* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download CRISIS EVALUATION OF THE PREGNANT AND POSTPARTUM
Survey
Document related concepts
History of psychiatric institutions wikipedia , lookup
Generalized anxiety disorder wikipedia , lookup
History of psychiatry wikipedia , lookup
Mental status examination wikipedia , lookup
Separation anxiety disorder wikipedia , lookup
Major depressive disorder wikipedia , lookup
History of mental disorders wikipedia , lookup
Factitious disorder imposed on another wikipedia , lookup
Controversy surrounding psychiatry wikipedia , lookup
Emergency psychiatry wikipedia , lookup
Child psychopathology wikipedia , lookup
Transcript
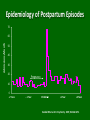
Sponsored by the POSTPARTUM DEPRESSION PROJECT MAINE ASSOCIATION OF PSYCHIATRIC PHYSICIANS (MAPP) CRISIS EVALUATION OF THE PREGNANT AND POSTPARTUM WOMAN: What to know on the frontlines Goals of this presentation: 1. Understand the importance of recognition of depression in pregnant and postpartum women 2. Know the spectrum of perinatal mood disorders 3. Know what represents a true psychiatric emergency 4. Know what circumstances raise the risk of harm to the baby 5. Recognize postpartum psychosis 6. Understand the consequences of untreated perinatal depression 7. Know how to assess the level of care needed 8. Discuss some typical case presentations Important Points: • Depression and other mental illness during pregnancy and postpartum most often is undiagnosed and untreated. • There is tremendous societal pressure to present as happy and well functioning during these times. • Women fear stigma, being judged as bad mothers, having their children taken away and that treatment with medication will harm their babies Important Points: • Women seeking out care are most often feeling frightened, ashamed and extremely vulnerable • There are 2 “clients” to consider: mother and baby • NONJUDGMENTAL AND INFORMED ASSESSMENT IS KEY DEPRESSION DURING PREGNANCY • Between 10-20% of women will experience significant depression during pregnancy • This will be a first episode for one third • Routine screening for depression during pregnancy is uncommon • Typically depression during pregnancy is untreated or incompletely treated • Women who have discontinued their psychotropic medication in order to get pregnant are at high risk for relapse SIGNIFICANCE Untreated depression during pregnancy is associated with serious short term risks and long term mental health and health consequences for mother and her baby. THE MOST COMMON COMPLICATION OF CHILDBIRTH IS DEPRESSION Epidemiology of Postpartum Episodes 70 Admissions/Month 60 50 40 30 20 Pregnancy 10 0 –2 Years – 1 Year Childbirth +1 Year +2 Years Kendell RE et al. Br J Psychiatry. 1987;150:662-673. Spectrum of Postpartum Mood Disorders Postpartum Psychosis Postpartum Symptom Severity Postpartum Depression (10-15%) Postpartum Blues (50-85%) None BABY BLUES • Baby Blues usually develop 3-5 days after delivery • Hallmark is emotional reactivity • Occur in 70-80 % of all new mothers • Normal reactions to the hormonal changes and stress of having a baby • “Baby blues” persisting beyond 2 weeks or showing signs of worsening raise questions about PPD PPD: EARLY RECOGNITION • PPD is most often missed despite multiple contacts with health care providers • The most significant factor in the duration of PPD is delay in receiving treatment • Depression often persists for months to years after childbirth, with lingering effects on physical and psychological functioning following recovery from depressive episodes 12 RISK FACTORS • Depression during pregnancy is the best predictor of post partum depression • Prenatal anxiety • History of mood disorder, especially PPD and bipolar disorder • Recently having stopped antidepressants or other psychotropics prior to pregnancy • Past history of trauma • Pregnancy or neonatal loss or complications • Difficult infant temperament • Lack of social support or marital conflict • Recent loss or stressful life events • History of sexual abuse • Low self esteem • Breastfeeding difficulties PRESENTATION OF PPD • Usually develops slowly over the first three months, often beginning within the first 4 weeks, though some women have a more acute onset • May affect ability to care for the baby • Signs and symptoms are those of Major Depression---depressed mood, irritability, loss of interest and appetite, fatigue insomnia. • Often complain of being physically and emotionally exhausted PRESENTATION OF PPD Some common features: • Often express concerns about her ability to care for her baby or anxiety about the baby’s well being • Anxiety symptoms are common including frank panic disorder, hypochondriasis, and most common, generalized anxiety disorder • Women are often unable to sleep even when given the opportunity PRESENTATION OF PPD • Frequently have intrusive, obsessional ruminations • Usually focused on the baby, often violent in nature • Egodystonic , VERY troubling to mothers • NO problem with reality testing i.e. nonpsychotic. • One study showed 50% of women with PPD had these obsessional thoughts VERY IMPORTANT TO DISTINGUISH OBSESSIONAL THOUGHTS FROM PSYCHOSIS! • NOT associated with psychotic symptoms • Experienced as inside the head • May be experienced dramatically as images in the mind, e.g. as knives or bloody babies, etc • Are often accompanied by protective or avoidant behaviors, e.g. hiding all the knives, refusing to bathe the baby, similar to the hand washing used to neutralize the anxiety of fears that accompany OCD • DO NOT increase the risk of harm to the baby • DO NOT necessitate separating mother and baby Questions to Ask: “Woman who have just had babies commonly report having a lot of anxiety including repetitive scary thoughts …..” – Have you been having any scary thoughts? – Have you been experiencing any frightening thoughts or images that you just can’t get out of your head? POST PARTUM PSYCHOSIS • A PSYCHIATRIC EMERGENCY WHICH REQUIRES IMMEDIATE INTERVENTION • Typical onset is within 2 weeks after delivery, first symptoms often within 48-72 hours • Earliest signs are restlessness, irritability and insomnia • Often very labile in presentation • Often looks “organic” with a lot of confusion and disorientation • Most often consistent with mania or a mixed state POST PARTUM PSYCHOSIS • Includes agitation, paranoia, delusions, disorganized thinking and impulsivity • Thoughts of harming the baby are frequently driven by delusions—Child must be saved from harm, child is malevolent, dangerous, has special powers, is Satan or God • Auditory hallucinations instructing the mother to harm herself or the child are common • Rates of infanticide associated with untreated postpartum psychosis have been estimated to be as high as 4%. Other Considerations • The onset or worsening of OCD, PTSD and panic disorder can also occur postpartum. There can be considerable overlap with PPD. • PTSD can develop in response to a traumatic birth experience or pregnancy loss • PTSD can emerge in pregnancy when past physical or sexual trauma is reexpereinced • Often are intermingled with symptoms of PPD Postpartum Psychiatric Illness Associated with Significant Mortality • Suicide rate is increased 70 fold in the postpartum year • Women with severe postpartum psychiatric illness also have a higher risk of death from other causes Decision Making about Level of Care • Safety –of mother and baby; i.e. risk of suicide, harm to baby, capacity to care for herself and the baby • Presence of psychosis • Availability of care– medical and mental health care providers familiar with perinatal illness • Access to care – both availability and mother’s capacity and willingness to access INVOLVING THE FAMILY and OTHERS • Isolation and feeling overwhelmed are often huge problems • Need to also assess the level of psycho social support • Need to assess the woman’s willingness and capacity to accept it– may need to encourage her acceptance • Whether or not a woman can manage at home is hugely influenced by these factors Treatment intervention SELECTION OF TREATMENT: Hospitalization: Necessary for postpartum psychosis, acute suicidality, severe depression without adequate support in the community Disadvantage: • This involves separating the mother and baby which may or may not always be ideal • We do not have specialized inpatient facilities for treating postpartum illness Treatment intervention Outpatient treatment: Appropriate if supports are available, resources are good, and no imminent risk Advantages: • Does not separate mother and baby • Supports often rally in a crisis Disadvantages: • Sometimes women benefit from a relief of responsibility from child care • Not all provider are adequately trained in providing care to women with perinatal mental illness • PCP’s, OB’s, are not always easily reached at the time that women present to crisis services Treatment Intervention These women need follow-up calls Postpartum Support International (PSI www.postpartum.net is an extremely important resource and has a Maine contact Treatment of PPD Selection of treatment: • **First requires good evaluation, review of prior history and assessment forsuicidality/dangerousness • Individual psychotherapy--CBT /IPT • Medication can be used with relative safety in nursing mothers • Support groups • Community support programs • Hospitalization Treatment of Postpartum Psychosis • Requires inpatient hospitalization • Get treated as affective psychosis—i.e. as Bipolar disorder • Medication treatment is necessary beginning with an antipsychotic/mood stabilizer such as Zyprexa/Lamictal • ECT is rapid and effective Role of the Crisis Worker Evaluation and Triage You also provide a very important FIRSTLINE INTERVENTION: Be sensitive– “those thoughts are very scary but they are not uncommon” Be reassuring— “this will get better, it’s not your fault” Be knowledgeable, provide education– “PPD is common and affects many mothers” REMEMBER: • Perinatal mood disorders have a significant impact on the current and future health of mother and child and stresses the functioning of the family. TREATMENT FOR THE MOTHER IS AN EARLY INTERVENTION OR PREVENTION FOR THE CHILD CASE PRESENTATIONS, QUESTIONS, AND DISCUSSIONS CASE # 1 A 30 y/o married mother of 4 year old and 7 month old sons revealed that she was having intrusive violent images of harming her infant son. The patient reported that she had similar violent images after the birth of her first son and that she was generally more stressed and anxious then because her first baby “never slept.” They also had just moved to the area and she was isolated and without support. She had intrusive images in which she would see herself putting the baby in a pot of boiling water. She was horrified by the images and could not imagine ever harming her baby. She managed these thoughts and images which were the most intense when she was in the kitchen by either moving the baby out of the kitchen or keeping him on the periphery while she worked in the kitchen. Gradually over months, as the baby slept better and she became more involved with activities and established new relationships her anxiety and the depression that accompanied it subsided. She was so horrified that she never disclosed these experiences to anyone. She did well for the subsequent 3 years and through her next pregnancy though was fearful that this experience would recur following the birth of her second son. She began to have the same intrusive thoughts and images soon after he was born. Despite this baby being a good sleeper and not having the same level of exhaustion, the images and thoughts persisted and had been so horrifying that her anxiety escalated to the point of panic attacks on a couple of occasions. She was by horrified images of putting this baby in a pot of boiling water as she would never want to harm her baby. She had begun to have disturbed sleep and to experience some depressive symptoms as well. She had no history of prior psychiatric treatment. She sought help from her PCP because of her increasing anxiety and the distress caused by the frequency of the disturbing thoughts and images of hurting her baby. Her PCP evaluated her and gave her a prescription for Zoloft, but sent her to the ED to be evaluated by the crisis team. CASE # 2 This is a 32 year old woman whose husband called with concern about her. She is 10 days postpartum with their second child. She is usually very upbeat, busy, talkative, and he was concerned that she is just “not herself”. She has a prior history of PPD with their first child. He was advised to bring her into the ED. She reported that she was “okay, but just unable to get much sleep”. She was noticed to be easily distractible, unfocused and to be unable maintain eye contact, but there was nothing else remarkable on her mental status exam. She was advised to follow-up with outpatient care including her OBGYN and told to call the crisis line if things worsen. He called back urgently the following day saying that she was much worse and brought her to the ED. She walked stiffly and robotically with a blank stare. When asked if she was okay, she answered abruptly “No!” but didn’t elaborate. Her husband disclosed that she told him that she heard people talking in her head. He found her sitting in front of the window for an extended period of time seemingly unaware that the baby was crying. When he asked her what she was doing, she abruptly came to and said “nothing.” Later she told him God would surely punish her for being a bad mother. CASE # 3 This a 28 year old married white female who presents in her 6th month of pregnancy. This is her 2nd pregnancy, but her first baby died having been born prematurely at 27 weeks with an infection. She suffered from depression following the loss of that baby but did not receive any treatment. She reports that this pregnancy has been going well and that all of the ultrasounds and tests indicate that the baby is healthy. She has been anxious from the start of the pregnancy however as she feared that would experience another loss. She has had increased anxiety symptoms over the past week, has had difficulty sleeping and has lost her appetite. For the past three nights she has woken up with anxiety attacks and has been unable to get back to sleep. She finds herself focused on the experience of previous pregnancy loss. She is scheduled for an ultrasound at the end of the week, but instead of looking to that for reassurance she is terrified of going to the test and uncertain if she can “even get there”. She has been crying and sad, no longer feeling any joy in having a baby; instead she only has fear of the potential loss of one. CASE # 4 This is a 29 year old married woman who is 3 months postpartum with her 3rd child. Her first two pregnancies and postpartum periods were uneventful. This pregnancy was complicated by premature labor and the need to be on bed rest for several weeks. This was very stressful since her first 2 children are ages 5 and 7 and she felt that she was not able to be a good mother to them while she was on bed rest. Her delivery was uncomplicated and her baby was born healthy but early at 35 weeks. The initial postpartum period was stressful because the baby had difficulty latching on when nursing. This had gone very easily with her first 2 babies and she hadn’t expected this. She had hoped to be able to give more attention to her older children now that she was off bed rest but the new baby was so hard to nurse and it took so much time. She also worried that he wasn’t getting enough to eat because he wanted to eat so frequently. In fact, even when he was sleeping she was worrying about the next feeding. She worried about his gaining enough weight and whether or not he was okay. She checked on him 4 or 5 times every time he was sleeping to make sure he was breathing okay. At the same time, she was not sleeping and was only eating to keep up her milk supply since she had no appetite. She told her doctor that she couldn’t sleep and her doctor prescribed some sleep medication but she was so afraid that she wouldn’t wake up if the baby was awake and didn’t take it. She knew that something was wrong because she couldn’t relax but didn’t know what was happening. She was bathing the baby and had a terrible image that came into her head of putting the baby’s head under the water and feared that she could be “just like Andrea Yates” and decided that she needed to come to the ED for assessment.