* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
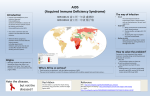
Download Acquired Immunodeficiency Syndrome (AIDS/HIV)
Neglected tropical diseases wikipedia , lookup
Trichinosis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Schistosomiasis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
West Nile fever wikipedia , lookup
Oesophagostomum wikipedia , lookup
Neonatal infection wikipedia , lookup
Hepatitis C wikipedia , lookup
Hepatitis B wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Diagnosis of HIV/AIDS wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Epidemiology of HIV/AIDS wikipedia , lookup
Microbicides for sexually transmitted diseases wikipedia , lookup
Back to REPORTABLE DISEASES Acquired Immunodeficiency Syndrome (AIDS/HIV) Reporting Obligations Laboratory confirmed cases of HIV infection shall be reported to the local Health Unit. Epidemiology Aetiologic Agent: The human immunodeficiency virus (HIV) is a retrovirus of which two types have been identified: type 1 (HIV-1) and type 2 (HIV-2). They are serologically and geographically distinct but have similar epidemiological characteristics. The pathogenicity of HIV-2 may be lower than that of HIV-1; they have genotypic and phenotypic differences. HIV-2 has lower disease progression and lower rates of mother-to-child transmission. Clinical Presentation: AIDS is a severe, life threatening clinical condition and is an advanced HIV related disease. This syndrome represents the late clinical stage of HIV infection resulting from progressive damage to the immune system, leading to one or more of many opportunistic infections and cancers of which bacterial pneumonia is one of the common presentations. Symptoms of acute HIV infection may include fever, arthralgia or myalgia, rash, lymphadenopathy, sore throat, fatigue, headache, oral ulcers and or genital ulcers, weight loss, nausea, vomiting or diarrhea. Acute symptoms, if present, occur two to four weeks after the initial infection and last from one to two weeks or as long as several months. In Canada, AIDS is diagnosed when a person with HIV develops one or more “AIDS- defining” symptoms. Modes of transmission: • Person- to- person through unprotected sexual intercourse • Contact with infected body fluids: sexual fluids, blood, and breast milk • The use of HIV infected-contaminated needles and syringes and some drug paraphernalia, including sharing by injection drug users • Transfusion of infected blood or its components, organ and tissue transplants • Contact of abraded skin or mucosa with body secretions such as blood, semen and CSF • The presence of another STI in either the source or the exposed person, particularly ulcerative lesions such as syphilis or genital herpes, increases the potential for sexual transmission of HIV. • Occupational exposure to HIV infection: percutaneous injury with a sharp object potentially contaminated with blood or other bodily fluid: mucous membrane exposure to blood or other bodily fluid • Vertical transmission from mother to infant during pregnancy, delivery or breast feeding • While virus has occasionally been found in saliva, tears, urine and bronchial secretions, transmission after contact with these secretions in the absence of blood has not been reported REPORTABLE DISEASES TOOLKIT Information for Health Care Professionals Incubation Period: Variable: time from initial infection to detectable antibodies (window period) is usually 1-3 months. The time from HIV infection to diagnosis of AIDS has an observed range of less than one year to 15 years or longer. Period of Communicability: Not known precisely; begins early after onset of HIV infection presumably extending throughout life. Infectivity during the first months is considered to be high; it increases with viral load, with worsening clinical status and with the presence of other STIs. Risk Factors/Susceptibility The Ontario Advisory Committee on HIV/AIDS has identified four populations at greatest risk of acquiring HIV/AIDS in Ontario, including gay and bisexual men, African and Caribbean Ontarians, Aboriginal Ontarians and people who use injection drugs. See Modes of Transmission for specific risk factors. Diagnosis & Laboratory Testing The diagnosis of HIV infection is based primarily on a positive serologic test. Persons with HIV infection may be totally asymptomatic. Therefore, serologic testing is recommended when there is a high index of suspicion (e.g., high-risk behaviour and/or suspicious clinical symptoms and signs). Persons may also present with specific opportunistic infections or other conditions indicative of underlying immunosuppression. See ‘PHO Labstract May 2016, HIV patient information sheet: If You’ve Just Found Out You Are HIV Positive’. TESTING INFORMATION & REQUISITION Treatment & Case Management The Public Health Agency of Canada provides information related to: screening, testing, post-test procedures, post-diagnosis clinical management and disclosure of HIV. Patient Information PATIENT FACT SHEET Additional Resources 1. Public Health Agency of Canada, “Human Immunodeficiency Virus – HIV Screening & Testing Guide.” 2. CATIE. “Canada’s source for HIV and hepatitis C information.” 3. Canadian AIDS Society publication. “HIV Transmission: Factors that Affect Biological Risk”, 2013. 4. AMMI Canada, The Use of Early Antiretroviral Therapy in HIV-infected Persons. References 1. Ministry of Health and Long Term Care, Infectious Diseases Protocol, 2014. 2. Heymann, D.L., Control of Communicable Disease Manual (19th Ed.), Washington, American Public Health Association, 2008. Leeds, Grenville & Lanark District Health Unit, Oct 2016