* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Anesthetics and adjuvants
Survey
Document related concepts
Pharmacognosy wikipedia , lookup
Toxicodynamics wikipedia , lookup
Pharmacogenomics wikipedia , lookup
History of general anesthesia wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Plateau principle wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Nicotinic agonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Drug interaction wikipedia , lookup
NMDA receptor wikipedia , lookup
Psychopharmacology wikipedia , lookup
Transcript
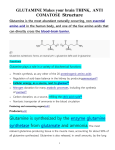
Anesthetics and adjuvants Tom Archer, MD, MBA UCSD Anesthesia Many Ways to Skin A Cat • No “best anesthetic” by outcome measures. • We want to achieve hypnosis, amnesia, analgesia, immobility and autonomic stability. • “Synergy” takes advantage of multiple agents. • So: “Garbage anesthesia” is OK! Drugs vs. the human touch • The best “tranquilizer” or “sedative” may be your calm, reassuring and informative presence! • Don’t forget the power you have to set the patient at ease. • Take the time, and don’t be afraid to make human contact with your patients. • The “solution” is not always a drug. Broad Themes (1) • Tailor the anesthetic to the patient’s needs, preferences and co-morbidities. Make use of “side effects” of our drugs. • Regional vs. general • Pre-emptive analgesia • Synergy (“garbage anesthesia”) Broad Themes (2) • Receptor model of drug action: NMDA, GABA, Ach, opioid, norepinephrine, dopamine, glycine… • Receptors open ion channels (Na+ or Cl-), thereby promoting or inhibiting action potential formation. • Agonists, modulators and antagonists at receptors (NMDA, GABA, alpha, beta, Ach, Broad Themes (3) • Direct vs. indirect drug actions. – Example: • N2O, ketamine and desflurane are DIRECT myocardial depressants, but… • They usually cause cardiovascular stimulation because of sympathetic stimulation. Regional Anesthesia • Many people would like to believe that regional is “safer” or “better” than GA, but there is no evidence for this in terms of mortality and major morbidity (except in OB?). • So: Tailor anesthesia to individual needs, preferences and clinical situation, and do what you do best! “Preemptive Analgesia” • Can we prevent “sensitization” to pain, via regional, ketamine or methadone, and thus diminish post-op pain? • Controversial area with some evidence in favor of regional, and ketamine and methadone, both of which block NMDA receptors. Synergy • Use two or more agents to avoid large doses (and significant undesired side effects) of any single agent. • Examples: – – – – propofol and fentanyl opioid and NSAIDs volatile agent and non-depolarizing NMB agent benzodiazepine, barbiturate and ethanol Synergy– How does it work? Synergy means that agonist effects are multiplicative. Effect of propofol and fentanyl depends on the product of the concentrations. “Fentanyl Neuron” Pain Response: Inhibition Movement “Pain Neuron” Inhibition “Propofol Neuron” “Ouch!!” Hypertension, Tachycardia "Isobologram": Propofol and Fentanyl Concentrations Which Prevent 50% of Rats From Moving in Response to Tail Clamp 14 Fentanyl Concentration 12 10 8 Series1 6 4 2 0 0 2 4 6 8 Propofol Concentration 10 12 14 Synergy • Drug Effect = [Drug A] X [Drug B] • Mathematically this is a hyperbola. So, let’s rejoice in the diversity of our pharmacology! • Multiple drugs imply danger and / or benefit of drug interactions. • Anesthesiologists routinely use drugs synergistically– on purpose. Using synergy and the concentration– response curve to get the effects we want– sedation, paralysis, analgesia, etc. Surfing the Concentration-- Response Curve Response (paralysis, respiratory rate, sleepiness, etc.) 120 100 80 60 Series1 40 20 0 0 2 4 6 8 Drug Concentration 10 12 14 16 How do receptors influence nerve activity? • A nerve cell integrates the input of the cells which impinge upon it. • Nerve cell responds to its “constituents.” • Drugs “stuff the ballot box” by predisposing nerve cells to fire (EPSP) or not fire (IPSP). Fig. 48.12 Copyright © 2002 Pearson Education, Inc., publishing as Benjamin Cummings “Ligand- gated ion channels”: opened by GABA, NMDA, acetylcholine, glycine or serotonin binding to their receptors. • Summation: graded potentials (EPSPs and IPSPs) are summed to either depolarize or hyperpolarize a postsynaptic neuron. Fig. 48.14 Copyright © 2002 Pearson Education, Inc., publishing as Benjamin Cummings Example: Ligand NMDA opens Na+ channels, depolarizing the nerve cell body and promoting action potential formation: the vote is “pain!” or “awaken!” NMDA Receptors • When activated, they open and allow Na+ to depolarize the nerve cell membrane, promoting pain perception. • Ketamine, phencyclidine (“Angel Dust”) and Mg++ block these Na+ channels in the NMDA receptor. • Clinically ketamine blocks pain transmission and Mg++ is an anticonvulsant. Example: GABA receptor opens an inhibitory Cl- channel. Benzodiazepines, barbiturates and ETOH “turn up the gain” (modulate) the GABA receptor’s function. GABA Opens Cl- Channels, Hyperpolarizing the Nerve Cell Body and Inhibiting Action Potential Formation: The Vote is “No Pain!” or “Sleep!” Benzodiazepines, barbiturates and ethanol work synergistically on the GABA receptor to cause sleep and amnesia. IV anesthetics– broad themes • Pain on injection (propofol, etomidate). • Excitement / movement as patient falls asleep (etomidate, methohexital). • Hemodynamic effects (direct and indirect, on stroke volume, contractility, heart rate and systemic vascular resistance). • Tailor induction agent to the situation: eg, What do you use in a hypovolemic, hypertensive or asthmatic patient? IV anesthetics– broad themes • In general– watch your dose to avoid problems. Use– and be afraid of-- synergy. • IV induction agents can affect stroke volume, heart rate, contractility and systemic vascular resistance. • We don’t usually measure CO, SVR (except with LIDCO!). • BP knocked down by: – Propofol > Pentothal > Midazolam > Etomidate > Ketamine. Opioids– themes • Very common drugs and very complex mechanisms of analgesic action. • Close the “gate” in spinal cord, both by direct action in the substantia gelatinosa of dorsal horn and by activating inhibitory, descending pathways. Opioids work within dorsal horn of spinal cord and by activating descending inhibitory pathways Opioid activates descending, inhibitory pathways Opioid directly closes gate in dorsal horn Painful stimulus The “gate” Opioids-- themes • Analgesia without (much) sedation. • Respiratory “depression”– rate decreased >> tidal volume (TV is maintained). Slow, deep, “narcotized” respiration. • Decreased cough reflex (tolerance to ETT). “Eight is great” for analgesia and tolerating ETT. Opioids-- themes • Nausea, urinary retention, itching and constipation. Memorize these. • Histamine release: Demerol / MS >>> fentanyl / remifentanil / alfentanil / sufentanil. Histamine can cause decrease in BP due to vasodilation. Histamine also causes itching. • Narcotics (except meperidine) can increase vagal tone ---> – bradycardia Opioids-- themes • “Multi-modal analgesia”: other words for “synergy”: opioid, NSAID or acetaminophen, and local. Patient is comfortable (until she gets home!) Opioids • No effect on myocardial contractility. Hence, MS used for high risk cardiac surgery beginning in the late 1960’s. • Fentanyl (and congeners) have largely replaced MS as primary “anesthetic” narcotic. Opioid Antagonists • Titrate Naloxone to Effect. 20-40 micrograms at a time. Amp has 400 mcg. Other antagonists • Atropine (Ach antagonist) blocks Ach effect on muscarinic receptors (heart) without affecting Ach effect at nicotinic receptors (neuromuscular junction and sympathetic ganglia). Atropine (and scopalomine) enter CNS, but, IMHO, danger of delirium from modest doses of atropine is over-rated. For severe bradycardia, please use atropine– and fast! • Neostigmine (anticholinesterase) increases Ach present at muscarinic and nicotinic receptors. Does not enter CNS. • Physostigmine (anticholinesterase which enters CNS) will reverse “central anticholinergic syndrome” due to atropine or scopalomine. • Flumazenil will reverse benzodiazepine effect on GABA receptor. Remember: benzo “receptor” is part of GABA receptor. PONV • “Multi-modal” approach– SYNERGY! • 5HT blocker, dexamethasone and droperidol. Danger of droperidol is VASTLY overrated! VERY little risk at doses equal or less than 1.25mg. • Hydration • Oxygen? (effect on gut?) PONV • Propofol • Limit Opioids. • Avoid N2O? I use N20 a lot. • I am liberal with antiemetics. Local Anesthetics Structure of LAs: Lipophilic, Linkage and Hydrophilic Parts of Molecules: Ester Amide Amides and Ester LAs, Ionized (BH+) and Unionized (B) Forms B Form Crosses Membrane, BH+ Forms Plugs Na+ Channel LA Speed of Onset • Quantity of B (non-ionized form). • Adding bicarbonate takes H+ away from BH+, forming B. B crosses cell membrane faster than BH+. • BH+ blocks Na+ channels from the inside of the nerve axon. Toxicity to LAs • LAs block Na+ channels in inhibitory nerves in the brain CNS excitement. • Seizures occur before cardiac depression. • LAs block Na+ channels and depolarization (conduction) in heart muscle and electrical tissue- reduced contractility and SA and AV heart blocks. • Also block Na+ channels in smooth muscle arteriolar tissue - vasodilation. Susceptibility to Blockade with LAs • Sympathetic > Pain / Temperature > Proprioception > Touch and Pressure > Motor. My opinion: test block with ice, not pin. • Absorption rate: IV > Tracheal > Intercostal > Caudal > Rest of Epidural Space > Brachial Plexus > Leg Blocks > Subcutaneous LAs Don’t Work Well in Infected Tissue– Why? • Infected Tissue is Acidic. • BH+ Form Predominates. Can’t Cross Nerve Cell Membrane. Allergy to LAs • Very, very rare with amides. Amides have two “i”s in their names, e.g. lidocaine. • More common with esters, but still rare. Esters have one “i” in their names, e.g. procaine. • Preservatives can cause allergy– when in doubt, use preservative free solutions. • Epinephrine in dentist’s office is most common cause of “allergy” (palpitations, fear, tinnitus). Metabolism of LA’s • Esters– plasma cholinesterase (just like Sux and mivacurium). • Amides-- liver Plasma cholinesterase • Metabolizes succinylcholine (Sch), mivacurium, ester LA’s. • Inhibited by neostigmine (anticholinesterase). • If you give Sch after neostigmine– you can get prolonged Sch block due to inhibition of plasma cholinesterase by neostigmine. Gaseous Anesthetics What’s the difference between “gaseous” and “volatile” anesthetics? “Gaseous” vs. “volatile” • Ether, halothane, sevoflurane, desflurane, isoflurane, etc. are gaseous and volatile. Volatile agents are liquids which evaporate. • N2O is gaseous but not volatile, since N2O is a gas at room temperature. • The gaseous form of a substance that is primarily liquid at room temperature is a “vapor.” We use the vapors of volatile agents. MAC (minimum alveolar concentration) • MAC is a partial pressure (not a %!). MAC as a % varies with atmospheric pressure. • MAC = k x O/G. Site of GA action is probably lipid. • Lipid solubility also determines potency of LAs. Site of LA action is probably lipid. Solubility (blood-gas partition coefficient) of inhaled agents in water inversely correlates with rate of rise of alveolar concentration. Low Blood / Gas Partition Coefficient (Low Solubility of Gas in Water) Causes “Quick-On and Quick-Off” Effects of Desflurane and Sevoflurane Agent Relatively Insoluble in Water (Blood and Tissue)—Little Uptake by Tissues, Rapid Rise of Fa- Fi. Examples: N2O, desflurane, sevoflurane, Water (Blood or Tissue) Alveolar Gas Desflurane Desflurane FA / FI (N2O and desflurane) at UTHSCSA FA / FI for N2O and desflurane 1.20 1.00 FA / FI 0.80 Fe/Fi N2O 0.60 Fe/Fi Des 0.40 0.20 0.00 0 2 4 6 8 10 Minutes 12 14 16 18 High Blood / Gas Partition Coefficient (High Solubility of Gas in Water) Causes “Slow-On and Slow-Off” Effects of Isoflurane, Halothane and Diethyl Ether. Agent Highly Soluble in Water (Blood and Tissues)—Much Uptake by Tissues, Slow Rise of Fa - Fi. Examples: Isoflurane or Halothane or Ether. Alveolar Gas Water (Blood or Tissue) Halothane Halothane FA / FI at UTHSCSA (N2O and isoflurane) FA / FI for N2O and isoflurane 1.2 1 FA / FI 0.8 Fe/Fi N2O 0.6 Fe/Fi Iso 0.4 0.2 0 0 2 4 6 8 Minutes 10 12 14 16 Volatile Anesthetics (Ethers) • Isoflurane (I), Desflurane (D) and Sevoflurane (S) all decrease SVR. • Reflex (compensatory) increase in heart rate and CO. • BP falls, since SVR decreases more than CO increases. Volatile Anesthetic: Desflurane • Desflurane causes sympathetic activation at >6%. Tachycardia and hypertension. • Irritates larynx (and bronchi?). Causes cough at high concentration. Volatile Anesthetic: Sevoflurane • Non-irritating. Great for inhalation induction (has replaced halothane). Volatile Anesthetic-- Halothane • Halothane (alkane) decreases HR, contractility and SVR. • Decreased CO and BP • Sensitizes myocardium to arrythmogenic effect of epinephrine. Volatile Agents (not N2O) • Act synergistically with (“potentiates”) NMB agents. • This attribute is VERY useful clinically– we can use less NMB agent and reverse it more easily. • DON’T overdo the NMBs (especially when you go into practice.) • “Relaxation does not necessarily require relaxant.” Use propofol, hyperventilation, deeper volatile agent, flex table, etc. Please remember this! It will make your life much more pleasant. Neuromuscular blocking agents (NMBs) • Also potentiated by, Mg++, aminoglycosides, cold, acidosis. Parting thought • Use synergy! • Use your heart and your personality! • Be careful out there. • Vigilance! The End