* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Appendix B - Chickenpox
Survey
Document related concepts
Neglected tropical diseases wikipedia , lookup
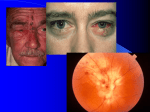
Immunocontraception wikipedia , lookup
Surround optical-fiber immunoassay wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Germ theory of disease wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Henipavirus wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
DNA vaccination wikipedia , lookup
Infection control wikipedia , lookup
West Nile fever wikipedia , lookup
Globalization and disease wikipedia , lookup
Vaccination wikipedia , lookup
Hepatitis B wikipedia , lookup
Transcript
Infectious Diseases Protocol Appendix B: Provincial Case Definitions for Reportable Diseases Disease: Varicella (Chickenpox) Revised January 2014 Varicella (Chickenpox) 1.0 Provincial Reporting Confirmed cases of disease 2.0 Type of Surveillance Case-by-case and aggregate reporting 3.0 Case Classification 3.1 Confirmed Case Clinical evidence of illness (see section 5.0) and laboratory confirmation of infection: • Isolation or direct antigen detection of varicella-zoster virus (VZV) from an appropriate clinical specimen (e.g., vesicle/lesion fluid or swab) OR • Detection of VZV deoxyribonucleic acid (DNA) OR • Seroconversion or a significant rise (e.g. fourfold or greater) by any standard serologic assay in varicella-zoster Immunoglobulin G (IgG) titre between acute and convalescent sera OR • Positive serologic test for varicella-zoster Immunoglobulin M (IgM) antibody OR Clinical evidence of illness (see section 5.0) in a person with an epidemiologic link to a laboratory-confirmed case of chickenpox or VZV infection. 3.2 Probable Case Clinical evidence of illness in the absence of laboratory confirmation or epidemiological link to a laboratory confirmed case. Note: Probable case definitions are provided as guidelines to assist with case finding and public health management, and are not for reporting purposes. 4.0 Laboratory Evidence 4.1 Laboratory Confirmation Any of the following will constitute a confirmed case of varicella: • • Culture isolation of VZV Detection of VZV DNA by NAAT 2 • • • Antigen detection of VZV DNA Seroconversion or a significant rise (e.g. fourfold or greater) in VZV IgG titre by any standard serologic assay Positive serologic test for VZV IgM antibody using a capture assay 4.2 Approved/Validated Tests • • • • Standard culture for VZV Direct fluorescent antibody (DFA) test for VZV antigen NAAT for VZV DNA Commercial tests for anti-VZV IgG and IgM antibody For further testing information including specimen collection, refer to the Public Health Ontario Laboratories Test Directory, available at: http://www.publichealthontario.ca/en/ServicesAndTools/LaboratoryServices/Pages/Index.asp x Note: Lesion specimens should be sent to the Public Health Ontario Laboratories (PHOL) for virus detection and genotyping when it is necessary to differentiate between wild-type vs. vaccine strains. PHOL refers specimen samples to the National Microbiology Lab for genotyping. 4.3 Indications and Limitations • • • • • Detection of VZV may be performed in non-routine specimens (e.g., sterile or respiratory sites). Consult with the microbiologist at the PHOL prior to submitting specimen(s). Optimal recovery of VZV is achieved if specimens (e.g., vesicle/lesion fluid or swab) are obtained 2-3 days after rash onset and from fresh vesicles. For serology, an acute serum specimen for VZV IgM and IgG testing should be collected within 7-10 days of symptom onset and convalescent serum specimen for VZV IgG testing should be repeated 2-3 weeks after the initial (acute) sample. Caution must be taken when reviewing serological data without reference to the clinical evidence as the response to VZV reactivation (herpes zoster) may be the same as to primary varicella. For urgent testing in cases of VZV (e.g., pregnancy, immunocompromised), call the PHOL Customer Service Centre prior to submission. 5.0 Clinical Evidence Clinical illness is characterized by a pruritic rash with rapid evolution from macules to papules, vesicles and crusts; all stages may be simultaneously present; lesions are superficial and may appear in crops. 6.0 ICD Code(s) 6.1 ICD-10 Code(s) B01 Varicella 3 6.2 ICD-9/ICD-9CM Code(s) 052 Chickenpox 7.0 Comments Varicella-like rashes that occur within two weeks after immunization may be due to either wild-type or vaccine-virus. Appropriate specimen(s) should be collected for laboratory determination of wild-type vs. vaccine strains. After immunization, a varicella-like rash can present at the injection site or is generalized in 3%-5% of vaccinees after the first dose and 1% after a second dose, usually within five to 26 days. A varicella-like rash occurring between 5-42 days after varicella vaccination should be reported as an adverse event following immunization (AEFI) if they meet the provincial case definition specified in Appendix B AEFI, unless wild-type virus is detected. 8.0 Sources Public Health Agency of Canada. Varicella (chickenpox): nationally notifiable since 19241959, 1986 onwards. In: Case definitions for communicable diseases under national surveillance. Can Commun Dis Rep. 2009 [cited 2013 Aug 27];35S2:61. Available from: http://web.archive.org/web/20130521221647/http://www.phac-aspc.gc.ca/publicat/ccdrrmtc/09pdf/35s2-eng.pdf Ontario Agency for Health Protection and Promotion (Public Health Ontario).Varicella testing guidelines. Toronto, ON: Queen’s Printer for Ontario;2012. Available from: http://web.archive.org/web/20120111112240/http://www.oahpp.ca/services/specimencollection-guide.html. Public Health Agency of Canada (homepage on the Internet). Ottawa, ON: Her Majesty the Queen in Right of Canada; 2011. National Microbiology Laboratory - guide to services. Genotyping (wild-type vs. vaccine strain differentiation): Genotyping of varicella-zoster virus (VZV) to differentiate between wild-type strain and vaccine strain. 2011 Feb 18 [cited 2013 Aug 27]. Available from: http://www.nmllnm.gc.ca/guide2/tests_engview.php?refdiagID=227 Nationally Notifiable Diseases Case Definitions with Canadian Public Health Laboratory Network (CPHLN) and Epidemiologic Group Draft Edits. 2007. Based on case definitions as written in : Advisory Committee on Epidemiology. Health Canada. Case definitions for diseases under national surveillance. Can Commun Dis Rep. 2000 [cited 2013 Aug 27]; 26 Suppl 3:i-iv 1-122. Available from: http://www.phac-aspc.gc.ca/publicat/ccdrrmtc/00pdf/cdr26s3e.pdf. Pathogen Regulation Directorate, Public Health Agency of Canada. Varicella-zoster virus: Pathogen safety data sheet - Infectious substances. Ottawa, ON: Her Majesty the Queen in Right of Canada;2011 [cited 2013 Aug 27]. Available from: http://www.phac-aspc.gc.ca/labbio/res/psds-ftss/var-zo-eng.php. Lopez A, Schmid S, Bialek, S. Chapter 17: Varicella. In: Roush SW, McIntyre L, Baldy LM, eds. Manual for the surveillance of vaccine-preventable diseases. 5th ed. Atlanta, GA: Centers for Disease Control and Prevention; 2011. Available from: http://www.cdc.gov/vaccines/pubs/surv-manual/chpt17-varicella.html. 4 Roush, SW, Beall, B, Cassiday, MS, Gentsch, J, Icenogle, J, Mayer, L, et. al. Chapter 22: Laboratory support for the surveillance of vaccine-preventable diseases. In: Roush SW, McIntyre L, Baldy LM, eds. Manual for the surveillance of vaccine-preventable diseases. 5th ed. Atlanta, GA: Centers for Disease Control and Prevention; 2012 [cited 2013 Aug 27]. Available from: http://www.cdc.gov/vaccines/pubs/surv-manual/chpt22-lab-support.html. 9.0 Additional Resources Ontario. Ministry of Health and Long-Term Care.Timely entry of cases and outbreaks. iPHIS Bulletin. Toronto, ON: Queen’s Printer for Ontario; 2012:17 (or as current). National Notifiable Diseases Surveillance System (homepage on the Internet). Atlanta, GA: Centers for Disease Control and Prevention; 2010. 2010 case definition: Varicella (chickenpox). 2012 Dec 7 [cited 2013 Aug 27]. Available from: http://wwwn.cdc.gov/NNDSS/script/casedef.aspx?CondYrID=890&DatePub=1/1/2010 12:00:00 AM 10.0 Document History Table 1: History of Revisions Revision Date January 2014 Document Section General Description of Revisions New template. Sections 9.0 Additional Resources and 10.0 Document History Added. 3.1 Confirmed Case First sentence changed from “Laboratory confirmation of infection with clinically compatible signs and symptoms in the absence of recent immunization with varicella-containing vaccine” to “Clinical evidence of illness (see section 5.0) and laboratory confirmation of infection”. First bullet point changed from “Isolation or direct antigen detection of varicella-zoster virus (VZV) from an appropriate clinical specimen (e.g., vesicle/lesion fluid or swab submitted in viral transport media)” to “Isolation or direct antigen detection of varicella-zoster virus (VZV) from an appropriate clinical specimen (e.g., vesicle/lesion fluid or swab)”. Second bullet point changed from “Detection of VZV DNA by nucleic acid amplification test (NAT)” to “Detection of VZV deoxyribonucleic acid (DNA)”. Final sentence changed from “Clinically 5 Revision Date Document Section Description of Revisions compatible signs and symptoms” to “Clinical evidence of illness (see section 5.0) in a person with an epidemiologic link to a laboratory-confirmed case of chickenpox or VZV infection”. 3.2 Probable Case Addition of probable case. 4.1 Laboratory Confirmation Changed from “Any of the following will constitute a confirmed case of Chickenpox: Positive for varicella-zoster virus (VZV) IgM antibody, Seroconversion or rise in VZV specific IgG titre, Positive VZV culture with immunofluorescence (IF), Positive NAT for VZV” to “Any of the following will constitute a confirmed case of varicella: Culture isolation of VZV, Detection of VZV DNA by NAAT, Antigen detection of VZV DNA, Seroconversion or a significant rise (e.g. fourfold or greater) in VZV IgG titre by any standard serologic assay, Positive serologic test for VZV IgM antibody using a capture assay” 4.2 Approved/ Validated Tests Second bullet point added (“Direct fluorescent antibody (DFA) test for VZV antigen”). Final two paragraphs added (“For further testing information…” and “ Note” Lesions specimens should be sent to Public Health Ontario Laboratories…”). 4.3 Indications and Limitations First, second, third and fourth bullet points added. 5.0 Clinical Evidence Deletion of “and have a predominantly central to peripheral distribution” from end of sentence. 7.0 Comments Entire section revised. 8.0 Sources Updated. 6 © 2014 Queen’s Printer for Ontario