* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Lecture 4: Hepatic Variability
Survey
Document related concepts
Psychopharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug design wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Neuropharmacology wikipedia , lookup
Theralizumab wikipedia , lookup
Prescription costs wikipedia , lookup
Wilson's disease wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Transcript
Variability of Hepatic
Drug Metabolism &
Dosage Adjustment
Objectives
• Discuss hepatic disease and other
factors which impact hepatic drug
metabolism.
• Review calculations of Hepatic
extraction and clearance.
• Understand the impact of hepatic first
pass extraction on oral bioavailability.
• Based on the extraction ratio, estimate
whether the clearance of a drug will be
mainly dependent on liver blood flow
rate or intrinsic enzyme activity.
• Calculate hepatic clearance,
extraction, half-life and dosage
requirements based on changes in blood
flow and intrinsic metabolic activity in
patients.
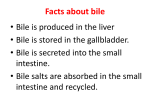
HEPATIC CLEARANCE
Important drug clearance route. Most lipidsoluble drugs are metabolized by one or
more enzymes within the liver.
As liver is major metabolic organ,
generally consider hepatic clearance as
metabolism. However drugs and their
metabolites can also be secreted from
hepatocytes into bile. Biliary Secretion
Hepatic disorders caused by multitude of
diseases.
- Has impact on a number of metabolic
enzyme systems and physiological
factors within the liver.
HEPATIC DISEASE
2 Major types of Liver Disease
Cirrhosis- Hepatoctyes replaced by nonfunctional connective tissue.
- Permanent loss of functional hepatocytes.
- Portal vein hypertension and shunting of
blood flow around liver.
- Liver blood flow
- Production of plasma proteins
Hepatitis- Inflammation of liver causing
function or cell death of hepatocytes.
• Acute- Mild/ Transient changes in
hepatic function
• Chronic - Often irreversible
hepatocyte damage
- Can progress to cirrhosis.
Effect on Metabolism
1) Enzyme Activity/Capacity
- Effects on drug metabolism may be
different depending on enzyme
system.
Cirrhosis :
• Generally see Drug metabolism
– require dosage adjustment.
Acute Viral Hepatitis:
Some drugs changed
• approx 50% of drugs affected
2) Hepatic Blood Flow:
Q in chronic liver disease (cirrhosis,
alcholism, hepatitis).
portal blood shunted (bypass liver)
PK EFFECTS:
Alterations in Hepatic Clearance
(CLH) and F (Liver
Bioavailability )
DOSES OF METABOLIZED DRUGS
OFTEN NEED TO BE REDUCED
Likewise enzyme capacity/ affinity
and/or liver blood flow also affected
by :
-
Genetic polymorphisms
Exposure to drugs/ environmental
Age
Physiological Factors
- Activity, cardiac output
- Other Diseases
- Inflammatory disease
- Renal disease
All important sources of variability in
hepatic clearance.
Hepatic Clearance
LIVER
Blood OUT
Blood IN
25% Hepatic Artery
75% Portal Vein
Hepatic Vein
Bile
Remember:
Physiological definition of Hepatic
Clearance is dependent on Blood flow
(Q) to the liver and Efficiency of the
liver to clear the drug from blood.
CL H = Q (ER)
CLH : Hepatic Clearance
Q: Flow rate through liver
ER: Hepatic Extraction Ratio
(0-1)
represents the proportion of drug
entering liver that is metabolized
or excreted upon EACH pass
through the liver.
ER= CLH/Q
Plasma vs Blood
Q = Liver Flow
Blood: Q = 1.5 L/min
Plasma Q = 825 ml/min
Use:
Plasma flow with plasma clearance &
Blood flow with blood clearance
Q plasma = (1- HCT) Q blood
HCT = hematocrit
The fraction of blood volume
which is taken up by erythorcytes.
Average HCT = 0.45
Drug can be removed by liver in two manners:
1)
•
Removal of drug from the systemic
circulation
Hepatic Clearance- (CLH) is a
component of total body clearance.
Drug dissolved in blood/plasma is
removed during each pass through
liver.
2) Pre-systemic removal of drug (1st pass)
Drug is directly absorbed into portal
vein and exposed to liver prior to entry
into systemic circulation.
•
Removal of drug upon the 1st pass
through liver decreases oral
bioavailability.
•
Hepatic 1st pass Extraction is a
component of oral bioavailability.
Therefore, Liver extraction efficiency
impacts both systemic hepatic clearance
(hepatic clearance) and oral
bioavailability (1st pass effect) of drugs.
Need to consider systemic
availability for orally
administered drugs.
Fraction remaining after 1st pass
thru liver (fer ) :
fer = 1 - ER
fer Liver bioavailability,
liver first pass availability.
But also need to consider absorption!
Bioavailability (F)
Oral bioavailability (F) involves a
combination of processes:
- dissolution in gut (fdis)
- absorption (fabs)
- liver first pass (fer)
F = fdis x fabs x fer
If entire dose is absorbed :
fdis = 1 , fabs = 1
so
F would be equal to fer
Remember:
F * Dosepo = Doseiv
Problem
A new drug Zee® is completely
eliminated through hepatic
metabolism to inactive metabolites.
After a 100 mg IV dose to healthy
patients, plasma samples were
collected, a total body clearance
(CLT) of 400 mL/min
was calculated.
Q1. What is the predicted hepatic
ER of Zee® ?
ER = CLH / QH
-
Q2. Assuming complete intestinal
absorption, what is the equivalent
oral dose of Zee® ?
fer = 1-ER
Q3. If the intestinal absorption of
Zee® is incomplete (70%) - what
oral dose is required?
F = fdis x fabs x fer
Not always so simple…..
Hepatic extraction is
dependent on
several factors that can
change
Calculation of ER based on
mechanism
ER dependent on:
1. Uptake of drug (partitioning)
Capacity 2. Amt of enzyme
& Affinity 3. Metabolic activity (Vmax, km)
4. Blood flow (Qh)
1, 2 & 3 = Intrinsic clearance (CLint)
ER =
CL int__
CLint + Qh
Other important equations describing
this relationship:
Substituting ER with CLH
(ER= CLH/Q) to describe in terms of CLH:
CLH = Qh * CL int_
CLint + Qh
Rearrangement of equation to describe
relationship in terms of CL int :
CL int = CLH * Qh
( Qh -CLH)
CLint – Intrinsic clearance. The
inherent ability of the liver to
metabolize drugs in the absence of
limitations. Ideal situation. Reflects
total enzyme activity.
CLH- “actual clearance” – based on
intrinsic enzyme activity and
limitations (factors which limit
access to metabolic enzymes).
These equations allow us to describe
CLH and ER based on liver blood
flow and enzyme parameters
Describing clearance in all possible terms
(ie- using the more complex equations,
which factor in CLint) allows us to
estimate drug clearance when
physiologic or disease conditions causes
changes in either liver blood flow or
intrinsic enzyme activity.
Intrinsic enzyme activity can change:
– Genetic polymorphisms
– Environmental pollutants
enzyme induction
– Drug-drug interactions
enzyme induction/ inhibition.
- Hepatic Disease
Liver Blood flow can change:
–
–
–
–
–
Activity ( Q)
Posture
Food ( Q)
Hepatic Disease
Changes in cardiac output
Estimating Impact of Changes
Relative impact of changes in Q or enzyme
activity (Clint) on the hepatic clearance,
bioavailability or half-life of a drug
depends on how efficiently the drug is
removed/extracted by the liver
Generally ***…..
High: ER > 0.7
Very efficiently removed from liver.
Low: ER< 0.3
Low efficiency in extraction
Intermediate ER 0.3 - 0.7
****This an arbitrary division of groups –
there is no absolute ranking system.
Typical drug examples
High ER :
Verapamil, lidocaine, propranolol,
nitroglycerin, cocaine, morphine
Intermediate ER:
Aspirin, Quinidine
Nortriptyline
Low ER:
Antipyrine, NSAIDs, Diazepam,
Erythromycin, Phenytoin
Theophylline, Warfarin
* Low ER does not mean it is not
metabolized.
Impact of variability in Q
and enzyme function on
Hepatic Clearance (CLH)
CLH = Qh * CL int_
CLint + Qh
Highly Extracted Drugs
Clint >>> Qh
CLH
CLint is approx
equal to
( CLint + Qh )
Qh * CL int_
CLint
CLint terms cancel out.
CLH Qh
Hepatic clearance approximates blood
flow.
Qh is limiting factor
Flow dependent/limited.
Low Extracted Drugs
(ER<0.3)
CLH = Qh * CL int_
CLint + Qh
Qh >> CL int
So (Clint + Q) is approx equal to Q
CLH
Qh * CL int_
Qh
CLH CL int
Hepatic Clearance approximates
inherent metabolic activity.
CLint is limiting factor
CAPACITY LIMITED.
Effect of Physiological changes
on CLH
Based on this…should be able to
make”quick” initial prediction on drug
metabolism & clearance for high and
low extracted drugs.
• No shortcuts for Intermediate Extraction
drugs.
• Relative changes in ER (bioavailability)
will be differentially affected by changes
in Q or CLint .
• The relative tendency after moderate
changes.
For instance if blood flow decreases to 0 ……
You should be calling 911, not estimating
hepatic clearance.
• Dramatic changes will affect clearance of
all drugs.
Dosage Route
1) IV doses
-Consider effects on hepatic
clearance and t½.
2) Oral doses
- Consider effects on 1st pass
through liver (fer) , hepatic
clearance and t½
- 1st pass is an important parameter
for High E drugs.
- Since so much drug enters liver
on 1st pass, both Qh and CL int are
important
- If Q too fast: ed access to
enzymes
Impact of Variability of
liver blood flow and
enzyme activity on oral
bioavailability.
fer = 1 - ER
substitute in equation
for ER as defined by CLint
= 1- [ CL int/ (CLint+Qh)]
fer =
High ER:
__Qh___
CL int + Qh
CL int >> Qh
fer Qh / CL int
* fer is dependent on BOTH
Qh and CLint
Change in Blood Flow:
Sample Problem
Two drugs (A & B) are completely
metabolized in the liver by CYP2D6.
The following is known about A & B*
* Blood data. Qh = 1.5 L/min
DRUG
V (L)
CLT (L/min)
t1/2 (hr)
A
B
30
30
0.15
1.35
2.31
0.26
• Intestinal absorption is complete for
both drugs.
Q. Determine expected CLT, t1/2 and F
of Drug A & B in congestive heart
failure patients which have a 40% in
cardiac output
- 40% CO
Solution:
-
(CO by 40%) then Q by 40%
Assume CL int is unchanged
i)
Calculate original CL int
- based on original values of Q &
CLH.
ii) Determine CLH
use new Q and original CL int
iii) Determine t½ using new CLT
(CLT = CLH)
- assume V not changed
iv) Calculate ER
- use new CLH and new Q
v) Calculate fer using new ER
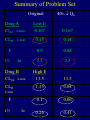
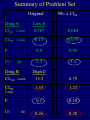
Summary of Problem Set
Original
Drug A
Clint L/min
CLH
L/min
F
t½
hr
Drug B
CLint L/min
CLH
40% Qh
Low E
0.167
0.167
0.15
0.14
0.9
0.84
2.3
2.5
High E
13.5
13.5
1.35
0.84
0.1
0.06
0.26
0.41
L/min
F
t½
hr
LIVER BLOOD FLOW
ER = 0.1
IV
ER = 0.9
CLH
↑ t½
fer
CLH
↑ t½
PO
High ER: fer Qh / CL int
Changes in Enzyme
Activity. Problem –part B
Two drugs (A & B) are completely
metabolized in the liver by CYP2D6.
The following is known about A & B*
* Blood data. Qh = 1.5 L/min
DRUG
V (L)
CLT (L/min)
t1/2 (hr)
A
30
0.15
2.31
B
30
1.35
0.26
• Intestinal absorption is complete for both
drugs.
Q. Calculate the expected CLT, t1/2
and F of Drug A & B in patients
with CYP2D6 polymorphism that is
associated with 50 % in enzyme
activity ( 50 % CLint ).
Solution :
•
Assume only CLint changes,
- no change in Q.
i)
Calclulate original CL int .
ii) Calculate new CL int .
Polymorphism: 50% CL int
iii) Determine CLH
- use new CL int and original Q
CLH = Qh * CL int_
CLint + Qh
iv) Determine t1/2 using new CLT
(CLT = CLH)
- assume V not changed
v) Calculate ER using new CLH
- with original Q
vi) Calculate fer
Summary of Problem Set
Original
Drug A
Clint L/min
CLH
L/min
F
t½
hr
Drug B
CLint L/min
CLH
50% Clint
Low E
0.167
0.084
0.15
0.079
0.9
0.95
2.3
4.4
High E
13.5
6.75
1.35
1.23
0.1
0.18
0.26
0.28
L/min
F
t½
hr
INTRINSIC CLEARANCE
ER = 0.1
IV
ER = 0.9
CLH
↑t½
CLH
↑t½
F
PO
High ER: fer Qh / CL int
Review graphs depicting
general changes in plasma drug
concentration time curves with
alterations in Q or CLint
Page 342 –343
Applied Biopharm & PK 5th Ed.
--
Dosage Adjustment in
patients
Still talking about the same two drugs…
The standard daily oral dose required
to obtain a therapeutic steady state
concentration in normal patients is:
Drug A = 25 mg
Drug B = 200 mg
Q. Calculate the oral dose of Drug A
and Drug B required in patients
with the CYP2D6 polymorphic SNP
varients (50% activity).
Css = FN *DOSEN
CLTN *τ
= FP *DOSEP
CLTP* τ
• Using N subscript to refer to normal and P
subscript to refer to patient with polymorphism.
• If using same dosing intervals (τ) –
terms cancel out
So….
FN *DOSEN
CLTN
= FP *DOSEP
CLTP
Solution:
Drug A
Normal: F =0.9 CLT= 9 L/hr
Dose = 25 mg every 24 hr
Polymorphism : F= 0.95 CLT =4.75 L/hr
Dose = ? mg / 24 hr
Drug B
Normal: F =0.1 CLT= 81 L/hr
Dose = 200 mg every 24 hr
Polymorphism: F= 0.18 CLT = 73.8 L/hr
Dose = ? mg / 24 hr
Real Life Situation
Many cases occur in which we do
not have all of this information for a
specific drug (ie- values for hepatic
or total body clearance) or person
(blood flow or enzyme activity in
individual).
Assessment of Liver function
in patients
Want marker/measure of hepatic function
which we can use to predict CLH of
drugs.
• Like creatinine clearance in renal disease
Major difficulty in estimating CLH is that
hepatic disease has different effects on
different enzyme systems
• Numerous pathways of drug metabolism.
• Drugs may be metabolized by > 1
enzyme.
NO GOLD STANDARD or parameter to
classify patients with hepatic impairment
(HI).
- Child-Pugh Index has been used in PK
studies to classify patients into very broad
categories of hepatic function (normal,
moderate liver disease, severe liver disease)
- Liver function tests (ALT, AST) only indicate
that liver damage has occurred.
Liver function tests
1) Antipyrine
marker of enzymatic capacity
Hepatic Clearance independent of Q
2) Indocyanine Green (ICG)
High E (E 0.7-0.9) dye
Hepatic Clearance related to Q
3) Galactose blood conc.
Quantitative liver function test
Measure galactose conc. 1 hour after
administration of 0.5 g/kg.
4) Erythromycin Breath Test
in vivo test to measureCYP3A activity.
IV Admin of 14 C-labeled erythromycin
analyze 14-C in expired breath after 20 min.
*Very specialized tests used experimentally,
clinical research studies – not used in
general clinical practice.
Dosage Considerations in Hepatic
Disease
- Most liver function tests only
indicate that the liver has been
damaged; they do not assess the
function or CLint of specific
enzymes in liver.
- Hepatic blood circulation and flow
is also difficult & $$$$ to assess in
clinical settings.
- Hence, patients with hepatic failure
(or enzyme deficiencies) are often
dosed based on estimations of the
remaining liver function (or enzyme
activity) and knowledge of the
fraction of drug eliminated via that
route.
Fraction of drug
metabolized
[CLH] HI: Hepatic CL in liver disease
[CLH] Norm: Hepatic CL in normal
[ CLT]: Total body clearance
fm: fraction of drug metabolized ( 1-fe)
RL = Remaining liver function
= [CLH] HI/ [CLH] Norm
[CLT]HI = [CLH] HI + [CLR]Norm
[CLT]HI = RL*[ CLT]norm * fm + [CLT]norm* fe
Thinking in Terms of Dose:
DOSEHI = [(RL * fm) + fe ] * DOSEnorm
Problem
A novel drug Prostop used to treat prostrate
cancer, is excreted primarily through
metabolism (95%). In patients in
normal hepatic function, the average
total body clearance is 62 L/hr, the t½
is 5.5 hours and the normal daily dose
is 250 mg every 8 hours.
For patients with severe liver disease with a
50% reduction in hepatic function :
Estimate the clearance and t½ of Prostop
Recommend a daily dosing regimen.
Solution
Drug: Prostop
fraction metabolized (fm) = 0.95
Assume non-metabolized is cleared
renally {fe = 0.05}
CLTnorm 62 L/hr
DOSEnorm 250 mg every 8 hours
Patients with liver disease:
50% remaining liver function (RL)
Assume normal renal function
Assume Vd is not affected
Drug:
fm = 0.95 fe = 0.05 CLTnorm = 62 L/hr
Patients: RL = 0.5
i) Estimate Clearance in these patients.
[CLT]HI = [CLH] HI + [CLR]Norm
= { RL*[ CL]norm *fm} + {[CL]norm* fe}
ii) Calculate t½ in these patients.
CLT = K * V
t ½ = 0.693 * V /CLT
* 1st need to calculate Vd (not changed
from normal)
Normal : t½ = 5.5; CLT = 62 L/hr
Liver failure: CLT = 32.55 L/hr; t½ = ?
iii) Dosage Recommendation
DOSEnorm = 250 mg Q8H = 750 mg/day
* Drug available in 100, 250, 500 mg caps.
DOSEHI = [(RL * fm) + fe ] * DOSEnorm
Could also use this method to
calculate dose for polymorphisms of
enzyme activity when CLint values
are unknown & can not be
calculated based on CLH.
- Consider fraction metabolized by
polymorphic enzyme and remaining
enzyme activity.
Practice Problem 1
Prezic is a newly marketed
antidepressant drug, eliminated by
hepatic metabolism and renal excretion.
Plasma and urine data was determined
following administration of 10 mg IV
dose to a 68 kg male subject (45 years
old). Assume a liver plasma flow rate of
825 ml/min.
PLASMA DATA (Prezic) :
AUC 0-24 = 256 g*hr/L
AUC 0-inf = 256.2 g*hr/L
t½ = 3 hr
URINE DATA:
Urine Collection Period
0-6 hr
6-12 hr
12-24 hr
Amount in urine (mg)
0.489
0.122
0.031
Q. Calculate CLT, CLr, CLint and ER for
Prezic in this patient.
Practice Problem 1b
Administration of acebutolol causes a
reduction in hepatic plasma flow
to approximately 650 ml/min.
Estimate the hepatic clearance and t 1/2 in this
Patient if Prezic is taken with acebutolol.
Assume that neither renal clearance or intrinsic
clearance is affected.
A. CLH = ________________ L/hr?
B. t 1/2 = ________________ hr?
Practice Problem 2.
On the graph below, draw a representative line
(exact numbers not required) depicting the
anticipated change in plasma concentration
versus time curve for a highly extracted
drug when:
a) liver blood flow is reduced
b) liver blood flow is increased?
100
Cp
10
1
0.1
0
5
10
15
20
25
30
Time
For each line, use a different color or line format
and label the lines accordingly..