema preceded gastrointestinal symptoms of Crohn’s disease (Table 1), we suggest two diagnostic characteristics which may help early diagnosis of MCD on the vulva. First, if the vulvar swelling is nontender or painless, MCD rather than infectious diseases should be included in the differential diagnosis. MCD represents another ‘‘great imitator’’ and it resembles many other dermatoses.1 Most of the reported cases have been clinically misdiagnosed as 2010 Japanese Dermatological Association cellulitis, erysipelas, lichenoid eruptions and various sexually transmitted diseases1 and vulvar swelling as a manifestation of CD commonly misdiagnosed as cellulitis or sexual abuse.10 So, non-tenderness or painlessness in MCD could be an important clinical feature in the differential diagnosis with infectious diseases. Many reported vulvar CD were painless, especially when occurring in children.4–6,8–11 In Table 1, pain was not observed in six out of nine cases, and in the remaining three cases, vulvar symptom was not described. We speculate that those three cases would have been painless because the authors would have probably stated the symptom if there was pain or tenderness. In addition, many reported MCD cases in male patients presenting penile and scrotal swelling 305 J.-H. Mun et al. or edema did not accompany pain.12–19 In perianal CD, Alexander-Williams et al.20 previously suggested that the relative lack of pain, multiplicity of lesions and edema of skin tags can be important clinical indicators if perianal CD occurred as the first manifestation. We do not think that every vulvar CD shows lack of pain but we assume that most genital swelling in MCD at its first manifestation without secondary lesions such as fissure, erosion, ulcer or abscess would be painless or non-tender. We suggest that following MCD cases need to address the presence of tenderness or pain because such a clinical feature can be a useful information for clinicians. Second, if a patient has perianal lesions such as skin tags, anal fissures, ulcers, fistulas, perianal abscesses and anorectal strictures with vulvar swelling, MCD should be considered. In our case, anal skin tags were small and asymptomatic, and were not of clinical interest in the first place. Presence of perianal disease was noted on presentation in 81% of pediatric patients with MCD.10 Therefore, if a patient presents vulvar swelling, careful examination of the anus as well as the vulva is needed. Because vulvar CD is very rare, there is no consistent treatment for genital CD. The most effective treatment for cutaneous CD seems to be oral metronidazole, and other treatments such as systemic corticosteroids, topical corticosteroids, azathioprine, cyclosporine, sulfasalazine and tetracycline have been used sucessfully.1 Metastatic Crohn’s disease usually postdates or coincides with gastrointestinal symptoms, but in 25% of cases, dermatological lesions precede the onset of overt intestinal symptoms.1 Without intestinal manifestations, the diagnosis is extremely difficult. So we suggest that if vulvar swelling or edema is non-tender or painless and accompanies perianal diseases, CD should be taken into consideration. For definite diagnosis, skin biopsy and colonoscopy need to be performed. Vulvar CD has been a diagnostic challenge not only for dermatologists but also for gastroenterologists, gynecologists, pediatricians and urologists. Delayed diagnosis of CD can result in many complications such as malnutrition, delayed pubertal development, intestinal obstruction, hemorrhage and emotional issues. In this context, our suggestion for early diagnosis has clinical significance. 306 Je-Ho MUN, Su-Han KIM, Do-Sang JUNG, Hyun-Chang KO, Moon-Bum KIM, Kyung-Sool KWON Department of Dermatology, School of Medicine, Pusan National University, Busan, Korea REFERENCES 1 Palamaras I, El-Jabbour J, Pietropaolo N et al. Metastatic Crohn’s disease: a review. J Eur Acad Dermatol Venereol 2008; 22: 1033–1043. 2 Hackzell-Bradley M, Hedblad MA, Stephansson EA. Metastatic Crohn’s disease. Report of 3 cases with special reference to histopathologic findings. Arch Dermatol 1996; 132: 928–932. 3 Mountain JC. Cutaneous ulceration in Crohn’s disease. Gut 1970; 11: 18–26. 4 Lally MR, Orenstein SR, Cohen BA. Crohn’s disease of the vulva in an 8-year-old girl. Pediatr Dermatol 1988; 5: 103–106. 5 Werlin SL, Esterly NB, Oechler H. Crohn’s disease presenting as unilateral labial hypertrophy. J Am Acad Dermatol 1992; 27: 893–895. 6 Guerrieri C, Ohlsson E, Ryden G, Westermark P. Vulvitis granulomatosa: a cryptogenic chronic inflammatory hypertrophy of vulvar labia related to cheilitis granulomatosa and Crohn’s disease. Int J Gynecol Pathol 1995; 14: 352–359. 7 Ploysangam T, Heubi JE, Eisen D, Balistreri WF, Lucky AW. Cutaneous Crohn’s disease in children. J Am Acad Dermatol 1997; 36: 697–704. 8 Porzionato A, Alaggio R, Aprile A. Perianal and vulvar Crohn’s disease presenting as suspected abuse. Forensic Sci Int 2005; 155: 24–27. 9 Pinna AL, Atzori L, Ferreli C, Aste N. Cutaneous Crohn disease in a child. Pediatr Dermatol 2006; 23: 49–52. 10 Keiler S, Tyson P, Tamburro J. Metastatic cutaneous Crohn’s disease in children: case report and review of the literature. Pediatr Dermatol 2009; 26: 604–609. 11 Kuloglu Z, Kansu A, Demirceken F et al. Crohn’s disease of the vulva in a 10-year-old girl. Turk J Pediatr 2008; 50: 197–199. 12 Neri I, Bardazzi F, Fanti PA, Guidetti MS. Penile Crohn’s disease: a case report. Genitourin Med 1995; 71: 45– 46. 13 Acker SM, Sahn EE, Rogers HC, Maize JC, Moscatello SA, Frick KA. Genital cutaneous Crohn disease: two cases with unusual clinical and histopathologic features in young men. Am J Dermatopathol 2000; 22: 443–446. 14 Case Records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 21-2000. A 13-year-old boy with genital edema and abdominal pain. N Engl J Med 2000; 343: 127–133. 2010 Japanese Dermatological Association Letter to the Editor 15 Escher JC, Stoof TJ, van Deventer SJ, van Furth AM. Successful treatment of metastatic Crohn disease with infliximab. J Pediatr Gastroenterol Nutr 2002; 34: 420– 423. 16 Poon KS, Gilks CB, Masterson JS. Metastatic Crohn’s disease involving the genitalia. J Urol 2002; 167: 2541– 2542. 17 Macaya A, Marcoval J, Bordas X, Moreno A, Vazquez S, Peyri J. Crohn’s disease presenting as prepuce and scrotal edema. J Am Acad Dermatol 2003; 49: S182–S183. 2010 Japanese Dermatological Association 18 Zelhof B, Biyani CS, Anathhanam AJ, Pollock B, Browning AJ. Severe penile edema: an unusual presentation of metastatic Crohn disease. Int J Urol 2006; 13: 189–191. 19 Lane VA, Vajda P, King D, Stahlschmidt J, Sugarman I, Subramaniam R. Metastatic Crohn’s disease: two cases of penile Crohn’s and literature review. J Pediatr Urol 2009; 6: 270–273. 20 Alexander-Williams J, Buchmann P. Perianal Crohn’s disease. World J Surg 1980; 4: 203–208. 307